Proposal for the Inclusion of Tobacco Use in Suicide Risk Scales: Results of a Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Search Strategy
2.3. Inclusion and Exclusion Criteria
2.4. Data Extraction
2.5. Summary Measures
2.6. Quality Assessment
2.7. Heterogeneity and Publication Bias
2.8. Sensitivity and Subgroup Analysis
3. Results
3.1. Studies Included
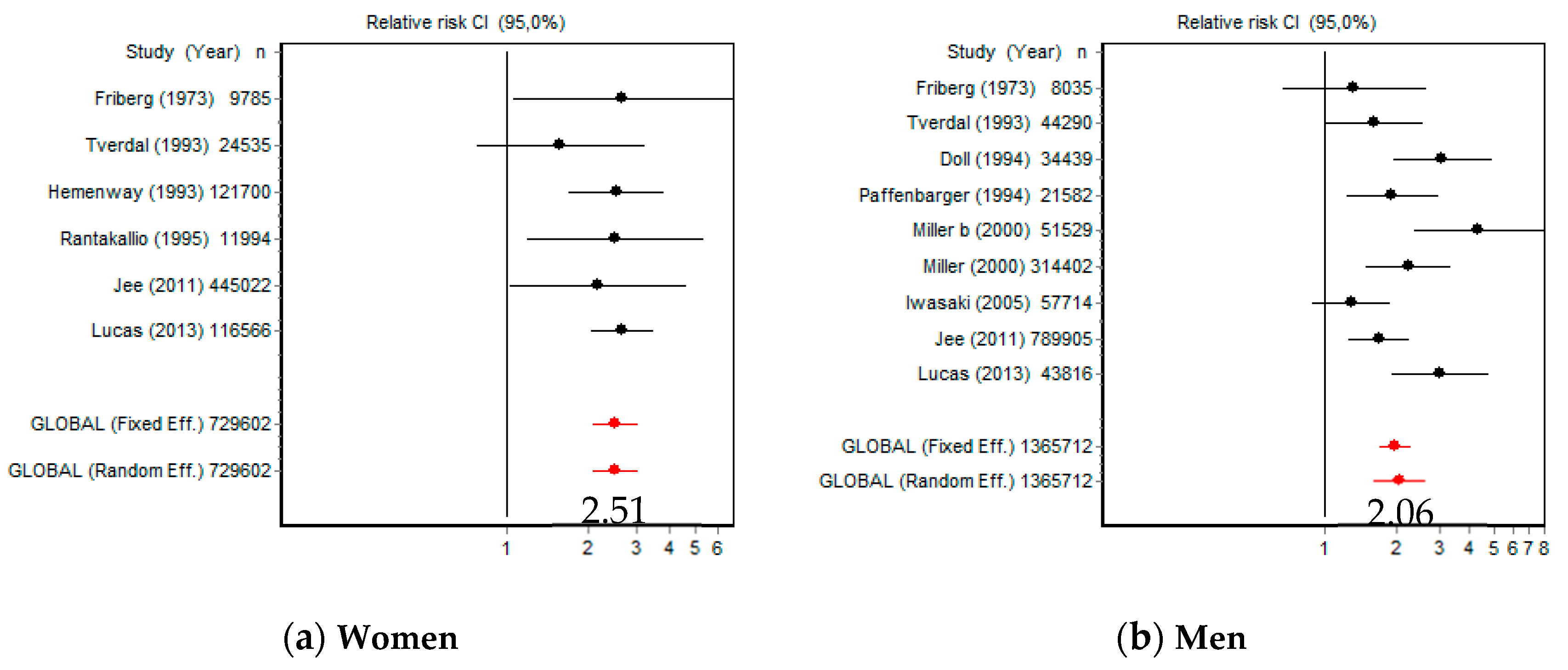
3.2. Smoking and Risk of Death by Suicide
3.3. Smoking and Risk of Suicide Ideation
3.4. Smoking and Risk of Suicide Attempts
3.5. Smoking and Risk of Suicidal Behaviours
3.6. Publication Bias
3.7. Sensitivity Analysis
3.8. Subgroup Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization Suicide. Available online: https://www.who.int/es/news-room/fact-sheets/detail/suicide (accessed on 17 June 2020).
- Instituto Nacional de Estadística. Suicidio. 2019. Available online: https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176780&menu=ultiDatos&idp=1254735573175 (accessed on 17 June 2020).
- Sudak, H.; Maxim, K.; Carpenter, M. Suicide and stigma: A review of the literature and personal reflections. Acad. Psychiatry 2008, 32, 136–142. [Google Scholar] [CrossRef]
- Anseán, A. Suicidios. Manual De Prevención, Intervención Y Postvención de la Conducta Suicida, 2nd ed.; Fundación Salud Mental España: Madrid, Spain, 2014. [Google Scholar]
- World Health Organization Tobacco. Available online: https://www.who.int/es/news-room/fact-sheets/detail/tobacco (accessed on 17 June 2020).
- Piña, A.; Peralta, F.J.; De la Vega, D.; Giner, L.; Guija, J. Tabaco y suicidio. In Proceedings of the Conferencia Hospital Universitario Virgen Macarena, Sevilla, Spain, 2 May 2018; Available online: https://psiquiatria.com/bibliopsiquis/tabaco-y-suicidio (accessed on 17 June 2020).
- Ribeiro, J.D.; Franklin, J.C.; Fox, K.R.; Bentley, K.H.; Kleiman, E.M.; Chang, B.P.; Nock, M.K. Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: A meta-analysis of longitudinal studies. Psychol. Med. 2016, 46, 225–236. [Google Scholar] [CrossRef]
- Tanskanen, A.; Tuomilehto, J.; Viinamäki, H.; Vartiainen, E.; Lehtonen, J.; Puska, P. Smoking and the risk of suicide. Acta Psychiatr. Scand. 2000, 101, 243–245. [Google Scholar] [CrossRef] [PubMed]
- Hughes, J.R. Smoking and suicide: A brief overview. Drug Alcohol. Depend. 2008, 98, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Bolton, J.; Spiwak, R.; Sareen, J. Predicting suicide attempts with the SAD PERSONS scale: A longitudinal analysis. J. Clin. Psychiatry 2012, 73, e735. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Yang, X.; Ge, Z.; Hao, Y.; Wang, Q.; Liu, F.; Gu, D.; Huang, J. Cigarette smoking and risk of completed suicide: A meta-analysis of prospective cohort studies. J. Psychiatr. Res. 2012, 46, 1257–1266. [Google Scholar] [CrossRef]
- Poorolajal, J.; Darvishi, N. Smoking and suicide: A meta-analysis. PLoS ONE 2016, 11, e0156348. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and metaanalyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef]
- Wells, G.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Metaanalyses. 2019. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 20 December 2020).
- Beard, J.D.; Umbach, D.M.; Joppin, J.A.; Richards, M.; Alavanja, M.C.R.; Blair, A.; Sandler, D.P.; Kamel, F. Suicide and Pesticide Use among Pesticide Applicators and Their Spouses in the Agricultural Health Study. Environ. Health Perspect. 2011, 119, 1610–1615. [Google Scholar] [CrossRef]
- Berlin, I.; Hakes, J.K.; Hu, M.C.; Covey, L.S. Tobacco Use and Suicide Attempt: Longitudinal Analysis with Retrospective Reports. PLoS ONE 2015, 10, e0122607. [Google Scholar] [CrossRef]
- Clarke, D.; Eaton, W.W.; Petronis, K.R.; Ko, J.Y.; Chatterjee, A.; Anthony, J.C. Increased Risk of Suicidal Ideation in Smokers and Former Smokers Compared to Never Smokers: Evidence from the Baltimore ECA Follow-Up Study. Suicide Life Threat Behav. 2010, 40, 307–318. [Google Scholar] [CrossRef][Green Version]
- Doll, R.; Peto, R.; Wheatley, K.; Gray, R.; Sutherland, I. Mortality in relation to smoking: 40 years’ observations on male British doctors. BMJ 1994, 309, 901–911. [Google Scholar] [CrossRef]
- Evins, A.E.; Korhonen, T.; Kinnunen, T.H.; Kaprio, J. Prospective association between tobacco smoking and death by suicide: A competing risks hazard analysis in a large twin cohort with 35-year follow-up. Psychol. Med. 2017, 47, 2143–2154. [Google Scholar] [CrossRef] [PubMed]
- Friberg, L.; Cederlöf, R.; Lorich, U.; Lundman, T.; de Faire, U. Mortality in Twins in Relation to Smoking Habits and Alcohol Problems. Arch. Environ. Health 1973, 27, 294–304. [Google Scholar] [CrossRef]
- Hemenway, D.; Solnick, S.J.; Colditz, G.A. Smoking and Suicide among Nurses. Am. J. Public Health 1993, 83, 249–251. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, M.; Akechi, T.; Uchitomi, Y.; Tsugane, S. Japan Public Health Center-based Prospective Study on Cancer and Cardiovascular Disease (JPHC study) Group. Ann. Epidemiol. 2005, 15, 286–292. [Google Scholar] [CrossRef]
- Jee, S.H.; Kivimaki, M.; Kang, H.C.; Park, I.S.; Samet, J.M.; Batty, G.D. Cardiovascular disease risk factors in relation to suicide mortality in Asia: Prospective cohort study of over one million Korean men and women. Eur. Heart J. 2011, 32, 2773–2780. [Google Scholar] [CrossRef]
- Kang, H.J.; Stewart, R.; Jeonk, B.O.; Kim, S.Y.; Bae, K.Y.; Kim, S.W.; Kim, J.M.; Shin, I.S.; Yoon, J.S. Suicidal ideation in elderly Korean population: A two-year longitudinal study. Int. Psychogeriatr. 2014, 26, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Borges, G.; Sampson, N.; Miller, M.; Nock, M.K. The association between smoking and subsequent suicide-related outcomes in the National Comorbidity Survey panel sample. Mol. Psychiatry 2009, 14, 1132–1142. [Google Scholar] [CrossRef]
- Leistikow, B.N.; Martin, D.C.; Samuels, S.J. Injury death excesses in smokers: A 1990–95 United States national cohort study. Inj. Prev. 2000, 6, 277–280. [Google Scholar] [CrossRef]
- Lucas, M.; O’Reilly, E.J.; Mirzaei, F.; Okereke, O.I.; Unger, L.; Miller, M.; Ascherio, A. Cigarette smoking and completed suicide: Results from 3 prospective cohorts of American adults. J. Affect Disord. 2013, 151, 1053–1058. [Google Scholar] [CrossRef]
- Miller, M.; Hemenway, D.; Bell, N.S.; Yore, M.M.; Amoroso, P.J. Cigarette Smoking and Suicide: A Prospective Study of 300,000 Male Active-duty Army Soldiers. Am. J. Epidemiol. 2000, 151, 1060–1063. [Google Scholar] [CrossRef]
- Miller, M.; Hemenway, D.; Rimm, E. Cigarettes and Suicide: A Prospective Study of 50 000 Men. Am. J. Public Health 2000, 90, 768–773. [Google Scholar] [CrossRef] [PubMed]
- Paffenbarger, R.S.; Lee, I.M.; Leung, R. Physical activity and personal characteristics associated with depression and suicide in American college men. Acta Psychiatr. Scand. Suppl. 1994, 377, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Rantakallio, P.; Läärä, E.; Koiranen, M. A 28 year follow up of mortality among women who smoked during pregnancy. BMJ 1995, 311, 477–480. [Google Scholar] [CrossRef][Green Version]
- Riala, K.; Taanila, A.; Hakko, H.; Räsänen, P. Longitudinal Smoking Habits as Risk Factors for Early-Onset and Repetitive Suicide Attempts: The Northern Finland 1966 Birth Cohort Study. Ann. Epidemiol. 2009, 19, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Sonderman, J.S.; Munro, H.M.; Blot, W.J.; Tarone, R.E.; McLaughlin, J.K. Suicides, Homicides, Accidents, and Other External Causes of Death among Blacks and Whites in the Southern Community Cohort Study. PLoS ONE 2014, 9, e114852. [Google Scholar] [CrossRef] [PubMed]
- Tverdal, A.; Thelle, D.; Stensvold, I.; Leren, P.; Bjartveit, K. Mortality in relation to smoking history: 13 years’ follow-up of 68,000 Norwegian men and women 35–49 years. J. Clin. Epidemiol. 1993, 46, 475–487. [Google Scholar] [CrossRef]
- Sathian, B.; Menezes, R.G.; Asim, M.; Mekkodathil, A.; Sreedharan, J.; Banerjee, I.; van Teijlingen, E.R.; Roy, B.; Subramanya, S.H.; Kharoshah, M.A.; et al. Cigarette smoking dose-response and suicidal ideation among young people in Nepal: A cross-sectional study. Nepal. J. Epidemiol. 2020, 10, 821–829. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; McKeown, R.; Hussey, J.; Thompson, S.; Woods, J. Gender differences in risk factors for attempted suicide among young adults: Findings from the Third National Health and Nutrition Examination Survey. Ann. Epidemiol. 2005, 15, 167–174. [Google Scholar] [CrossRef] [PubMed]
- Benowitz, N.L. Nicotine addiction. N. Engl. J. Med. 2010, 362, 2295–2303. [Google Scholar] [CrossRef]
- Berlin, I. Monoamine Oxidase Inhibitors for Smoking Cessation. In Medication Treatments for Nicotine Dependence; George, T.P., Weinberger, A.H., Eds.; Taylor and Francis: Boca Raton, FL, USA, 2007; pp. 109–121. [Google Scholar]
- Malone, K.M.; Waternaux, C.; Haas, G.L.; Cooper, T.B.; Li, S.; Mann, J.J. Cigarette smoking, suicidal behavior, and serotonin function in major psychiatric disorders. Am. J. Psychiatry 2003, 160, 773–779. [Google Scholar] [CrossRef]
- Keilp, J.G.; Oquendo, M.A.; Stanley, B.H.; Burke, A.K.; Cooper, T.B.; Malone, K.M.; Mann, J. Future suicide attempt and responses to serotonergic challenge. Neuropsychopharmacology 2010, 35, 1063–1072. [Google Scholar] [CrossRef] [PubMed]
- Aubin, H.J.; Berlin, I.; Reynaud, M. Current smoking, hypoxia, and suicide. Am. J. Psychiatry 2011, 168, 326–327. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.; Mickelson, J.B.; Brenner, B.E.; Haws, C.A.; Yurgelun-Todd, D.A.; Renshaw, P.F. Altitude, gun ownership, rural areas, and suicide. Am. J. Psychiatry 2011, 168, 49–54. [Google Scholar] [CrossRef]
- Dome, P.; Lazary, J.; Kalapos, M.P.; Rihmer, Z. Smoking, nicotine and neuropsychiatric disorders. Neurosci. Biobehav. Rev. 2010, 34, 295–342. [Google Scholar] [CrossRef]
- Flensborg-Madsen, T.; von Scholten, M.B.; Flachs, E.M.; Mortensen, E.L.; Prescott, E.; Tolstrup, J.S. Tobacco smoking as a risk factor for depression. A 26-year population-based follow-up study. J. Psychiatr Res. 2011, 45, 143–149. [Google Scholar] [CrossRef]
- Jokinen, J.; Carlborg, A.; Martensson, B.; Forslund, K.; Nordstrom, A.L.; Nordstrom, P. DST non-suppression predicts suicide after attempted suicide. Psychiatry Res. 2007, 150, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Jokinen, J.; Nordström, A.L.; Nordström, P. ROC analysis of dexamethasone suppression test threshold in suicide prediction after attempted suicide. J. Affect Disord. 2008, 106, 145–152. [Google Scholar] [CrossRef]
- Rømer, K.; Buhl, M.; Hesse, M.; Lehmann, T.; Mulbjerg, M.; Uffe, M.; Voon, V. Impulsivity traits and addiction-related behaviors in youth. J. Behav. Addict 2018, 7, 317–330. [Google Scholar] [CrossRef] [PubMed]
- Cyders, M.A.; Smith, G.T.; Spillane, N.S.; Fischer, S.; Annus, A.M.; Peterson, C. Integration of impulsivity and positive mood to predict risky behavior: Development and validation of a measure of positive urgency. Psychol. Assess 2007, 19, 107–118. [Google Scholar] [CrossRef]
- Windfuhr, K.; Kapur, N. Suicide and mental illness: A clinical review of 15 years findings from the UK National Confidential Inquiry into Suicide. Br. Med. Bull. 2011, 100, 101–121. [Google Scholar] [CrossRef]
- Phillips, M.R. Rethinking the role of mental illness in suicide. Am. J. Psychiatry 2010, 167, 731–733. [Google Scholar] [CrossRef] [PubMed]
- Boksa, P. Smoking, psychiatric illness and the brain. J. Psychiatry Neurosci. 2017, 42, 147–149. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Milena, A.; Martínez-Fernández, M.L.; Redondo-Olmedilla, M.; Alvárez, C.; Jiménez, I.; Mesa, I. Motivaciones para el consumo de tabaco entre los adolescentes de un instituto urbano. Gac. Sanit. 2012, 26, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Abarca, C.; Gheza, C.; Coda, C.; Elicer, B. Revisión de literatura para identificar escalas estandarizadas de evaluación del riesgo suicida en adultos usuarios de atención primaria de salud. Medwave 2018, 18, e7246. [Google Scholar] [CrossRef]
- Grupo de trabajo de la Guía de Práctica Clínica de Prevención y Tratamiento de la Conducta Suicida. Guía de Práctica Clínica de Prevención y Tratamiento de la Conducta Suicida. Plan de Calidad para el Sistema Nacional de Salud del Ministerio de Sanidad, Política Social e Igualdad. Agencia de Evaluación de Tecnologías Sanitarias de Galicia (Avalia-t). 2012. Available online: https://portal.guiasalud.es/wp-content/uploads/2019/01/GPC_481_Conducta_Suicida_Avaliat_compl.pdf (accessed on 17 June 2020).
- Rangel-Garzón, C.X.; Suárez-Beltrán, M.F.; Escobar-Córdoba, F. Escalas de evaluación de riesgo suicida en atención primaria. Rev. Fac. Med. 2015, 63, 707–716. [Google Scholar] [CrossRef]
- Anonymous. The reality of risk assessment. Lancet Psychiatry 2020, 7, 1003–1004. [Google Scholar] [CrossRef]
- Navarro, N. El abordaje del suicidio: revisión de las estrategias autonómicas para su intervención. Rev. Esp. Salud Pública 2020, 94, e1–e8. [Google Scholar]




| 1st Author Year | Country | Population | Sex | Age | Follow-Up (Years) | Sample | Suicidal Behaviours | NOS Quality |
|---|---|---|---|---|---|---|---|---|
| Beard 2011 | USA | Pesticide applicators | Both | >18 | 13.3 | 81,998 | Suicide | 8 |
| Berlin 2015 | USA | General | Both | >18 | 3.5 | 34,653 | Attempt | 9 |
| Clarke 2010 | USA | General | Both | 18–54 | 12 | 1292 | Ideation | 9 |
| Doll 1994 | Britain | Doctors | Male | >35 | 40 | 10,812 | Suicide | 5 |
| Evins 2017 | Finland | Twins | Both | >18 | 6 | 32,564 | Suicide | 8 |
| Friberg 1973 | Switzerland | Twins | Both | >36 | 11 | 17,849 | Suicide | 7 |
| Hemenway 1993 | USA | Nurses | Female | 30–55 | 12 | 107,083 | Suicide | 6 |
| Iwasaki 2005 | Japan | General | Male | >40 | 10 | 45,209 | Suicide | 8 |
| Jee 2011 | Korea | General | Both | 30–95 | 14 | 1,234,927 | Suicide | 8 |
| Kang 2014 | Korea | General | Both | >65 | 2.4 | 909 | Ideation | 9 |
| Kessler 2009 | USA | General | Both | 15–54 | 13 | 5001 | I/P/A | 9 |
| Leistikow 2000 | USA | General | Both | >18 | 5 | 82,461 | Suicide | 9 |
| Lucas 2013 | USA | Health professionals | Both | >25 | 32 | 253,033 | Suicide | 7 |
| Miller 2000a | USA | Army soldiers | Male | >17 | 10 | 314,402 | Suicide | 7 |
| Miller 2000b | USA | Health professionals | Male | 40–75 | 8 | 51,529 | Suicide | 7 |
| Paffenbarger 1994 | USA | Harvard alumni | Male | 35–74 | 27 | 21,569 | Suicide | 6 |
| Rantakallio 1995 | Finland | Pregnant women | Female | 14–49 | 28 | 11,994 | Suicide | 7 |
| Riala 2009 | Finland | General | Both | 14–31 | 17 | 8332 | Attempt | 8 |
| Sonderman 2014 | USA | General | Both | 40–79 | 9 | 73,422 | Suicide | 8 |
| Tverdal 1993 | Norway | General | Both | 35–49 | 13.3 | 68,825 | Suicide | 9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Echeverria, I.; Cotaina, M.; Jovani, A.; Mora, R.; Haro, G.; Benito, A. Proposal for the Inclusion of Tobacco Use in Suicide Risk Scales: Results of a Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 6103. https://doi.org/10.3390/ijerph18116103
Echeverria I, Cotaina M, Jovani A, Mora R, Haro G, Benito A. Proposal for the Inclusion of Tobacco Use in Suicide Risk Scales: Results of a Meta-Analysis. International Journal of Environmental Research and Public Health. 2021; 18(11):6103. https://doi.org/10.3390/ijerph18116103
Chicago/Turabian StyleEcheverria, Iván, Miriam Cotaina, Antonio Jovani, Rafael Mora, Gonzalo Haro, and Ana Benito. 2021. "Proposal for the Inclusion of Tobacco Use in Suicide Risk Scales: Results of a Meta-Analysis" International Journal of Environmental Research and Public Health 18, no. 11: 6103. https://doi.org/10.3390/ijerph18116103
APA StyleEcheverria, I., Cotaina, M., Jovani, A., Mora, R., Haro, G., & Benito, A. (2021). Proposal for the Inclusion of Tobacco Use in Suicide Risk Scales: Results of a Meta-Analysis. International Journal of Environmental Research and Public Health, 18(11), 6103. https://doi.org/10.3390/ijerph18116103







