Using the Water and Sanitation for Health Facility Improvement Tool (WASH FIT) in Zimbabwe: A Cross-Sectional Study of Water, Sanitation and Hygiene Services in 50 COVID-19 Isolation Facilities
Abstract
1. Introduction
2. Materials and Methods
2.1. WASH FIT Assessment
2.2. Data Collection
2.3. Data Analysis
3. Ethical Review
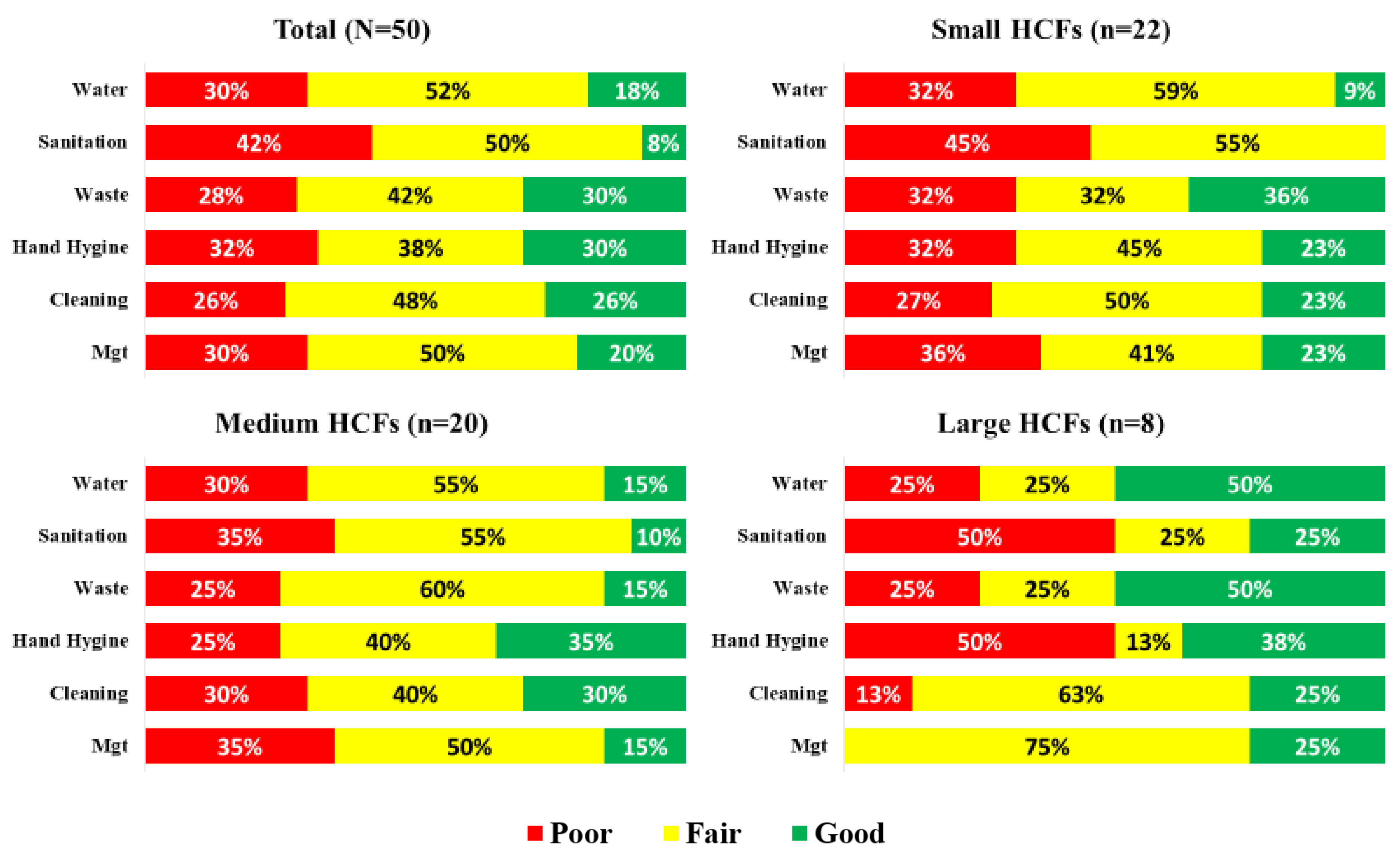
4. Results
4.1. Water Domain
4.2. Sanitation Domain
4.3. Health Care Waste Domain
4.4. Hand Hygiene Domain
4.5. Facility Environment, Cleanliness and Disinfection Domain
4.6. Management Domain
4.7. WASH FIT Summary Measures
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Essential Environmental Health Standards in Health Care; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- WHO. WHO Guidelines on Hand Hygiene in Health Care. In First Global Patient Safety Challenge: Clean Care Is Safer Care; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Cronk, R.; Bartram, J. Environmental conditions in health care facilities in low-and middle-income countries: Coverage and inequalities. Int. J. Hyg. Environ. Health 2018, 221, 409–422. [Google Scholar] [CrossRef] [PubMed]
- WHO; UNICEF. Global Progress Report On Water, Sanitation and Hygiene in Health Care Facilities: Fundamentals First; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Bouzid, M.; Cumming, O.; Hunter, P.R. What is the impact of water sanitation and hygiene in healthcare facilities on care seeking behaviour and patient satisfaction? A systematic review of the evidence from low-income and middle-income countries. BMJ Glob. Health 2018, 3, e000648. [Google Scholar] [CrossRef] [PubMed]
- Pessoa-Silva, C.L.; Dharan, S.; Hugonnet, S.; Touveneau, S.; Posfay-Barbe, K.; Pfister, R.; Pittet, D. Dynamics of bacterial hand contamination during routine neonatal care. Infect. Control. Hosp. Epidemiol. 2004, 25, 192–197. [Google Scholar] [CrossRef] [PubMed]
- Kuti, B.P.; Ogunlesi, T.A.; Oduwole, O.; Oringanje, C.; Udoh, E.E.; Meremikwu, M.M. Hand hygiene for the prevention of infections in neonates. Cochrane Database Syst. Rev. 2019, 2019, CD013326. [Google Scholar] [CrossRef]
- Trampuz, A.; Widmer, A.F. Hand hygiene: A frequently missed lifesaving opportunity during patient care. Mayo Clin. Proc. 2004, 79, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Allegranzi, B.; Bagheri Nejad, S.; Combescure, C.; Graafmans, W.; Attar, H.; Donaldson, L.; Pittet, D. Burden of endemic health-care-associated infection in developing countries: Systematic review and meta-analysis. Lancet 2011, 377, 228–241. [Google Scholar] [CrossRef]
- WHO. Report on the Burden of Endemic Health Care-Associated Infection Worldwide; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Watson, J.; D’Mello-Guyett, L.; Flynn, E.; Falconer, J.; Esteves-Mills, J.; Prual, A.; Hunter, P.; Allegranzi, B.; Montgomery, M.; Cumming, O. Interventions to improve water supply and quality, sanitation and handwashing facilities in healthcare facilities, and their effect on healthcare-associated infections in low-income and middle-income countries: A systematic review and supplementary scoping review. BMJ Global Health 2019, 4, e001632. [Google Scholar]
- Kohler, P.; Renggli, S.; Lüthi, C. WASH and gender in health care facilities: The uncharted territory. Health Care Women Int. 2017, 8, 1–10. [Google Scholar] [CrossRef]
- Graham, W.J.; Morrison, E.; Dancer, S.; Afsana, K.; Aulakh, A.; Campbell, O.M.; Cross, S.; Ellis, R.; Enkubahiri, S.; Fekad, B.; et al. What are the threats from antimicrobial resistance for maternity units in low- and middle-income countries? Glob. Health Action 2016, 9, 33381. [Google Scholar] [CrossRef] [PubMed]
- WHA Resolution EB144.R5, May 2019. Available online: https://apps.who.int/gb/ebwha/pdf_files/EB144/B144_R5-en.pdf (accessed on 23 May 2021).
- WHO; UNICEF. WASH in Health Care Facilities: From Resolution to Revolution; 2019. Available online: https://www.washinhcf.org/wp-content/uploads/2019/10/Resolution-to-Revolution_Meeting-Report_Zambia2019_final.pdf (accessed on 1 February 2021).
- Hirai, M.; Nyamandi, V.; Kanyowa, T.; Barak, J.; Overmars, M.; Ngwakum, P.; Cronin, A. Water, Sanitation and Hygiene in Health Care Facilities in Zimbabwe: An Overview; United Nations Children’s Fund: New York, NY, USA, 2020. [Google Scholar]
- McGriff, J.A.; Denny, L. What COVID-19 reveals about the neglect of WASH within infection prevention in low-resource healthcare facilities. ASTMH 2020, 103, 1762–1764. [Google Scholar] [CrossRef] [PubMed]
- Johns Hopkins University and Medicine. COVID-19 Dashboard; 2021. Available online: https://coronavirus.jhu.edu/map.html (accessed on 23 May 2021).
- Ministry of Health and Child Care (MoHCC). Zimbabwe COVID-19 SitRep 22/05/2021; MoHCC: Harare, Zimbabwe, 2021.
- Ashinyo, M.E.; Amegah, K.E.; Dubik, S.D.; Ntow-Kummi, G.; Adjei, M.K.; Amponsah, J.; Ayivase, J.T.; Amoah, S.; Ashinyo, A.; Sodzi-Tettey, S. Evaluation of water, sanitation and hygiene status of COVID-19 healthcare facilities in Ghana using the WASH FIT approach. J. Water Sanit. Hyg. Dev. 2021, in press. [Google Scholar] [CrossRef]
- WHO; UNICEF. Water and Sanitation for Health Facility Improvement Tool ‘WASH FIT’: A Practical Guide for Improving QoC through Water, Sanitation, and Hygiene in Healthcare Facilities. 2018. Available online: http://www.who.int/water_sanitation_health/publications/water-and-sanitation-for-health-facility-improvement-tool/en/ (accessed on 17 January 2021).
- StataCorp. Stata Statistical Software: Release 14; StataCorp LP: College Station, TX, USA, 2015. [Google Scholar]
- The National Task Force on Cholera Elimination. Zimbabwe Multi-Sectoral Cholera Elimination Plan 2018–2028; MoHCC: Harare, Zimbabwe, 2020.
- The Government of Zimbabwe (GoZ). National Development Strategy 1 January 2021–December 2025; GoZ: Harare, Zimbabwe, 2020.
- Patel, K.; Kalpana, P.; Trivedi, P.; Yasobant, S.; Saxena, D. Assessment of Water, Sanitation and Hygiene in HCFs: Which Tool to Follow? Rev. Environ. Health 2019, 34, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Weber, N.; Martinsen, A.L.; Sani, A.; Elom Kokou Assigbley, E.; Azzouz, C.; Hayter, A.; Ayite, K.; Amivi Afefa Bibiane, B.; Kokou Mawule, D.; Gelting, R. Strengthening health care facilities through Water, Sanitation and Hygiene (WASH) improvements: A pilot evaluation of ‘WASH FIT’ in Togo. Health Secur. 2018, 16, S54–S65. [Google Scholar] [CrossRef] [PubMed]
- Maina, M.; Tosas-Auguet, O.; McKnight, J.; Zosi, M.; Kimemia, G.; Mwaniki, P.; Hayter, A.; Montgomery, M.; Schultsz, C. Extending the use of the World Health Organisations’ water sanitation and hygiene assessment tool for surveys in hospitals—From WASH-FIT to WASH-FAST. PLoS ONE 2019, 14, e0226548. [Google Scholar] [CrossRef] [PubMed]
- Weber, N.; Patrick, M.; Hayter, A.; Martinsen, A.L.; Gelting, R. A conceptual evaluation framework for the water and sanitation for health facility improvement tool (WASH FIT). J. Water Sanit. Hyg. Dev. 2019, 9, 380–391. [Google Scholar] [CrossRef]
- WHO; UNICEF. What is WASH FIT? WHO: Geneva, Switzerland, 2020; Available online: https://www.washinhcf.org/wp-content/uploads/2020/12/What-is-WASH-FIT.pdf (accessed on 30 March 2021).

| Variables | n (%) |
|---|---|
| Province | |
| Bulawayo | 3 (6) |
| Manicaland | 5 (10) |
| Mashonaland Central | 5 (10) |
| Mashonaland East | 3 (6) |
| Masvingo | 9 (18) |
| Matabeleland North | 8 (16) |
| Matabeleland South | 7 (14) |
| Midlands | 10 (20) |
| Hospital size | |
| Small (<100 beds) | 22 (44) |
| Medium (100–199 beds) | 20 (40) |
| Large (200 beds or more) | 8 (16) |
| HCF type | |
| Public hospital | 40 (80) |
| Private hospital | 3 (6) |
| Public health center/post | 5 (10) |
| Private health center/post | 2 (4) |
| Type of Water Source | |
| Public taps/standpipe | 23 (46) |
| Hand pumps/boreholes | 14 (28) |
| Piped connection | 11 (22) |
| Surface water | 1 (2) |
| Other | 1 (2) |
| Type of Sanitation Facility | |
| Flush toilet | 43 (86) |
| Pit latrine with a slab | 5 (10) |
| Ventilated improved pit | 1 (2) |
| Pit latrine without a slab | 1 (2) |
| mean (std) | |
| Daily inpatients | 37.0 (51.3) |
| Daily outpatients | 67.9 (67.9) |
| Number of beds | 138.7 (164.2) |
| WASHFIT Essential Indicators | Total | Small | Medium | Large | Ratings |
|---|---|---|---|---|---|
| Water | |||||
| Improved water supply piped into the facility or on premises and available | 1.44 | 1.23 | 1.60 | 1.63 | Fair |
| Water services available at all times and of sufficient quantity for all uses | 0.94 | 0.91 | 0.85 | 1.25 | Poor |
| A reliable drinking water station is present and accessible for staff, patients and care takers at all times and in all locations/wards | 1.12 | 1.00 | 1.05 | 1.63 | Fair |
| Drinking water is safely stored in a clean bucket/tank with cover and tap | 1.36 | 1.23 | 1.35 | 1.75 | Fair |
| Sanitation | |||||
| Number of available and usable toilets or improved latrines for patients | 1.04 | 1.09 | 0.95 | 1.13 | Fair |
| Toilets or improved latrines clearly separated for staff and patients | 1.16 | 1.23 | 1.05 | 1.25 | Fair |
| Toilets or improved latrines clearly separated for male and female | 1.52 | 1.45 | 1.70 | 1.25 | Good |
| At least one toilet or improved latrine provides the means to manage menstrual hygiene needs | 0.56 | 0.68 | 0.45 | 0.50 | Poor |
| At least one toilet meets the needs of people with reduced mobility | 0.34 | 0.18 | 0.50 | 0.38 | Poor |
| Functioning hand hygiene stations within 5 meters of latrines | 1.14 | 1.09 | 1.10 | 1.38 | Fair |
| Health Care Waste | |||||
| A trained person is responsible for the management of health care waste in the health care facility | 1.36 | 1.55 | 1.20 | 1.25 | Fair |
| Functional waste collection containers in close proximity to all waste generation points for: non-infectious (general) waste, infectious waste, and sharps waste | 0.98 | 0.77 | 1.05 | 1.38 | Poor |
| Waste correctly segregated at all waste generation points | 1.04 | 0.95 | 1.05 | 1.25 | Fair |
| Functional burial pit/fenced waste dump or municipal pick-up available for disposal of non-infectious waste | 1.46 | 1.45 | 1.35 | 1.75 | Fair |
| Incinerator or alternative treatment technology for the treatment of infectious and sharp waste is functional and of a sufficient capacity | 1.26 | 1.32 | 1.15 | 1.38 | Fair |
| Sufficient energy available for incineration or alternative treatment technologies | 0.88 | 0.76 | 0.72 | 0.99 | Poor |
| Hand Hygiene | |||||
| Functioning hand hygiene stations are available at all points of care | 1.26 | 1.09 | 1.40 | 1.38 | Fair |
| Hand hygiene promotion materials clearly visible and understandable at key places | 1.22 | 1.09 | 1.40 | 1.13 | Fair |
| Facility Environment, Cleanliness and Disinfection | |||||
| The exterior of the facility is well-fenced, kept generally clean (free from solid waste, stagnant water, no animal and human feces in or around the facility premises) | 1.50 | 1.50 | 1.45 | 1.63 | Good |
| General lighting sufficiently powered and adequate to ensure safe provision of health care including at night | 1.20 | 1.23 | 1.15 | 1.25 | Fair |
| Floors and horizontal work surfaces appear clean | 1.42 | 1.23 | 1.70 | 1.25 | Fair |
| Appropriate and well-maintained materials for cleaning are available | 1.06 | 0.86 | 1.15 | 1.38 | Fair |
| At least two pairs of household cleaning gloves and one pair of overalls or apron and boots in a good state for each cleaning and waste disposal staff member | 0.88 | 0.77 | 1.05 | 0.75 | Poor |
| At least one member of staff can demonstrate the correct procedures for cleaning and disinfection and apply them as required to maintain clean and safe rooms | 1.46 | 1.45 | 1.50 | 1.38 | Fair |
| Beds have insecticide treated nets to protect patients from mosquito-borne diseases | 0.72 | 0.50 | 1.00 | 0.63 | Poor |
| Management | |||||
| WASH FIT or other quality improvement/management plan for the facility is in place, implemented and regularly monitored | 0.94 | 0.86 | 1.05 | 0.88 | Poor |
| An annual planned budget for the facility is available and includes funding for WASH infrastructure, services, personnel and the continuous procurement of WASH items, which is sufficient to meet the needs of the facility | 0.72 | 0.50 | 0.75 | 1.25 | Poor |
| An up-to-date diagram of the facility management structure is clearly visible and legible | 1.30 | 1.05 | 1.45 | 1.63 | Fair |
| Adequate cleaners and WASH maintenance staff are available | 1.14 | 1.14 | 1.15 | 1.13 | Fair |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hirai, M.; Nyamandi, V.; Siachema, C.; Shirihuru, N.; Dhoba, L.; Baggen, A.; Kanyowa, T.; Mwenda, J.; Dodzo, L.; Manangazira, P.; et al. Using the Water and Sanitation for Health Facility Improvement Tool (WASH FIT) in Zimbabwe: A Cross-Sectional Study of Water, Sanitation and Hygiene Services in 50 COVID-19 Isolation Facilities. Int. J. Environ. Res. Public Health 2021, 18, 5641. https://doi.org/10.3390/ijerph18115641
Hirai M, Nyamandi V, Siachema C, Shirihuru N, Dhoba L, Baggen A, Kanyowa T, Mwenda J, Dodzo L, Manangazira P, et al. Using the Water and Sanitation for Health Facility Improvement Tool (WASH FIT) in Zimbabwe: A Cross-Sectional Study of Water, Sanitation and Hygiene Services in 50 COVID-19 Isolation Facilities. International Journal of Environmental Research and Public Health. 2021; 18(11):5641. https://doi.org/10.3390/ijerph18115641
Chicago/Turabian StyleHirai, Mitsuaki, Victor Nyamandi, Charles Siachema, Nesbert Shirihuru, Lovemore Dhoba, Alison Baggen, Trevor Kanyowa, John Mwenda, Lilian Dodzo, Portia Manangazira, and et al. 2021. "Using the Water and Sanitation for Health Facility Improvement Tool (WASH FIT) in Zimbabwe: A Cross-Sectional Study of Water, Sanitation and Hygiene Services in 50 COVID-19 Isolation Facilities" International Journal of Environmental Research and Public Health 18, no. 11: 5641. https://doi.org/10.3390/ijerph18115641
APA StyleHirai, M., Nyamandi, V., Siachema, C., Shirihuru, N., Dhoba, L., Baggen, A., Kanyowa, T., Mwenda, J., Dodzo, L., Manangazira, P., Chirume, M., Overmars, M., Honda, Y., Chouhan, A., Nzara, B., Vavirai, P., Sithole, Z., Ngwakum, P., Chitsungo, S., & Cronin, A. A. (2021). Using the Water and Sanitation for Health Facility Improvement Tool (WASH FIT) in Zimbabwe: A Cross-Sectional Study of Water, Sanitation and Hygiene Services in 50 COVID-19 Isolation Facilities. International Journal of Environmental Research and Public Health, 18(11), 5641. https://doi.org/10.3390/ijerph18115641






