Abstract
Sleep is receiving increasing attention in public health. The aim of this umbrella review is to determine what non-pharmacological sleep health interventions have been evaluated among healthy populations, by examining target groups, settings, and effectiveness in improving sleep quality and duration. Comprehensive searches were conducted in five electronic databases (January 1975–February 2019), yielding 6505 records. Thirty-five articles were selected meeting the following eligibility criteria: (1) systematic reviews or meta-analyses of (2) sleep health interventions in (3) primarily healthy populations. Two reviewers independently screened for inclusion, extracted the data, and assessed the review quality. This umbrella review was registered with PROSPERO (CRD42019126291). Eleven intervention types were defined, and their effectiveness discussed. Substantial evidence demonstrated the effectiveness of later school start times, behavior change methods, and mind–body exercise. Other intervention types, including sleep education or relaxation techniques, demonstrated some promising impacts on sleep, but with less consistent evidence. Results were limited by high heterogeneity between studies, mixed results, and variable review quality. Nevertheless, this umbrella review is a first step towards understanding the current state of sleep health promotion and gives an overview of interventions across the lifespan.
1. Introduction
Sleep health has been defined as “a multidimensional pattern of sleep-wakefulness, adapted to individual, social, and environmental demands, promoting physical, and mental well-being” [1]. Insufficient sleep may contribute to chronic diseases, such as obesity [2], cardiovascular disease [3], and diabetes [4]. Lack of sleep may also lead to depression [5], other mood disorders [6], and reductions in cognitive performance, including memory and learning difficulties [7]. Workplace injuries, accidents, and medical errors can also result from insufficient sleep, as daytime drowsiness and fatigue can diminish alertness and decrease reaction time [8,9].
Poor sleep health is a global issue, and studies show an increasing prevalence of inadequate sleep [10,11]. One study estimated that, by 2030, the total number of older adults with sleep problems in low-income countries will be 260 million, an increase from 150 million in 2010 [10]. Ohayon (2011) estimated that the prevalence of people with sleep deficits in various countries ranged from 20% to 41.7% [12]. Worldwide, insufficient sleep affects every age group, although in many countries it remains unidentified and underreported [10,13]. Poor sleep also negatively affects the world economy. A combined estimate for the U.S., Canada, the UK, Germany, and Japan, put the annual economic loss due to sleep problems at USD 680 billion [14].
Most large-scale public health education programs and campaigns have been created to influence diet and exercise, without considering sleep [15,16]. Likewise, the US health agenda in 2010 included guidelines for physical activity and diet as important health-related behaviors, and sleep was not included [17]. However, sleep has recently made its way onto the US health agenda [18], and sleep deprivation reduction is also an emerging public health priority in the UK [19].
Therefore, the aim of promoting healthy sleep is expected to receive growing attention in the next decades. Sleep health promotion involves improving sleep duration and quality. Such work targets sleep-related health behaviors and knowledge among healthcare professionals, policy makers, and the general population [20,21]. Sleep duration is normally defined as the cumulative amount of sleep during the nightly episode of rest, or over a 24-h period [22]. Sleep quality is described as “one’s satisfaction with the sleep experience, integrating aspects of sleep initiation, sleep maintenance, sleep quantity, and refreshment upon awakening” [23]. Measures and tools for measuring sleep duration and quality vary, and can be classified as objective or subjective.
Several systematic reviews and meta-analyses have been conducted on sleep health interventions, examining different intervention types, target groups, and settings. However, an ‘umbrella review’, providing an overview of all systematic reviews published across the wide-ranging field of sleep health promotion, is missing from the literature. The purpose of this umbrella review is to systematically summarize the scope and effectiveness of sleep interventions in primarily healthy populations, i.e., not diagnosed with a sleep disorder or specific disease. More specifically, it aims to determine what kinds of non-pharmacological sleep health interventions have been implemented, in what target groups and settings, and how effective they are in improving sleep quality and duration. This overview of sleep health interventions across the lifespan is also meant to introduce interested researchers to this relatively new field of sleep health.
2. Materials and Methods
2.1. Search Strategy and Selection Criteria
The Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines were adapted for conducting this umbrella review [24]. A systematic search was implemented using six online bibliographic databases/search engines: PubMed, Medical Literature Analysis and Retrieval System Online (MEDLINE), the Psychological Information Database (PsycINFO), Excerpta Medica dataBASE (Embase), the Cumulative Index to Nursing and Allied Health Literature (CINAHL), and the Cochrane Library, from 1975 to January 2019. The search terms “health education”, “intervention”, “sleep”, “program evaluation”, and related synonyms, were used in the search strategy, including Medical Subject Headings (MeSH) terms in PubMed and thesaurus terms in PsycINFO. A filter was used to limit the retrieved articles to systematic reviews and meta-analyses. The search syntax is available in Appendix A.
Selection criteria were established using the PICOS strategy (Population, Intervention, Comparison, Outcome, Study design). Articles had to include (1) primarily healthy populations (i.e., systematic review/meta-analysis should not be directed at populations with a specific diagnosed (sleep) disorder); (2) sleep health promotion interventions; (3) any public health intervention settings (i.e., not laboratory settings); (4) the evaluation of sleep duration and/or quality; and (5) a systematic review or meta-analysis study design. Only references published in English were eligible. Reviews involving a majority of research participants diagnosed with sleep disorders or other specific conditions, like cancer, were excluded. Articles were also excluded if they were not published in scientific journals, e.g., theses, book chapters, and conference proceedings. This review was registered a priori with PROSPERO (CRD42019126291).
2.2. Screening and Data Extraction
After removing duplicates, two researchers (U.A. and L.P.) first screened the titles and then the abstracts, using the selection criteria. In cases of disagreement, articles were included in the next step. The researchers then performed full-text screening and any disagreements were resolved through discussion with a third reviewer (R.M.).
Two reviewers (U.A. and E.D.) extracted the data independently and any disagreements were resolved through consultation. The Joanna Briggs Institute form was adapted for data extraction. Designs of included studies were categorized into three types: RCTs, crossover study, and quasi-experimental. The quasi-experimental category comprised controlled non-randomized, pre-/posttest, and time series designs [25].
While extracting the data, definitions of the intervention types were developed considering the interventions most commonly found in the literature. The studies of each review were categorized as one of the defined intervention types; this allowed grouping of particular sleep promotion methods when examining their prevalence and effectiveness. Individual studies from selected reviews were “excluded” and not considered in the conclusions if they did not aim to measure any relevant sleep-related outcome, were conducted in a laboratory setting, or had unsuitable study designs for interventions. Results based on single studies were not listed in the results table, to avoid giving unjustified weight to individual studies.
2.3. Methodological Quality Assessment
Methodological quality was assessed using the JBI Critical Evaluation Controller for Systematic Reviews, which consists of 10 items, awarded 0 or 1 [26]. Quality scores of 0–5 were considered weak, scores of 6–8 were moderate, and scores of 9 or 10 were strong. Two reviewers (U.A. and E.D.) performed the assessment independently and disagreements were resolved by discussion with a third reviewer (R.M.).
A common limitation in umbrella reviews is the overlap of primary evidence. This occurs when different reviews reference the same component studies, leading to “double-counting” of results and overstating evidence [27]. A “corrected covered area” (CCA) measure, developed by Pieper et al. (2014), was calculated to evaluate this degree of overlap in the primary data [28].
3. Results
3.1. Description of Reviews
3.1.1. Included Reviews, Studies, and Quality Assessment
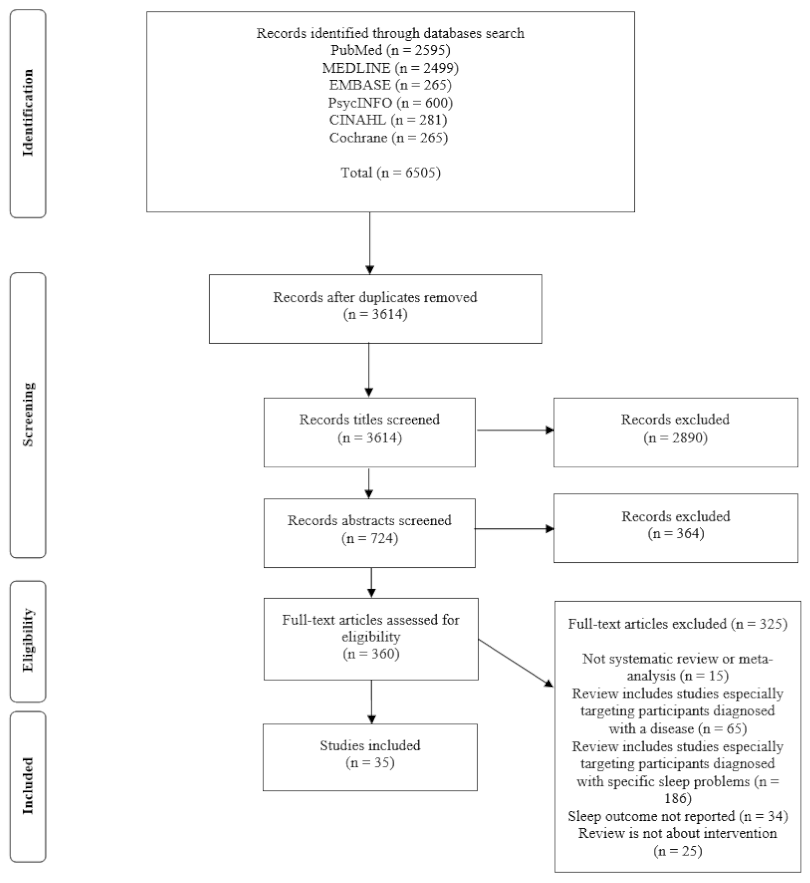
Thirty-five systematic reviews were included after screening, as depicted in Figure 1. Seventeen included meta-analyses. The number of studies included in these reviews ranged from 4 [29,30] to 112 [31]. A total of 552 primary studies were included. After examining the overlap between studies reported in multiple reviews, only 443 unique studies were found. Fifty-six studies were found in two reviews, and 21 other studies were included in three or more reviews. The CCA value was calculated at 0.72, which is interpreted as only a small overlap of the component studies [28].
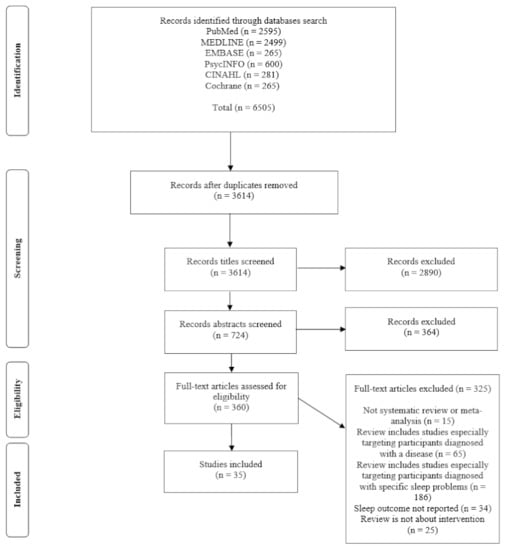
Figure 1.
PRISMA diagram of the literature search.
The quality assessment ratings are presented in Table S1: Ratings of the included reviews using the JBI Quality Assessment Criteria for Systematic Reviews. Twenty-one reviews were rated high quality, 11 moderate, and three low. For most reviews, the question, inclusion criteria, search strategy, sources used, and criteria for appraising studies were stated clearly. However, the assessment of potential publication bias was particularly lacking, and was not assessed in 20 reviews.
3.1.2. Intervention Types
Eleven intervention categories were grouped, mainly on the basis of the techniques used in the interventions and not, for example, on the theoretical background (Table 1). The intervention types were sleep education, behavior change methods (BCM), relaxation techniques, physical exercise, mind–body exercise (MBE), aromatherapy and/or massage, psychotherapy, environmental interventions, and later school start times. Some reviews also included multicomponent interventions that incorporated multiple intervention types. There were also some other, less commonly observed interventions, such as hypnosis, biofeedback, and magnet therapy, which were gathered into an “other” category.

Table 1.
Categories of intervention types, definition, and population targeted.
3.1.3. Target Populations
The characteristics of the individual reviews are summarized in Table 2, by age categories. Five reviews included only infants and young children (0–5 years) [29,32,33,34,62], while ten reviews included school-aged children and/or adolescents (5–17 years) [35,36,37,38,39,40,47,59,60,61]. More than half of the reviews examined adults (>17 years), and four focused exclusively on elderly populations [30,31,41,42,43,44,45,46,48,49,50,51,52,53,54,55,56,57,58,63]. Some reviews included only very specific groups, such as college students [30,44], shift workers [41,49], athletes [42], or pregnant women [51].

Table 2.
Characteristics of and conclusions on the effectiveness of the intervention types of the included reviews: categorized by age category.
3.1.4. Intervention Settings
Most reviews included studies that were conducted in multiple settings [29,31,32,33,34,35,36,38,41,43,45,46,49,51,52,57,58,62,63]. In reviews that focused on single intervention settings, these included schools [37,39,59,60,61], universities [30,44], the community [54,55], the workplace [49], outpatient settings [47], hospitals [48,50], nursing homes [56], and gyms [53]. One review did not clearly report the setting [42].
3.1.5. Sleep Measures
Sleep duration was usually measured using the total sleep time (TST) in a single night or the average TST across a period of time. Sleep quality was measured through composite scores on questionnaires, like the frequently used Pittsburgh Sleep Quality Index (PSQI). Sleep onset latency (SOL) was also considered a sleep quality measure. In infants and young children, the number of night awakenings and bedtime problems were considered indicators of sleep quality [34,62].
Both objective and subjective tools were used to measure outcomes. Actigraphy and polysomnography were commonly used objective tools. Subjective tools included many sleep indices, such as the PSQI or the Insomnia Severity Index, as well as other self-report tools like parent reports, sleep diaries, interviews, and non-standard questionnaires. Twenty-nine reviews included a combination of subjective and objective measures. Four reviews included studies that only measured sleep outcomes subjectively, while two reviews did not identify the measuring techniques.
3.2. Types of Interventions and Their Effectiveness
Table 2 displays the review characteristics, including types and descriptions of interventions, number of eligible studies, study designs, populations, and the results by review. Below, each intervention type and the evidence of its effectiveness is reviewed systematically.
3.2.1. Sleep Education
Seventeen reviews included sleep education, with wide variations in approaches [29,30,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46]. These interventions included information on sleep health, sleep cycles, consequences of insufficient sleep, and/or sleep hygiene tips. However, some reviews provided only vague descriptions of the content included. Many methods were used to deliver sleep education, including seminars, pamphlets, telephone calls, and online information. Targeted populations for sleep education varied, but college students and parents with infants and young children were common.
Ten out of the seventeen reviews showed small positive effects of sleep education on sleep duration and/or quality measures [29,32,33,34,35,37,38,39,42,43], though in three, the effects were not maintained at follow-up [35,38,39]. For the remaining reviews, two showed no significant effects on sleep duration [44,46], and one reported insufficient evidence [30]. Although sleep education interventions were included in the meta-analyses in four other reviews, they were combined with different intervention types, so no conclusions could be drawn [36,40,41,45]. In two reviews, interventions aimed to increase sleep knowledge in school settings [30,37]. While these reviews showed increases in sleep-related knowledge, this was not accompanied by any change in sleep-related behaviors or sleep quality/duration. While some sleep education interventions demonstrated small positive impacts on sleep duration and/or quality, the results were quite mixed.
3.2.2. Behavior Change Methods (BCM)
Eleven reviews covered BCM using varying techniques for different target populations [29,32,33,34,38,40,42,45,47,48,49]. A common target group for BCM was infants and children, with methods implemented by their parents. Examples of BCM are standardized bedtimes, scheduled awakenings, positive routines, controlled comforting, and gradual extinction (i.e., parents leave children alone for extended periods, ignoring protests and crying) [34,40,47]. Prescribed sleep wake schedules were used in infants, athletes, and shift workers [42,45,49]. BCM were also often employed in combination with sleep education.
In one review, each for infants, athletes, and shift workers, improvements in sleep duration and/or quality were demonstrated [33,42], while one review did not report sleep duration outcome data [49]. Three other reviews with infants and children showed improvement in sleep quality [34,40,47], and another showed improvement in both sleep duration and quality [32]. Two reviews demonstrated inconsistent evidence [38,48], and one did not report specifically on the effectiveness of BCM [45]. Overall, there is substantial evidence that BCM in infants and children (as managed by parents) increases sleep duration and quality [29,32,33,34,40,47]. There is also some encouraging (but more limited) evidence for other populations.
3.2.3. Relaxation Techniques
Nine reviews examined relaxation techniques [31,35,41,44,45,48,50,51,52]. Participants varied in the reviews (adolescents, shift workers, college students, pregnant women, and hospitalized adults). The diversity of techniques used in this category was notable, ranging from progressive muscle relaxation, to mindfulness, relaxing music, etc.
Improvements in sleep duration and/or quality varied from small to large positive effects. Sleep quality was measured in most reviews, while fewer examined sleep duration. One review showed that varying relaxation techniques improved sleep quality with a medium effect size [44]. One review demonstrated that relaxation had small to large positive effects on sleep quality [50], while another review demonstrated mixed results on sleep duration and quality [31]. In five reviews, relaxation techniques were not separately described in terms of effectiveness [35,41,45,48,51]. The strongest evidence in this category was for listening to relaxing music, supported by a meta-analysis [52]. Evidence for other relaxation techniques was more mixed.
3.2.4. Physical Exercise Interventions
Seven reviews assessed the effect of physical exercise on sleep outcomes, including aerobic exercise [45,51,53,55], shadow boxing [54], Pilates [46], and low-intensity exercise [56]. The participant groups varied, but the reviews targeted more women than men, including some specific subgroups: postmenopausal, pregnant, postpartum, and middle-aged women.
The effectiveness of physical exercise in improving sleep also ranged from small to large effects. One review showed small effects on sleep quality [55], while three reviews showed large effects on sleep quality [46,51,53]. Mixed results on sleep duration were reported in one review [56], while another review showed medium effects on sleep duration [54]. One meta-analysis combined a physical exercise study with different interventions, not reporting the effectiveness of physical exercise alone [45]. Physical exercise interventions have shown some promising improvements in sleep duration and quality, but the sample sizes in these reviews were relatively small.
3.2.5. Mind–Body Exercise (MBE)
Mind–body exercise was categorized as a separate intervention type, combining physical activity with meditative components. Six reviews included studies that used MBE [31,51,53,54,55,57]. Common forms of MBE were tai chi, yoga, and Qigong, but there were also less-common techniques, such as the Rességuier method, which promotes patient awareness of bodily perceptions and control. Participants varied, but older adults were often targeted.
The effectiveness of MBE to improve sleep was mixed, but quite consistently positive. One review reported that tai chi had medium effects on sleep duration and large effects on sleep quality [54], while another reported that tai chi had small effects on sleep quality [55]. Another review assessed different types of MBE, and reported positive effects on sleep duration and quality [31]. For yoga interventions, one review reported improvement in sleep quality [51], while another showed no significant effects [53]. Moreover, a meta-analysis pooled data from 14 MBE interventions, demonstrating medium effects in improving sleep quality in older people with sleep complaints undiagnosed with sleep disorders [57]. MBE was investigated in many studies, including several RCTs, and consistently showed positive impacts, particularly in older adults.
3.2.6. Aromatherapy and/or Massage Interventions
Many interventions combined both aromatherapy and massage, so these two techniques were placed into one category. Six reviews examined aromatherapy and/or massage [46,48,50,51,56,58]. Participants varied, and these interventions were often conducted in healthcare settings, such as hospitals and nursing homes.
Two reviews demonstrated that massage combined with aromatherapy has larger effects on sleep quality than aromatherapy alone [46,50]. In contrast, one meta-analysis demonstrated the opposite; while sleep quality consistently improved, a subgroup analysis demonstrated that inhalation aromatherapy was more effective than a combined approach [58]. One review reported massage as the most promising approach to improve sleep quality among pregnant women compared to other interventions [51]. Additional reviews included interventions using both aromatherapy and massage, but the results were inconsistent [48,56]. Overall, there is some evidence of improvement in sleep quality with both massage and aromatherapy.
3.2.7. Environmental Interventions
Five reviews included environmental interventions [46,48,49,50,56]. There was notable variation in the techniques used to modify the environment to promote sleep. For instance, daytime bright-light therapy, through the influence of circadian rhythms, was used to improve sleep duration and quality among shift workers and hospitalized patients [48,49]. Nature sounds, white noise, or noise reduction were different techniques to augment the auditory environment [48,50]. Other interventions included infants staying in their mother’s hospital rooms [46], adjusting bedroom temperature levels, and reducing sleep interruptions for nighttime nursing [56]. Environmental interventions were often conducted in monitored facilities, such as hospitals or care facilities.
Evidence of the effectiveness of environmental interventions is mixed. One review reported that bright-light therapy and nature sounds had a large positive effect on sleep quality [50], and another reported that bright light improved sleep duration and/or quality, but not significantly [49]. Another review concluded that sleep duration and quality were improved through the use of bright light and white noise [48]. However, noise reduction and reducing night-time nursing care did not show increases in sleep duration [56]. One review examined environmental interventions with other interventions, and did not report specific results separately [46]. High heterogeneity and few studies were found in the literature, providing very limited evidence.
3.2.8. Psychotherapy
Four reviews included psychotherapy, conducted online, in groups, or one-on-one with therapists [40,41,44,46]. Most studies employed cognitive behavior therapy (CBT), but other psychotherapeutic interventions were also observed, such as implosive therapy and constructive worry. Participants varied, including college students, shift workers, and postpartum women.
The reported effectiveness of CBT differed. One review examined CBT and other psychotherapeutic methods, and it showed that CBT had large positive effects on sleep duration, SOL, and other sleep quality metrics. In the same review, other psychotherapeutic interventions showed medium impacts on sleep duration and some sleep quality measures, but not SOL [44]. This review provided the most substantial evidence for psychotherapy. The remaining three reviews combined CBT studies with other interventions, making it difficult to determine the effect of psychotherapy [40,41,46]. In the present umbrella review, we found limited evidence for the use of psychotherapy to promote sleep health in healthy populations.
3.2.9. Later School Start Interventions
Four reviews examined this intervention type, and participants were adolescents and children in formal school settings. School start times were delayed 20–85 min. Two meta-analyses reported an increase in sleep duration: one with a MD of 18–65 min and the other with a MD of 1.39 h [59,61]. In an additional review, the values of sleep duration increasing ranged from 25 to 77 min across the included studies [60]. The demonstrated effect substantially increased when start times were delayed more than 60 min in comparison to the controls. Overall, very large sample sizes were included in these interventions. This may suggest strong evidence for later school start times, despite the lower number of reviews.
3.2.10. Multicomponent Interventions
Eighteen reviews included multicomponent interventions, which combined techniques from multiple categories [29,31,32,33,34,36,37,38,40,41,44,45,48,49,50,51,56,62]. Interventions that combined sleep education and BCM targeting infants and children were common and showed positive effects on sleep duration and/or quality [29,32,33,34,62]. The substantial heterogeneity between the multicomponent interventions across different reviews preclude drawing a firm conclusion on their effectiveness.
3.2.11. Other Types of Interventions
Seven reviews included other less commonly observed interventions. These were dietary interventions, hypnosis, biofeedback therapy, magnet therapy, drinking herbal tea, acupuncture, cryostimulation (where the body is exposed temporarily to extremely cold temperatures), and infrared light treatment [31,42,44,46,50,51,63]. One review examined only dietary interventions, which aim to improve sleep by finely manipulating nutritional intake [63]. The review demonstrated no effects in natural (non-laboratory) settings. One review showed that infrared light irradiation and cryostimulation improved sleep duration and/or quality in athletes [42]. Acupuncture was reported in two reviews [50,51], and one demonstrated positive effects on sleep quality [51]. The effectiveness of other interventions varied, and there were few studies.
4. Discussion
Sleep health promotion is an emerging issue in public health. The aim of this research was to conduct an umbrella review, a review of reviews, of sleep health interventions in the general population. Common types of interventions, target groups, and settings were identified, and conclusions were drawn regarding effects on sleep duration and quality.
The scope of the reviews varied widely. Some were very broad, including all non-pharmacological sleep interventions and addressing multiple target groups. Reviews targeting only specific groups, such as shift workers, often included a wide range of intervention types, providing overviews of all sleep promotion interventions in that group. Other reviews only included one intervention type and addressed only one target group (e.g., later school times for children/adolescents). Furthermore, the methodological quality also varied, though many reviews were rated as high quality. Lower-quality reviews reported insufficient details on interventions, designs, methods, and results of the included studies, and/or failed to provide concrete recommendations. Only 7 of the 35 reviews adopted the PRISMA guidelines for reporting.
The most commonly observed intervention types were sleep education and behavior change methods. Sleep education interventions consist of providing basic education about sleep (e.g., what is sleep and its health benefits), often combined with sleep hygiene tips (e.g., ‘No caffeine in the evenings’). Sleep education is frequently conducted in school-aged populations, such as children or college students. Behavior change methods are interventions based on behavioral theories, i.e., strategies to improve sleep by augmenting certain associations with sleeping. Examples of this include using bedtime routines for children, or not rewarding attention seeking and crying at bedtime. As the examples show, behavior change methods often target infants, although some adult subgroups, such as athletes and shift workers, were targeted as well [42,49].
Another common intervention was relaxation techniques. This could involve using such techniques during the day (such as mindfulness) or specifically around bedtime (e.g., progressive muscle relaxation, and listening to music). In interventions defined as ‘mind–body interventions’, meditative techniques are combined with physical exercise, such as tai chi. In contrast, physical exercise interventions only involved physical activity to improve sleep, without explicit relaxation components (e.g., aerobics). While these three intervention types were observed in various target groups, mind–body and physical exercise were investigated in adults in particular [31,53,54,55,57].
Fewer reviews included aromatherapy and/or massage, which involved the use of fragrant oils that are inhaled or massaged into the skin. Massage is implemented alone or often in combination with aromatherapy, involving manual techniques implemented by a therapist (e.g., back massage and foot reflexology). These interventions are often observed in healthcare facilities, such as nursing homes. Another less commonly observed sleep intervention type is environmental interventions, the modification of sleep environments. Examples include bright light and noise or temperature adjustment, the techniques most often used in healthcare settings. Later school start times were also less commonly observed, which involved changing the time of school starts to correspond with the circadian rhythms of adolescents (teenagers undergo a delay in their sleep–wake rhythm, as a consequence of biological processes during puberty) [64]. However, this is the most common intervention for adolescents, when considering the number of study participants. School districts may set policies to start school days at 9:00 instead of 8:00, as is recommended by the included reviews [59,60,61]. Likewise, the American Academy of Pediatrics recommends that middle and high schools aim to start no earlier than 8:30 [65].
The most common example among the therapies was cognitive behavioral therapy, which aims to support patients in identifying and changing destructive or disturbing patterns of thoughts that negatively affect behavior and emotions [66]. It should be noted that cognitive behavioral therapy for insomnia is widely acknowledged as an effective treatment for people diagnosed with insomnia [67]. However, in the present review, addressing the general public, evidence for its effectiveness was limited. Lastly, multicomponent interventions were commonly observed. In particular, sleep education was often combined with behavior change methods, though physical exercise, mindfulness, and environmental modifications were sometimes combined with sleep education too.
Although the 11 defined intervention types adequately describe the sleep health interventions in the included reviews, the distinctions between the intervention categories were sometimes not as straightforward as might be assumed. For example, giving sleep hygiene tips was considered sleep education, but these tips often suggest bedtime relaxation or creating a dark, quiet sleeping environment. One could then argue that education on sleep hygiene also has relaxation and environmental components. Furthermore, CBT and BCM partly share their theoretical underpinning. Nevertheless, CBT and BCM were considered as separate intervention types, as techniques as well as implementers varied considerably. However, in determining the 11 intervention types, the main focus of an intervention could always be identified.
Three categories showed substantially more evidence for improving sleep duration and/or quality: behavior change methods, mind–body exercise, and later school start times. These categories consistently demonstrated statistically significant improvements with relatively large effect sizes. Many reviews featuring behavior change methods and mind–body exercise included rigorous RCT study designs. This included two meta-analyses primarily analyzing behavior change methods [33,62], and two meta-analyses of exclusively mind–body exercises [54,57]. Later school start times also demonstrated strong effects in two reviews with particularly large participant samples. The eight additional intervention types defined in this review also demonstrated some promising impacts on sleep, but with less research conducted and/or less consistent evidence. Some techniques demonstrated higher effectiveness than others within categories. For example, listening to music seemed to be more effective than other relaxation techniques.
These conclusions should be interpreted with caution. There was heterogeneity in study designs, outcome measures, populations targeted, and specific techniques. Generalization is another concern, as some data is from narrow target groups or settings and results may not be applicable in other contexts. For instance, physical exercise to improve sleep was mostly implemented for women, and environmental interventions were mainly applied in healthcare settings. These interventions may not demonstrate similar effectiveness in other populations or settings. Moreover, there were contradictory findings regarding the relative effectiveness of some specific techniques within categories. For example, one meta-analysis showed aromatherapy to be more effective than massage [58], while another showed that massage was the more effective technique of the two [46].
4.1. Strengths and Limitations
This review had some notable limitations. First, overlapping of primary studies between reviews is a common limitation in umbrella reviews. However, only a small amount of overlap was detected with the CCA calculation [28]. There was a high degree of heterogeneity, which made direct comparisons between reviews impossible. Publication bias may have limited what studies were published and included in reviews, which in turn may be a limitation of this umbrella review. Likewise, the quality of an umbrella review depends on the quality of the included reviews, which in turn depends on the quality of the primary studies. Therefore, there may be some undetected sources of bias. However, it is reassuring that the quality scores of most included reviews were strong.
A strength of this review was the broad variety of electronic databases in its search strategy, allowing a broad overview of all possible types of non-pharmacological interventions used across all age groups and settings. Two reviewers conducted the entire screening, data extraction, and quality assessment independently, increasing the validity of the extracted data and methodological strength of the research.
4.2. Implications for Practice and Future Research
Sleep health promotion has been gaining attention in public health, and effective interventions are being developed that improve sleep duration and quality in the general population. Currently, policies regarding sleep have been implemented within different countries and organizations, including later school start times, regulations for shift worker hours, and public education on sleep health [59,68]. Practitioners and policy makers may profit from the insights of this present review to extend such initiatives.
This review also suggests recommendations for future research. As previously mentioned, some intervention types have only targeted specific groups or have not been investigated thoroughly. For instance, mind–body and physical exercise has had promising results among adults and elderly people, so future research could demonstrate if this approach would be effective in children or adolescents. In this age of smartphone technology, apps may be a new channel for sleep intervention implementation, which could be further explored (e.g., to implement behavior control methods more systematically).
In the included reviews, the lack of behavioral theory in intervention development was surprising. Behavioral theory is used to effectively predict and alter many health behaviors, but its use has been very limited in sleep health [69,70]. In fact, only one included review specifically reported and emphasized the foundations of behavioral theory within its interventions [37]. While there is a small amount of research regarding the factors influencing sleep health and sleep behaviors [71,72], most interventions were not developed explicitly considering these factors, nor how they apply to specific target groups. More research into sleep-related factors and the application of theoretical frameworks of behavior change are lacking in the literature, requiring further research. To steer the reporting and comparability of reviews, following PRISMA guidelines is also heavily encouraged in future reviews.
5. Conclusions
This umbrella review is the first to provide an overview of strategies used in the rapidly evolving field of sleep health promotion, shedding light on target populations and intervention settings. Later school start times, behavior change methods, and mind–body exercise provided the most evidence of effectively improving sleep. Other interventions, such as sleep education, relaxation techniques, physical exercise, aromatherapy, massage, psychotherapy, and environmental interventions, also showed promising but inconsistent or limited results. Conclusions should be considered with caution, as there was high heterogeneity between studies. Nevertheless, this umbrella review can be seen as a first step towards reaching a greater understanding of sleep health promotion.
Supplementary Materials
The following is available online at https://www.mdpi.com/article/10.3390/ijerph18115533/s1, Table S1: Ratings of the included reviews using the JBI Quality Assessment Criteria for Systematic Reviews.
Author Contributions
R.M. and U.A. conceived the idea for the study; U.A. and E.D. performed the data extraction, synthesis, and quality assessments, with input of R.M.; U.A. wrote the first draft, and E.D. and R.M. made substantial contributions; and all authors contributed to the interpretation of findings, and critical revision of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by a scholarship to U.A. from the Saudi Arabia Ministry of Education (Albaha University).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All relevant data are within the manuscript.
Acknowledgments
Special thanks to Louk Peters for helping in the screening process.
Conflicts of Interest
There has been no conflict of interest declared.
Appendix A
PubMed Search Syntax.
((((((((((((((((((((((((((((((((((((((((((((((health education[MeSH Terms]) OR health education[Title/Abstract]) OR health promotion[Title/Abstract]) OR educat*[Title/Abstract]) OR promot*[Title/Abstract]) OR education program*[Title/Abstract]) OR Behavior*[Title/Abstract]) OR Behaviour*[Title/Abstract]) OR advice[Title/Abstract]) OR Sleep intervention*[Title/Abstract]) OR Sleep program*[Title/Abstract]) OR Sleep intervention program*[Title/Abstract]) OR Sleep hygiene intervention[Title/Abstract]) OR Sleep hygiene program*[Title/Abstract]) OR Sleep campaign*[Title/Abstract]) OR Sleep hygiene campaign*[Title/Abstract]) OR Sleep train*[Title/Abstract]) OR Sleep cours*[Title/Abstract]) OR Sleep improvement program*[Title/Abstract]) OR Sleep improvement intervention*[Title/Abstract]) OR Sleep management cours*[Title/Abstract]) OR Sleep management program*[Title/Abstract]) OR Sleep management intervention[Title/Abstract]) OR Sleep management campaign*[Title/Abstract]) OR Sleep module*[Title/Abstract]) OR Sleep hygiene module*[Title/Abstract]) OR Sleep intervention cours*[Title/Abstract]) OR Sleep hygiene cours*[Title/Abstract]) OR Sleep lesson*[Title/Abstract]) OR Sleep hygiene lesson*[Title/Abstract]) OR Sleep component*[Title/Abstract]) OR Sleep hygiene component*[Title/Abstract]) OR Sleep part*[Title/Abstract]) OR Sleep hygiene part*[Title/Abstract]) OR Sleep education program*[Title/Abstract]) OR Sleep education campaign*[Title/Abstract]) OR Sleep education cours*[Title/Abstract]) OR Sleep behavior* program*[Title/Abstract]) OR Sleep behaviour* program*[Title/Abstract]) OR Sleep hygiene education[Title/Abstract]) OR Sleep hygiene education program*[Title/Abstract]) OR Sleep hygiene education relaxation training[Title/Abstract]) OR Sleep hygiene education cognitive therapy[Title/Abstract])) AND ((((((((((intervention[Title/Abstract]) OR program*[Title/Abstract]) OR Impact*[Title/Abstract]) OR Prevent*[Title/Abstract]) OR Experiment*[Title/Abstract]) OR Train*[Title/Abstract]) OR Course[Title/Abstract]) OR Campaign[Title/Abstract]) OR Promot*[Title/Abstract]) OR Educat*[Title/Abstract])) AND (((((((((((sleep*[Title/Abstract]) OR sleep deprivation[MeSH Terms]) OR sleep hygiene[MeSH Terms]) OR sleep latency[MeSH Terms]) OR sleep onset[Title/Abstract]) OR time in bed[Title/Abstract]) OR Night rest[Title/Abstract]) OR Bed time[Title/Abstract]) OR Bedtime[Title/Abstract]) OR Sleep time[Title/Abstract]) OR nap*[Title/Abstract])) AND (((((((((program evaluation[MeSH Terms]) OR evaluat*[Title/Abstract]) OR Assess*[Title/Abstract]) OR Influence*[Title/Abstract]) OR Effect*[Title/Abstract]) OR Test*[Title/Abstract]) OR Improv*[Title/Abstract]) OR Trial[Title/Abstract]) OR control[Title/Abstract]).
References
- Buysse, D.J. Sleep health: Can we define it? Does it matter? Sleep 2014, 37, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Cappuccio, F.P.; Taggart, F.M.; Kandala, N.B.; Currie, A.; Peile, E.; Stranges, S.; Miller, M.A. Meta-analysis of short sleep duration and obesity in children and adults. Sleep 2008, 31, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Cappuccio, F.P.; Cooper, D.; D’ Elia, L.; Strazzullo, P.; Miller, M.A. Sleep duration predicts cardiovascular outcomes: A systematic review and meta-analysis of prospective studies. Eur. Heart J. 2011, 32, 1484–1492. [Google Scholar] [CrossRef] [PubMed]
- Cappuccio, F.P.; D’Elia, L.; Strazzullo, P.; Miller, M.A. Quantity and quality of sleep and incidence of type 2 diabetes: A systematic review and meta-analysis. Diabetes Care 2010, 33, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Wu, C.; Gan, Y.; Qu, X.; Lu, Z. Insomnia and the risk of depression: A meta-analysis of prospective cohort studies. BMC Psychiatry 2016, 16, 375. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, A.N.; Walker, M.P. The role of sleep in emotional brain function. Annu. Rev. Clin. Psychol. 2014, 10, 679–708. [Google Scholar] [CrossRef]
- Lo, J.; Groeger, J.A.; Cheng, G.H.; Dijk, D.J.; Chee, M. Self-reported sleep duration and cognitive performance in older adults: A systematic review and meta-analysis. Sleep Med. 2016, 17, 87–98. [Google Scholar] [CrossRef]
- Nazari, H.; Moradi, A.; Rahmani, K. A systematic review of the effect of various interventions on reducing fatigue and sleepiness while driving. Chin. J. Traumatol. Zhonghua Chuang Shang Za Zhi 2017, 20, 249–258. [Google Scholar] [CrossRef]
- Ramadan, M.; Al-saleh, K. The association of sleep deprivation on the occurrence of errors by nurses who work the night shift. Curr. Health Sci. J. 2014, 40, 97–103. [Google Scholar] [CrossRef]
- Stranges, S.; Tigbe, W.; Gómez, F.; Thorogood, M.; Kandala, N. Sleep problems: An emerging global epidemic? Findings from the INDEPTH WHO-SAGE study among more than 40,000 older adults from 8 countries across Africa and Asia. Sleep 2012, 35, 1173–1181. [Google Scholar] [CrossRef]
- Grunstein, R.R. Global perspectives on sleep and health issues. J. Natl. Inst. Public Health 2012, 61, 35–42. [Google Scholar]
- Ohayon, M.M. Epidemiological overview of sleep disorders in the general population. Sleep Med. Res. 2011, 2, 1–9. [Google Scholar] [CrossRef]
- Chattu, V.K.; Manzar, M.D.; Kumary, S.; Burman, D.; Spence, D.W.; Pandi-Perumal, S.R. The global problem of insufficient sleep and its serious public health implications. Healthcare 2018, 7, 1. [Google Scholar] [CrossRef]
- Hafner, M.; Stepanek, M.; Taylor, J.; Troxel, W.M.; van Stolk, C. Why sleep matters—The economic costs of insufficient sleep: A cross-country comparative analysis. Rand Health Q. 2017, 6, 11. [Google Scholar]
- Altevogt, B.M.; Colten, H. (Eds.) Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem; National Academies Press: Washington, DC, USA, 2006; pp. 178–180. [Google Scholar] [CrossRef]
- Hale, L.; Troxel, W.; Buysse, D.J. Sleep health: An opportunity for public health to address health equity. Annu. Rev. Public Health 2020, 41, 81–99. [Google Scholar] [CrossRef]
- Luyster, F.S.; Strollo, P.J.; Zee, P.C.; Walsh, J.K. Sleep: A health imperative. Sleep 2012, 35, 727–734. [Google Scholar] [CrossRef]
- 2020 Topics and Objectives—Objectives A–Z|Healthy People 2020. Available online: https://www.healthypeople.gov/2020/topics-objectives/topic/sleep-health/objectives (accessed on 20 November 2020).
- Royal Society for Public Health. Waking up to the Health Benefits of Sleep. Available online: https://www.rsph.org.uk/resourceLibrary/waking-up-to-the-health-benefits-of-sleep.html (accessed on 20 November 2020).
- Sorscher, A.J. How is your sleep: A neglected topic for health care screening. J. Am. Board Fam. Med. JABFM 2008, 21, 141–148. [Google Scholar] [CrossRef]
- Siengsukon, C.F.; Al-dughmi, M.; Stevens, S. Sleep health promotion: Practical information for physical therapists. Phys. Ther. 2017, 97, 826–836. [Google Scholar] [CrossRef]
- Kline, C. Sleep Duration. In Encyclopedia of Behavioral Medicine; Gellman, M.D., Turner, J.R., Eds.; Springer: New York, NY, USA, 2013; pp. 1808–1810. Available online: https://link.springer.com/referenceworkentry/10.1007%2F978-1-4419-1005-9_846 (accessed on 20 November 2020).
- Kline, C. Sleep Quality. In Encyclopedia of Behavioral Medicine; Gellman, M.D., Turner, J.R., Eds.; Springer: New York, NY, USA, 2013; pp. 1811–1813. Available online: https://link.springer.com/referenceworkentry/10.1007%2F978-1-4419-1005-9_849 (accessed on 20 November 2020).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Chiang, I.; Jhangiani, R.; Price, P. Quasi-Experimental Research. In Research Methods in Psychology, 2nd ed.; BCcampus; University of Minnesota Libraries Publishing Edition: Minneapolis, MN, USA, 2015; Volume 135, Available online: https://opentextbc.ca/researchmethods/chapter/quasi-experimental-research (accessed on 20 November 2020).
- Aromataris, E.; Fernandez, R.; Godfrey, C.M.; Holly, C.; Khalil, H.; Tungpunkom, P. Summarizing systematic reviews: Methodological development, conduct and reporting of an umbrella review approach. Int. J. Evid. Based Healthc. 2015, 13, 132–140. [Google Scholar] [CrossRef]
- Cooper, H.; Koenka, A.C. The overview of reviews: Unique challenges and opportunities when research syntheses are the principal elements of new integrative scholarship. Am. Psychol. 2012, 67, 446. [Google Scholar] [CrossRef]
- Pieper, D.; Antoine, S.; Mathes, T.; Neugebauer, E.; Eikermann, M. Systematic review finds overlapping reviews were not mentioned in every other overview. J. Clin. Epidemiol. 2014, 67, 368–375. [Google Scholar] [CrossRef]
- Bryanton, J.; Beck, C.; Montelpare, W. Postnatal parental education for optimizing infant general health and parent-infant relationships. Cochrane Database Syst. Rev. 2013, 28, Cd004068. [Google Scholar] [CrossRef]
- Dietrich, K.; Francis, M.; Knibbs, D.; Umali, L.; Truglio, M. Effectiveness of sleep education programs to improve sleep hygiene and/or sleep quality in college students: A systematic review. JBI Database Syst. Rev. Implement. Rep. 2016, 14, 108–134. [Google Scholar] [CrossRef] [PubMed]
- Neuendorf, R.; Wahbeh, H.; Chamine, I.; Yu, J.; Hutchison, K.; Oken, S. The effects of mind-body interventions on sleep quality: A systematic review. Evid.-Based Complement. Altern. Med. ECAM 2015, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Crichton, G.; Symon, B. Behavioral management of sleep problems in infants under 6 months—What works? J. Dev. Behav. Pediatr. 2016, 37, 164–171. [Google Scholar] [CrossRef]
- Kempler, L.; Sharpe, L.; Miller, C.; Bartlett, D. Do psychosocial sleep interventions improve infant sleep or maternal mood in the postnatal period? A systematic review and meta-analysis of randomised controlled trials. Sleep Med. Rev. 2016, 29, 15–22. [Google Scholar] [CrossRef]
- Mindell, A.; Kuhn, B.; Lewin, S.; Meltzer, L.; Sadeh, A. Behavioral treatment of bedtime problems and night wakings in infants and young children. Sleep 2006, 29, 1263–1276. [Google Scholar] [CrossRef]
- Arora, T.; Taheri, S. Is sleep education an effective tool for sleep improvement and minimizing metabolic disturbance and obesity in adolescents? Sleep Med. Rev. 2017, 36, 3–12. [Google Scholar] [CrossRef]
- Aslund, L.; Arnberg, F.; Kanstrup, M.; Lekander, M. Cognitive and behavioral interventions to improve sleep in school-age children and adolescents: A systematic review and meta-analysis. J. Clin. Sleep Med. 2018, 14, 1937–1947. [Google Scholar] [CrossRef]
- Blunden, S.; Chapman, J.; Rigney, G. Are sleep education programs successful? The case for improved and consistent research efforts. Sleep Med. Rev. 2012, 16, 355–370. [Google Scholar] [CrossRef]
- Busch, V.; Altenburg, M.; Harmsen, A.; Chinapaw, J. Interventions that stimulate healthy sleep in school-aged children: A systematic literature review. Eur. J. Public Health 2017, 27, 53–65. [Google Scholar] [CrossRef]
- Chung, F.; Chan, S.; Lam, Y.; Lai, S.; Yeung, F. School-based sleep education programs for short sleep duration in adolescents: A systematic review and meta-analysis. J. Sch. Health 2017, 87, 401–408. [Google Scholar] [CrossRef]
- Meltzer, J.; Mindell, A. Systematic review and meta-analysis of behavioral interventions for pediatric insomnia. J. Pediatr. Psychol. 2014, 39, 932–948. [Google Scholar] [CrossRef]
- Barger, L.K.; Runyon, M.S.; Renn, M.L.; Moore, C.G.; Weiss, P.M.; Condle, J.P.; Flickinger, K.L.; Divecha, A.A.; Coppler, P.J.; Sequeira, D.J.; et al. Effect of fatigue training on safety, fatigue, and sleep in emergency medical services personnel and other shift workers: A systematic review and meta-analysis. Prehosp. Emerg. Care 2018, 22, 58–68. [Google Scholar] [CrossRef]
- Bonnar, D.; Bartel, K.; Kakoschke, N.; Lang, C. Sleep interventions designed to improve athletic performance and recovery: A systematic review of current approaches. Sports Med. 2018, 48, 683–703. [Google Scholar] [CrossRef]
- Chung, F.; Lee, T.; Yeung, F.; Chan, S.; Chung, Y.; Lin, L. Sleep hygiene education as a treatment of insomnia: A systematic review and meta-analysis. Fam. Pract. 2018, 35, 365–375. [Google Scholar] [CrossRef]
- Friedrich, A.; Schlarb, A. Let’s talk about sleep: A systematic review of psychological interventions to improve sleep in college students. J. Sleep Res. 2018, 27, 4–22. [Google Scholar] [CrossRef]
- Murawski, B.; Wade, L.; Plotnikoff, C.; Lubans, R.; Duncan, J. A systematic review and meta-analysis of cognitive and behavioral interventions to improve sleep health in adults without sleep disorders. Sleep Med. Rev. 2018, 40, 160–169. [Google Scholar] [CrossRef]
- Owais, S.; Chow, T.; Furtado, M.; Frey, N.; Van, J. Non-pharmacological interventions for improving postpartum maternal sleep: A systematic review and meta-analysis. Sleep Med. Rev. 2018, 41, 87–100. [Google Scholar] [CrossRef]
- Halal, E.; Nunes, L. Education in children’s sleep hygiene: Which approaches are effective? A systematic review. J. Pediatr. 2014, 90, 449–456. [Google Scholar] [CrossRef] [PubMed]
- Tamrat, R.; Goyal, M.; Huynh, M. Non-pharmacologic interventions to improve the sleep of hospitalized patients: A systematic review. J. Gen. Intern. Med. 2014, 29, 788–795. [Google Scholar] [CrossRef] [PubMed]
- Slanger, T.E.; Gross, J.V.; Pinger, A.; Morfeld, P.; Bellinger, M.; Duhme, A.L.; Reichardt Ortega, R.A.; Costa, G.; Driscoll, T.R.; Foster, R.G.; et al. Person-directed, non-pharmacological interventions for sleepiness at work and sleep disturbances caused by shift work. Cochrane Database Syst. Rev. 2016, CD010641. [Google Scholar] [CrossRef]
- Hellström, A.; Willman, A. Promoting sleep by nursing interventions in health care settings: A systematic review. Worldviews Evid. Based Nurs. 2011, 8, 128–142. [Google Scholar] [CrossRef] [PubMed]
- Hollenbach, D.; Broker, R.; Herlehy, S.; Stuber, K. Non-pharmacological interventions for sleep quality and insomnia during pregnancy: A systematic review. J. Can. Chiropr. Assoc. 2013, 57, 260–270. [Google Scholar] [PubMed]
- de Niet, G.; Tiemens, B.; Lendemeijer, B.; Hutschemaekers, G. Music-assisted relaxation to improve sleep quality: Meta-analysis. J. Adv. Nurs. 2009, 65, 1356–1364. [Google Scholar] [CrossRef] [PubMed]
- Rubio, Á.; Marín, E.; Ramos, J.; Hernandez, V.; Pérez, R. Effect of exercise on sleep quality and insomnia in middle-aged women: A systematic review and meta-analysis of randomized controlled trials. Maturitas 2017, 100, 49–56. [Google Scholar] [CrossRef]
- Du, S.; Dong, J.; Zhang, H.; Jin, S.; Xu, G.; Liu, Z.; Chen, L.; Yin, H.; Sun, Z. Taichi exercise for self-rated sleep quality in older people: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2015, 52, 368–379. [Google Scholar] [CrossRef]
- Yang, Y.; Ho, H.; Chien, Y.; Chen, C. Exercise training improves sleep quality in middle-aged and older adults with sleep problems: A systematic review. J. Physiother. 2012, 58, 157–163. [Google Scholar] [CrossRef]
- Koch, S.; Haesler, E.; Tiziani, A.; Wilson, J. Effectiveness of sleep management strategies for residents of aged care facilities: Findings of a systematic review. J. Clin. Nurs. 2006, 15, 1267–1275. [Google Scholar] [CrossRef]
- Wu, W.; Kwong, E.; Lan, Y.; Jiang, Y. The effect of a meditative movement intervention on quality of sleep in the elderly: A systematic review and meta-analysis. J. Altern. Complement. Med. 2015, 21, 509–519. [Google Scholar] [CrossRef]
- Hwang, E.; Shin, S. The effects of aromatherapy on sleep improvement: A systematic literature review and meta-analysis. J. Altern. Complement. Med. 2015, 21, 61–68. [Google Scholar] [CrossRef]
- Morgenthaler, I.; Hashmi, S.; Croft, B.; Dort, L.; Heald, L.; Mullington, J. High school start times and the impact on high school students: What we know, and what we hope to learn. J. Clin. Sleep Med. 2016, 12, 1681–1689. [Google Scholar] [CrossRef]
- Minges, E.; Redeker, S. Delayed school start times and adolescent sleep: A systematic review of the experimental evidence. Sleep Med. Rev. 2016, 28, 86–95. [Google Scholar] [CrossRef]
- Marx, R.; Tanner, E.; Davison, C.; Ufholz, L.A.; Freeman, J.; Shankar, R.; Newton, L.; Brown, R.; Parpia, A.; Cozma, I.; et al. Later school start times for supporting the education, health, and well-being of high school students. Cochrane Database Syst. Rev. 2017, 7, CD009467. [Google Scholar] [CrossRef]
- Mihelic, M.; Morawska, A.; Filus, A. Effects of early parenting interventions on parents and infants: A meta-analytic review. J. Child Fam. Stud. 2017, 26, 1507–1526. [Google Scholar] [CrossRef]
- Knowlden, P.; Hackman, L.; Sharma, M. Systematic review of dietary interventions targeting sleep behavior. J. Altern. Complement. Med. 2016, 22, 349–362. [Google Scholar] [CrossRef]
- Louzada, F.M.; Silva, A.G.; Peixoto, C.A.; Menna-Barreto, L. The adolescence sleep phase delay: Causes, consequences and possible interventions. Sleep Sci. 2008, 1, 49–53. [Google Scholar]
- American Academy of Pediatrics. School start times for adolescents. Pediatrics 2014, 134, 642–649. [Google Scholar] [CrossRef]
- Hofmann, S.G.; Asnaani, A.; Vonk, I.J.; Sawyer, A.T.; Fang, A. The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognit. Ther. Res. 2012, 36, 427–440. [Google Scholar] [CrossRef]
- Mitchell, M.D.; Gehrman, P.; Perlis, M.; Umscheid, C.A. Comparative effectiveness of cognitive behavioral therapy for insomnia: A systematic review. BMC Fam. Pract. 2012, 13, 40. [Google Scholar] [CrossRef] [PubMed]
- Barnes, C.M.; Drake, C.L. Prioritizing sleep health: Public health policy recommendations. Perspect. Psychol. Sci. 2015, 10, 733–737. [Google Scholar] [CrossRef] [PubMed]
- Lubas, M.; Szklo, M. A critical review of education-based sleep interventions for undergraduate students: Informing future directions in intervention development. Adolesc. Res. Rev. 2019, 4, 249–266. [Google Scholar] [CrossRef]
- Gruber, R. School-based sleep education programs: A knowledge-to-action perspective regarding barriers, proposed solutions, and future directions. Sleep Med. Rev. 2017, 36, 13–28. [Google Scholar] [CrossRef]
- Belmon, L.S.; Stralen, M.M.; Busch, V.; Harmsen, I.A.; Chinapaw, M.J. What are the determinants of children’s sleep behavior? A systematic review of longitudinal studies. Sleep Med. Rev. 2019, 43, 60–70. [Google Scholar] [CrossRef]
- Johnson, D.A.; Billings, M.E.; Hale, L. Environmental determinants of insufficient sleep and sleep disorders: Implications for population health. Curr. Epidemiol. Rep. 2018, 5, 61–69. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).