Improved Inpatient Care through Greater Patient–Doctor Contact under the Hospitalist Management Approach: A Real-Time Assessment
Abstract
1. Introduction
2. Methods
2.1. Data Source
2.2. Measures
2.2.1. Patient–Doctor Contact
2.2.2. Medical Call Response
- (a)
- Example of patient–doctor contact recording slip
| Patient ID | Time “ | Purpose | Duration | Contact Doctor |
| 1: Day 2: Night | 1: procedure; 2: condition check; 3: rounding; 4: requested referral; 5: consultation including explanation, prescription, consent; 6: others | Mins | 1: hospitalist; 2: training doctor *; 3: other doctor | |
| 1a23c0 | 1 | 4 | 5 | 1 |
| 1a5544 | 1 | 3 | 6 | 1,3 |
| “ Day (06:00–21:59), night (22:00–05:59); * training doctors: intern or resident doctor. | ||||
- (b)
- Example of medical call response slip
| Patient ID | Time “ | Contact Doctor | Purpose | Contact | Response Time after the Call |
| 1: Day 2: Night | 1: hospitalist; 2: training doctor *; 3: other doctor | 1: procedure; 2: condition check; 3: rounding; 4: requested referral; 5: consultation including explanation, prescription, consent; 6: others | 1: succeed 2: Not succeed | Mins | |
| 1a23c0 | 1 | 1 | 5 | 1 | 2 |
| 1a5544 | 1 | 2 | 1 | 2 | 5 |
| “ Day (06:00–21:59), night (22:00–05:59); * training doctors: intern or resident doctor. | |||||
2.3. Covariates
2.4. Statistical Analyses
2.5. Ethical Statement
3. Results
3.1. Association of the Frequency of Patient–Doctor Contact
3.2. Patient–Doctor Contact Duration Per Session
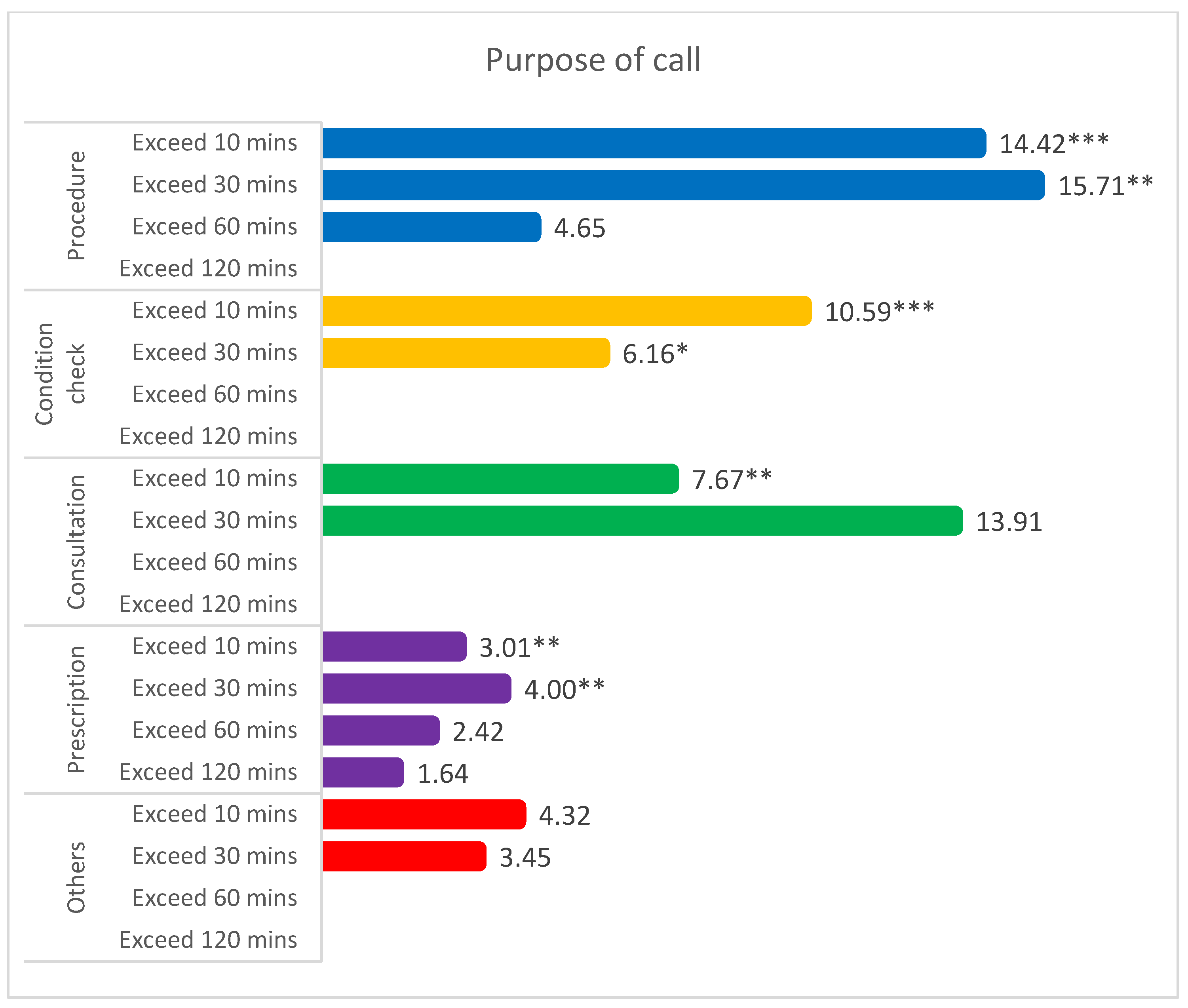
3.3. Association of Cumulative Contact Time with the Purpose of Patient–Doctor Contact
3.4. Response to a Medical Call and Resolving the Issue
4. Discussion
Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Disclaimer
References
- Barber, R.M.; Fullman, N.; Sorensen, R.J.; Bollyky, T.; McKee, M.; Nolte, E.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; et al. Healthcare access and quality index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990-2015: A novel analysis from the global burden of disease study 2015. Lancet 2017, 390, 231–266. [Google Scholar] [CrossRef]
- Sutker, W.L. The physician’s role in patient safety: What’s in it for me? Proceedings (Bayl. Univ. Med. Cent.) 2008, 21, 9–14. [Google Scholar] [CrossRef]
- Chipidza, F.E.; Wallwork, R.S.; Stern, T.A. Impact of the doctor-patient relationship. Prim. Care Companion CNS Disord. 2015, 17. [Google Scholar] [CrossRef]
- Plantinga, L.C.; Fink, N.E.; Sadler, J.H.; Levey, A.S.; Levin, N.W.; Rubin, H.R.; Coresh, J.; Klag, M.J.; Powe, N.R. Frequency of patient-physician contact and patient outcomes in hemodialysis care. J. Am. Soc. Nephrol. 2004, 15, 210–218. [Google Scholar] [CrossRef]
- Plantinga, L.C.; Jaar, B.G.; Fink, N.E.; Sadler, J.H.; Levin, N.W.; Coresh, J.; Klag, M.J.; Powe, N.R. Frequency of patient–physician contact in chronic kidney disease care and achievement of clinical performance targets. Int. J. Qual. Health Care 2005, 17, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Mohr, D.C.; Ho, J.; Duffecy, J.; Reifler, D.; Sokol, L.; Burns, M.N.; Jin, L.; Siddique, J. Effect of telephone-administered vs face-to-face cognitive behavioral therapy on adherence to therapy and depression outcomes among primary care patients: A randomized trial. JAMA 2012, 307, 2278–2285. [Google Scholar] [CrossRef] [PubMed]
- Hausman, A. Modeling the patient-physician service encounter: Improving patient outcomes. J. Acad. Mark. Sci. 2004, 32, 403. [Google Scholar] [CrossRef]
- Yi, C.; Guo, Q.; Lin, J.; Li, J.; Yu, X.; Yang, X. Patient-doctor contact interval and clinical outcomes in continuous ambulatory peritoneal dialysis patients. Am. J. Nephrol. 2017, 45, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, T.; Karaboyas, A.; Robinson, B.M.; Li, Y.; Fukuhara, S.; Bieber, B.A.; Rayner, H.C.; Andreucci, V.E.; Pisoni, R.L.; Port, F.K.; et al. Associations of frequency and duration of patient-doctor contact in hemodialysis facilities with mortality. J. Am. Soc. Nephrol. 2013, 24, 1493–1502. [Google Scholar] [CrossRef]
- Tates, K.; Antheunis, M.L.; Kanters, S.; Nieboer, T.E.; Gerritse, M.B. The effect of screen-to-screen versus face-to-face consultation on doctor-patient communication: An experimental study with simulated patients. J. Med. Internet Res. 2017, 19, e421. [Google Scholar] [CrossRef] [PubMed]
- Paterick, T.E.; Patel, N.; Tajik, A.J.; Chandrasekaran, K. Improving health outcomes through patient education and partnerships with patients. Proceedings (Bayl. Univ. Med. Cent.) 2017, 30, 112–113. [Google Scholar] [CrossRef]
- Brédart, A.; Bouleuc, C.; Dolbeault, S. Doctor-patient communication and satisfaction with care in oncology. Curr. Opin. Oncol. 2005, 17, 351–354. [Google Scholar] [CrossRef]
- Darmayanti, D.; Simatupang, T.M.; Rudito, P. Patient engagement activities with health care professionals in continuous ambulatory peritoneal dialysis therapy: An exploratory pilot study. Int. J. Nephrol. Renov. Dis. 2019, 12, 103–112. [Google Scholar] [CrossRef]
- Barnett, P.B. Rapport and the hospitalist. Am. J. Med. 2001, 111, 31–35. [Google Scholar] [CrossRef]
- Custer, A.; Rein, L.; Nguyen, D.; Wentworth, K.; Dhamoon, A. Development of a real-time physician–patient communication data collection tool. BMJ Open Qual. 2019, 8, e000599. [Google Scholar] [CrossRef] [PubMed]
- Wachter, R.M.; Goldman, L. The emerging role of “hospitalists” in the American health care system. N. Engl. J. Med. 1996, 335, 514–517. [Google Scholar] [CrossRef] [PubMed]
- Dugdale, D.C.; Epstein, R.; Pantilat, S.Z. Time and the patient-physician relationship. J. Gen. Intern. Med. 1999, 14 (Suppl. 1), S34–S40. [Google Scholar] [CrossRef]
- Bell, R.A.; Kravitz, R.L.; Thom, D.; Krupat, E.; Azari, R. Unmet expectations for care and the patient-physician relationship. J. Gen. Intern. Med. 2002, 17, 817–824. [Google Scholar] [CrossRef] [PubMed]
- Ogden, J.; Bavalia, K.; Bull, M.; Frankum, S.; Goldie, C.; Gosslau, M.; Jones, A.; Kumar, S.; Vasant, K. “I want more time with my doctor”: A quantitative study of time and the consultation. Fam. Pract. 2004, 21, 479–483. [Google Scholar] [CrossRef] [PubMed]
- Nobili, A.; Garattini, S.; Mannucci, P.M. Multiple diseases and polypharmacy in the elderly: Challenges for the internist of the third millennium. J. Comorbidity 2011, 1, 28–44. [Google Scholar] [CrossRef]
- Golchin, N.; Frank, S.H.; Vince, A.; Isham, L.; Meropol, S.B. Polypharmacy in the elderly. J. Res. Pharm Pract. 2015, 4, 85–88. [Google Scholar] [CrossRef]
- Lees, J.; Chan, A. Polypharmacy in elderly patients with cancer: Clinical implications and management. Lancet Oncol. 2011, 12, 1249–1257. [Google Scholar] [CrossRef]
- Kuo, Y.-F.; Sharma, G.; Freeman, J.L.; Goodwin, J.S. Growth in the care of older patients by hospitalists in the United States. N. Engl. J. Med. 2009, 360, 1102–1112. [Google Scholar] [CrossRef]
- Aiken, L.H.; Sermeus, W.; Van den Heede, K.; Sloane, D.M.; Busse, R.; McKee, M.; Bruyneel, L.; Rafferty, A.M.; Griffiths, P.; Moreno-Casbas, M.T.; et al. Patient safety, satisfaction, and quality of hospital care: Cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ 2012, 344, e1717. [Google Scholar] [CrossRef] [PubMed]
- Wachter, R.M.; Goldman, L. Zero to 50,000—The 20th anniversary of the hospitalist. N. Engl. J. Med. 2016, 375, 1009–1011. [Google Scholar] [CrossRef] [PubMed]
- White, H.L.; Glazier, R.H. Do hospitalist physicians improve the quality of inpatient care delivery? A systematic review of process, efficiency and outcome measures. BMC Med. 2011, 9, 58. [Google Scholar] [CrossRef] [PubMed]
- Jang, S.-I. Korean hospitalist system implementation and development strategies based on pilot studies. J. Korean Med. Assoc. 2019, 62, 558–563. [Google Scholar] [CrossRef]
- Jang, S.-I.; Park, E.-C.; Nam, J.M.; Chae, W.; Lee, N.-K.; Kim, J.Y.; Lee, J.E.; Cho, Y.D. A Study on the Implementation and the Evaluation of Korean Hospitalist System to Improve the Quality of Hospitalization (Phase 2); Institute of Health Services Research, Yonsei University: Seoul, Korea, 2018. [Google Scholar]
- Chae, W.; Park, E.C.; Lee, K.Y.; Kang, H.J.; Lee, W.Y.; Kim, Y.M.; Jang, S.I. Development and evolution of hospital medicine in korea. J. Hosp. Med. 2021, 16, 247–250. [Google Scholar] [CrossRef]
- Arora, N.K. Interacting with cancer patients: The significance of physicians’ communication behavior. Soc. Sci. Med. 2003, 57, 791–806. [Google Scholar] [CrossRef]
- Shenolikar, R.A.; Balkrishnan, R.; Hall, M.A. How patient-physician encounters in critical medical situations affect trust: Results of a national survey. BMC Health Serv. Res. 2004, 4, 24. [Google Scholar] [CrossRef]
- Coffman, J.; Rundall, T.G. The impact of hospitalists on the cost and quality of inpatient care in the united states: A research synthesis. Med. Care Res. Rev. 2005, 62, 379–406. [Google Scholar] [CrossRef] [PubMed]
- Levine, R.; Shore, K.; Lubalin, J.; Garfinkel, S.; Hurtado, M.; Carman, K. Comparing physician and patient perceptions of quality in ambulatory care. Int. J. Qual. Health Care 2012, 24, 348–356. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Han, S.J.; Jung, H.-W.; Oh, D.-Y.; Lee, J.H.; Moon, S.D.; Lee, S.; Yoon, J.-H. Comparisons of clinical outcomes between weekday-only and full-time, 24-h/7-day coverage hospitalist systems. J. Korean Med. Sci. 2020, 35. [Google Scholar] [CrossRef] [PubMed]
| Variables | Total | Case (Hospitalist Ward) | Control (Non-Hospitalist Ward) | p-Value | Adjusted Difference ⁺ | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | ± | SD | Mean | ± | SD | Mean | ± | SD | β | SE | ||
| Total | 7.3 | ± | 9.0 | 10.1 | ± | 11.0 | 4.2 | ± | 4.0 | <0.001 | 5.6 *** | 0.3 |
| Sex | ||||||||||||
| Male | 7.0 | ± | 8.2 | 9.7 | ± | 10.0 | 4.2 | ± | 4.2 | <0.001 | 5.5 *** | 0.4 |
| Female | 7.7 | ± | 9.8 | 10.4 | ± | 11.8 | 4.1 | ± | 3.7 | <0.001 | 5.7 *** | 0.4 |
| Age | ||||||||||||
| 19 and below | 6.0 | ± | 5.8 | 7.9 | ± | 7.7 | 4.3 | ± | 2.5 | 0.080 | 1.6 * | 0.8 |
| 20–29 | 6.1 | ± | 6.6 | 9.3 | ± | 8.7 | 4.2 | ± | 3.8 | <0.001 | 3.9 * | 1.6 |
| 30–39 | 6.3 | ± | 6.3 | 8.4 | ± | 7.2 | 3.7 | ± | 3.6 | <0.001 | 4.6 *** | 1.0 |
| 40–49 | 6.5 | ± | 5.7 | 8.4 | ± | 6.3 | 4.0 | ± | 3.4 | <0.001 | 4.0 *** | 0.5 |
| 50–59 | 7.1 | ± | 9.1 | 9.8 | ± | 11.3 | 3.8 | ± | 3.2 | <0.001 | 5.6 *** | 0.6 |
| 60–69 | 7.7 | ± | 9.9 | 10.8 | ± | 12.3 | 4.1 | ± | 3.6 | <0.001 | 6.7 *** | 0.6 |
| 70–79 | 7.8 | ± | 9.9 | 10.9 | ± | 12.3 | 4.3 | ± | 4.0 | <0.001 | 6.3 *** | 0.6 |
| 80 and above | 8.6 | ± | 10.6 | 11.0 | ± | 12.1 | 5.4 | ± | 7.0 | <0.001 | 4.5 *** | 1.1 |
| Medical division | ||||||||||||
| Internal medicine | 7.2 | ± | 9.2 | 9.4 | ± | 11.4 | 4.6 | ± | 4.2 | <0.001 | 4.5 *** | 0.3 |
| Surgery | 7.8 | ± | 8.4 | 11.9 | ± | 9.3 | 2.9 | ± | 3.0 | <0.001 | 8.7 *** | 0.5 |
| Admission type | ||||||||||||
| General admission | 7.7 | ± | 9.4 | 10.7 | ± | 11.4 | 4.2 | ± | 4.1 | <0.001 | 6.2 *** | 0.3 |
| ER admission | 4.1 | ± | 2.7 | 4.5 | ± | 3.1 | 3.8 | ± | 2.3 | 0.017 | 1.0 ** | 0.3 |
| Region | ||||||||||||
| Capital | 6.6 | ± | 7.1 | 8.7 | ± | 8.3 | 4.2 | ± | 4.3 | <0.001 | 4.4 *** | 0.3 |
| Rural | 9.8 | ± | 13.1 | 14.1 | ± | 15.8 | 3.9 | ± | 2.5 | <0.001 | 10.1 *** | 0.8 |
| CCI ‡ | ||||||||||||
| 0 | 6.0 | ± | 7.5 | 8.2 | ± | 9.9 | 4.1 | ± | 3.7 | <0.001 | 3.4 *** | 0.5 |
| 1 | 8.1 | ± | 10.2 | 10.0 | ± | 13.0 | 5.9 | ± | 4.9 | <0.001 | 3.2 *** | 0.9 |
| 2 | 6.9 | ± | 7.6 | 9.3 | ± | 8.8 | 3.9 | ± | 4.1 | <0.001 | 5.7 *** | 0.4 |
| 3 | 10.0 | ± | 11.8 | 13.7 | ± | 13.4 | 3.6 | ± | 2.9 | <0.001 | 9.4 *** | 1.2 |
| 4< | 9.9 | ± | 12.9 | 14.1 | ± | 15.1 | 3.7 | ± | 3.2 | <0.001 | 10.2 *** | 1.1 |
| Variables | Contact Time (min) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Hospitalist | Training Doctor | Other Doctor | p-Value | |||||||||
| Mean | ± | SD | Mean | ± | SD | Mean | ± | SD | Mean | ± | SD | ||
| Total | |||||||||||||
| 4.9 | ± | 4.5 | 4.7 | ± | 3.7 | 5.0 | ± | 4.5 | 5.6 | ± | 7.6 | <0.001 | |
| Medical division | |||||||||||||
| Internal medicine | 4.7 | ± | 4.6 | 4.4 | ± | 3.2 | 4.9 | ± | 4.3 | 5.8 | ± | 8.2 | <0.001 |
| Surgery | 5.5 | ± | 4.3 | 5.6 | ± | 4.5 | 4.9 | ± | 3.4 | 3.8 | ± | 2.6 | <0.001 |
| Admission type | |||||||||||||
| General admission | 4.5 | ± | 3.8 | 4.7 | ± | 3.7 | 4.4 | ± | 4.1 | 3.8 | ± | 4.2 | <0.001 |
| ER admission | 9.2 | ± | 8.2 | 7.4 | ± | 4.1 | 8.0 | ± | 3.6 | 13. 6 | ± | 13.5 | <0.001 |
| Region | |||||||||||||
| Capital | 5.1 | ± | 4.8 | 5.0 | ± | 3.9 | 4.4 | ± | 3.9 | 8.3 | ± | 9.4 | <0.001 |
| Rural | 4.5 | ± | 4.03 | 4.1 | ± | 3.1 | 7.5 | ± | 5.7 | 3.3 | ± | 4.5 | <0.001 |
| Shift | |||||||||||||
| Day | 4.9 | ± | 4.5 | 4.7 | ± | 3.6 | 4.9 | ± | 4.5 | 5.6 | ± | 7.6 | <0.001 |
| Night | 5.8 | ± | 4.3 | 7.5 | ± | 5.0 | 6.2 | ± | 5.3 | 5.8 | ± | 2.9 | 0.196 |
| Purpose of the contacts | |||||||||||||
| Procedure | 11.0 | ± | 10.3 | 8.8 | ± | 7.7 | 9.4 | ± | 6.6 | 27.7 | ± | 16.4 | <0.001 |
| Condition check | 4.5 | ± | 3.3 | 4.4 | ± | 3.2 | 4.4 | ± | 3.4 | 7.0 | ± | 8.1 | <0.001 |
| Rounding | 3.8 | ± | 2.2 | 4.2 | ± | 2.2 | 3.1 | ± | 2.5 | 3.0 | ± | 2.1 | <0.001 |
| Consultation with other doctors | 9.3 | ± | 5.8 | 9.2 | ± | 10.1 | 9.3 | ± | 6.1 | 9.4 | ± | 6.2 | 0.996 |
| Consultation with patients | 7.7 | ± | 5.8 | 7.9 | ± | 6.4 | 7.7 | ± | 5.0 | 9.4 | ± | 8.8 | 0.099 |
| Others | 6.1 | ± | 7.9 | 5.5 | ± | 7.7 | 5.1 | ± | 5.7 | 17.5 | ± | 17.7 | 0.079 |
| Variables | Patient–Doctor Contact Duration Per Session (min) | |||||
|---|---|---|---|---|---|---|
| Training Doctor | Other Doctor | |||||
| β | SE | p-Value | β | SE | p-Value | |
| Total | ||||||
| −1.23 | 0.06 | <0.001 | 0.44 | 0.09 | <0.001 | |
| Medical division | ||||||
| Internal medicine | −1.70 | 0.07 | <0.001 | 0.25 | 0.09 | 0.004 |
| Surgery | −0.50 | 0.13 | <0.001 | −1.10 | 0.46 | 0.017 |
| Admission type | ||||||
| General admission | −0.70 | 0.06 | <0.001 | −0.97 | 0.08 | <0.001 |
| ER admission | −3.56 | 0.43 | <0.001 | 5.93 | 0.52 | <0.001 |
| Region | ||||||
| Capital | −1.72 | 0.07 | <0.001 | 3.40 | 0.15 | <0.001 |
| Rural | 1.38 | 0.12 | <0.001 | −1.71 | 0.09 | <0.001 |
| Shift | ||||||
| Day | −1.21 | 0.12 | <0.001 | 0.43 | 0.09 | <0.001 |
| Night | −2.87 | 0.59 | <0.001 | −3.81 | 1.50 | 0.011 |
| Purpose of the contacts | ||||||
| Procedure | −2.35 | 0.60 | <0.001 | 15.22 | 1.01 | <0.001 |
| Condition check | −1.65 | 0.11 | <0.001 | 1.25 | 0.28 | <0.001 |
| Rounding | −1.47 | 0.04 | <0.001 | −0.95 | 0.05 | <0.001 |
| Consultation with other doctors | 1.28 | 1.23 | 0.301 | −0.01 | 0.99 | 0.994 |
| Consultation with patients | −0.57 | 0.24 | 0.017 | 0.72 | 0.84 | 0.386 |
| Others | −3.15 | 6.11 | 0.611 | 23.78 | 7.55 | 0.004 |
| Variables | Cumulative Contact Time (min) | ||
|---|---|---|---|
| Hospitalist Ward | p-Value | ||
| β | SE | ||
| Cumulative contact time | |||
| Total | 32.29 | 1.54 | <0.001 |
| Procedure | 2.39 | 0.50 | <0.001 |
| Condition check | 5.82 | 0.46 | <0.001 |
| Rounding | 16.38 | 0.71 | <0.001 |
| Consultation with other doctors | 1.27 | 0.24 | <0.001 |
| Consultation with patients | 6.53 | 0.35 | <0.001 |
| Others | 0.10 | 0.05 | 0.035 |
| Medical division | |||
| Internal medicine | |||
| Total | 25.76 | 1.67 | <0.001 |
| Procedure | 1.25 | 0.55 | 0.024 |
| Condition check | 4.39 | 0.46 | <0.001 |
| Rounding | 13.50 | 0.78 | <0.001 |
| Consultation with other doctors | 1.70 | 0.31 | <0.001 |
| Consultation with patients | 4.95 | 0.39 | <0.001 |
| Others | 0.13 | 0.06 | 0.025 |
| Surgery | |||
| Total | 52.42 | 3.63 | <0.001 |
| Procedure | 6.05 | 1.15 | <0.001 |
| Condition check | 10.32 | 1.39 | <0.001 |
| Rounding | 25.42 | 1.63 | <0.001 |
| Consultation with other doctors | −0.04 | 0.03 | 0.165 |
| Consultation with patients | 10.99 | 0.76 | <0.001 |
| Others | −0.02 | 0.06 | 0.717 |
| Region | |||
| Capital area | |||
| Total | 26.62 | 1.64 | <0.001 |
| Procedure | 1.08 | 0.52 | 0.038 |
| Condition check | 4.00 | 0.49 | <0.001 |
| Rounding | 16.06 | 0.88 | <0.001 |
| Consultation with other doctors | 0.14 | 0.20 | 0.4898 |
| Consultation with patients | 5.61 | 0.39 | <0.001 |
| Others | 0.13 | 0.06 | 0.037 |
| Rural area | |||
| Total | 53.35 | 3.78 | <0.001 |
| Procedure | 6.44 | 1.28 | <0.001 |
| Condition check | 11.89 | 1.16 | <0.001 |
| Rounding | 20.44 | 1.13 | <0.001 |
| Consultation with other doctors | 5.41 | 0.81 | <0.001 |
| Consultation with patients | 9.07 | 0.80 | <0.001 |
| Others | 0.00 | 0.01 | 0.608 |
| Variable | Non-Hospitalist | ||
|---|---|---|---|
| OR | 95%CI | p-Value | |
| Exceed 10 mins | 4.14 | (3.15–5.44) | <0.001 |
| Exceed 30 mins | 4.96 | (2.75–8.95) | <0.001 |
| Exceed 60 mins | 5.06 | (1.73–14.78) | 0.003 |
| Exceed 120 mins | 6.07 | (0.66–55.76) | 0.111 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chae, W.; Choi, D.-W.; Park, E.-C.; Jang, S.-I. Improved Inpatient Care through Greater Patient–Doctor Contact under the Hospitalist Management Approach: A Real-Time Assessment. Int. J. Environ. Res. Public Health 2021, 18, 5718. https://doi.org/10.3390/ijerph18115718
Chae W, Choi D-W, Park E-C, Jang S-I. Improved Inpatient Care through Greater Patient–Doctor Contact under the Hospitalist Management Approach: A Real-Time Assessment. International Journal of Environmental Research and Public Health. 2021; 18(11):5718. https://doi.org/10.3390/ijerph18115718
Chicago/Turabian StyleChae, Wonjeong, Dong-Woo Choi, Eun-Cheol Park, and Sung-In Jang. 2021. "Improved Inpatient Care through Greater Patient–Doctor Contact under the Hospitalist Management Approach: A Real-Time Assessment" International Journal of Environmental Research and Public Health 18, no. 11: 5718. https://doi.org/10.3390/ijerph18115718
APA StyleChae, W., Choi, D.-W., Park, E.-C., & Jang, S.-I. (2021). Improved Inpatient Care through Greater Patient–Doctor Contact under the Hospitalist Management Approach: A Real-Time Assessment. International Journal of Environmental Research and Public Health, 18(11), 5718. https://doi.org/10.3390/ijerph18115718








