Maintaining Medical Resources to Treat Paediatric Injuries during COVID-19 Lockdown Is Essential—An Epidemiological Analysis of a Level 1 Trauma Centre in Central Europe
Abstract
1. Introduction
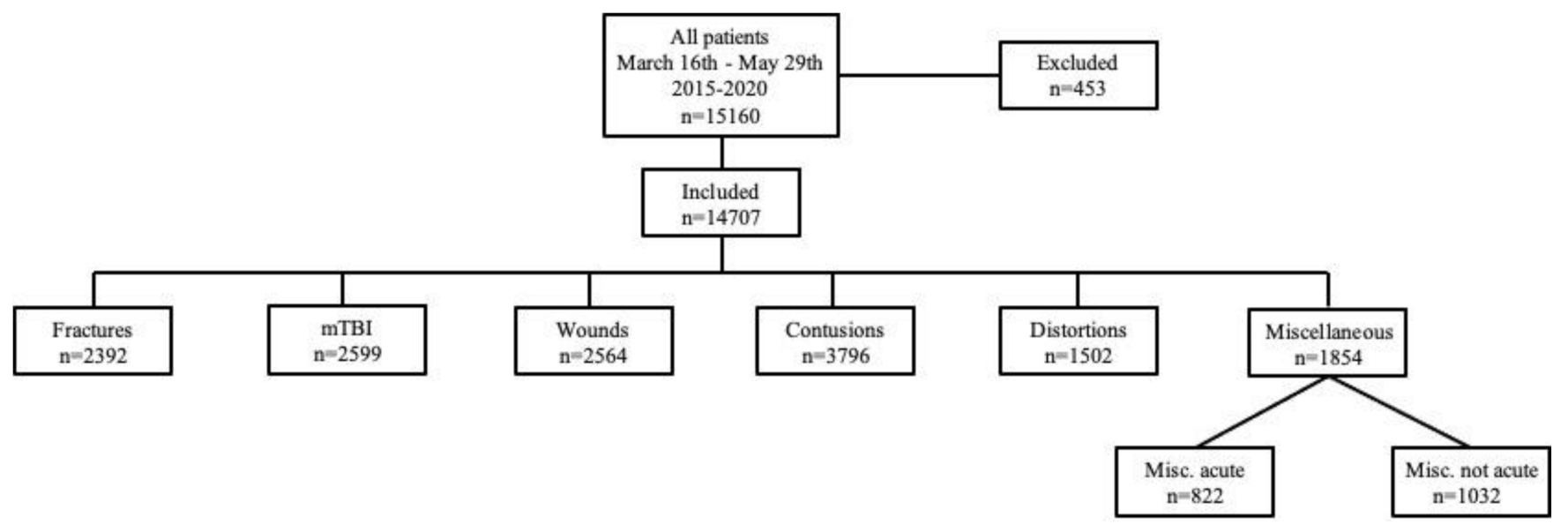
2. Materials and Methods
3. Results
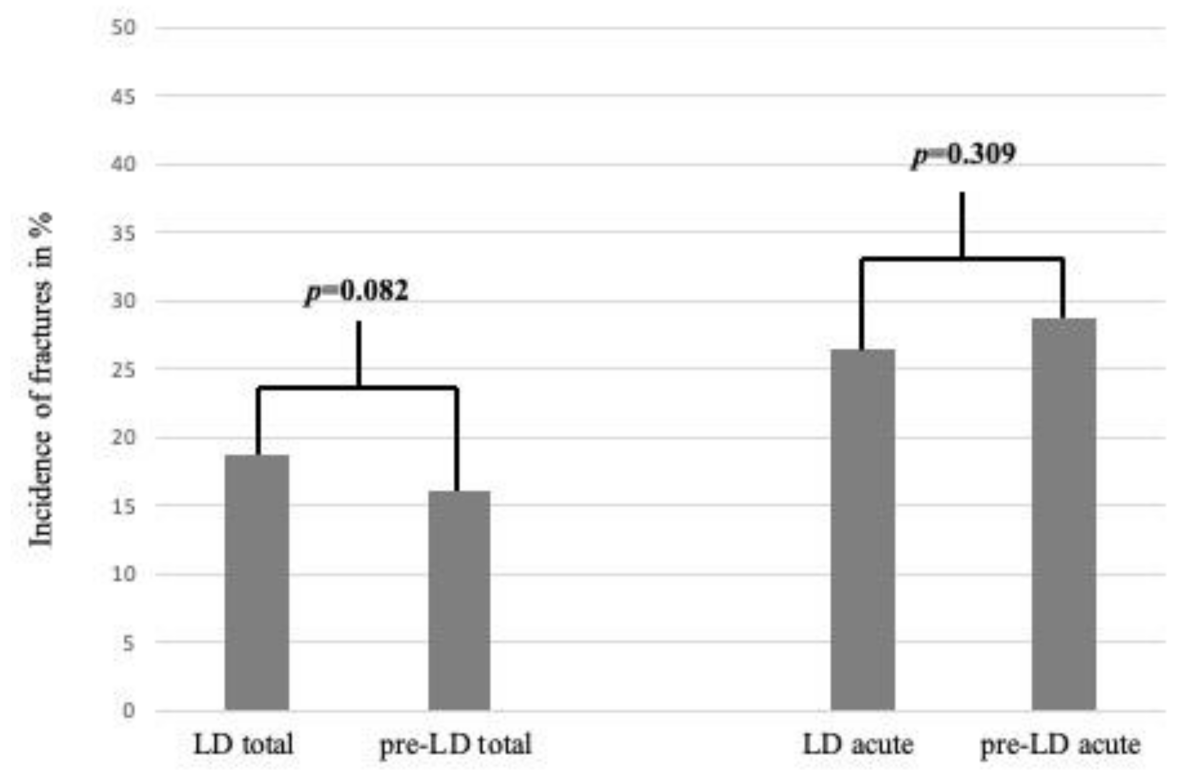
3.1. Fractures during LD vs. the Pre-LD Period
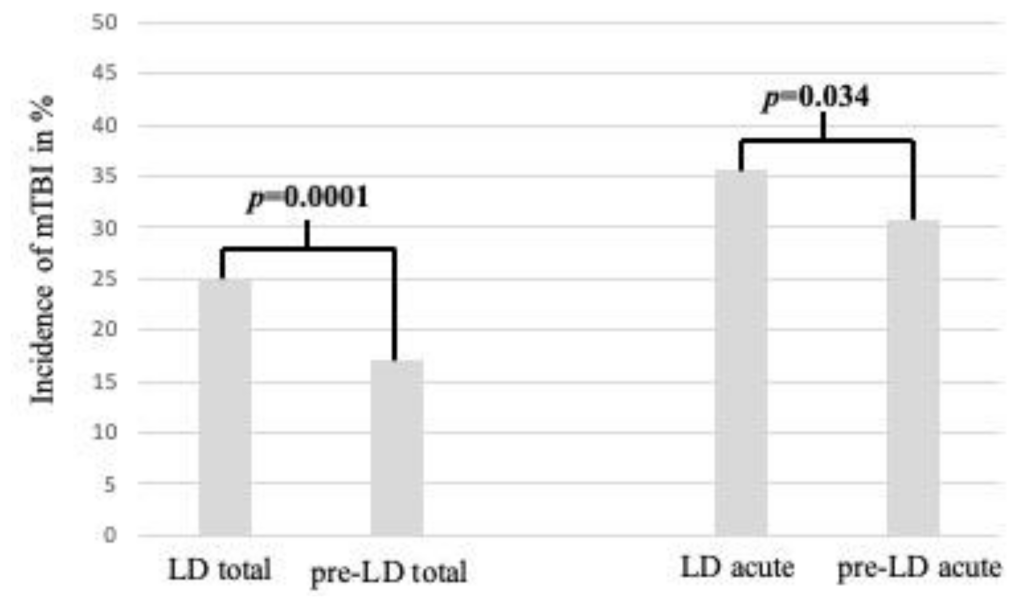
3.2. mTBIs during LD vs. the Pre-LD Era
3.3. Wounds during LD vs. the Pre-LD Era
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bram, J.T.; Johnson, M.A.; Magee, L.C.; Mehta, N.N.; Fazal, F.Z.; Baldwin, K.D.; Riley, J.; Shah, A.S. Where Have All the Fractures Gone? The Epidemiology of Pediatric Fractures During the COVID-19 Pandemic. J. Pediatr. Orthop. 2020, 40, 373–379. [Google Scholar] [CrossRef] [PubMed]
- Federal Ministry of Social Affairs, H. Care and consumer Protection, Verordnung des Bundesministers für Soziales, Gesundheit, Pflege und Konsumentenschutz gemäß § 2 Z 1 des COVID-19-Maßnahmengesetzes; Austrian Government: Vienna, Austria, BGBl. II Nr. 98/2020.
- Pollak, M.; Kowarz, N.; Partheymüller, J. Chronologie zur Corona-Krise in Österreich—Teil 1: Vorgeschichte, der Weg in den Lockdown, die Akute Phase und Wirtschaftliche Folgen. Available online: https://viecer.univie.ac.at/corona-blog/corona-blog-beitraege/blog51/ (accessed on 3 June 2020).
- Pollak, M.K.N.; Partheymüller, J. Chronologie zur Corona-Krise in Österreich—Teil 2: Von den Ersten Lockerungen Hinzu einer Normalisierung des Öffentlichen Lebens. Available online: https://viecer.univie.ac.at/corona-blog/corona-blog-beitraege/blog60/ (accessed on 26 June 2020).
- Keays, G.; Friedman, D.; Gagnon, I. Injuries in the time of COVID-19. Health Promot. Chronic. Dis. Prev. Can. 2020, 40, 336–341. [Google Scholar] [CrossRef]
- Baxter, I.; Hancock, G.; Clark, M.; Hampton, M.; Fishlock, A.; Widnall, J.; Flowers, M.; Evans, O. Paediatric orthopaedics in lockdown: A study on the effect of the SARS-Cov-2 pandemic on acute paediatric orthopaedics and trauma. Bone Joint Open 2020, 1, 424–430. [Google Scholar] [CrossRef] [PubMed]
- Turgut, A.; Arlı, H.; Altundağ, Ü.; Hancıoğlu, S.; Egeli, E.; Kalenderer, Ö. Effect of COVID-19 pandemic on the fracture demographics: Data from a tertiary care hospital in Turkey. Acta Orthop. Traumatol. Turc. 2020, 54, 355–363. [Google Scholar] [CrossRef]
- Hernigou, J.; Morel, X.; Callewier, A.; Bath, O.; Hernigou, P. Staying home during “COVID-19” decreased fractures, but trauma did not quarantine in one hundred and twelve adults and twenty eight children and the “tsunami of recommendations” could not lockdown twelve elective operations. Int. Orthop. 2020, 44, 1473–1480. [Google Scholar] [CrossRef]
- Simma, B.; Lutschg, J.; Callahan, J.M. Mild head injury in pediatrics: Algorithms for management in the ED and in young athletes. Am. J. Emerg. Med. 2013, 31, 1133–1138. [Google Scholar] [CrossRef] [PubMed]
- Buki, A.; Kovacs, N.; Czeiter, E.; Schmid, K.; Berger, R.P.; Kobeissy, F.; Italiano, D.; Hayes, R.L.; Tortella, F.C.; Mezosi, E.; et al. Minor and repetitive head injury. Adv. Tech. Stand. Neurosurg. 2015, 42, 147–192. [Google Scholar] [PubMed]
- Memeo, A.; Priano, D.; Caldarini, C.; Trezza, P.; Laquidara, M.; Montanari, L.; Randell, P. How the pandemic spread of COVID-19 affected children’s traumatology in Italy: Changes of numbers, anatomical locations, and severity. Minerva. Pediatr. 2020. [Google Scholar] [CrossRef]
- Nabian, M.H.; Vosoughi, F.; Najafi, F.; Khabiri, S.S.; Nafisi, M.; Veisi, J.; Rastgou, V.; Ghamari, S.; Aakhashi, A.; Bahrami, N.; et al. Epidemiological pattern of pediatric trauma in COVID-19 outbreak: Data from a tertiary trauma center in Iran. Injury 2020, 51, 2811–2815. [Google Scholar] [CrossRef] [PubMed]
- Raitio, A.; Ahonen, M.; Jääskelä, M.; Jalkanen, J.; Luoto, T.T.; Haara, M.; Nietosvaara, Y.; Salonen, A.; Pakkasjärvi, N.; Laaksonen, T.; et al. Reduced Number of Pediatric Orthopedic Trauma Requiring Operative Treatment during COVID-19 Restrictions: A Nationwide Cohort Study. Scand. J. Surg. 2020. [Google Scholar] [CrossRef] [PubMed]
- Williams, N.; Winters, J.; Cooksey, R. Staying home but not out of trouble: No reduction in presentations to the South Australian paediatric major trauma service despite the COVID-19 pandemic. ANZ J. Surg. 2020, 90, 1863–1864. [Google Scholar] [CrossRef] [PubMed]
- Toniolo-Barrios, M.; Pitt, L. Mindfulness and the challenges of working from home in times of crisis. Bus. Horiz. 2020, 64, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Del Boca, D.; Oggero, N.; Profeta, P.; Rossi, M. Women’s and men’s work, housework and childcare, before and during COVID-19. Rev. Econ. Househ. 2020, 18, 1001–1017. [Google Scholar] [CrossRef] [PubMed]
- Kamins, J.; Giza, C.C. Concussion-Mild Traumatic Brain Injury: Recoverable Injury with Potential for Serious Sequelae. Neurosurg Clin. N. Am. 2016, 27, 441–452. [Google Scholar] [CrossRef] [PubMed]
- Greco, T.; Ferguson, L.; Giza, C.; Prins, M.L. Mechanisms underlying vulnerabilities after repeat mild traumatic brain injuries. Exp. Neurol. 2019, 317, 206–213. [Google Scholar] [CrossRef] [PubMed]
- Gilmartin, S.; Barrett, M.; Bennett, M.; Begley, C.; Chroinin, C.N.; O’Toole, P.; Blackburn, C. The effect of national public health measures on the characteristics of trauma presentations to a busy paediatric emergency service in Ireland: A longitudinal observational study. Ir. J. Med. Sci. 2021, 1–7. [Google Scholar] [CrossRef]
- Sugand, K.; Park, C.; Morgan, C.; Dyke, R.; Aframian, A.; Hulme, A.; Evans, S.; Sarraf, K.M. COVERT Collaborative. Impact of the COVID-19 pandemic on paediatric orthopaedic trauma workload in central London: A multi-centre longitudinal observational study over the “golden weeks”. Acta Orthop. 2020, 91, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Wong, F.L.; Antoniou, G.; Williams, N.; Cundy, P.J. Disruption of paediatric orthopaedic hospital services due to the COVID-19 pandemic in a region with minimal COVID-19 illness. J. Child. Orthop. 2020, 14, 245–251. [Google Scholar] [CrossRef] [PubMed]

| 2020 | n= | % of All Injuries | Male | Male Mean Age ± SD | Female | Female Mean Age ± SD | Total Mean Age ± SD |
|---|---|---|---|---|---|---|---|
| n/% | n/% | ||||||
| Total | 844 | 100 | 480/100% | 6.9 ± 5.9 | 364/100% | 6.7 ± 5.4 | 6.9 ± 5.7 |
| Fractures | 158 | 18.7 | 98/20.4% | 8.3 ± 5.1 | 60/16.5% | 8.1 ± 4.9 | 8.2 ± 5.0 |
| mTBIs | 212 | 25.1 | 126/26.3% | 4.3 ± 5.1 | 86/23.6% | 3.7 ± 4.5 | 4.1 ± 4.8 |
| Wounds | 188 | 22.3 | 115/24.0% | 5.8 ± 4.8 | 73/20.1% | 7.1 ± 5.9 | 6.3 ± 5.3 |
| Contusions | 132 | 15.6 | 66/13.8% | 8.2 ± 5.9 | 66/18.1% | 6.8 ± 5.8 | 8.4 ± 5.8 |
| Distortions | 50 | 5.9 | 25/5.2% | 13.8 ± 3.8 | 25/6.9% | 12.4 ± 4.0 | 13.1 ± 3.9 |
| Miscellaneous | 104 | 12.3 | 50/10.4% | 7.2 ± 6.0 | 54/14.8% | 6.2 ± 5.5 | 6.7 ± 5.8 |
| Miscellaneous acute | 39 | 4.6 | 17/3.5% | 8.6 ± 6.8 | 22/6.0% | 6.9 ± 6.3 | 7.7 ± 6.7 |
| Miscellaneous non-acute | 65 | 7.7 | 33/6.9% | 6.4 ± 5.3 | 32/8.8% | 5.8 ± 4.9 | 6.1 ± 5.1 |
| 2019 | n= | % of All Injuries | Male | Male Mean Age ± SD | Female | Female Mean Age ± SD | Total Mean Age ± SD |
| n/% | n/% | ||||||
| Total | 2736 | 100 | 1555/100% | 8.9 ± 5.7 | 1181/100% | 8.6 ± 5.6 | 8.8 ± 5.6 |
| Fractures | 424 | 15.5 | 247/15.9% | 10.3 ± 4.7 | 177/15.0% | 9.0 ± 4.6 | 9.8 ± 4.7 |
| mTBIs | 514 | 18.8 | 274/17.6% | 5.5 ± 5.4 | 240/20.3% | 5.6 ± 5.5 | 5.5 ± 5.4 |
| Wounds | 440 | 16.1 | 264/17.0% | 6.9 ± 5.4 | 1761/14.9% | 7.2 ± 5.5 | 7.0 ± 5.4 |
| Contusions | 720 | 26.3 | 428/27.5% | 10.1 ± 5.3 | 292/24.7% | 10.7 ± 5.0 | 10.3 ± 5.2 |
| Distortions | 274 | 10 | 147/9.5% | 12.5 ± 4.5 | 127/10.8% | 12.2 ± 4.1 | 12.4 ± 4.3 |
| Miscellaneous | 364 | 13.3 | 195/12.5% | 8.7 ± 5.8 | 169/14.3% | 8.0 ± 5.7 | 8.4 ± 5.8 |
| Miscellaneous acute | 153 | 5.6 | 70/4.5% | 10.3 ± 5.5 | 83/7.0% | 9.4 ± 5.8 | 9.9 ± 5.7 |
| Miscellaneous non-acute | 211 | 7.7 | 125/8.0% | 7.9 ± 5.7 | 86/7.3% | 6.5 ± 5.2 | 7.3 ± 5.6 |
| 2018 | n= | % of All Injuries | Male | Male Mean Age ± SD | Female | Female Mean Age ± SD | Total Mean Age ± SD |
| n/% | n/% | ||||||
| Total | 2684 | 100 | 1530/100% | 8.5 ± 5.6 | 1154/100% | 8.3 ± 5.5 | 8.4 ± 5.5 |
| Fractures | 496 | 18.5 | 294/19.2% | 9.4 ± 4.8 | 202/17.5% | 8.8 ± 4.3 | 9.2 ± 4.6 |
| mTBIs | 464 | 17.3 | 264/17.3% | 5.2 ± 5.0 | 200/17.3% | 4.7 ± 5.1 | 5.0 ± 5.0 |
| Wounds | 438 | 16.3 | 278/18.2% | 7.0 ± 5.3 | 160/13.9% | 7.2 ± 5.5 | 7.1 ± 5.4 |
| Contusions | 652 | 24.3 | 360/23.5% | 9.4 ± 5.2 | 292/25.3% | 9.5 ± 5.1 | 9.5 ± 5.2 |
| Distortions | 286 | 10.7 | 140/9.2% | 12.3 ± 4.9 | 146/12.7% | 12.7 ± 4.2 | 12.5 ± 4.6 |
| Miscellaneous | 348 | 13 | 194/12.7% | 8.9 ± 5.9 | 154/13.3% | 6.9 ± 5.6 | 8.0 ± 5.9 |
| Miscellaneous acute | 154 | 5.7 | 79/5.2% | 12.7 ± 3.9 | 75/6.5% | 12.6 ± 4.0 | 8.9 ± 5.9 |
| Miscellaneous non-acute | 194 | 7.2 | 115/7.5% | 7.9 ± 6.0 | 79/6.8% | 7.5 ± 5.2 | 7.3 ± 5.7 |
| 2017 | n= | % of All Injuries | Male | Male Mean Age ± SD | Female | Female Mean Age ± SD | Total Mean Age ± SD |
| n/% | n/% | ||||||
| Total | 2778 | 100 | 1641/100% | 9.1 ± 5.5 | 1137/100% | 8.4 ± 5.7 | 8.8 ± 5.6 |
| Fractures | 466 | 16.8 | 305/18.6% | 10.4 ± 4.6 | 161/14.2% | 8.5 ± 4.3 | 9.7 ± 4.6 |
| mTBIs | 495 | 17.8 | 288/17.6% | 5.8 ± 5.4 | 207/18.2% | 4.7 ± 5.2 | 5.3 ± 5.3 |
| Wounds | 439 | 15.8 | 278/16.9% | 7.4 ± 5.6 | 161/14.2% | 6.6 ± 5.4 | 7.1 ± 5.5 |
| Contusions | 757 | 27.3 | 439/26.8% | 10.3 ± 5.0 | 318/28.0% | 9.4 ± 5.4 | 9.9 ± 5.2 |
| Distortions | 289 | 10.4 | 149/9.1% | 12.5 ± 4.4 | 140/12.3% | 12.9 ± 4.0 | 12.7 ± 4.2 |
| Miscellaneous | 332 | 12 | 182/11.1% | 9.4 ± 5.8 | 150/13.2% | 8.7 ± 6.0 | 9.0 ± 5.9 |
| Miscellaneous acute | 173 | 6.2 | 94/5.7% | 10.5 ± 5.4 | 79/6.9% | 9.2 ± 5.8 | 9.9 ± 5.7 |
| Miscellaneous non-acute | 159 | 5.7 | 88/5.4% | 8.3 ± 5.8 | 71/6.2% | 8.0 ± 6.0 | 8.2 ± 5.9 |
| 2016 | n= | % of All Injuries | Male | Male Mean Age ± SD | Female | Female Mean Age ± SD | Total Mean Age ± SD |
| n/% | n/% | ||||||
| Total | 2931 | 100 | 1697/100% | 9.4 ± 5.6 | 1234/100% | 8.5 ± 5.6 | 9.0 ± 5.6 |
| Fractures | 442 | 15.1 | 283/16.7% | 10.9 ± 4.4 | 159/12.9% | 8.9 ± 4.6 | 10.2 ± 4.6 |
| mTBIs | 498 | 17 | 274/16.1% | 6.0 ± 5.4 | 224/18.2% | 5.5 ± 5.4 | 5.8 ± 5.4 |
| Wounds | 499 | 17 | 309/18.2% | 6.6 ± 5.4 | 190/15.4% | 6.5 ± 5.3 | 6.6 ± 5.3 |
| Contusions | 787 | 26.9 | 451/26.6% | 10.7 ± 5.2 | 336/27.2% | 9.7 ± 5.3 | 10.2 ± 5.5 |
| Distortions | 355 | 12.1 | 192/11.3% | 13.0 ± 4.1 | 163/13.2% | 12.0 ± 4.2 | 12.6 ± 4.2 |
| Miscellaneous | 350 | 11.9 | 188/11.1% | 9.8 ± 5.7 | 162/13.1% | 8.4 ± 6.0 | 9.2 ± 5.9 |
| Miscellaneous acute | 153 | 5.2 | 85/5.0% | 10.1 ± 6.0 | 68/5.5% | 9.5 ± 5.4 | 9.8 ± 5.8 |
| Miscellaneous non-acute | 197 | 6.7 | 103/6.1% | 9.7 ± 5.3 | 94/7.6% | 7.5 ± 6.2 | 8.7 ± 5.9 |
| 2015 | n= | % of All Injuries | Male | Male Mean Age ± SD | Female | Female Mean Age ± SD | Total Mean Age ± SD |
| n/% | n/% | ||||||
| Total | 2734 | 100 | 1554/100% | 9.1 ± 5.6 | 1180/100% | 8.7 ± 5.8 | 8.9 ± 5.7 |
| Fractures | 406 | 14.9 | 257/16.5% | 10.4 ± 4.8 | 149/12.6% | 10.2 ± 4.4 | 10.3 ± 4.6 |
| mTBIs | 416 | 15.2 | 230/14.8% | 5.7 ± 5.5 | 186/15.8% | 5.4 ± 5.7 | 5.6 ± 5.6 |
| Wounds | 560 | 20.5 | 334/21.5% | 7.1 ± 5.5 | 226/19.2% | 8.4 ± 6.0 | 7.6 ± 5.7 |
| Contusions | 748 | 27.4 | 418/26.9% | 10.1 ± 5.1 | 330/28.0% | 9.6 ± 5.5 | 9.9 ± 5.3 |
| Distortions | 248 | 9.1 | 131/8.4% | 12.5 ± 4.5 | 117/9.9% | 12.1 ± 4.6 | 12.3 ± 4.6 |
| Miscellaneous | 356 | 13 | 184/11.8% | 10.1 ± 5.9 | 172/14.6% | 8.9 ± 6.0 | 9.6 ± 6.0 |
| Miscellaneous acute | 150 | 5.5 | 69/4.4% | 11.1 ± 5.5 | 81/6.9% | 9.1 ± 6.1 | 10.0 ± 5.9 |
| Miscellaneous non-acute | 206 | 7.5 | 115/7.4% | 9.5 ± 6.1 | 91/7.7% | 8.7 ± 5.8 | 9.2 ± 6.0 |
| Average of Pre-LD Period (2015–2019) | n= | % of All Injuries | LD Era | n= | % of All Injuries | p-Value | p-Value (Compared to Only Acute Injuries) |
|---|---|---|---|---|---|---|---|
| Total | 2773 | 100 | Total | 844 | 100 | ||
| Fractures | 447 | 16.2 | Fractures | 158 | 18.7 | 0.082 | 0.309 |
| mTBIs | 477 | 17.2 | mTBIs | 212 | 25.1 | 0.0001 | 0.034 |
| Wounds | 475 | 17.1 | Wounds | 188 | 22.3 | 0.0009 | 0.0001 |
| Contusions | 733 | 26.4 | Contusions | 132 | 15.6 | 0.0001 | - |
| Distortions | 290 | 10.5 | Distortions | 50 | 5.9 | 0.0001 | - |
| Miscellaneous | 350 | 12.6 | Miscellaneous | 104 | 12.3 | 0.858 | - |
| Miscellaneous acute | 157 | 5.6 | Miscellaneous acute | 39 | 4.6 | - | - |
| Miscellaneous non-acute | 967 | 7.0 | Miscellaneous non-acute | 65 | 7.7 | - | - |
| Fractures in LD (2020) | Total | m/f | Op | m/f | Conservatively | m/f |
|---|---|---|---|---|---|---|
| 158 | 97/61 | 23/14.6% | 13/10 | 135/85.4% | 84/51 | |
| Upper Extremity | 116/73.4% | 72/44 | 20/17.2% | 11/9 | 96/82.8% | 61/35 |
| Lower Extremity | 30/19% | 16/14 | 3/10% | 2/1 | 27/90% | 14/13 |
| Axial Skeleton | 12/7.6% | 9/3 | 0 | -/- | 12 | 9/3 |
| Fractures Pre-LD (2015–2019) | Total | m/f | Op | m/f | Conservatively | m/f |
|---|---|---|---|---|---|---|
| 447 | 277/170 | 46/10.3% | 30/15 | 401/89.7% | 247/154 | |
| Upper Extremity | 314/70.2% | 199/115 | 37/11.8% | 25/12 | 277/88.2% | 174/103 |
| Lower Extremity | 110/24.6% | 63/47 | 8/7.3% | 5/3 | 102/92.7% | 58/44 |
| Axial Skeleton | 23/5.1% | 16/7 | 1/4.3% | -/- | 22/95.7% | 15/7 |
| mTBIs | m/f | |
|---|---|---|
| LD (2020) | 212 | 126/86 |
| Pre-LD (2015–2019) | 477 | 266/211 |
| Wounds | Total | Laceration (of the Head n= and in %) | Bite (Human/Animal) | Cut | Amputation | Skin Defect | Stab | Op/Conservative Wound Management | m/f | Mean Age |
|---|---|---|---|---|---|---|---|---|---|---|
| LD (2020) | 188 | 130 (123; 94.6%) | 6 (3/3) | 37 | 1 | 3 | 11 | 7/181 | 115/73 | 6.3 ± 5.3 |
| Mean Pre-LD (2015–19) | 475 | 327 (283, 86.4%) | 34(6/23) | 83 | 1 | 7 | 27 | 8/467 | 292/182 | 7.1 ± 5.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Payr, S.; Schuller, A.; Dangl, T.; Scheider, P.; Sator, T.; Chocholka, B.; Jaindl, M.; Schwendenwein, E.; Tiefenboeck, T.M. Maintaining Medical Resources to Treat Paediatric Injuries during COVID-19 Lockdown Is Essential—An Epidemiological Analysis of a Level 1 Trauma Centre in Central Europe. Int. J. Environ. Res. Public Health 2021, 18, 5829. https://doi.org/10.3390/ijerph18115829
Payr S, Schuller A, Dangl T, Scheider P, Sator T, Chocholka B, Jaindl M, Schwendenwein E, Tiefenboeck TM. Maintaining Medical Resources to Treat Paediatric Injuries during COVID-19 Lockdown Is Essential—An Epidemiological Analysis of a Level 1 Trauma Centre in Central Europe. International Journal of Environmental Research and Public Health. 2021; 18(11):5829. https://doi.org/10.3390/ijerph18115829
Chicago/Turabian StylePayr, Stephan, Andrea Schuller, Theresia Dangl, Philipp Scheider, Thomas Sator, Britta Chocholka, Manuela Jaindl, Elisabeth Schwendenwein, and Thomas M. Tiefenboeck. 2021. "Maintaining Medical Resources to Treat Paediatric Injuries during COVID-19 Lockdown Is Essential—An Epidemiological Analysis of a Level 1 Trauma Centre in Central Europe" International Journal of Environmental Research and Public Health 18, no. 11: 5829. https://doi.org/10.3390/ijerph18115829
APA StylePayr, S., Schuller, A., Dangl, T., Scheider, P., Sator, T., Chocholka, B., Jaindl, M., Schwendenwein, E., & Tiefenboeck, T. M. (2021). Maintaining Medical Resources to Treat Paediatric Injuries during COVID-19 Lockdown Is Essential—An Epidemiological Analysis of a Level 1 Trauma Centre in Central Europe. International Journal of Environmental Research and Public Health, 18(11), 5829. https://doi.org/10.3390/ijerph18115829








