A Space-Time Analysis of Rural Older People’s Outdoor Mobility and Its Impact on Self-Rated Health: Evidence from a Taiwanese Rural Village
Abstract
:1. Introduction
2. Literature Review
2.1. Rural Built Environment and Older People
2.2. Older People’s Mobility and Its Association with Self-Rated Health
2.3. Space-Time Path for Understanding Mobility
3. Methods
3.1. Location and Participants
3.2. Measure Tools
3.2.1. Basic Demographic Characteristics Data Sheet
3.2.2. Short Portable Mental Status Questionnaire (SPMSQ)
3.2.3. GPS Tracking
3.2.4. The Medical Outcomes Study 36-Item Short-Form (SF-36)
3.2.5. In-Depth Interviews
3.3. Variables
3.3.1. Dependent Variable: Self-Rated Health (SRH)
3.3.2. Independent Variables: Distance, Time, and Space of Mobility
3.4. Analysis
4. Results and Discussion
4.1. Space-Time Path of Older People and Health
“Every day, I will go to a mobile vendor to buy fresh vegetables or daily necessities. After my first recovery from a serious illness, my mental health was greatly affected by my husband’s physical disability. I often felt depressed, lost and unable to lift my spirits. After the introduction of my neighbors, I would take time for volunteer service or to have a meal with other elders in the community development association within a week, hoping to improve my mental state.”
“I like to exercise under the viaduct, because it’s convenient to go there, and it’s shade, not afraid of the sun and rain, and the space is long enough for walking. My friends also like to exercise there. Every day we can meet and chat there.”
“At present, the circular footpath and integrated park are under construction in Zhutian middle school, hoping to meet the lack of sports and rest space in the village. After all, we are all older. Every day, when we think of cycling for a distance before we can get under the viaduct, we sometimes feel too lazy to do it.”
“There is no traditional market or fresh supermarket in the village. I don’t think it’s convenient to buy vegetables and daily necessities. Many fresh fruits and vegetables need to be bought in the markets of Neipu Township in the East, Chaozhou Town in the South and Pingtung city in the north. I need to travel a long distance to these places, so it is often my son’s daughter-in-law who lives in a nearby village who takes me to the market to buy them together, and then carries the grandson who has just finished class back to my son’s home to cook and eat dinner together.”
“My son lives in the next village. He moved out when he was 16. At that time, the next village opened a new factory and the salaries are very attractive. That’s why he decided to leave, although he did not wish to... Now I often go to their home to help them cook and look after their children.”
4.2. The Relationship between Mobility and Self-Rated Health
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Global Strategy and Action Plan on Ageing and Health; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Ministry of Interior. The Yearly Statistics of Ministry of Interior. Available online: https://www.moi.gov.tw/files/site_stuff/321/2/year/year.html (accessed on 3 April 2020).
- Chen, L.-K.; Inoue, H.; Won, C.-W.; Lin, C.-H.; Lin, K.-F.; Tsay, S.-F.; Lin, P.-F.; Li, S.-H. Challenges of urban aging in Taiwan: Summary of urban aging forum. J. Clin. Gerontol. Geriatr. 2013, 4, 97–101. [Google Scholar] [CrossRef] [Green Version]
- Lin, Y.-Y.; Huang, C.-S. Aging in Taiwan: Building a Society for Active Aging and Aging in Place. Gerontologist 2015, 56, 176–183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- UNECE. Older Persons in Rural and Remote Areas. UNECE Policy Brief on Ageing No. 18. 2017. Available online: https://unece.org/policy-briefs.html (accessed on 3 April 2020).
- Li, L.W.; Liu, J.; Xu, H.; Zhang, Z. Understanding rural–urban differences in depressive symptoms among older adults in China. J. Aging Health 2016, 28, 341–362. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, P.C.; Yen, M.; Fetzer, S.J. Quality of life in elders living alone in Taiwan. J. Clin. Nurs. 2008, 17, 1610–1617. [Google Scholar] [CrossRef]
- Wang, J.-J.; Snyder, M.; Kaas, M. Stress, loneliness, and depression in Taiwanese rural community-dwelling elders. Int. J. Nurs. Stud. 2001, 38, 339–347. [Google Scholar] [CrossRef]
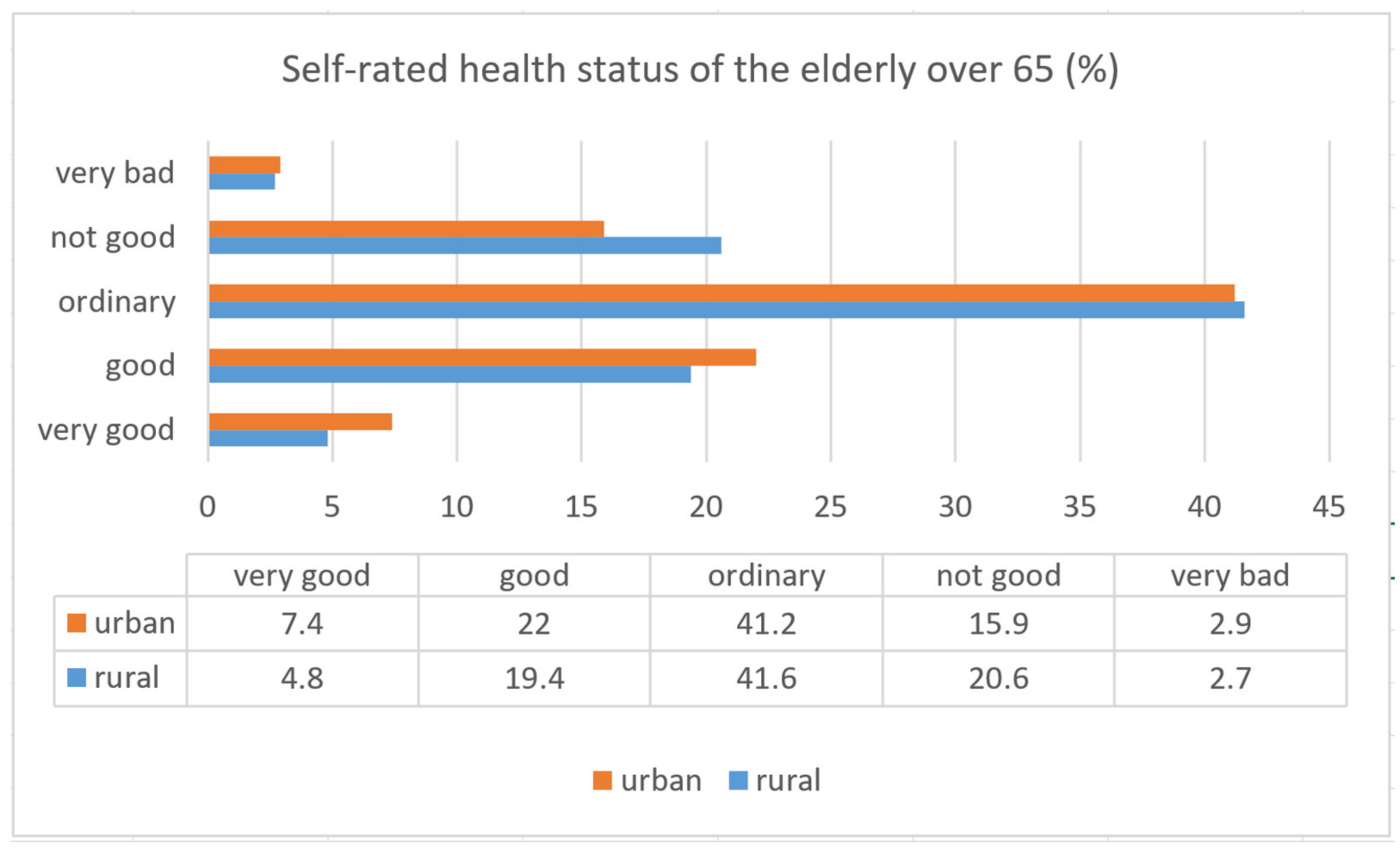
- National Health Interview Report 2013 Released by Taiwan Health Promotion Administration, Ministry of Health and Welfare. Available online: https://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=364&pid=6543 (accessed on 1 January 2020).
- Cuignet, T.; Perchoux, C.; Caruso, G.; Klein, O.; Klein, S.; Chaix, B.; Kestens, Y.; Gerber, P. Mobility among older adults: Deconstructing the effects of motility and movement on wellbeing. Urban Stud. 2020, 57, 383–401. [Google Scholar] [CrossRef]
- Franke, T.; Sims-Gould, J.; Chaudhury, H.; Winters, M.; McKay, H. ‘It makes your life worthwhile. It gives you a purpose in living’: Mobility experiences among active older adults with low income. Ageing Soc. 2019, 39, 1639–1666. [Google Scholar] [CrossRef]
- Goins, R.T.; Jones, J.; Schure, M.; Rosenberg, D.E.; Phelan, E.A.; Dodson, S.; Jones, D.L. Older adults’ perceptions of mobility: A metasynthesis of qualitative studies. Gerontologist 2015, 55, 929–942. [Google Scholar] [CrossRef]
- Litwin, H.; Levinson, M. The association of mobility limitation and social networks in relation to late-life activity. Ageing Soc. 2018, 38, 1771–1790. [Google Scholar] [CrossRef]
- Meijering, L. Towards meaningful mobility: A research agenda for movement within and between places in later life. Ageing Soc. 2021, 41, 711–723. [Google Scholar] [CrossRef] [Green Version]
- Ng, S.T.; Tengku-Aizan, H.; Tey, N.P. Perceived health status and daily activity participation of older Malaysians. Asia Pac. J. Public Health 2011, 23, 470–484. [Google Scholar] [CrossRef]
- Haustein, S.; Siren, A. Older people’s mobility: Segments, factors, trends. Transp. Rev. 2015, 35, 466–487. [Google Scholar] [CrossRef] [Green Version]
- Aird, R.L.; Buys, L. Active aging: Exploration into self-ratings of “being active,” out-of-home physical activity, and participation among older Australian adults living in four different settings. J. Aging Res. 2015, 2015. [Google Scholar] [CrossRef] [Green Version]
- Curl, A.; Thompson, C.W.; Alves, S.; Aspinall, P. Outdoor environmental supportiveness and older people’s quality of life: A personal projects approach. J. Hous. Elder. 2016, 30, 1–17. [Google Scholar] [CrossRef] [Green Version]
- Levasseur, M.; Généreux, M.; Bruneau, J.-F.; Vanasse, A.; Chabot, É.; Beaulac, C.; Bédard, M.-M. Importance of proximity to resources, social support, transportation and neighborhood security for mobility and social participation in older adults: Results from a scoping study. BMC Public Health 2015, 15, 1–19. [Google Scholar] [CrossRef] [Green Version]
- Lin, T.; Sakuno, S. Successful aging and leisure environment: A comparative study of urban and rural areas in Taiwan. Waseda J. Sport Sci. 2012, 9, 1–16. [Google Scholar]
- Wei, H.-C.; Tsai, L.-Y. Evaluation of a Senior-Friendly Traffic Environment in the Suburban Areas. J. Gerontechnol. Serv. Manag. 2017, 5, 191–205. [Google Scholar] [CrossRef]
- Yu, L.Z. The relationship between different leisure environments and successful aging on the elderly. Master’s Thesis, Institute of Sports and Leisure Management, National Taiwan Normal University, Taipei, Taiwan, 2009. [Google Scholar]
- Golant, S.M. Explaining the ageing in place realities of older adults. In Geographical Gerontology; Routledge: New York, NY, USA, 2017; pp. 189–202. [Google Scholar]
- Sun, Y.; Phillips, D.R.; Wong, M. A study of housing typology and perceived age-friendliness in an established Hong Kong new town: A person-environment perspective. Geoforum 2018, 88, 17–27. [Google Scholar] [CrossRef]
- Gardner, P. The role of social engagement and identity in community mobility among older adults aging in place. Disabil. Rehabil. 2014, 36, 1249–1257. [Google Scholar] [CrossRef]
- Elshof, H.; Haartsen, T.; van Wissen, L.J.; Mulder, C.H. The influence of village attractiveness on flows of movers in a declining rural region. J. Rural. Stud. 2017, 56, 39–52. [Google Scholar] [CrossRef] [Green Version]
- Vidickienė, D. Attractiveness of rural areas for young, educated women in post-industrial society. East. Eur. Countrys. 2017, 171–190. [Google Scholar] [CrossRef] [Green Version]
- Schröder, L.; Flägel, K.; Goetz, K.; Steinhäuser, J. Mobility concepts and access to health care in a rural district in Germany: A mixed methods approach. BMC Fam. Pract. 2018, 19, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Chen, H.; Liu, Y.; Zhu, Z.; Li, Z. Does where you live matter to your health? Investigating factors that influence the self-rated health of urban and rural Chinese residents: Evidence drawn from Chinese general social survey data. Health Qual. Life Outcomes 2017, 15, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Camarero, L.; Oliva, J. Thinking in rural gap: Mobility and social inequalities. Palgrave Commun. 2019, 5, 1–7. [Google Scholar] [CrossRef]
- Clarke, P.; Twardzik, E. The role of the built environment for healthy aging: Barriers and enablers. In Handbook of Aging and the Social Sciences; Elsevier: Amsterdam, The Netherlands, 2021; pp. 115–130. [Google Scholar]
- Choi, Y.J. Age-friendly features in home and community and the self-reported health and functional limitation of older adults: The role of supportive environments. J. Urban Health 2020, 97, 471–485. [Google Scholar] [CrossRef]
- Rantanen, T.; Portegijs, E.; Viljanen, A.; Eronen, J.; Saajanaho, M.; Tsai, L.-T.; Kauppinen, M.; Palonen, E.-M.; Sipilä, S.; Iwarsson, S. Individual and environmental factors underlying life space of older people–study protocol and design of a cohort study on life-space mobility in old age (LISPE). BMC Public Health 2012, 12, 1–17. [Google Scholar] [CrossRef] [Green Version]
- Rantanen, T. Promoting mobility in older people. J. Prev. Med. Public Health 2013, 46, S50. [Google Scholar] [CrossRef]
- Carver, L.F.; Beamish, R.; Phillips, S.P.; Villeneuve, M. A scoping review: Social participation as a cornerstone of successful aging in place among rural older adults. Geriatrics 2018, 3, 75. [Google Scholar] [CrossRef] [Green Version]
- Lawton, M.P. The elderly in context: Perspectives from environmental psychology and gerontology. Environ. Behav. 1985, 17, 501–519. [Google Scholar] [CrossRef]
- Kahana, E.; Kahana, B.; Lee, J.E. Proactive approaches to successful aging: One clear path through the forest. Gerontology 2014, 60, 466–474. [Google Scholar] [CrossRef] [Green Version]
- Portegijs, E.; Iwarsson, S.; Rantakokko, M.; Viljanen, A.; Rantanen, T. Life-space mobility assessment in older people in Finland; measurement properties in winter and spring. BMC Res. Notes 2014, 7, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Siltanen, S.; Rantanen, T.; Portegijs, E.; Tourunen, A.; Poranen-Clark, T.; Eronen, J.; Saajanaho, M. Association of tenacious goal pursuit and flexible goal adjustment with out-of-home mobility among community-dwelling older people. Aging Clin. Exp. Res. 2019, 31, 1249–1256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Skantz, H.; Rantanen, T.; Palmberg, L.; Rantalainen, T.; Aartolahti, E.; Portegijs, E.; Viljanen, A.; Eronen, J.; Rantakokko, M. Outdoor mobility and use of adaptive or maladaptive walking modifications among older people. J. Gerontol. Ser. A 2020, 75, 806–812. [Google Scholar] [CrossRef] [Green Version]
- Fillekes, M.P.; Kim, E.-K.; Trumpf, R.; Zijlstra, W.; Giannouli, E.; Weibel, R. Assessing Older Adults’ Daily Mobility: A Comparison of GPS-Derived and Self-Reported Mobility Indicators. Sensors 2019, 19, 4551. [Google Scholar] [CrossRef] [Green Version]
- Nordbakke, S.; Schwanen, T. Well-being and mobility: A theoretical framework and literature review focusing on older people. Mobilities 2014, 9, 104–129. [Google Scholar] [CrossRef]
- World Health Organization. Global Age-Friendly Cities: A Guide; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Stjernborg, V. The meaning of social participation for daily mobility in later life: An ethnographic case study of a senior project in a Swedish urban neighbourhood. Ageing Int. 2017, 42, 374–391. [Google Scholar] [CrossRef] [Green Version]
- Zeitler, E.; Buys, L. Mobility and out-of-home activities of older people living in suburban environments: ‘Because I’m a driver, I don’t have a problem’. Ageing Soc. 2015, 35, 785–808. [Google Scholar] [CrossRef] [Green Version]
- Webber, S.C.; Porter, M.M.; Menec, V.H. Mobility in older adults: A comprehensive framework. Gerontologist 2010, 50, 443–450. [Google Scholar] [CrossRef] [Green Version]
- Hjorthol, R.J.; Levin, L.; Sirén, A. Mobility in different generations of older persons: The development of daily travel in different cohorts in Denmark, Norway and Sweden. J. Transp. Geogr. 2010, 18, 624–633. [Google Scholar] [CrossRef]
- Lin, Y.-H.; Chen, H.-C.; Hsu, N.-W.; Chou, P. Validation of Global Self-Rated Health and Happiness Measures Among Older People in the Yilan Study, Taiwan. Front. Public Health 2020, 8. [Google Scholar] [CrossRef]
- Pérez-Zepeda, M.U.; Belanger, E.; Zunzunegui, M.V.; Phillips, S.; Ylli, A.; Guralnik, J. Assessing the validity of self-rated health with the short physical performance battery: A cross-sectional analysis of the international mobility in aging study. PLoS ONE 2016, 11, e0153855. [Google Scholar] [CrossRef] [PubMed]
- Hanibuchi, T.; Nakaya, T.; Murata, C. Socio-economic status and self-rated health in East Asia: A comparison of China, Japan, South Korea and Taiwan. Eur. J. Public Health 2012, 22, 47–52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Y.; Nima, Q.; Yu, B.; Xiao, X.; Zeng, P.; Suolang, D.; He, R.; Ciren, Z.; Wangqing, P.; Laba, C. Determinants of self-rated health among an older Tibetan population in a Chinese plateau area: Analysis based on the conceptual framework for determinants of health. BMC Public Health 2021, 21, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Cachioni, M.; Cipolli, G.C.; Borim, F.S.A.; Batistoni, S.S.T.; Yassuda, M.S.; Neri, A.L.; Paúl, C. Factors Associated With Positive Self-Rated Health: Comparing Older Adults in Brazil and in Portugal. Front. Public Health 2021, 9, 258. [Google Scholar]
- Fjell, A.; Berit, S.C.; Hermann, M.; Rongve, A.; Aßmus, J.; Kvinge, L.; Seiger, Å.; Skaug, K.; Boström, A.-M. Factors associated with self-rated health in a Norwegian population of older people participating in a preventive home visit program: A cross-sectional study. BMC Geriatr. 2020, 20, 1–12. [Google Scholar] [CrossRef]
- Portegijs, E.; Rantakokko, M.; Mikkola, T.M.; Viljanen, A.; Rantanen, T. Association between physical performance and sense of autonomy in outdoor activities and life-space mobility in community-dwelling older people. J. Am. Geriatr. Soc. 2014, 62, 615–621. [Google Scholar] [CrossRef] [Green Version]
- Reigal, R.E.; Páez-Maldonado, J.A.; Pastrana-Brincones, J.L.; Morillo-Baro, J.P.; Hernández-Mendo, A.; Morales-Sánchez, V. Physical Activity Is Related to Mood States, Anxiety State and Self-Rated Health in COVID-19 Lockdown. Sustainability 2021, 13, 5444. [Google Scholar] [CrossRef]
- Jylhä, M.; Guralnik, J.M.; Balfour, J.; Fried, L.P. Walking difficulty, walking speed, and age as predictors of self-rated health: The women’s health and aging study. J. Gerontol. Ser. A Biol. Sci. Med Sci. 2001, 56, M609–M617. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.; Schneider, T.; Faß, E.; Lochbaum, M. Personal social capital and self-rated health among middle-aged and older adults: A cross-sectional study exploring the roles of leisure-time physical activity and socioeconomic status. BMC Public Health 2021, 21, 1–11. [Google Scholar] [CrossRef]
- Laukkanen, P.; Heikkinen, E.; Kauppinen, M. Muscle strength and mobility as predictors of survival in 75–84-year-old people. Age Ageing 1995, 24, 468–473. [Google Scholar] [CrossRef]
- Rappe, E.; Kivelä, S.-L.; Rita, H. Visiting outdoor green environments positively impacts self-rated health among older people in long-term care. HortTechnology 2006, 16, 55–59. [Google Scholar] [CrossRef] [Green Version]
- Sperlich, S.; Beller, J.; Epping, J.; Tetzlaff, J.; Geyer, S. Trends in self-rated health among the elderly population in Germany from 1995 to 2015–the influence of temporal change in leisure time physical activity. BMC Public Health 2020, 20, 113. [Google Scholar] [CrossRef] [PubMed]
- Xu, D.; Arling, G.; Wang, K. A cross-sectional study of self-rated health among older adults: A comparison of China and the United States. BMJ Open 2019, 9, e027895. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hagerstrand, T. What about People in Regional Science? In Papers and Proceedings of the Regional Science Association; Springer: Berlin/Heidelberg, Germany, 1970. [Google Scholar]
- Miller, H.J. Activities in space and time. In Handbook of Transport Geography and Spatial Systems; Emerald Group Publishing Limited: Bingley, UK, 2004. [Google Scholar]
- Miller, H.J. Time Geography and Space–Time Prism. In International Encyclopedia of Geography: People, the Earth, Environment and Technology; Wiley: Hoboken, NJ, USA, 2016; pp. 1–19. [Google Scholar]
- Chai, Y.; Chen, Z. Towards mobility turn in urban planning: Smart travel planning based on space-time behavior in Beijing, China. In Big Data Support of Urban Planning and Management; Springer: Berlin/Heidelberg, Germany, 2018; pp. 319–337. [Google Scholar]
- Roberts, H.; Helbich, M. Multiple environmental exposures along daily mobility paths and depressive symptoms: A smartphone-based tracking study. Environ. Int. 2021, 156, 106635. [Google Scholar] [CrossRef]
- Fillekes, M.P.; Giannouli, E.; Kim, E.-K.; Zijlstra, W.; Weibel, R. Towards a comprehensive set of GPS-based indicators reflecting the multidimensional nature of daily mobility for applications in health and aging research. Int. J. Health Geogr. 2019, 18, 1–20. [Google Scholar] [CrossRef] [Green Version]
- Bayat, S.; Naglie, G.; Rapoport, M.J.; Stasiulis, E.; Widener, M.J.; Mihailidis, A. A GPS-Based Framework for Understanding Outdoor Mobility Patterns of Older Adults with Dementia: An Exploratory Study. Gerontology 2021, 1–15. [Google Scholar] [CrossRef]
- Franke, T.; Winters, M.; McKay, H.; Chaudhury, H.; Sims-Gould, J. A grounded visualization approach to explore sociospatial and temporal complexities of older adults’ mobility. Soc. Sci. Med. 2017, 193, 59–69. [Google Scholar] [CrossRef]
- Schmidt, T.; Kerr, J.; Kestens, Y.; Schipperijn, J. Challenges in using wearable GPS devices in low-income older adults: Can map-based interviews help with assessments of mobility? Transl. Behav. Med. 2019, 9, 99–109. [Google Scholar] [CrossRef]
- Clarke, P.; Gallagher, N.A. Optimizing mobility in later life: The role of the urban built environment for older adults aging in place. J. Urban Health 2013, 90, 997–1009. [Google Scholar] [CrossRef] [Green Version]
- Frantál, B.; Klapka, P.; Nováková, E. When home becomes a cage: Daily activities, space-time constraints, isolation and the loneliness of older adults in urban environments. Morav. Geogr. Rep. 2020, 28, 322–337. [Google Scholar]
- Hirsch, J.A.; Winters, M.; Clarke, P.; McKay, H. Generating GPS activity spaces that shed light upon the mobility habits of older adults: A descriptive analysis. Int. J. Health Geogr. 2014, 13, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Khanal, A.; Edwards, E.C.; Corcoran, J. Walking behaviours in older adults: A GPS-based survey in Brisbane. In Proceedings of the Australasian Transport Research Forum (ATRF), 41st, 2019, Canberra, ACT, Australia, 30 September–2 October 2019. [Google Scholar]
- McDowell, I. Measuring Health: A Guide to Rating Scales and Questionnaires; Oxford University Press: New York, NY, USA, 2006. [Google Scholar]
- Ware, J.; Snoww, K.; Ma, K.; Bg, G. SF36 Health Survey: Manual and Interpretation Guide. Linc. RI Qual. Metr. Inc. 1993, 1993, 30. [Google Scholar]
- Ware, J.E. Improvements in short-form measures of health status: Introduction to a series. J. Clin. Epidemiol. 2008, 61, 1–5. [Google Scholar] [CrossRef]
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med. Care 1992, 473–483. [Google Scholar] [CrossRef]
- Lam, C.L.; Eileen, Y.; Gandek, B.; Fong, D.Y. The SF-36 summary scales were valid, reliable, and equivalent in a Chinese population. J. Clin. Epidemiol. 2005, 58, 815–822. [Google Scholar] [CrossRef] [Green Version]
- Lefever, D.W. Measuring geographic concentration by means of the standard deviational ellipse. Am. J. Sociol. 1926, 32, 88–94. [Google Scholar] [CrossRef]
- Sherman, J.E.; Spencer, J.; Preisser, J.S.; Gesler, W.M.; Arcury, T.A. A suite of methods for representing activity space in a healthcare accessibility study. Int. J. Health Geogr. 2005, 4, 1–21. [Google Scholar] [CrossRef] [Green Version]
- York Cornwell, E.; Cagney, K.A. Aging in activity space: Results from smartphone-based GPS-tracking of urban seniors. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2017, 72, 864–875. [Google Scholar] [CrossRef]
- Yuill, R.S. The standard deviational ellipse; an updated tool for spatial description. Geogr. Ann. Ser. B Hum. Geogr. 1971, 53, 28–39. [Google Scholar] [CrossRef]
- Benyamini, Y.; Blumstein, T.; Lusky, A.; Modan, B. Gender differences in the self-rated health–mortality association: Is it poor self-rated health that predicts mortality or excellent self-rated health that predicts survival? Gerontologist 2003, 43, 396–405. [Google Scholar] [CrossRef] [Green Version]
- Deeg, D.J.H.; Kriegsman, D.M.W. Concepts of Self-Rated Health: Specifying the Gender Difference in Mortality Risk. Gerontologist 2003, 43, 376–386. [Google Scholar] [CrossRef] [Green Version]
- Lyyra, T.-M.; Leskinen, E.; Jylhä, M.; Heikkinen, E. Self-rated health and mortality in older men and women: A time-dependent covariate analysis. Arch. Gerontol. Geriatr. 2009, 48, 14–18. [Google Scholar] [CrossRef]
- Mossey, J.M.; Shapiro, E. Self-rated health: A predictor of mortality among the elderly. Am. J. Public Health 1982, 72, 800–808. [Google Scholar] [CrossRef] [Green Version]
- Soytas, M.A.; Kose, T. Gender Differences in Self) Reported Health Status: Cross) country Evidence from Turkey and the United States. Job Mark. Pap. 2014, 11, 1–30. [Google Scholar]
- Rantakokko, M.; Portegijs, E.; Viljanen, A.; Iwarsson, S.; Kauppinen, M.; Rantanen, T. Changes in life-space mobility and quality of life among community-dwelling older people: A 2-year follow-up study. Qual. Life Res. 2016, 25, 1189–1197. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.; Myers, O. Using GPS-based wearable sensors to capture life-space mobility among community-dwelling older adults. Innov. Aging 2019, 3, S371. [Google Scholar]
- Mardini, M.T.; Nerella, S.; Kheirkhahan, M.; Ranka, S.; Fillingim, R.B.; Hu, Y.; Corbett, D.B.; Cenko, E.; Weber, E.; Rashidi, P. The Temporal Relationship Between Ecological Pain and Life-Space Mobility in Older Adults With Knee Osteoarthritis: A Smartwatch-Based Demonstration Study. JMIR mHealth uHealth 2021, 9, e19609. [Google Scholar] [CrossRef]






| Gender | 65% Female |
|---|---|
| Age | Mean: 67.5 years, SD: 5.8 years Range: 55–74 |
| Marital status | Married: 80% Widowed: 20% |
| Highest level of education attained | Primary: 20%, Secondary school: 20%, High school: 60%, |
| Means of transport | Bicycle: 5% Motorcycle: 70% Automobile: 25% |
| Statistical Value | Mean ± Standard Deviation | Mean ± Standard Deviation (Male) | Mean ± Standard Deviation (Female) |
|---|---|---|---|
| physical functioning, PF | 79.75 ± 14.09 | 86.43 ± 7.48 | 90.71 ± 9.32 |
| role-physical, RP | 68.75 ± 17.91 | 75.00 ± 0.00 | 65.38 ± 21.74 |
| bodily pain, BP | 80.00 ± 17.66 | 94.00 ± 0.00 | 72.46 ± 17.84 |
| general health, GH | 71.25 ± 20.25 | 90.71 ± 9.32 | 60.77 ± 16.31 |
| validity, VT | 81.50 ± 15.31 | 92.86 ± 2.67 | 75.38 ± 15.87 |
| social function, SF | 82.50 ± 7.48 | 85.71 ± 4.72 | 80.77 ± 8.25 |
| role-emotion, RE | 70.00 ± 10.26 | 76.19 ± 16.27 | 66.67 ± 0.00 |
| mental health, MH | 75.20 ± 16.75 | 85.14 ± 3.80 | 69.85 ± 18.66 |
| Physical Component Summary, PCS | 74.94 ± 12.99 | 86.54 ± 1.89 | 68.69 ± 12.02 |
| Mental Component Summary, MCS | 77.30 ± 9.51 | 84.98 ± 2.88 | 73.17 ± 9.29 |
| Statistical Value | Average Value | Standard Deviation | Maximum | Minimum Value |
|---|---|---|---|---|
| Average daily standard deviation elliptical area (Km2) | 9.77 | 13.40 | 59.2395 | 0.1512 |
| Average daily moving distance (Km) | 10.84 | 11.35 | 37.19 | 0.45 |
| Average daily outing time (hours) | 4.77 | 2.65 | 10.3 | 1.3 |
| Statistical Value | Average Value | Category (I) | Category (II) | Category (III) |
|---|---|---|---|---|
| PCS | 74.94 | 62.58 | 78.88 | 80.78 |
| MCS | 77.30 | 70.85 | 76.76 | 81.38 |
| Average daily standard deviation elliptical area (Km2) | 9.77 | 0.94 | 4.25 | 17.27 |
| Average daily moving distance (Km) | 10.84 | 2.90 | 6.19 | 17.48 |
| Average daily outing time (hours) | 4.77 | 2.37 | 3.53 | 6.70 |
| PCS | MCS | Average Daily Standard Deviation Elliptical Area | Average Daily Moving Distance | Average Daily Outing Time | ||
|---|---|---|---|---|---|---|
| PCS | Pearson Correlation | 1.000 | 0.897 ** | 0.480 * | 0.369 | 0.450 * |
| Sig. (two-tailed) | 0.000 | 0.032 | 0.110 | 0.047 | ||
| N | 20 | 20 | 20 | 20 | 20 | |
| MCS | Pearson Correlation | 0.897 ** | 1.000 | 0.524 * | 0.556 ** | 0.538 ** |
| Sig. (two-tailed) | 0.000 | 0.018 | 0.011 | 0.014 | ||
| N | 20 | 20 | 20 | 20 | 20 | |
| Average daily standard deviation elliptical area | Pearson Correlation | 0.480 * | 0.524 * | 1.000 | 0.700 ** | 0.797 ** |
| Sig. (two-tailed) | 0.032 | 0.018 | 0.001 | 0.000 | ||
| N | 20 | 20 | 20 | 20 | 20 | |
| Average daily moving distance | Pearson Correlation | 0.369 | 0.556 ** | 0.700 ** | 1.000 | 0.754 ** |
| Sig. (two-tailed) | 0.110 | 0.011 | 0.001 | 0.000 | ||
| N | 20 | 20 | 20 | 20 | 20 | |
| Average daily outing time | Pearson Correlation | 0.450 * | 0.538 ** | 0.797 ** | 0.754 ** | 1.000 |
| Sig. (two-tailed) | 0.047 | 0.014 | 0.000 | 0.000 | ||
| N | 20 | 20 | 20 | 20 | 20 | |
| PCS | MCS | Age | Education Level | ||
|---|---|---|---|---|---|
| PCS | Pearson Correlation | 1.000 | 0.897 * | 0.353 | −0.137 |
| Sig. (two-tailed) | 0.000 | 0.127 | 0.564 | ||
| N | 20 | 20 | 20 | 20 | |
| MCS | Pearson Correlation | 0.897 * | 1.000 | 0.251 | −0.166 |
| Sig. (two-tailed) | 0.000 | 0.286 | 0.483 | ||
| N | 20 | 20 | 20 | 20 | |
| Age | Pearson Correlation | 0.353 | 0.251 | 1.000 | −0.619 * |
| Sig. (two-tailed) | 0.127 | 0.286 | 0.004 | ||
| N | 20 | 20 | 20 | 20 | |
| Education level | Pearson Correlation | −0.137 | −0.166 | −0.619 * | 1.000 |
| Sig. (two-tailed) | 0.564 | 0.483 | 0.004 | ||
| N | 20 | 20 | 20 | 20 | |
| Gender | N | Mean | Std. Dev. | Std. Err. | |
|---|---|---|---|---|---|
| PCS | male female | 7 13 | 86.71 68.85 | 1.890 12.020 | 0.714 3.334 |
| MCS | male female | 7 13 | 84.71 73.15 | 2.812 9.371 | 1.063 2.599 |
| Levene’s Test for Equality of Variances | t-Test for Equality of Means | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| F | Sig. | T | df | Sig. (2-tailed) | Mean Difference | Std. Error Difference | 95%Confidence Interval of the Difference | |||
| Lower | Upper | |||||||||
| PCS | Equal variances assumed Equal variances not assumed | 10.767 | 0.004 | 3.860 5.241 | 18 13.072 | 0.001 0.000 | 17.868 17.868 | 4.629 3.409 | 8.142 10.507 | 27.594 25.229 |
| MCS | Equal variances assumed Equal variances not assumed | 14.173 | 0.001 | 3.153 4.117 | 18 15.482 | 0.006 0.001 | 11.560 11.560 | 3.667 2.808 | 3.857 5.592 | 19.264 17.529 |
| Marital Status | N | Mean | Std. Dev. | Std. Err. | |
|---|---|---|---|---|---|
| Average daily moving distance (km) | married widowed | 16 4 | 12.686 3.478 | 11.953 3.249 | 0.2.988 1.624 |
| Average daily outing time (hour) | married widowed | 16 4 | 5.363 2.375 | 2.626 0.763 | 0.656 0.381 |
| Average daily standard deviation elliptical area (Km2) | married widowed | 16 4 | 11.718 3.4775 | 14.382 1.376 | 3.596 0.688 |
| Levene’s Test for Equality of Variances | t-Test for Equality of Means | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| F | Sig. | T | df | Sig. (2-tailed) | Mean Difference | Std. Error Difference | 95% Confidence Interval of the Difference | |||
| Lower | Upper | |||||||||
| Average daily moving distance (km) | Equal variances assumed Equal variances not assumed | 5.756 | 0.027 | 1.499 2.708 | 18 17.524 | 0.151 0.015 | 9.209 9.209 | 6.145 3.401 | −3.700 2.049 | 22.118 16.368 |
| Average daily outing time (hour) | Equal variances assumed Equal variances not assumed | 3.458 | 0.079 | 2.211 3.935 | 18 17.092 | 0.040 0.001 | 2.988 2.988 | 1.351 0.759 | 0.149 1.386 | 5.826 4.589 |
| Average daily standard deviation elliptical area (Km2) | Equal variances assumed Equal variances not assumed | 2.001 | 0.174 | 1.328 2.665 | 18 16.012 | 0.201 0.017 | 9.758 9.758 | 7.346 3.661 | −5.676 1.997 | 25.191 17.518 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chao, T.S.; Jiang, X.; Sun, Y.; Yu, J.-Z. A Space-Time Analysis of Rural Older People’s Outdoor Mobility and Its Impact on Self-Rated Health: Evidence from a Taiwanese Rural Village. Int. J. Environ. Res. Public Health 2021, 18, 5902. https://doi.org/10.3390/ijerph18115902
Chao TS, Jiang X, Sun Y, Yu J-Z. A Space-Time Analysis of Rural Older People’s Outdoor Mobility and Its Impact on Self-Rated Health: Evidence from a Taiwanese Rural Village. International Journal of Environmental Research and Public Health. 2021; 18(11):5902. https://doi.org/10.3390/ijerph18115902
Chicago/Turabian StyleChao, Tzuyuan Stessa, Xiaoqin Jiang, Yi Sun, and Jheng-Ze Yu. 2021. "A Space-Time Analysis of Rural Older People’s Outdoor Mobility and Its Impact on Self-Rated Health: Evidence from a Taiwanese Rural Village" International Journal of Environmental Research and Public Health 18, no. 11: 5902. https://doi.org/10.3390/ijerph18115902
APA StyleChao, T. S., Jiang, X., Sun, Y., & Yu, J.-Z. (2021). A Space-Time Analysis of Rural Older People’s Outdoor Mobility and Its Impact on Self-Rated Health: Evidence from a Taiwanese Rural Village. International Journal of Environmental Research and Public Health, 18(11), 5902. https://doi.org/10.3390/ijerph18115902






