Environmental and Air Pollution Factors Affecting Allergic Eye Disease in Children and Adolescents in India
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Period, Location, and Approval
2.2. Cases
2.3. Data Retrieval and Processing
2.4. Statistical Analysis
3. Results
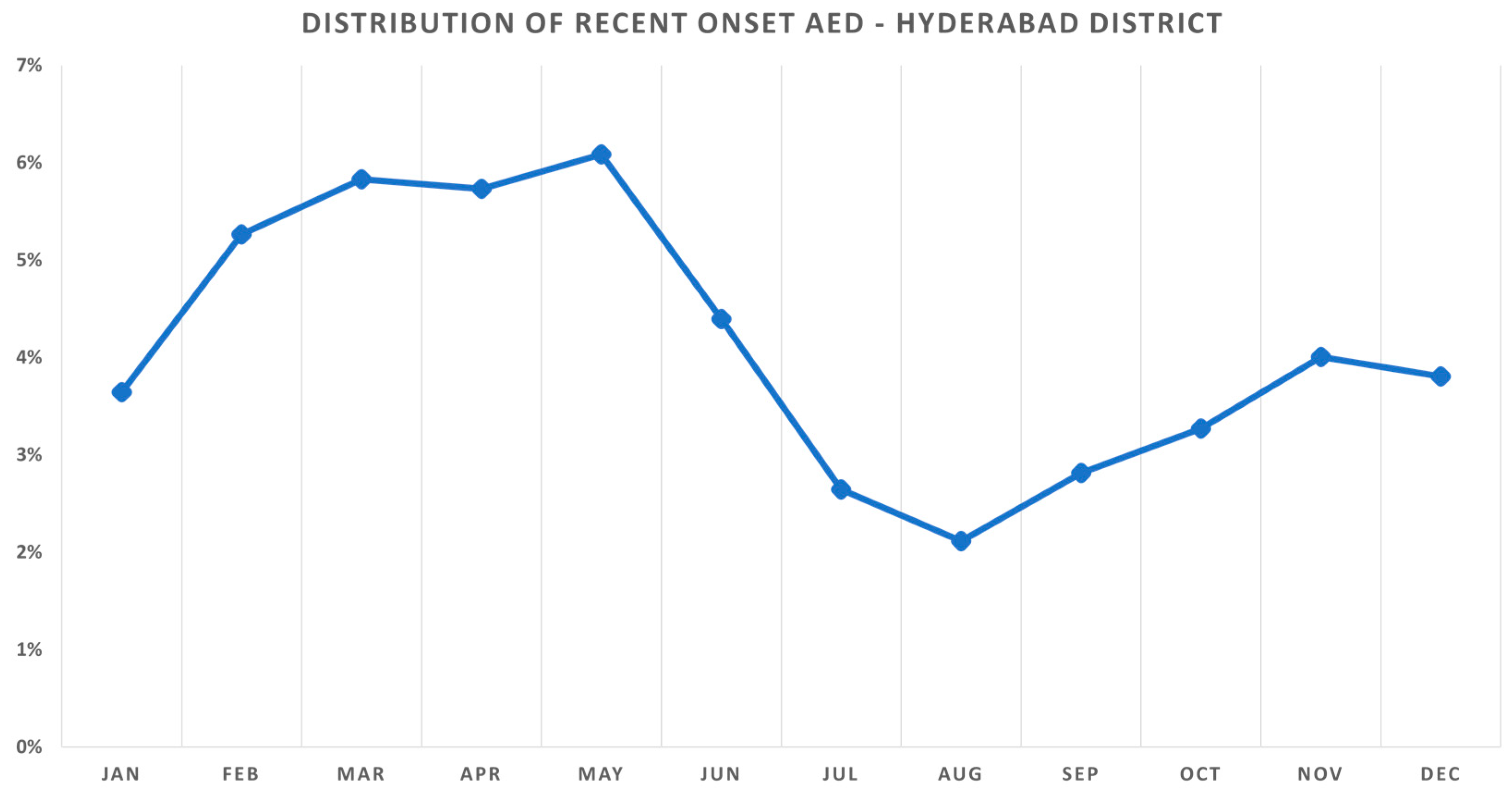
3.1. Demographics
3.2. Humidity
3.3. Rainfall
3.4. Temperature
3.5. Windspeed
3.6. Particulate Matter 10 (PM10)
3.7. Particulate Matter 2.5 (PM2.5)
3.8. Ozone (O3)
3.9. Carbon Monoxide (CO)
3.10. Nitrogen Dioxide (NO2)
3.11. Sulfur Dioxide (SO2)
3.12. Multivariate Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Available online: https://www.who.int/news-room/detail/02-05-2018-9-out-of-10-people-worldwide-breathe-polluted-air-but-more-countries-are-taking-action (accessed on 2 May 2020).
- Available online: https://www.who.int/airpollution/ambient/health-impacts/en/ (accessed on 2 May 2020).
- Chang, C.J.; Yang, H.H.; Chang, C.A.; Tsai, H.Y. Relationship between air pollution and outpatient visits for nonspecific conjunctivitis. Invest Ophthalmol. Vis. Sci. 2012, 53, 429–433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miyazaki, D.; Fukagawa, K.; Fukushima, A.; Fujishima, H.; Uchio, E.; Ebihara, N.; Shoji, J.; Takamura, E.; Namba, K.; Ohashi, Y.; et al. Air pollution significantly associated with severe ocular allergic inflammatory diseases. Sci Rep. 2019, 9, 18205. [Google Scholar] [CrossRef] [Green Version]
- Dermer, H.; Galor, A.; Hackam, A.S.; Mirsaeidi, M.; Kumar, N. Impact of seasonal variation in meteorological conditions on dry eye severity. Clin. Ophthalmol. 2018, 12, 2471–2481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saxena, R.; Srivastava, S.; Trivedi, D.; Anand, E.; Joshi, S.; Gupta, S.K. Impact of environmental pollution on the eye. Acta Ophthalmol. Scand. 2003, 81, 491–494. [Google Scholar] [CrossRef] [PubMed]
- Das, A.V.; Donthineni, P.R.; Prashanthi, G.S.; Basu, S. Allergic eye disease in children and adolescents seeking eye care in India: Electronic medical records driven big data analytics report II. Ocul. Surf. 2019, 17, 683–689. [Google Scholar] [CrossRef] [PubMed]
- Rao, G.N.; Khanna, R.C.; Athota, S.M.; Rajshekar, V.; Rani, P.K. Integrated model of primary and secondary eye care for underserved rural areas: The L V Prasad Eye Institute experience. Indian J. Ophthalmol. 2012, 60, 396–400. [Google Scholar] [CrossRef] [PubMed]
- Das, A.V.; Kammari, P.; Vadapalli, R.; Basu, S. Big data and the eyeSmart electronic medical record system - An 8-year experience from a three-tier eye care network in India. Indian J. Ophthalmol. 2020, 68, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Telangana State Development Planning Society. Available online: https://tsdps.telangana.gov.in/ (accessed on 2 April 2020).
- Available online: https://app.cpcbccr.com/ccr/#/caaqm-dashboard-all/caaqm-landing/data (accessed on 2 April 2020).
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.; Zhong, T.; Li, H.; Xu, J.; Ye, X.; Mu, Z.; Lu, Y.; Mashaghi, A.; Zhou, Y.; Tan, M.; et al. Ambient air pollution, weather changes, and outpatient visits for allergic conjunctivitis: A retrospective registry study. Sci Rep. 2016, 1, 23858. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sugiyama, T.; Ueda, K.; Seposo, X.T.; Nakashima, A.; Kinoshita, M.; Matsumoto, H.; Ikemori, F.; Honda, A.; Takano, H.; Michikawa, T.; et al. Health effects of PM2.5 sources on children’s allergic and respiratory symptoms in Fukuoka, Japan. Sci. Total Environ. 2020, 709, 136023. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.J.; Chang, H.H.; Chiang, C.Y.; Lai, C.Y.; Hsu, M.Y.; Wang, K.R.; Han, H.H.; Chen, L.Y.; Lin, D.P.C. A Murine Model of Acute Allergic Conjunctivitis Induced by Continuous Exposure to Particulate Matter 2.5. Invest Ophthalmol. Vis. Sci. 2019, 60, 2118–2126. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Kim, E.K.; Kim, H.Y.; Kim, T.I. Effects of Exposure to Ozone on the Ocular Surface in an Experimental Model of Allergic Conjunctivitis. PLoS ONE 2017, 12, e0169209. [Google Scholar]
- Das, A.V.; Basu, S. Epidemic Keratoconjunctivitis in India: Trend Analysis and Implications for Viral Outbreaks. Indian J. Ophthalmol. 2020, 68, 732–736. [Google Scholar] [PubMed]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Das, A.V.; Basu, S. Environmental and Air Pollution Factors Affecting Allergic Eye Disease in Children and Adolescents in India. Int. J. Environ. Res. Public Health 2021, 18, 5611. https://doi.org/10.3390/ijerph18115611
Das AV, Basu S. Environmental and Air Pollution Factors Affecting Allergic Eye Disease in Children and Adolescents in India. International Journal of Environmental Research and Public Health. 2021; 18(11):5611. https://doi.org/10.3390/ijerph18115611
Chicago/Turabian StyleDas, Anthony Vipin, and Sayan Basu. 2021. "Environmental and Air Pollution Factors Affecting Allergic Eye Disease in Children and Adolescents in India" International Journal of Environmental Research and Public Health 18, no. 11: 5611. https://doi.org/10.3390/ijerph18115611
APA StyleDas, A. V., & Basu, S. (2021). Environmental and Air Pollution Factors Affecting Allergic Eye Disease in Children and Adolescents in India. International Journal of Environmental Research and Public Health, 18(11), 5611. https://doi.org/10.3390/ijerph18115611






