The Identification and Referral to Improve Safety Programme and the Prevention of Intimate Partner Violence
Abstract
1. Introduction
1.1. Background
1.2. Definitions
1.3. Scale of the Problem
- Globally the lifetime prevalence of physical and sexual intimate partner violence and abuse for women is around 30% [14].
- In the United States findings from the 1998 National Violence Against Women Survey showed that 1.5 million women are raped or physically assaulted by an intimate partner annually [15]. In addition, only 36% of the women injured during their most recent rape and 30% of the women injured during their most recent physical assault received some type of medical treatment [15]. Other studies found an incidence of battering from 7% to 44%, depending on the sampled population [15].
- Across Europe, an average of 22% of women report experiencing physical and/or sexual violence and that 43% have experienced psychological abuse from the age of 15 [16]. A total of 58% of women across Europe who did not feel that they had an equal say in household finances experienced psychological abuse compared to 22% of women who believed that they had an equal say [16].
- In the UK, the reported rate of physical and/or sexual violence was 29% and psychological abuse 46% [17]. Out of the reported crimes, 25% of women had reported the most serious incident of intimate partner violence and abuse [17]. However, women are more likely to contact healthcare services about the most serious incident of abuse they had experienced [17].
- In England and Wales between 2019/2020 the crime survery estimates that 2.3 million adults aged 16–74 years experienced domestic abuse [19].
1.4. The Causes of Intimate Partner Violence and Abuse
1.5. Financial Impact of DVA
1.6. Physical Impact of DVA
1.7. Psychological Impact of DVA
1.8. The Role of Healthcare Professionals
1.9. Training Programme for Healthcare Professionals in DVA
1.10. Identification and Referral to Improve Safety (IRIS)—A Training and Support Programme
- The history and background of IRIS.
- Review of available literature associated with IRIS.
- Discussion of randomised controlled trial of IRIS.
- Discussion of IRIS cost-effectiveness in primary care.
- Future of IRIS-Exploring the potential benefit of implementing an adapted IRIS programme into secondary care.
- Recommendation how to adapt the programme for secondary care.
- Suggestions for future research and studies with regards to IRIS.
1.11. The History and Background of IRIS
2. Materials and Methods
- The World Health Organisation for global definition prevalence of IPV
- United Nationas for definitions of different forms of DVA
- Office for National Statistics for domestic abuse in England and Wales
- Crime and criminal justice police reports for domestic abuse in Scotland
- Office of European Union for DVA and IPV statistics and costs
- National Violence Against Women Survery for data within the United States
3. Results
3.1. Randomised Controlled Trial of IRIS
3.2. Discussion of IRIS Cost-Effectiveness
4. Discussion
4.1. Introducing IRIS into Secondary Care
4.2. Why the Fracture Clinic?
4.3. Orthopaedic Presentation of IPV
4.3.1. Proposal—Introducing IRIS into Fracture Clinics
4.3.2. Recommendations—IRIS Pilot Study in Salford Fracture Clinic
4.3.3. The Potential Hurdle and Challenges of Implementing IRIS into Fracture Clinic
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability
Acknowledgments
Conflicts of Interest
References
- World Health Organisation. Global Status Report on Violence Prevention 2014; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- World Health Organization. Dept of Reproductive Health and Research. Intimate Partner Violence during Pregnancy. 2011. Available online: https://apps.who.int/iris/bitstream/handle/10665/70764/WHO_RHR_11.35_eng.pdf?sequence=1 (accessed on 29 May 2019).
- Campbell, J.C. Health consequences of intimate partner violence. Lancet 2002, 359, 1331–1336. [Google Scholar] [CrossRef]
- Walby, S.; Olive, P. Estimating the Costs of Gender-Based Violence in the European Union; Publications Office of the European Union: Luxembourg, 2014. [Google Scholar] [CrossRef]
- Oliver, R.; Alexander, B.; Roe, S.; Wlasny, M. The Economic and Social Costs of Domestic Abuse; Corporate Document Services: Leeds, UK, 2019. [Google Scholar]
- World Health Organization. Global and Regional Estimates of Violence against Women: Prevalence and Health Effects of Intimate Partner Violence and Non-Partner Sexual Violence; WHO: Geneva, Switzerland, 2013; Available online: https://apps.who.int/iris/bitstream/handle/10665/85239/9789241564625_eng.pdf?sequence=1 (accessed on 28 May 2019).
- Feder, G.; Davies, R.A.; Baird, K.; Dunne, D.; Eldridge, S.; Griffiths, C.; Gregory, A.; Howell, A.; Johnson, M.; Ramsay, J.; et al. Identification and Referral to Improve Safety (IRIS) of women experiencing domestic violence with a primary care training and support programme: A cluster randomised controlled trial. Lancet 2011, 378, 1788–1795. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. Guidance: Domestic Violence and Abuse: Multi-Agency Working; NICE: London, UK, 2012; Available online: https://www.nice.org.uk/guidance/ph50/chapter/3-context (accessed on 28 May 2019).
- Lewis, N.V.; Dowrick, A.; Sohal, A.; Feder, G.; Griffiths, C. Implementation of the Identification and Referral to Improve Safety programme for patients with experience of domestic violence and abuse: A theory-based mixed-method process evaluation. Health Soc. Care Community 2018, 27, e298–e312. [Google Scholar] [CrossRef]
- Identification and Referral to Improve Safety. IRIS Commissioning Guidance. The IRIS Solution—Responding to Domestic Violence and Abuse in General Practice; Howell, A., Johnson, M., Eds.; WHO: Geneva, Switzerland, 2018; Available online: http://www.irisdomesticviolence.org.uk/iris/uploads/documents/IRIS_CommissioningPack_Apr15_LoRes.pdf (accessed on 28 May 2019).
- Council of Europe and Conseil De L’europe. Council of Europe Convention on Preventing and Combating Violence against Women and Domestic Violence; Council of Europe: Strasbourg, France, 2011. [Google Scholar]
- United Nations. General Assembly Resolution 48/104 Containing the Declaration on the Elimination of Violence Against Women. Int. Leg. Mater. 1994, 33, 1049–1054. [Google Scholar] [CrossRef]
- Irisdomesticviolence.org.uk. Domestic Violence and Abuse—IRIS. 2019. Available online: http://www.irisdomesticviolence.org.uk/iris/domestic-abuse-and-health/domestic-violence-and-abuse/ (accessed on 31 May 2019).
- WHO. Violence against Women Prevalence Estimates, 2018. Global, Regional and National Prevalence Estimates for Intimate Partner Violence against Women and Global and Regional Prevalence Estimates for Non-Partner Sexual Violence against Women; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Kilpatrick, D.G. Rape and Sexual Assault, National Violence against Women Prevention Research Center. Ph.D. Thesis, Medical University of South Carolina, Charleston, SC, USA, 2000. [Google Scholar]
- European Union. Violence against Women an EU-Wide Survey; Main Results; Publication Office of The European Union: Luxembourg, 2014. [Google Scholar]
- Office for National Statistics. Intimate Partner Violence and Partner Abuse. England and Wales. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/compendium/focusonviolentcrimeandsexualoffences/yearendingmarch2015/chapter4intimatepersonalviolenceandpartnerabuse (accessed on 31 May 2019).
- Crime and Criminal Justice. Domestic Abuse Recorded by the Police in Scotland, 2018–2019; Scottish Executive Social Research; Scottish Government: Edinburgh, UK, 2019. Available online: https://www.gov.scot/publications/domestic-abuse-scotland-2018-2019-statistics/ (accessed on 14 May 2019).
- Office for National Statistics. Domestic Abuse in England and Wales Overview. 2020. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/bulletins/domesticabuseinenglandandwalesoverview/november2020 (accessed on 15 May 2021).
- Rakovec-Felser, Z. Domestic violence and abuse in intimate relationship from public health perspective. Health Psychol. Res. 2014, 2, 1821. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Intimate Partner Violence—Understanding and Addressing Violence against Women; WHO: Geneva, Switzerland, 2012; Available online: https://apps.who.int/iris/bitstream/handle/10665/77432/WHO_RHR_12.36_eng.pdf;jsessionid=3A693E4CA115DFC5938AAC31EB887E0E?sequence=1 (accessed on 31 May 2019).
- Walby, S. The Cost of Domestic Violence; Women and Equality Unit (DTI): London, UK; University of London Institutional Repository: London, UK, 2004. [Google Scholar]
- John, R.; Johnson, J.; Kukreja, S.; Found, M.; Lindow, S. Domestic violence: Prevalence and association with gynaecological symptoms. BJOG Int. J. Obstet. Gynaecol. 2004, 111, 1128–1132. [Google Scholar] [CrossRef] [PubMed]
- Mezey, G.; Bacchus, L.; Bewley, S.; Haworth, A. An Exploration of the Prevalence and Effects of Domestic Violence in Pregnancy; ESRC Full Research Report, L133251043; ESRC: Swindon, UK, 2002. [Google Scholar]
- Richardson, J.; Coid, J.; Petruckevitch, A.; Chung, W.S.; Moorey, S.; Feder, G. Identifying domestic violence: Cross sectional study in primary care. BMJ 2002, 324, 274. [Google Scholar] [CrossRef] [PubMed]
- Hahn, C.K.; Gilmore, A.K.; Aguayo, R.O.; Rheingold, A.A. Perinatal Intimate Partner Violence. Obstet. Gynecol. Clin. N. Am. 2018, 45, 535–547. [Google Scholar] [CrossRef]
- Belay, S.; Astatkie, A.; Emmelin, M.; Hinderaker, S.G. Intimate partner violence and maternal depression during pregnancy: A community-based cross-sectional study in Ethiopia. PLoS ONE 2019, 14, e0220003. [Google Scholar] [CrossRef]
- Anderson, K.; Van Ee, E. Mothers and Children Exposed to Intimate Partner Violence: A Review of Treatment Interventions. Int. J. Environ. Res. Public Health 2018, 15, 1955. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. Chronic Pain in over 16s: Assessment and Management; National Institute for Health and Care Excellence: London, UK, 2020; Available online: https://www.nice.org.uk/guidance/ng193/documents/draft-guideline (accessed on 14 May 2021).
- Maniadakis, N.; Gray, A. The economic burden of back pain in the UK. Pain 2000, 84, 95–103. [Google Scholar] [CrossRef]
- Campbell, J.; Jones, A.S.; Dienemann, J.; Kub, J.; Schollenberger, J.; O’Campo, P.; Gielen, A.C.; Wynne, C. Intimate Partner Violence and Physical Health Consequences. Arch. Intern. Med. 2002, 162, 1157–1163. [Google Scholar] [CrossRef] [PubMed]
- Jamieson, D.J.; Steege, J.F. The association of sexual abuse with pelvic pain complaints in a primary care population. Am. J. Obstet. Gynecol. 1997, 177, 1408–1412. [Google Scholar] [CrossRef]
- Chandan, J.S.; Thomas, T.; Raza, K.; Bradbury-Jones, C.; Taylor, J.; Bandyopadhyay, S.; Nirantharakumar, K. Intimate Partner Violence and the Risk of Developing Fibromyalgia and Chronic Fatigue Syndrome. J. Interpers. Violence 2019. [Google Scholar] [CrossRef] [PubMed]
- Trevillion, K.; Oram, S.; Feder, G.; Howard, L.M. Experiences of Domestic Violence and Mental Disorders: A Systematic Review and Meta-Analysis. PLoS ONE 2012, 7, e51740. [Google Scholar] [CrossRef] [PubMed]
- Miao, X.-R.; Chen, Q.-B.; Wei, K.; Tao, K.-M.; Lu, Z.-J. Posttraumatic stress disorder: From diagnosis to prevention. Mil. Med. Res. 2018, 5, 1–7. [Google Scholar] [CrossRef]
- Chand, S.P.; Arif, H. Depression. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2019; Available online: https://www.ncbi.nlm.nih.gov/books/NBK430847/ (accessed on 31 May 2019).
- König, H.; Konnopka, A. The excess costs of depression: A systematic review and meta-analysis. Epidemiol. Psychiatr. Sci. 2019, 29, 1–16. [Google Scholar] [CrossRef]
- MHFA Portal. Mental Health Statistics. 2020. Available online: https://mhfaengland.org/mhfa-centre/research-and-evaluation/mental-health-statistics/ (accessed on 14 May 2021).
- Golding, J.M. Intimate Partner Violence as a Risk Factor for Mental Disorders: A Meta-Analysis. J. Fam. Violence 1999, 14, 99–132. [Google Scholar] [CrossRef]
- Fischbach, R.L.; Herbert, B. Domestic violence and mental health: Correlates and conundrums within and across cultures. Soc. Sci. Med. 1997, 45, 1161–1176. [Google Scholar] [CrossRef]
- Devine, A.; Spencer, A.; Eldridge, S.; Norman, R.; Feder, G. Cost-effectiveness of Identification and Referral to Improve Safety (IRIS), a domestic violence training and support programme for primary care: A modelling study based on a randomised controlled trial. BMJ Open 2012, 2, e001008. [Google Scholar] [CrossRef]
- Robbins, R.; McLaughlin, H.; Banks, C.; Bellamy, C.; Thackray, D. Domestic violence and multi-agency risk assessment conferences (MARACs): A scoping review. J. Adult Prot. 2014, 16, 389–398. [Google Scholar] [CrossRef]
- Barbosa, E.C.; Verhoef, T.I.; Morris, S.; Solmi, F.; Johnson, M.; Sohal, A.; El-Shogri, F.; Dowrick, S.; Ronalds, C.; Griffiths, C.; et al. Cost-effectiveness of a domestic violence and abuse training and support programme in primary care in the real world: Updated modelling based on an MRC phase IV observational pragmatic implementation study. BMJ Open 2018, 8, e021256. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence. Who We Are? National Institute for Health and Care Excellence: London, UK, 2018. [Google Scholar]
- Rawlins, M.D.; Culyer, A.J. National Institute for Clinical Excellence and its value judgments. BMJ 2004, 329, 224–227. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. How NICE Measures Value for Money in Relation to Public Health Interventions, LGB10; National Institute for Health and Care Excellence: London, UK, 2013. [Google Scholar]
- Timmins, N.; Rawlins, M.; Appleby, J. A Terrible Beauty—A Short History of NICE; Ministry of Public Health: Nonthaburi, Thailand, 2017.
- Bellis, M.A.; Ashton, K.; Hughes, K.; Ford, K.; Bishop, J.; Paranjothy, S.; Public Health Wales. Adverse Childhood Experiences and Their Impact on Health-Harming Behaviours in the Welsh Adult Population: Alcohol Use, Drug Use, Violence, Sexual Behaviour, Incarceration, Smoking and Poor Diet; Public Health Wales: Cardiff, UK, 2015. [Google Scholar]
- Hegarty, K. Prevalence of abuse and intimate partner violence surgical evaluation (PRAISE) in orthopaedic fracture clinics: A multinational prevalence study. Lancet 2013, 382, 866–876. [Google Scholar] [CrossRef]
- Bhandari, M.; Dosanjh, S.; Tornetta, P.; Matthews, D. Musculoskeletal Manifestations of Physical Abuse after Intimate Partner Violence. J. Trauma Inj. Infect. Crit. Care 2006, 61, 1473–1479. [Google Scholar] [CrossRef]
- Bhandari, M.; Sprague, S.; Tornetta, P., III; D’Aurora, V.; Schemitsch, E.; Shearer, H.; Brink, O.; Mathews, D.; Dosanjh, S. (Mis)Perceptions About Intimate Partner Violence in Women Presenting for Orthopaedic Care: A Survey of Canadian Orthopaedic Surgeons. J. Bone Jt. Surg. 2008, 90, 1590–1597. [Google Scholar] [CrossRef]




| Description | Control Group | Intervention Group |
|---|---|---|
| Number of eligible women per practise | 3088 | 2945 |
| Recorded referral in the general practise electronic medical record | 12 | 223 |
| Recorded disclosure of domestic violence in general practise electronic medical record | 236 | 641 |
| Overall referrals received by specialist domestic violence agencies | 40 | 238 |
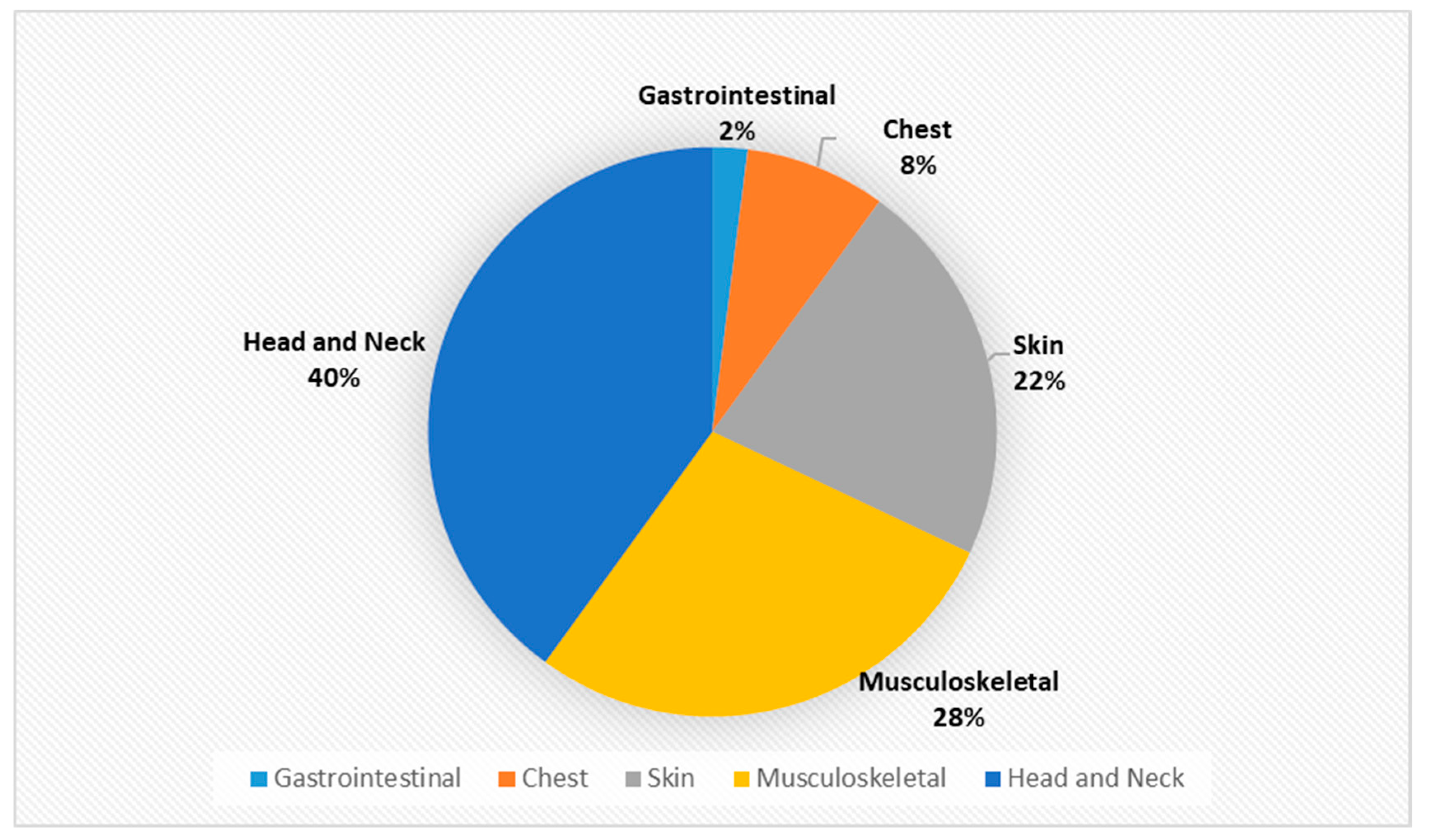
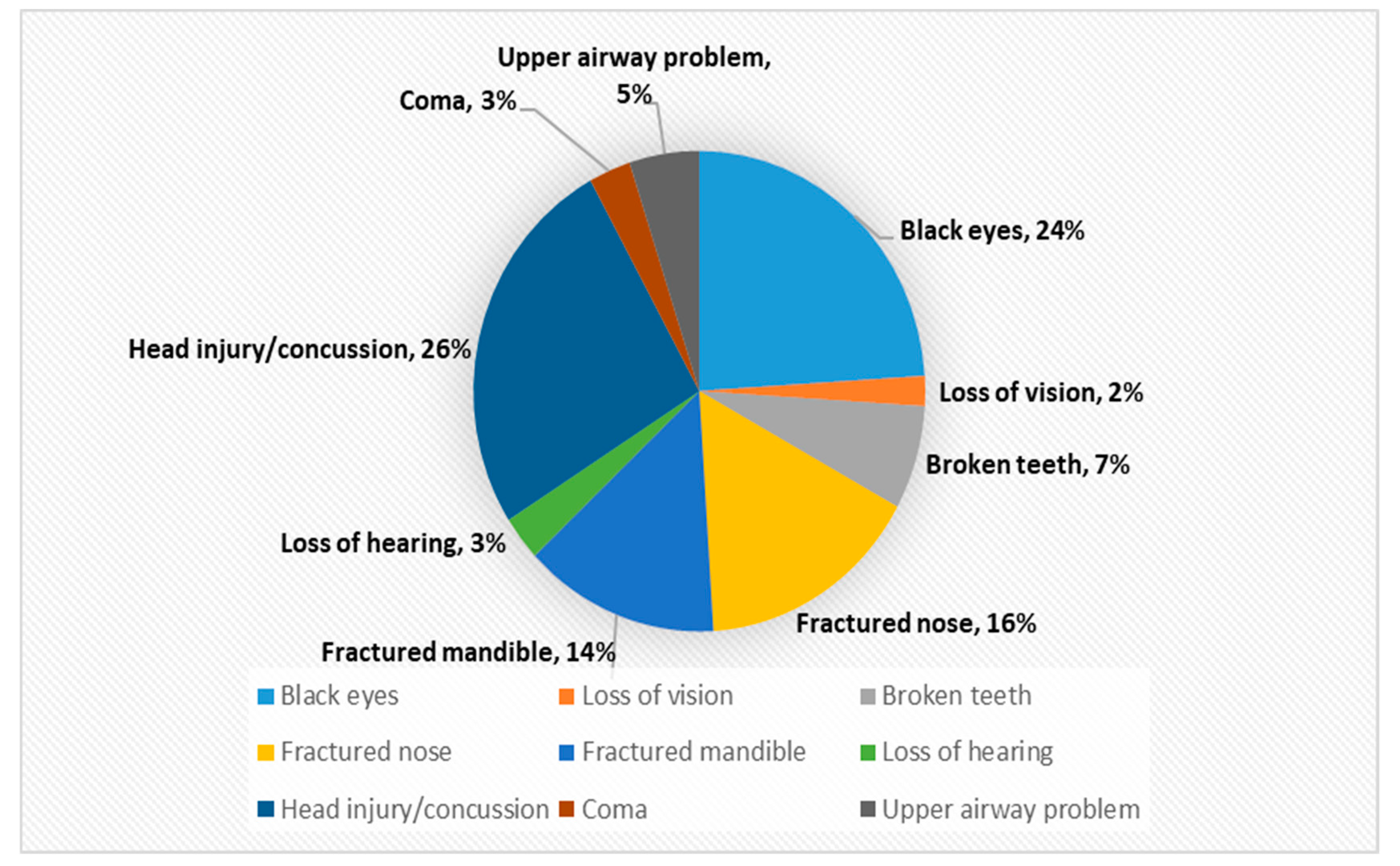
| Type of Injury | Number of Occurrences (n = 144) | Proportion (%) |
|---|---|---|
| Head and Neck | 58 | 40% |
| Black eyes | 14 | 10% |
| Loss of vision | 1 | 1% |
| Broken teeth | 4 | 3% |
| Fractured nose | 9 | 6% |
| Fractured mandible | 8 | 6% |
| Loss of hearing | 2 | 1% |
| Head injury/concussion | 15 | 10% |
| Coma | 2 | 1% |
| Upper airway problem | 3 | 2% |
| Musculoskeletal | 40 | 28% |
| Sprains | 21 | 15% |
| Neck Sprain | 6 | 4% |
| Wrist Sprain | 2 | 1% |
| Back sprain | 7 | 5% |
| Knee sprain | 2 | 1% |
| Ankle sprain | 2 | 1% |
| Foot sprain | 2 | 1% |
| Fracture/Dislocation | 17 | 12% |
| Fingers | 11 | 8% |
| Shoulder dislocation | 3 | 2% |
| Humerus fracture | 1 | 1% |
| Clavicle fracture | 1 | 1% |
| Pelvic fracture | 1 | 1% |
| Foot injury | 2 | 1% |
| Skin | 32 | 22% |
| Burns | 2 | 1% |
| Bruises | 12 | 8% |
| Scratches | 3 | 2% |
| Lacerations | 8 | 6% |
| Lumps | 1 | 1% |
| Stab wounds | 3 | 2% |
| Gunshot wounds | 1 | 1% |
| Bite wounds | 2 | 1% |
| Chest | 11 | 8% |
| Chest contusion | 3 | 2% |
| Fracture ribs Scratches | 8 | 6% |
| Gastrointestinal | 3 | 2% |
| Epigastric tenderness | 2 | 1% |
| Splenic Injury | 1 | 1% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akbari, A.R.; Alam, B.; Ageed, A.; Tse, C.Y.; Henry, A. The Identification and Referral to Improve Safety Programme and the Prevention of Intimate Partner Violence. Int. J. Environ. Res. Public Health 2021, 18, 5653. https://doi.org/10.3390/ijerph18115653
Akbari AR, Alam B, Ageed A, Tse CY, Henry A. The Identification and Referral to Improve Safety Programme and the Prevention of Intimate Partner Violence. International Journal of Environmental Research and Public Health. 2021; 18(11):5653. https://doi.org/10.3390/ijerph18115653
Chicago/Turabian StyleAkbari, Amir Reza, Benyamin Alam, Ahmed Ageed, Cheuk Yin Tse, and Andrew Henry. 2021. "The Identification and Referral to Improve Safety Programme and the Prevention of Intimate Partner Violence" International Journal of Environmental Research and Public Health 18, no. 11: 5653. https://doi.org/10.3390/ijerph18115653
APA StyleAkbari, A. R., Alam, B., Ageed, A., Tse, C. Y., & Henry, A. (2021). The Identification and Referral to Improve Safety Programme and the Prevention of Intimate Partner Violence. International Journal of Environmental Research and Public Health, 18(11), 5653. https://doi.org/10.3390/ijerph18115653






