1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has brought unprecedented changes, affecting everyday life in many different ways, including worries about health, employment, finances, and the challenges of combining work and family obligations [
1]. Social distancing, lockdowns, dwindling economy, and unemployment are posing major challenges all over the world, and creating stressful circumstances and health risks that can have a major impact on nighttime sleep, at a time when healthy sleep is of paramount importance in order to cope and adapt with this crisis and uncertainty about the future [
1].
Insomnia is the most common sleep-related complaint and the second most common overall complaint (after pain) reported in primary care practice, with about 30–50% of adults reporting problems with sleep in a given year [
2]. Based on many population studies, one-third of adults have frequent trouble falling asleep, staying asleep, or overall poor sleep quality [
3]. In addition to the substantial suffering of individuals with insomnia, the disorder also causes high societal costs because of sick leave, use of healthcare, and lost productivity. Insomnia is associated with, and is a suspected contributing factor to, conditions such as cardiac disease, diabetes, anxiety, and depression [
4]. While investigating the early impact of the COVID-19 pandemic on sleep and psychological symptoms in 5641 Chinese adults in mid-February 2020, Lin et al. noted very high rates of clinically significant insomnia (20%) and acute stress (15.8%) [
5].
Insomnia is associated with several adverse health outcomes, such as poor physical health, poor mental health, including symptoms of anxiety and depression, and decreased quality of life [
6,
7]. Cognitive behavioral therapy for insomnia (CBT-I), traditionally used to treat chronic insomnia, has recently been used to treat acute insomnia secondary to the situational changes from acute stress [
8,
9]. Although CBT-I is traditionally delivered in face-to-face individuals or group settings, remote delivery online or by telephone has also been used, albeit with less robust
supporting data. Though CBT-I is an effective and recommended first line treatment modality, it needs trained providers. Usually, there is a delay in therapeutic response, which limits its use and acceptance. Due to these limitations, most people choose pharmacological treatment for insomnia. Commonly used medications are short or intermediate acting benzodiazepine receptor agonists that have significant side effects. Notable side effects are drowsiness, fatigue, confusion, ataxia, falls, hip fractures, anterograde amnesia, anxiety, complex sleep related behaviors, such as sleepwalking, and serious adverse effects, including dependence, with grave consequences and economic burdens [
10]. Currently, an estimated USD 30–107 billion is annually spent on insomnia management in the U.S. [
11,
12]. In addition, insomnia has been reported to result in an annual loss of workplace productivity to an estimated USD 63.2 billion [
13]. Therefore, there is an urgent need to explore novel and innovative treatment modalities that are easily available with the least (or no) side effects and are cost-effective, without the need for in-person contact.
Yoga of Immortals (YOI) is a comprehensive program developed by ShivYog, an organization that teaches specific practices based on ancient yogic teachings [
14,
15]. Much of today’s yoga, meditation, and mindfulness practices are derived from these ancient yogic teachings [
16]. Although YOI has been in practice in the Eastern hemisphere for centuries with many health benefits, it was only taught through in-person meetings to a very few individuals. Hence, no published outcome data are available to date. A structured YOI program was recently developed for a mobile platform—a platform that is increasingly being utilized and accepted in today’s technological society. This study investigates whether the app-based YOI intervention effectively treats insomnia symptoms, especially in the background of a global pandemic that has caused immense population distress and simultaneous disruption of access to care.
3. Results
The demographic details categorized into age, gender, educational status, race and ethnicity, occupation, and associated psychiatric disorders are shown in
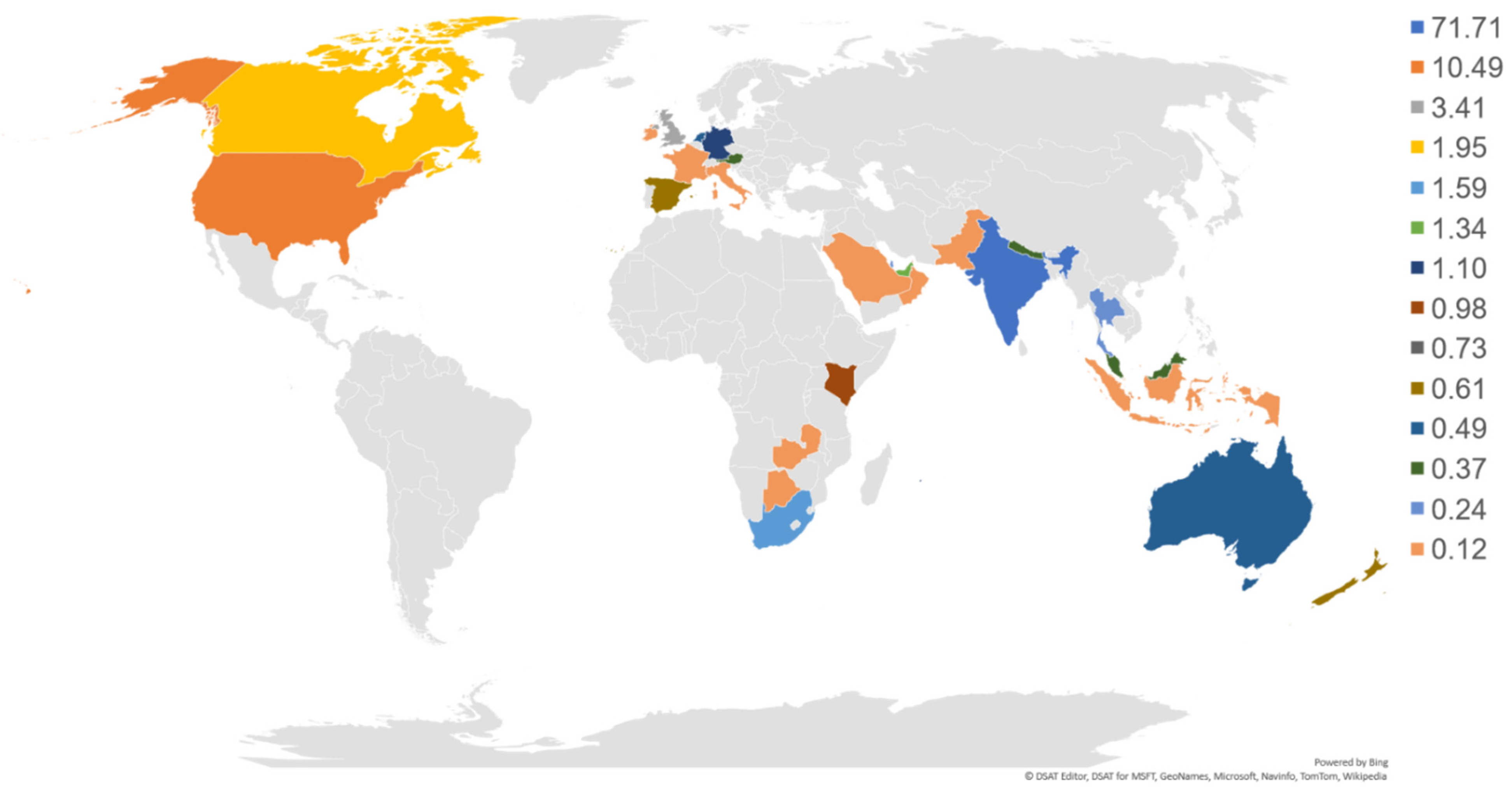
Table 1. The maximum percentage of participants were in the age group of 26–47 (61.8%), followed by 48–58 (23.0%), 59–69 (8%), and 18–25 (6.3%). The percentage of participants >70 was less than 1%. The study participants had more females (53.8%) than males (46.1%). The highest qualification ranked from school level to Ph.D. level. Geographically, participants were from 14 different countries; however, the maximum number of participants were of Asian race (88.4%) (
Figure 2).
Based on pre-survey (week 0) questionnaires, 41 (5%) participants had severe insomnia (SI), 92 (11.22%) had moderate insomnia (MI), 149 (18.17%) had subthreshold insomnia (STI) (
Table 2 and
Figure 3). Following YOI intervention, a marked reduction in the mean ISI score was noted in all categories, 23.88 ± 0.25 to 10.46 ± 1.27 in the severe group; 17.71 ± 0.21 to 6.51 ± 0.64 in the moderate group, and 10.87 ± 0.17 to 4.95 ± 0.38 in the subthreshold group (
Table 2).
At baseline, 41 participants had severe insomnia; 92, moderate insomnia; and 149 had subthreshold insomnia. At 8 weeks, these numbers were reduced to 9 in the severe group, 33 in the moderate group, and 74 in the subthreshold group, with an increase in the number of participants in the ‘no clinically significant insomnia’ category (537 at baseline; increased to 703 at 8 weeks). Compared to baseline, in the severe group, there was 92.68% reduction in the number of participants at 4 weeks and 78.05% reduction at 8 weeks. Likewise, the number of participants with moderate insomnia reduced by 70.65% at 4 weeks and 64.13% at 8 weeks. The number of participants with subthreshold insomnia reduced by 30.87% at 4 weeks and further reduced by 50.34% at 8 weeks (
Table 3). On the contrary, the number of participants with ‘no clinically significant insomnia’ increased by 27.75% at 4 weeks and 30.91% at 8 weeks (
Table 3), indicating that those participants in the severe, moderate, and subthreshold categories moved into the ‘no clinically significant insomnia’ category after YOI intervention.
When we analyzed the effect of YOI intervention in different age groups, there was a reduction in the number of participants with severe insomnia in all age groups except 59–69 years and 70–80 years. There was no one at baseline in the 59–69 age group, but two at 8 weeks. This may be due to the limited number of participants in these age groups. Likewise, there was no one at baseline in the 70–80 age group, but one at 8 weeks. In the moderate insomnia category, there was, again, a reduction in the number of participants in all age groups at 8 weeks, except for 59–69 years and 70–80 years. In the 59–69 age group, there were two participants at baseline, which remained the same at 8 weeks. In the subthreshold insomnia category, there was a reduction in the number of participants among all age groups at 8 weeks (
Table 3;
Figure 4, A1–D1).
Although the participants were instructed to practice the YOI daily, it is conceivable that not everyone can practice every day due to personal commitments and other constraints. Therefore, we studied the effect of the frequency of YOI practice on the insomnia scores and noted that most participants (79.4%) practiced the YOI daily; 15.98% practiced 4–6 times per week, while 4.63% practiced 2–3 times per week. The higher percentage of participants with daily practice could be a sign of participant acceptance of YOI intervention, which could be due to benefits received to participants through daily practice. The mean ISI score was lowest for the participants who practiced the YOI everyday (
Table 4;
Figure 5). The scores for daily practitioners were one-half (3.05 ± 0.16) compared to those who practiced YOI 2–3 times (6.63 ± 0.95), or 4–6 times per week 4.58 ± 0.42. This suggests that participants who practiced YOI daily had better improvement than those who did not (
Figure 5).
We also compared the effect of the frequency of YOI practice in different insomnia categories (
Table 5;
Figure 6). We observed a decreasing trend in mean ISI scores with an increase in the frequency of YOI practice. There was a statistically significant difference in severe and subthreshold insomnia categories. Those practicing YOI intervention every day had the lowest mean score than those practicing 4–6 times, followed by the highest average score for those practicing 2–3 times a week.
Mean ISI scores were also assessed in participants with self-reported psychiatric disorders (
Table 6). One hundred fifteen (14.02%) participants had psychiatric disorders, out of which 53 (46.09%) had more than one psychiatric disorder. In the latter group, the most commonly found conditions were major depression, generalized anxiety disorder (GAD), and eating disorders. After YOI intervention, we found a significant reduction in the mean ISI score in the multiple disorder group (13.53 ± 1.16 to 7.28 ± 0.97,
p ≤ 0.0001)
. The other group with a significant reduction in the mean ISI score was GAD (10.96 ± 1.60 to 5.26 ± 1.00,
p ≤ 0.01). Compared to baseline, the reduction in the mean scores at 8 weeks was ~50% in both.
4. Discussion
Sleep is a very important factor affecting the health of an individual, just like nutrition. It is a basic requirement for the normal functioning of metabolic, endocrine, neurological, and cognitive functions; it is vital for one’s health and general well-being. Currently, cognitive behavioral therapy (CBT-I) and pharmacological intervention constitute the mainstay treatments of insomnia. Clinical practice guidelines published by the American College of Physicians (2016) recommended CBT-I as the initial treatment for insomnia [
11]. Although CBT-I is considered the treatment of choice, the availability of trained personnel is the limiting factor for the effective implementation of a structured CBT-I program. In addition, CBT-I is not widely used, partly due to the cost of treatment by trained CBT-I providers and lack of insurance coverage for these services [
19]. Furthermore, psychological and behavioral interventions are complex, have various protocols, and may have varying degrees of success for different individuals [
20]. These issues with CBT-I carry even greater significance in the current setting of the COVID 19 pandemic.
According to the clinical practice guidelines published by the American College of Physicians (2016), CBT-I has been documented to result in a mean difference in the ISI score of −4.78 (95% CI, −6.45 to −3.11) compared to the inactive control [
11]. Our study noted a 13.42 point reduction in the ISI score in the severe group, an 11.2 point reduction in the moderate group, and a 5.92 point reduction in the subthreshold group (
Table 2) at 8 weeks following YOI intervention. Besides, the YOI mobile app-based intervention in the current study effectively reduced insomnia symptom severity at 4 weeks. It was maintained at 8 weeks with a statistically significant decrease in the mean ISI scores in all insomnia categories (
Table 2). YOI intervention also showed marked improvement in the ISI scores among most age groups (
Table 3)). We also assessed the effect of frequency of YOI practice on the outcomes and found a decreasing trend in the mean ISI scores with increasing frequency of practice among all insomnia categories (
Table 5;
Figure 6).
Regarding pharmacotherapy of insomnia, over the counter (OTC) sleep aids (e.g., diphenhydramine) are often used to manage sleeping difficulties, despite evidence suggesting such a practice may be risky. Prescription drug therapy includes benzodiazepines, non-benzodiazepine hypnotics, orexin receptor antagonist, the melatonin receptor agonist, ramelteon; the antidepressant, doxepin; and melatonin. Most prescription insomnia medications are either recommended on a limited basis or not recommended because of adverse outcomes. Observational studies have shown that hypnotic drugs may be associated with serious adverse effects, such as dementia, serious injury, and fractures [
21,
22].
A systematic evidence review of pharmacological therapies published by the American College of Physicians showed that eszopiclone, a non-benzodiazepine hypnotic, improved insomnia with a 4.6 point reduction in the ISI score [
11]. Another agent, suvorexant, an orexin receptor antagonist, resulted in a 1.2 point reduction in the ISI score. However, a much higher reduction in the ISI scores was observed in our study using YOI intervention, as described above, in the comparison of our data with CBT-I.
Complementary and alternative therapies, such as Chinese herbal medicine, and acupuncture have also been used to treat insomnia. However, there is a paucity of good quality evidence on these therapies in insomnia. For example, Yin et al. showed improvement in the ISI score with acupuncture at 2 and 4 weeks post-treatment [
23]. However, this is in-person treatment, and it requires the availability of a qualified and certified acupuncturist. In contrast, YOI is app-based and does not require an in-person visit.
Mind-body therapies (MBTs), including meditation, Tai chi, Qigong, and yoga, have been used to treat insomnia. These therapies have demonstrated some benefits in randomized control trials for insomnia and depression [
24,
25,
26]. However, in a systematic review and meta-analysis that included 10 studies with 926 participants using ISI, Wang et al. did not find significant reduction in the severity of insomnia symptoms (effect size:−0.26; 95% CI: −0.60 to −0.09;
p = 0.142) using mind–body therapies (MBTs) [
27]. Although YOI utilizes certain meditative movements and breath regulation and exercises, it is fundamentally different from Tai chi and Qigong, and uniquely connects the individual to the universal energy source.
Beneficial effects of seated meditation, breathing practices, and yoga asana practices are associated with a reduction in sympathetic nervous system activation. This is proven by parallel reductions in catecholamines epinephrine and norepinephrine levels [
28,
29], reducing the stress, thereby improving insomnia. Normal healthy sleep, regulation of circadian rhythm, and maintenance of internal biological clock are dependent on melatonin, a hormone secreted in the pineal gland [
30]. Meditation and yoga have been shown to enhance the activity of melatonin, thereby improving insomnia [
28].
In our study, participants were from all over the world, spanning 14 countries in different continents, different ethnic groups, educational and employment statuses, and included both genders. Therefore, we feel the results of our study are mostly generalizable; however, most of the participants (~88%) were Asian in this study. To our knowledge, ours is the first known study of YOI intervention in participants with self-reported insomnia.