Hybrid Tele and In-Clinic Occupation Based Intervention to Improve Women’s Daily Participation after Breast Cancer: A Pilot Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
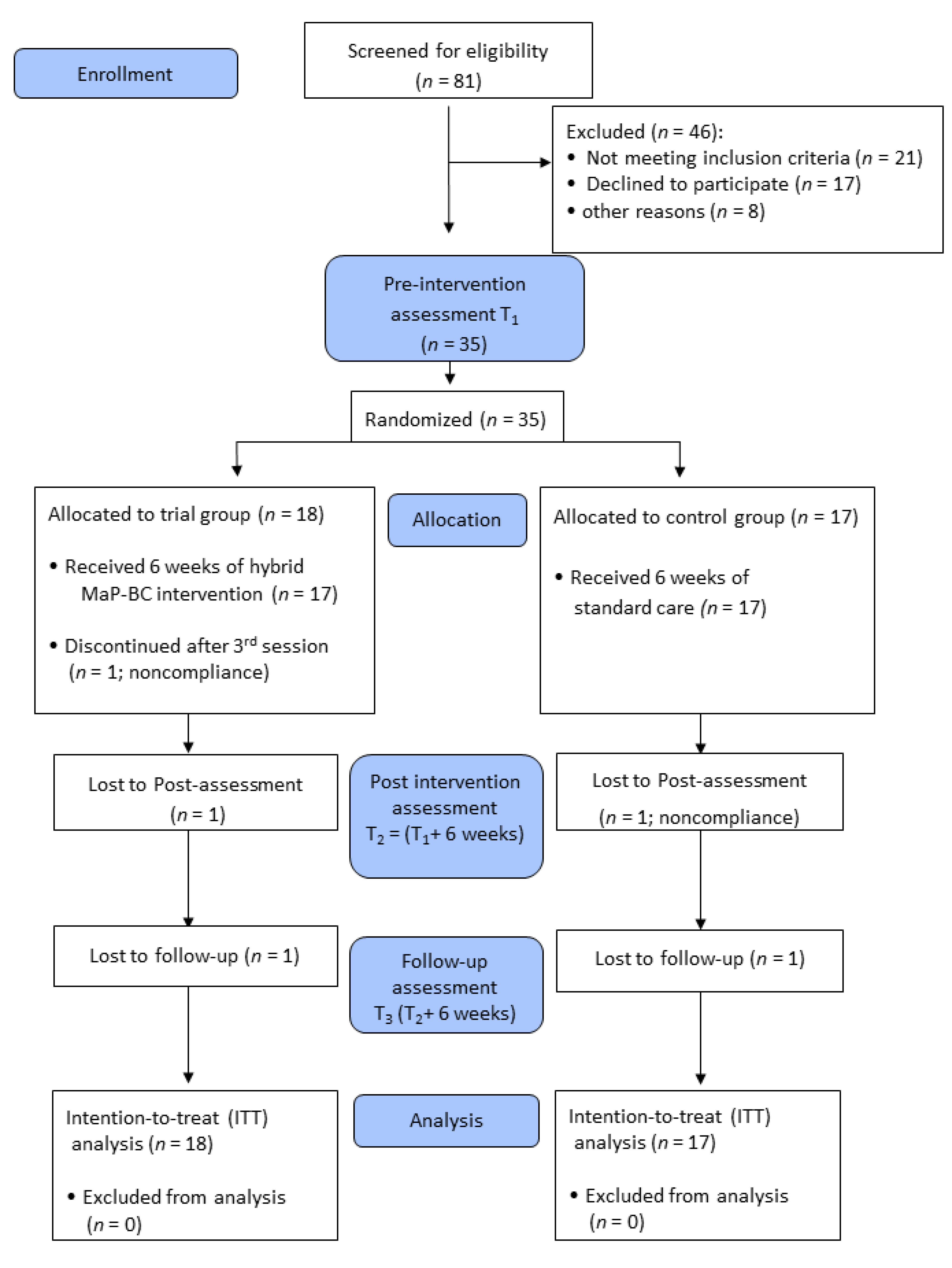
2.1. Participants
2.2. Procedure
MAP-BC Intervention
2.3. Measures
2.3.1. Primary Outcome
Canadian Occupational Performance Measure
2.3.2. Secondary Outcomes
Activity Card Sort
Disability of Arm, Shoulder, and Hand: Quick Version
Hydraulic Hand Dynamometer
Montreal Cognitive Assessment
Behavior Rating Inventory of Executive Function: Adult Version
Functional Assessment of Cancer Therapy-Breast
2.4. Statistical Analysis
3. Results
3.1. Primary Outcome
Participation in Meaningful Daily Activities (COPM)
3.2. Secondary Outcomes
4. Discussion
4.1. Study Limitations
4.2. Study Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Week | Session Type | Goals | Content and Examples |
|---|---|---|---|
| 1 | Clinic |
|
|
| Tele |
|
| |
| 2 | Clinic |
|
|
| Tele |
|
| |
| 3–5 | Clinic |
|
|
| Tele |
|
| |
| 6 | Tele |
| |
| Clinic |
|
|
References
- Runowicz, C.; Leach, C.; Lynn-Henry, N. American Cancer Society/American Society of Clinical oncology breast cancer sur-vivorship care guideline. CA Cancer J. Clin. 2016, 66, 43–73. [Google Scholar] [CrossRef]
- Keesing, S.; Rosenwax, L.; McNamara, B. Identifying the contribution of occupational therapy in meeting the needs of women survivors of breast cancer. Br. J. Occup. Ther. 2018, 81, 402–412. [Google Scholar] [CrossRef]
- Loubani-Hawaita, K.; Schreuer, N.; Milman, U. Participation in Daily Activities among Working Women Following Breast Cancer. Open J. Ther. Rehabil. 2016, 4, 150–162. [Google Scholar] [CrossRef] [Green Version]
- Von Blanckenburg, P.; Seifart, U.; Conrad, N.; Exner, C.; Rief, W.; Nestoriuc, Y. Quality of life in cancer rehabilitation: The role of life goal adjustment. Psycho-Oncology 2014, 23, 1149–1156. [Google Scholar] [CrossRef] [PubMed]
- Sleight, A.G.; Duker, L.I.S. Toward a Broader Role for Occupational Therapy in Supportive Oncology Care. Am. J. Occup. Ther. 2016, 70, 7004360030. [Google Scholar] [CrossRef] [Green Version]
- Eakman, A.M.; Eklund, M. The Relative Impact of Personality Traits, Meaningful Occupation and Occupational Value on Meaning in Life and Life Satisfaction. J. Occup. Sci. 2012, 19, 165–177. [Google Scholar] [CrossRef]
- Hack, T.F.; Kwan, W.B.; Thomas-MacLean, R.L.; Towers, A.; Miedema, B.; Tilley, A.; Chateau, D. Predictors of arm morbidity following breast cancer surgery. Psycho-Oncology 2010, 19, 1205–1212. [Google Scholar] [CrossRef]
- Nelson, C.J.; Nandy, N.; Roth, A.J. Chemotherapy and cognitive deficits: Mechanisms, findings, and potential interventions. Palliat. Support. Care 2007, 5, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Selamat, M.H.; Loh, S.Y.; MacKenzie, L.; Vardy, J. Chemobrain Experienced by Breast Cancer Survivors: A Meta-Ethnography Study Investigating Research and Care Implications. PLoS ONE 2014, 9, e108002. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsaras, K.; Papathanasiou, I.V.; Mitsi, D.; Veneti, A.; Kelesi, M.; Zyga, S.; Fradelos, E.C. Assessment of depression and anxiety in breast cancer patients: Prevalence and associated factors. Asian Pac. J. Cancer Prev. 2018, 19, 1661. [Google Scholar] [PubMed]
- Campbell-Enns, H.J.; Woodgate, R.L. The psychosocial experiences of women with breast cancer across the lifespan: A systematic review. Psycho-Oncology 2017, 26, 1711–1721. [Google Scholar] [CrossRef] [PubMed]
- Yuen, H.K.; Gibson, R.W.; Yau, M.K.; Mitcham, M.D. Actions and personal attributes of community-dwelling older adults to maintain independence. Phys. Occup. Ther. Geriatr. 2007, 25, 35–53. [Google Scholar] [CrossRef]
- Penttinen, H.M.; Saarto, T.; Kellokumpu-Lehtinen, P.; Blomqvist, C.; Huovinen, R.; Kautiainen, H.; Järvenpää, S.; Nikander, R.; Idman, I.; Luoto, R.; et al. Quality of life and physical performance and activity of breast cancer patients after adjuvant treatments. Psycho-Oncology 2011, 20, 1211–1220. [Google Scholar] [CrossRef] [PubMed]
- Pergolotti, M.; Williams, G.; Campbell, C.; Munoz, L.A.; Muss, H.B. Occupational Therapy for Adults with Cancer: Why It Matters. Oncologist 2016, 21, 314–319. [Google Scholar] [CrossRef] [Green Version]
- Kielhofner, G. Model of Human Occupation: Theory and Application, 4th ed.; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2008. [Google Scholar]
- Baxter, M.F.; Newman, R.; Longpré, S.M.; Polo, K.M. Occupational Therapy’s Role in Cancer Survivorship as a Chronic Condition. Am. J. Occup. Ther. 2017, 71, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Hegel, M.T.; Lyons, K.D.; Hull, J.G.; Kaufman, P.; Urquhart, L.; Li, Z.; Ahles, T.A. Feasibility study of a randomized controlled trial of a telephone-delivered problem-solving-occupational therapy intervention to reduce participation restrictions in rural breast cancer survivors undergoing chemotherapy. Psycho-Oncology 2011, 20, 1092–1101. [Google Scholar] [CrossRef] [Green Version]
- Loubani, K.; Schreuer, N.; Kizony, R. Participation in Daily Activities among Women Five Years Following Breast cancer. Am. J. Occup. Ther. 2021, 76. In Press. [Google Scholar]
- Loring, K.R.; Holman, H.R. Self-management education: History, definition, outcomes, and mechanisms. Ann. Behav. Med. 2003, 26, 1–7. [Google Scholar] [CrossRef]
- Nolte, E. Implementing person centred approaches. BMJ 2017, 358, j4126. [Google Scholar] [CrossRef]
- Gebbia, V.; Borsellino, N.; Ferraù, F.; Verderame, F.; Butera, A.; Giuffrida, D.; Tralongo, P. Cancer patient-centered home care: A new model for health care in oncology. Ther. Clin. Risk Manag. 2011, 7, 387–392. [Google Scholar] [CrossRef] [Green Version]
- Lyons, K.D.; Svensborn, I.A.; Kornblith, A.B.; Hegel, M.T. A Content Analysis of Functional Recovery Strategies of Breast Cancer Survivors. Occup. Particip. Health 2015, 35, 73–80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Newman, R.; Lyons, K.D.; Coster, W.J.; Wong, J.; Festa, K.; Ko, N.Y. Feasibility, acceptability and potential effectiveness of an occupation-focused cognitive self-management program for breast cancer survivors. Br. J. Occup. Ther. 2019, 82, 604–611. [Google Scholar] [CrossRef]
- Jakobsen, K.; Magnus, E.; Lundgren, S.; Reidunsdatter, R.J. Everyday life in breast cancer survivors experiencing challenges: A qualitative study. Scand. J. Occup. Ther. 2018, 25, 298–307. [Google Scholar] [CrossRef] [PubMed]
- Cole, M.; Tufano, R. Applied Theories in Occupational Therapy: A Practical Approach; Slack: Thorofare, NJ, USA, 2008. [Google Scholar]
- Toglia, J.P. The dynamic interactional model and the metacontext approach. In Cognition, Occupation and Participation across the Life Span, 4th ed.; Katz, N., Toglia, J., Eds.; AOTA Press: Bethessda, MD, USA, 2018; pp. 355–385. [Google Scholar]
- Rogante, M.; Grigioni, M.; Cordella, D.; Giacomozzi, C. Ten years of telerehabilitation: A literature overview of technologies and clinical applications. Neurorehabilition 2010, 27, 287–304. [Google Scholar] [CrossRef] [PubMed]
- Brennan, D.; Tindall, L.; Theodoros, D.; Brown, J.; Campbell, M.; Christiana, D.; Smith, D.; Cason, J.; Lee, A. A Blueprint for Telerehabilitation Guidelines. Int. J. Telerehabil. 2010, 2, 31–34. [Google Scholar] [CrossRef] [Green Version]
- Dart, E.H.; Whipple, H.M.; Pasqua, J.L.; Furlow, C.M. Chapter 13—Legal, Regulatory, and Ethical Issues in Telehealth Tech-nology. In Computer-Assisted and Web-Based Innovations in Psychology, Special Education, and Health; Luiselli, J.K., Fischer, A.J., Eds.; Academic Press: San Diego, CA, USA, 2016; pp. 339–363. [Google Scholar]
- Kizony, R.; Weiss, P.L.; Harel, S.; Feldman, Y.; Obuhov, A.; Zeilig, G.; Shani, M. Tele-rehabilitation service delivery journey from prototype to robust in-home use. Disabil. Rehabil. 2017, 39, 1532–1540. [Google Scholar] [CrossRef]
- Lambert, G.; Alos, N.; Bernier, P.; Laverdière, C.; Drummond, K.; Dahan-Oliel, N.; Lemay, M.; Veilleux, L.N.; Kairy, D. Patient and Parent Experiences with Group Telerehabilitation for Child Survivors of Acute Lymphoblastic Leukemia. Int. J. Environ. Res. Public Health 2021, 18, 3610. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [Green Version]
- Kizony, R.; Weiss, P.L.; Feldman, Y.; Shani, M.; Elion, O.; Harel, S.; Baum-Cohen, I. Evaluation of a Tele-Health System for upper extremity stroke rehabilitation. In Proceedings of the 2013 International Conference on Virtual Rehabilitation (ICVR), Philadelphia, PA, USA, 26–29 August 2013. [Google Scholar]
- Law, M.; Baptiste, S.; McColl, M.; Opzoomer, A.; Polatajko, H.; Pollock, N. The Canadian occupational performance measure: An outcome measure for occupational therapy. Can. J. Occup. Ther. 1990, 57, 82–87. [Google Scholar] [CrossRef]
- Carswell, A.; McColl, M.A.; Baptiste, S.; Law, M.; Polatajko, H.; Pollock, N. The Canadian Occupational Performance Measure: A Research and Clinical Literature Review. Can. J. Occup. Ther. 2004, 71, 210–222. [Google Scholar] [CrossRef]
- Eyssen, I.C.; Steultjens, M.P.M.; Oud, T.A.M.; Bolt, E.M.; Maasdam, A.; Dekker, J. Responsiveness of the Canadian Occupational Performance Measure. J. Rehabil. Res. Dev. 2011, 48, 517–528. [Google Scholar] [CrossRef]
- Sturkenboom, I.H.W.; Graff, M.J.L.; Hendriks, J.C.M.; Veenhuizen, Y.; Munneke, M.; Bloem, B.R. Efficacy of occupational therapy for patients with Parkinson’s disease: A randomised controlled trial. Lancet Neurol. 2014, 13, 557–566. [Google Scholar] [CrossRef]
- Baum, C.; Edwards, D. Activity Card Sort (ACS); Washington University School of Medicine: St. Louis, MO, USA, 2001. [Google Scholar]
- Katz, N.; Hartman-Maeir, A. The Activity Card Sort; Slack Inc.: Thorofare, NJ, USA, 2001. [Google Scholar]
- Sachs, D.; Josman, N. The Activity Card Sort: A Factor Analysis. OTJR 2003, 23, 165–174. [Google Scholar] [CrossRef]
- Institute for Work & Health. Quick Disability of Arm Shoulder—Quick DASH; 400 University Avenue, Suite 1800: Toronto, ON, Canada, 1996. [Google Scholar]
- Leblanc, M.; Stineman, M.; DeMichele, A.; Stricker, C.; Mao, J.J. Validation of QuickDASH Outcome Measure in Breast Cancer Survivors for Upper Extremity Disability. Arch. Phys. Med. Rehabil. 2014, 95, 493–498. [Google Scholar] [CrossRef] [Green Version]
- Mathiowetz, V.; Weber, K.; Volland, G.; Kashman, N. Reliability and validity of grip and pinch strength evaluations. J. Hand Surg. 1984, 9, 222–226. [Google Scholar] [CrossRef]
- Savva, C.; Giakas, G.; Efstathiou, M.; Karagiannis, C. Test-Retest Reliability of Handgrip Strength Measurement Using a Hydraulic Hand Dynamometer in Patients with Cervical Radiculopathy. J. Manip. Physiol. Ther. 2014, 37, 206–210. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I. The Montreal Cognitive Assessment (MOCA): A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Baxter, M.F.; Dulworth, A.N.; Smith, T.M. Identification of Mild Cognitive Impairments in Cancer Survivors. Occup. Ther. Health Care 2011, 25, 26–37. [Google Scholar] [CrossRef]
- Roth, R.M.; Gioia, G.A. Behavior Rating Inventory of Executive Function—Adult Version; Psychological Assessment Resources: Lutz, FL, USA, 2005. [Google Scholar]
- Brady, M.J.; Cella, D.F.; Mo, F.; Bonomi, A.E.; Tulsky, D.S.; Lloyd, S.R.; Deasy, S.; Cobleigh, M.; Shiomoto, G. Reliability and validity of the Functional Assessment of Cancer Therapy-Breast quality-of-life instrument. J. Clin. Oncol. 1997, 15, 974–986. [Google Scholar] [CrossRef] [PubMed]
- Hahn, E.A.; Segawa, E.; Kaiser, K.; Cella, D.; Smith, B.D. Health-related quality of life among women with ductal carcinomain situor early invasive breast cancer: Validation of the FACT-B (version 4). Expert Rev. Qual. Life Cancer Care 2016, 1, 99–109. [Google Scholar] [CrossRef] [Green Version]
- Brody, T. Clinical Trials: Study Design, Endpoints and Biomarkers, Drug Safety, and FDA and ICH Guidelines; Academic Press: London, UK, 2016. [Google Scholar]
- Fritz, C.O.; Morris, P.E.; Richler, J.J. “Effect size estimates: Current use, calculations, and interpretation”: Correction to Fritz et al. J. Exp. Psychol. Gen. 2012, 141, 30. [Google Scholar] [CrossRef]
- Miles, J.; Shevlin, M. Applying Regression and Correlation: A Guide for Students and Researchers; SAGE: Thousand Oaks, CA, USA, 2001. [Google Scholar]
- Lahart, I.M.; Metsios, G.S.; Nevill, A.M.; Carmichael, A.R. Physical activity for women with breast cancer after adjuvant therapy. Cochrane Database Syst. Rev. 2018, 1, CD011292. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Speck, R.M.; DeMichele, A.; Farrar, J.T.; Hennessy, S.; Mao, J.J.; Stineman, M.G.; Barg, F.K. Scope of symptoms and self-management strategies for chemotherapy-induced peripheral neuropathy in breast cancer patients. Support. Care Cancer 2012, 20, 2433–2439. [Google Scholar] [CrossRef] [PubMed]
- Nijjar, S.K.; D’Amico, M.I.; Wimalaweera, N.A.; Cooper, N.; Zamora, J.; Khan, K.S. Participation in clinical trials improves outcomes in women’s health: A systematic review and meta-analysis. BJOG 2017, 124, 863–871. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Belvis, A.G.; Ferre, F.; Specchia, M.L.; Valerio, L.; Fattore, G.; Ricciardi, W. The financial crisis in Italy: Implications for the healthcare sector. Health Policy 2012, 106, 10–16. [Google Scholar] [CrossRef] [PubMed]
| Variable | Intervention Group (n = 18) | Control Group (n = 17) | Between-Group Comparison | |||
|---|---|---|---|---|---|---|
| M (SD) | Range | M (SD) | Range | t | df | |
| Age (years) | 48.00 (11.14) | 28–69 | 52.06 (12.80) | 31–64 | −1.00 | 33.0 |
| Education (years) | 15.06 (1.92) | 12–17 | 13.94 (2.28) | 11–17 | 1.57 | 33.0 |
| Months since diagnosis | 14.56 (5.54) | 5–25 | 11.24 (3.17) | 6–17 | 2.19 * | 27.3 |
| n (%) | n (%) | χ2 | df | |||
| Marital status | ||||||
| Married | 11 (61.10) | 12 (70.60) | 0.35 | 1.0 | ||
| Other | 7 (38.90) | 5 (34.40) | ||||
| BC stage | ||||||
| 1 | 2 (11.10) | 6 (35.30) | 3.64 | 2.0 | ||
| 2 | 10 (55.60) | 5 (29.40) | ||||
| 3 | 6 (33.30) | 6 (35.30) | ||||
| Surgery | ||||||
| Lumpectomy | 10 (55.60) | 13 (76.50) | 1.70 | 1.0 | ||
| Mastectomy | 8 (44.40) | 4 (23.50) | ||||
| Medical therapy upon diagnosis | ||||||
| Chemo | 14 (77.80) | 11 (64.70) | 0.73 | 1.0 | ||
| Radio | 13 (72.20) | 12 (75.00) | 0.03 | 1.0 | ||
| Hormonal | 10 (55.60) | 13 (81.30) | 2.56 | 1.0 | ||
| Additional therapy | ||||||
| Lymphatic | 5 (27.80) | 4 (23.50) | 0.24 | 2.0 | ||
| None | 6 (33.30) | 7 (41.20) | ||||
| Other | 7 (38.90) | 6 (35.30) | ||||
| Measure | Intervention Group (n = 18) M (SD) | Control Group (n = 17) M (SD) | Group Effect | Time Effect | Interaction Effect | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | T1 | T2 | T3 | F(df) (1,33) | p | ηp2 | F(df) (2,66) | p | ηp2 | F(df) (2,66) | p | ηp2 | |
| COPM | |||||||||||||||
| PCOPM | 3.83 (1.60) | 6.01 (1.84) | 6.15 (1.84) | 4.01 (1.76) | 4.90 (1.85) | 5.35 (1.91) | 1.18 | 0.286 | 0.034 | 29.54 | 0.0001 | 0.472 | 3.51 | 0.036 | 0.096 |
| SCOPM | 2.63 (1.61) | 5.88 (2.64) | 6.04 (2.45) | 3.34 (1.58) | 4.84 (2.11) | 5.12 (2.41) | 0.44 | 0.511 | 0.013 | 37.15 | 0.0001 | 0.530 | 4.30 | 0.018 | 0.115 |
| ACS RAL | |||||||||||||||
| Total | 0.69 (0.18) | 0.73 (0.20) | 0.74 (0.20) | 0.58 (0.20) | 0.61 (0.20) | 0.59 (0.18) | 4.61 | 0.039 | 0.123 | 1.34 | 0.269 | 0.039 | 0.190 | 0.827 | 0.006 |
| IADL | 0.68 (0.20) | 0.74 (0.23) | 0.72 (0.23) | 0.60 (0.22) | 0.62 (0.23) | 0.63 (0.20) | 2.10 | 0.157 | 0.060 | 1.36 | 0.264 | 0.040 | 0.41 | 0.666 | 0.012 |
| Social | 0.65 (0.22) | 0.73 (0.24) | 0.69 (0.24) | 0.53 (0.28) | 0.56 (0.28) | 0.47 (0.23) | 5.43 | 0.026 | 0.141 | 1.88 | 0.161 | 0.054 | 0.96 | 0.388 | 0.028 |
| Motor performance | |||||||||||||||
| DASH | 48.19 (20.25) | 37.67 (22.13) | 34.72 (21.26) | 49.19 (20.58) | 44.02 (22.93) | 44.57 (22.73) | 0.70 | 0.407 | 0.021 | 9.28 | 0.0001 | 0.219 | 1.91 | 0.157 | 0.055 |
| Grip | 17.95 (5.98) | 18.99 (4.93) | 20.20 (5.63) | 16.61 (5.39) | 17.33 (5.79) | 16.73 (5.78) | 1.54 | 0.224 | 0.044 | 1.86 | 0.165 | 0.053 | 1.62 | 0.206 | 0.047 |
| Cognitive (BRIEF-A) | |||||||||||||||
| GEC | 64.33 (12.68) | 58.44 (11.34) | 58.44 (12.56) | 62.18 (12.19 | 60.00 (8.67) | 57.64 (10.80) | 0.02 | 0.893 | 0.001 | 8.01 | 0.001 | 0.195 | 0.95 | 0.394 | 0.028 |
| BRI | 58.17 (12.87) | 54.39 (12.17) | 54.94 (13.45) | 58.35 (12.68) | 56.12 (9.16) | 53.41 (10.02) | 0.02 | 0.900 | 0.0001 | 3.60 | 0.033 | 0.098 | 0.32 | 0.724 | 0.010 |
| MI | 63.28 (12.81) | 56.94 (10.60) | 56.50 (11.46) | 59.71 (12.60) | 57.94 (9.11) | 55.41 (9.83) | 0.12 | 0.727 | 0.004 | 9.76 | 0.0001 | 0.228 | 1.55 | 0.219 | 0.045 |
| FACT-B | |||||||||||||||
| Total | 91.55 (20.11) | 99.12 (21.24) | 100.75 (23.05) | 89.13 (14.82) | 94.99 (16.28) | 95.31 (16.83) | 0.44 | 0.510 | 0.0130 | 8.54 | 0.001 | 0.205 | 0.28 | 0.758 | 0.008 |
| EWB | 15.89 (4.31) | 17.11 (4.78) | 17.22 (4.60) | 16.06 (4.02) | 17.18 (5.02) | 16.82 (4.60) | 0.00 | 0.969 | 0.0000 | 2.28 | 0.110 | 0.065 | 1.30 | 0.882 | 0.004 |
| Measure | Median (Interquartile Range) | Freidman Test | |||||
|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | χ2 (df = 2) (p) | T1–T2 (p) | T2–T3 (p) | T1–T3 (p) | |
| Intervention group (n = 18) | |||||||
| ACS (high-leisure RAL) | 0.50 (0.32–0.79) | 0.67 (0.31–1.03) | 0.70 (0.38–1.00) | 8.58 (0.014) | −0.53 (0.593) | −1.90 (0.060) | 2.45 (0.014) |
| ACS (low-leisure RAL) | 0.81 (0.66–1.05) | 0.78 (0.63–1.03) | 0.82 (0.58–1.07) | 1.05 (0.591) | −0.31 (0.753) | −0.57 (0.570) | −0.16 (0.875) |
| Cognitive performance capacity (MOCA) | 27.00 (25.00–28.00) | 27.50 (26.75–28.25) | 29.00 (27.75–29.25) | 11.68 (0.003) | −1.38 (0.166) | −2.10 (0.036) | −2.89 (0.004) |
| Control group (n = 17) | |||||||
| ACS (high-leisure RAL) | 0.50 (0.18–0.65) | 0.42 (0.11–0.88) | 0.50 (0.18–0.81) | 1.45 (0.484) | −1.02 (0.310) | −0.20 (0.838) | −1.13 (0.258) |
| ACS (low-leisure RAL) | 0.75 (0.55–0.95) | 0.75 (0.63–1.01) | 0.75 (0.61–1.00) | 2.26 (0.323) | −1.38 (0.167) | −0.16 (0.875) | −1.10 (0.279) |
| Cognitive performance capacity (MOCA) | 26.00 (23.00–27.50) | 27.00 (24.50–28.50) | 26.00 (26.00–29.50) | 5.70 (0.058) | −1.91 (0.056) | −0.07 (0.944) | −1.56 (0.118) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Loubani, K.; Kizony, R.; Milman, U.; Schreuer, N. Hybrid Tele and In-Clinic Occupation Based Intervention to Improve Women’s Daily Participation after Breast Cancer: A Pilot Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 5966. https://doi.org/10.3390/ijerph18115966
Loubani K, Kizony R, Milman U, Schreuer N. Hybrid Tele and In-Clinic Occupation Based Intervention to Improve Women’s Daily Participation after Breast Cancer: A Pilot Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2021; 18(11):5966. https://doi.org/10.3390/ijerph18115966
Chicago/Turabian StyleLoubani, Khawla, Rachel Kizony, Uzi Milman, and Naomi Schreuer. 2021. "Hybrid Tele and In-Clinic Occupation Based Intervention to Improve Women’s Daily Participation after Breast Cancer: A Pilot Randomized Controlled Trial" International Journal of Environmental Research and Public Health 18, no. 11: 5966. https://doi.org/10.3390/ijerph18115966
APA StyleLoubani, K., Kizony, R., Milman, U., & Schreuer, N. (2021). Hybrid Tele and In-Clinic Occupation Based Intervention to Improve Women’s Daily Participation after Breast Cancer: A Pilot Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 18(11), 5966. https://doi.org/10.3390/ijerph18115966






