What Is the Evidence Globally for Culturally Safe Strategies to Improve Breast Cancer Outcomes for Indigenous Women in High Income Countries? A Systematic Review
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Eligibility Criteria
2.3. Search Strategy
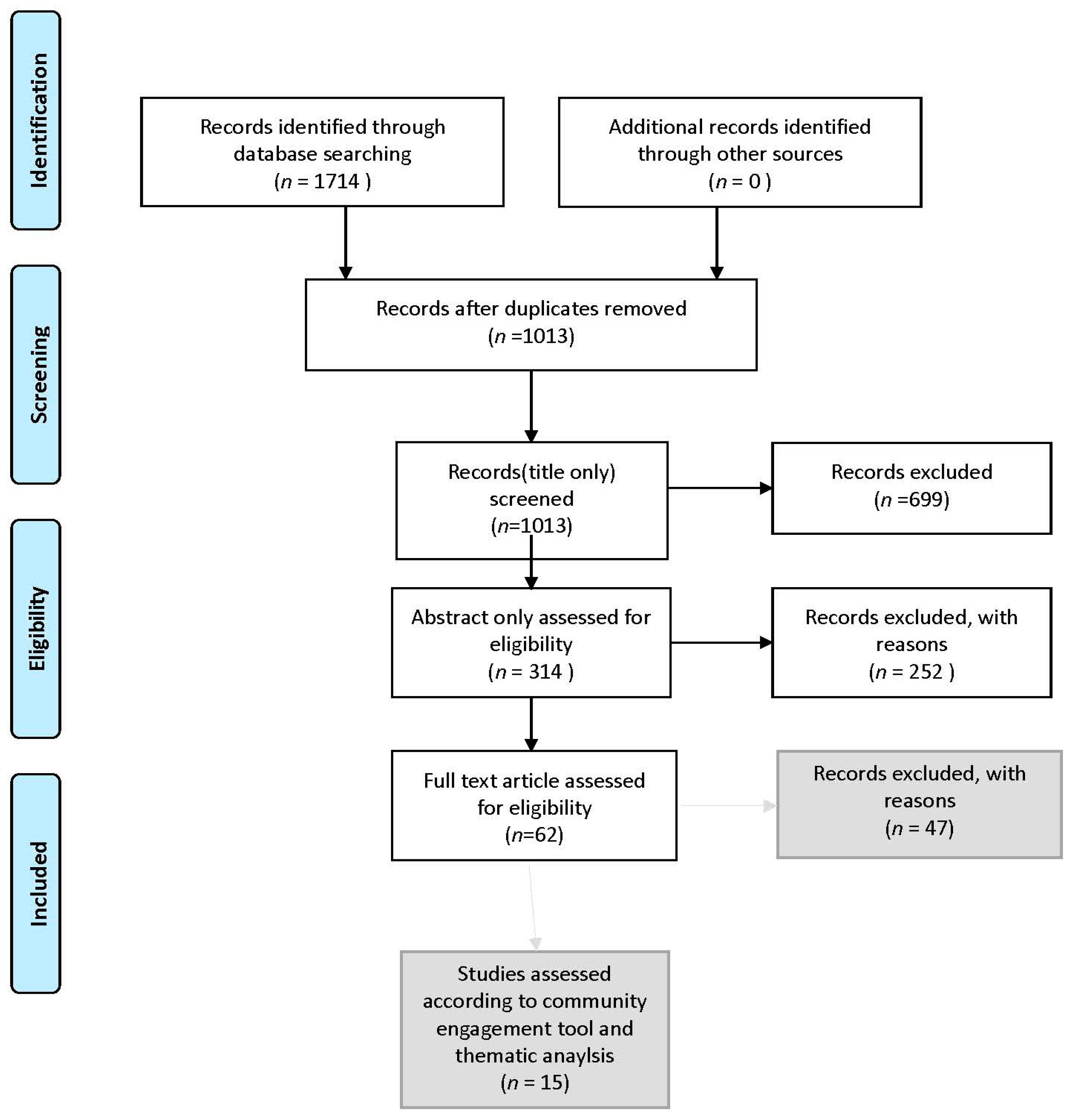
2.4. Study Selection Process
2.5. Community Engagement Assessment
2.6. Thematic Analysis
2.7. Data Extraction and Synthesis
3. Results
3.1. Community Engagement Tool
3.2. Thematic Analysis
4. Discussion
4.1. The Importance of Community Engagement
4.2. Themes Emerging in the Literature
Culture Making a Difference
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Australian Institute of Health and Welfare. Cancer in Aboriginal & Torres Strait Islander People of Australia; AIHW: Canberra, Australian, 2018.
- Australian Institute of Health and Welfare. BreastScreen Australia Monitoring Report 2019; AIHW: Canberra, Australian, 2019.
- Read, D.J.; Frentzas, S.; Ward, L.; De Ieso, P.; Chen, S.; Devi, V. Do histopathological features of breast cancer in Australian Indigenous women explain the survival disparity? A two decade long study in the Northern Territory. Asia Pac. J. Clin. Oncol. 2020. [Google Scholar] [CrossRef]
- Moore, S.P.; Soerjomataram, I.; Green, A.C.; Garvey, G.; Martin, J.; Valery, P.C. Breast cancer diagnosis, patterns of care and burden of disease in Queensland, Australia (1998-2004): Does being Indigenous make a difference? Int. J. Public Health 2016, 61, 435–442. [Google Scholar] [CrossRef] [PubMed]
- Tapia, K.A.; Garvey, G.; Mc Entee, M.; Rickard, M.; Brennan, P. Breast Cancer in Australian Indigenous Women: Incidence, Mortality, and Risk Factors. Asian Pac. J. Cancer Prev. APJCP 2017, 18, 873–884. [Google Scholar] [CrossRef]
- Dasgupta, P.; Baade, P.D.; Youlden, D.R.; Garvey, G.; Aitken, J.F.; Wallington, I.; Chynoweth, J.; Zorbas, H.; Roder, D.; Youl, P.H. Variations in outcomes for Indigenous women with breast cancer in Australia: A systematic review. Eur. J. Cancer Care 2017, 26, e12662. [Google Scholar] [CrossRef] [PubMed]
- Banham, D.; Roder, D.; Keefe, D.; Farshid, G.; Eckert, M.; Howard, N.; Canuto, K.; Brown, A.; CanDAD Aboriginal Community Reference Group and Other CanDAD Investigators. Disparities in breast screening, stage at diagnosis, cancer treatment and the subsequent risk of cancer death: A retrospective, matched cohort of aboriginal and non-aboriginal women with breast cancer. BMC Health Serv. Res. 2019, 19, 387. [Google Scholar] [CrossRef] [Green Version]
- Thompson, S.C. Indigenous women and breast cancer. Med. J. Aust. 2009, 190, 602. [Google Scholar] [CrossRef]
- Byers, L.; Michell, K.; McCullough, K. Awareness, acceptability and access to screening mammography for remote Aboriginal women. Health Promot. J. Austr. 2018, 29, 366–367. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J.; Kurnoth, P. Well Women Making a Diffence: Evaluation Report and Program Guide; Women’s Cancer Prevention Program, Department of Health and Community Services, Northern Territory Government: Darwin, Australian, 2000. [Google Scholar]
- Fox, W.; Powell, M.; Hyland, V.; Honeyball, F. Supportive care for women with breast cancer living in rural Australia. Cancer Forum 2017, 41, 62–66. [Google Scholar]
- Hedges, S.; Davidson, M.; Forrester, S.; Casey, A.; Pridmore, V.; Cooper, A.; Beauchamp, A.; McGrath, N. A Breast Screening Shawl to Help Aboriginal Women Feel More Comfortable and Culturally Safe. J. Glob. Oncol. 2018, 4, 40s. [Google Scholar] [CrossRef]
- McMichael, C.; Kirk, M.; Manderson, L.; Hoban, E.; Potts, H. Indigenous women’s perceptions of breast cancer diagnosis and treatment in Queensland. Aust. N. Zealand J. Public Health 2000, 24, 515–519. [Google Scholar] [CrossRef]
- Informit. ‘Orchid’ Breastscreen Queensland’s New 4WD Digital Mobile Service. Aborig. Isl. Health Work. J. 2010, 34, 39. [Google Scholar]
- Pilkington, L.; Haigh, M.M.; Durey, A.; Katzenellenbogen, J.M.; Thompson, S.C. Perspectives of Aboriginal women on participation in mammographic screening: A step towards improving services. BMC Public Health 2017, 17, 697. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reath, J.; Carey, M. Breast and cervical cancer in Indigenous women: Overcoming barriers to early detection. Aust. Fam. Physician 2008, 37, 178. [Google Scholar]
- Supramaniam, R.; Gibberd, A.; Dillon, A.; Goldsbury, D.E.; O’Connell, D.L. Increasing rates of surgical treatment and preventing comorbidities may increase breast cancer survival for Aboriginal women. BMC Cancer 2014, 14, 163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, R. Cultural safety: What does it mean for our work practice? Aust. N. Zealand J. Public Health. 2008, 23, 213–214. [Google Scholar] [CrossRef] [PubMed]
- Valery, P.C.; Bernardes, C.M.; de Witt, A.; Martin, J.; Walpole, E.; Garvey, G.; Williamson, D.; Meiklejohn, J.; Hartel, G.; Ratnasekera, I.U.; et al. Patterns of primary health care service use of Indigenous Australians diagnosed with cancer. Support Care Cancer 2020, 28, 317–327. [Google Scholar] [CrossRef] [PubMed]
- Gwynne, K. Applying Collective Impact to Wicked Problems in Aboriginal Health. Metrop. Univ. 2017, 28, 115. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [Green Version]
- Christie, V.; Gwynne, K. What is the evidence globally for culturally safe therapies in improving breast cancer outcomes for Indigenous women in wealthy countries? In PROSPERO; 2020; Available online: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=193019 (accessed on 30 July 2020).
- NHMRC (National Health & Medical Research Council). Road Map 3: A strategic framework for improving Aboriginal and Torres Strait Islander health through research; National Health and Medical Research Council: Canberra, Australia, 2018.
- Banner, R.O.; DeCambra, H.; Enos, R.; Gotay, C.; Hammond, O.W.; Hedlung, N.; Issell, B.F.; Matsunaga, D.S.; Tsark, J.A. A breast and cervical cancer project in a native Hawaiian community: Wai’anae cancer research project. Prev. Med. 1995, 24, 447–453. [Google Scholar] [CrossRef]
- Becker, S.A.; Affonso, D.D.; Beard, M.B.H. Talking circles: Northern Plains tribes American Indian women’s views of cancer as a health issue. Public Health Nurs. 2006, 23, 27–36. [Google Scholar] [CrossRef]
- Brown, S.R.; Nuno, T.; Joshweseoma, L.; Begay, R.C.; Goodluck, C.; Harris, R.B.; Brown, S.R.; Nuno, T.; Joshweseoma, L.; Begay, R.C.; et al. Impact of a community-based breast cancer screening program on Hopi women. Prev. Med. 2011, 52, 390–393. [Google Scholar] [CrossRef] [Green Version]
- Daley, C.; Filippi, M.; James, A.; Weir, M.; Braiuca, S.; Kaur, B.; Choi, W.; Greiner, K. American Indian Community Leader and Provider Views of Needs and Barriers to Mammography. J. Community Health 2012, 37, 307–315. [Google Scholar] [CrossRef]
- Daley, C.M.; Kraemer-Diaz, A.; James, A.S.; Monteau, D.; Joseph, S.; Pacheco, J.; Bull, J.W.; Cully, A.; Choi, W.S.; Greiner, K.A. Breast cancer screening beliefs and behaviors among American Indian women in Kansas and Missouri: A qualitative inquiry. J. Cancer Educ. Off. J. Am. Assoc. Cancer Educ. 2012, 27 (Suppl. 1), S32–S40. [Google Scholar] [CrossRef] [PubMed]
- English, K.C.; Fairbanks, J.; Finster, C.E.; Rafelito, A.; Luna, J.; Kennedy, M. A socioecological approach to improving mammography rates in a tribal community. Health Educ. Behav. 2008, 35, 396–409. [Google Scholar] [CrossRef] [PubMed]
- Friedman, D.B.; Hoffman-Goetz, L. Assessing cultural sensitivity of breast cancer information for older Aboriginal women. J. Cancer Educ. 2007, 22, 112–118. [Google Scholar] [CrossRef]
- Haozous, E.A.; Eschiti, V.; Lauderdale, J.; Hill, C. Use of the Talking Circle for Comanche Women’s Breast Health Education. J. Transcult. Nurs. 2010, 21, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Ka’opua, L.S.; Park, S.H.; Ward, M.E.; Braun, K.L. Testing the feasibility of a culturally tailored breast cancer screening intervention with Native Hawaiian women in rural churches. Health Soc. Work 2011, 36, 55–65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roh, S.; Burnette, C.E.; Lee, Y.S.; Jun, J.S.; Lee, H.Y.; Lee, K.H. Breast cancer literacy and health beliefs related to breast cancer screening among American Indian women. Soc. Work Health Care 2018, 57, 465–482. [Google Scholar] [CrossRef]
- Sanderson, P.R.; Teufel-Shone, N.I.; Baldwin, J.A.; Sandoval, N.; Robinson, F.; Sanderson, P.R.; Teufel-Shone, N.I.; Baldwin, J.A.; Sandoval, N.; Robinson, F. Breast cancer education for Navajo women: A pilot study evaluating a culturally relevant video. J. Cancer Educ. 2010, 25, 217–223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sinicrope, P.S.; Bauer, M.C.; Patten, C.A.; Austin-Garrison, M.; Garcia, L.; Hughes, C.A.; Bock, M.J.; Decker, P.A.; Yost, K.J.; Petersen, W.O.; et al. Development and Evaluation of a Cancer Literacy Intervention to Promote Mammography Screening Among Navajo Women: A Pilot Study. Am. J. Health Promot. AJHP 2020. [Google Scholar] [CrossRef]
- Strickland, C.J.; Hillaire, E. Conducting a Feasibility Study in Women’s Health Screening Among Women in a Pacific Northwest American Indian Tribe. J. Transcult. Nurs. 2016, 27, 42–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tolma, E.L.; Stoner, J.A.; Li, J.; Kim, Y.; Engelman, K.K. Predictors of regular mammography use among American Indian women in Oklahoma: A cross-sectional study. BMC Women’s Health 2014, 14, 101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liberato, S.C.; Brimblecombe, J.; Ritchie, J.; Ferguson, M.; Coveney, J. Measuring capacity building in communities: A review of the literature. BMC Public Health 2011, 11, 850. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- NHMRC (National Health & Medical Research Council). The NHMRC Road Map II: A Strategic Framework for Improving the Health of Aboriginal and Torres Strait Islander People. through Research; National Health and Medical Research Council: Canberra, Australia, 2010.
- Burhansstipanov, L.; Krebs, L.U.; Grass, R.; Wanliss, E.J.; Saslow, D. A review of effective strategies for native women’s breast health outreach and education. J. Cancer Educ. Off. J. Am. Assoc. Cancer Educ. 2005, 20, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Burhannistipanov, L. Cancer: A growing problem among American Indians and Alaska Natives. In Promises to Keep: Public Health Policy for American Indians and Alaska Natives in the 21st Century; Dixon, M., Roubideaux, Y., Association, A.P.H., Eds.; American Public Health Association: Northwest, WA, USA, 2001. [Google Scholar]
- Carrese, J.A.; Rhodes, L.A. Bridging cultural differences in medical practice. The case of discussing negative information with Navajo patients. J. Gen. Intern. Med. 2000, 15, 92–96. [Google Scholar] [CrossRef] [Green Version]
- Csordas, T. The Sore That Does Not Heal: Cause and Concept in the Navajo Experience of Cancer. J. Anthropol. Res. 1989, 45, 457–485. [Google Scholar] [CrossRef]
- Gwynne, K.; Jeffries, T.; Lincoln, M. Improving the efficacy of healthcare services for Aboriginal Australians. Aust. Health Rev. 2018. [Google Scholar] [CrossRef]
| Title | Authors | Reference | Numbers | Methods | Location |
|---|---|---|---|---|---|
| A breast and cervical cancer project in a native Hawaiian community: Wai’anae cancer research project | Banner, R.O. | [24] | 1260 | Baseline telephone survey | Hawaii, USA |
| DeCambra, H. | |||||
| Enos, R. | |||||
| Gotay, C. | |||||
| Hammond, O.W. | |||||
| Hedlung, N. | |||||
| Issell, B.F. | |||||
| Matsunaga, D.S. | |||||
| Tsark, J.A. | |||||
| Talking circles: Northern Plains tribes American Indian women’s views of cancer as a health issue | Becker, S.A. | [25] | 28 | Talking Circle and focus group methodology, combined with Affonso’s Focus Groups Analytic Schema. | South Dakota, USA |
| Affonso, D.D. | |||||
| Beard, M.B.H. | |||||
| Impact of a community-based breast cancer screening program on Hopi women | Brown, S.R. | [26] | 250 | Community meetings, focus groups, and researchers jointly developed a culturally appropriate survey instrument. | Arizona, USA |
| Nuno, T. | |||||
| Joshweseoma, L. | |||||
| Begay, R.C. | |||||
| Goodluck, C. | |||||
| Harris, R.B. | |||||
| Brown, S.R. | |||||
| Nuno, T. | |||||
| Joshweseoma, L. | |||||
| Begay, R.C. | |||||
| Goodluck, C. | |||||
| Harris, R.B. | |||||
| American Indian Community Leader and Provider Views of Needs and Barriers to Mammography | Daley, C. | [27] | 30 totals (n = 13 community leaders; n = 17 health providers) | Interviews | Kansas, USA |
| Filippi, M. | |||||
| James, A. | |||||
| Weir, M. | |||||
| Braiuca, S. | |||||
| Kaur, B. | |||||
| Choi, W. | |||||
| Greiner, K. | |||||
| Breast cancer screening beliefs and behaviors among American Indian women in Kansas and Missouri: a qualitative inquiry | Daley, C.M. | [28] | 84 | Focus groups | Kansas and Missouri, USA |
| Kraemer-Diaz, A. | |||||
| James, A.S. | |||||
| Monteau, D. | |||||
| Joseph, S. | |||||
| Pacheco, J. | |||||
| Bull, J.W. | |||||
| Cully, A. | |||||
| Choi, W.S. | |||||
| Greiner, K.A. | |||||
| A socioecological approach to improving mammography rates in a tribal community | English, K.C. | [29] | 25 | Focus groups | New Mexico, USA |
| Fairbanks, J. | |||||
| Finster, C.E. | |||||
| Rafelito, A. | |||||
| Luna, J. | |||||
| Kennedy, M. | |||||
| Assessing cultural sensitivity of breast cancer information for older Aboriginal women | Friedman, D.B. | [30] | 25 | Interviews | Ontario, Canada |
| Hoffman-Goetz, L. | |||||
| Use of the Talking Circle for Comanche Women’s Breast Health Education | Haozous, E.A. | [31] | 7 | Talking Circle | Oklahoma, USA |
| Eschiti, V. | |||||
| Lauderdale, J. | |||||
| Hill, C. | |||||
| Testing the feasibility of a culturally tailored breast cancer screening intervention with Native Hawaiian women in rural churches | Ka’opua, L.S. | [32] | 198 | randomized, two-group pre–post control group comparison | Hawaii, USA |
| Park, S.H. | |||||
| Ward, M.E. | |||||
| Braun, K.L. | |||||
| Perspectives of Aboriginal women on participation in mammographic screening: a step towards improving services | Pilkington, L. | [15] | 65 | Semi-structured interviews, focus group discussions and yarning sessions | Western Australia |
| Haigh, M.M. | |||||
| Durey, A. | |||||
| Katzenellenbogen, J.M. | |||||
| Thompson, S.C. | |||||
| Breast cancer literacy and health beliefs related to breast cancer screening among American Indian women | Roh, S. | [33] | 286 | Self-administered survey | South Dakota, US |
| Burnette, C.E. | |||||
| Lee, Y.S. | |||||
| Jun, J.S. | |||||
| Lee, H.Y. | |||||
| Lee, K.H. | |||||
| Breast cancer education for Navajo women: a pilot study evaluating a culturally relevant video | Sanderson, P.R. | [34] | 40 in total (n = 14 women diagnosed with breast cancer; n = 26 healthcare providers) | Questionnaires | Arizona, US |
| Teufel-Shone, N.I. | |||||
| Baldwin, J.A. | |||||
| Sandoval, N. | |||||
| Robinson, F. | |||||
| Development and Evaluation of a Cancer Literacy Intervention to Promote Mammography Screening Among Navajo Women: A Pilot Study | Sinicrope, P.S. | [35] | 25 | Interviews | Navajo Nation, US |
| Bauer, M.C. | |||||
| Patten, C.A. | |||||
| Austin-Garrison, M. | |||||
| Garcia, L. | |||||
| Hughes, C.A. | |||||
| Bock, M.J. | |||||
| Decker, P.A. | |||||
| Yost, K.J. | |||||
| Petersen, W.O. | |||||
| Buki, L.P. | |||||
| Garrison, E.R. | |||||
| Conducting a Feasibility Study in Women’s Health Screening Among Women in a Pacific Northwest American Indian Tribe | Strickland, C. June | [36] | 10 | Interviews | Pacific Northwest, US |
| Hillaire, Elaine | |||||
| Predictors of regular mammography use among American Indian women in Oklahoma: a cross-sectional study | Tolma, Eleni L. | [37] | 255 | Survey | Oklahoma |
| Stoner, Julie A. | |||||
| Li, Ji | |||||
| Kim, Yoonsang | |||||
| Engelman, Kimberly K. |
| Study | Issue Identified by the Community | Indigenous Governance | Capacity Building | Cultural Consideration in Design | Respecting Community Experience | Total Score |
|---|---|---|---|---|---|---|
| Banner et al. [24] | 1 | 1 | 1 | 1 | 4 | |
| Becker et al. [25] | 1 | 1 | 1 | 1 | 4 | |
| Brown et al. [26] | 1 | 1 | 1 | 1 | 4 | |
| Daley et al. 1 [27] | 1 | 1 | 1 | 1 | 4 | |
| Daley et al. 2 [28] | 1 | 1 | 1 | 1 | 4 | |
| English et al. [29] | 1 | 1 | 1 | 1 | 1 | 5 |
| Friedman et al. [30] | 0 | |||||
| Haozous et al. [31] | 1 | 1 | 1 | 3 | ||
| Ka’opua et al. [32] | 1 | 1 | 1 | 1 | 4 | |
| Pilkington et al. [15] | 1 | 1 | 1 | 3 | ||
| Roh et al. [33] | 0 | |||||
| Sanderson et al. [34] | 1 | 1 | ||||
| Sinicrope et al. [35] | 1 | 1 | 1 | 1 | 4 | |
| Strickland et al. [36] | 1 | 1 | 1 | 1 | 4 | |
| Tolma et al. [37] | 0 | |||||
| Total number of studies | 15 |
| Study | Theme 1: Silence | Theme 2: Service Access | Theme 3: Cultural Conception of Cancer | Theme 4: Family and Community Support |
|---|---|---|---|---|
| Banner et al. [24] | X | |||
| Becker et al. [25] | X | X | ||
| Brown et al. [26] | X | |||
| Daley et al. 1 [27] | X | X | ||
| Daley et al. 2 [28] | X | X | ||
| English et al. [29] | X | X | X | X |
| Friedman et al. [30] | X | |||
| Haozous et al. [31] | X | X | ||
| Ka’opua et al. [32] | X | X | ||
| Pilkington et al. [15] | X | X | ||
| Roh et al. [33] | X | X | ||
| Sanderson et al. [34] | X | X | X | |
| Sinicrope et al. [35] | X | X | ||
| Strickland et al. [36] | X | X | ||
| Tolma et al. [37] | X | X |
| Study | Success Factor 1: Community Participation; Researchers of Own Health Concerns | Success Fact 2: Incorporation of Culture in Research Design |
|---|---|---|
| Brown [26] | x | |
| Banner [24] | x | |
| Becker [25] | x | x |
| Daley et al. 1 [27] | x | |
| Daley et al. 2 [28] | x | x |
| English et al. [29] | x | x |
| Ka’opua et al. [32] | x | |
| Sinicrope et al. [35] | x | |
| Strickland et al. [36] | x | x |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Christie, V.; Green, D.; Amin, J.; Pyke, C.; Littlejohn, K.; Skinner, J.; McCowen, D.; Gwynne, K. What Is the Evidence Globally for Culturally Safe Strategies to Improve Breast Cancer Outcomes for Indigenous Women in High Income Countries? A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 6073. https://doi.org/10.3390/ijerph18116073
Christie V, Green D, Amin J, Pyke C, Littlejohn K, Skinner J, McCowen D, Gwynne K. What Is the Evidence Globally for Culturally Safe Strategies to Improve Breast Cancer Outcomes for Indigenous Women in High Income Countries? A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(11):6073. https://doi.org/10.3390/ijerph18116073
Chicago/Turabian StyleChristie, Vita, Debbie Green, Janaki Amin, Christopher Pyke, Karen Littlejohn, John Skinner, Deb McCowen, and Kylie Gwynne. 2021. "What Is the Evidence Globally for Culturally Safe Strategies to Improve Breast Cancer Outcomes for Indigenous Women in High Income Countries? A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 11: 6073. https://doi.org/10.3390/ijerph18116073
APA StyleChristie, V., Green, D., Amin, J., Pyke, C., Littlejohn, K., Skinner, J., McCowen, D., & Gwynne, K. (2021). What Is the Evidence Globally for Culturally Safe Strategies to Improve Breast Cancer Outcomes for Indigenous Women in High Income Countries? A Systematic Review. International Journal of Environmental Research and Public Health, 18(11), 6073. https://doi.org/10.3390/ijerph18116073








