Gender Differences in Prevalence and Risk Factors for Hypertension among Adult Populations: A Cross-Sectional Study in Indonesia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Study Design
2.2. Dependent Variables
2.3. Independent Variables
2.4. Ethical Considerations
2.5. Statistical Analysis
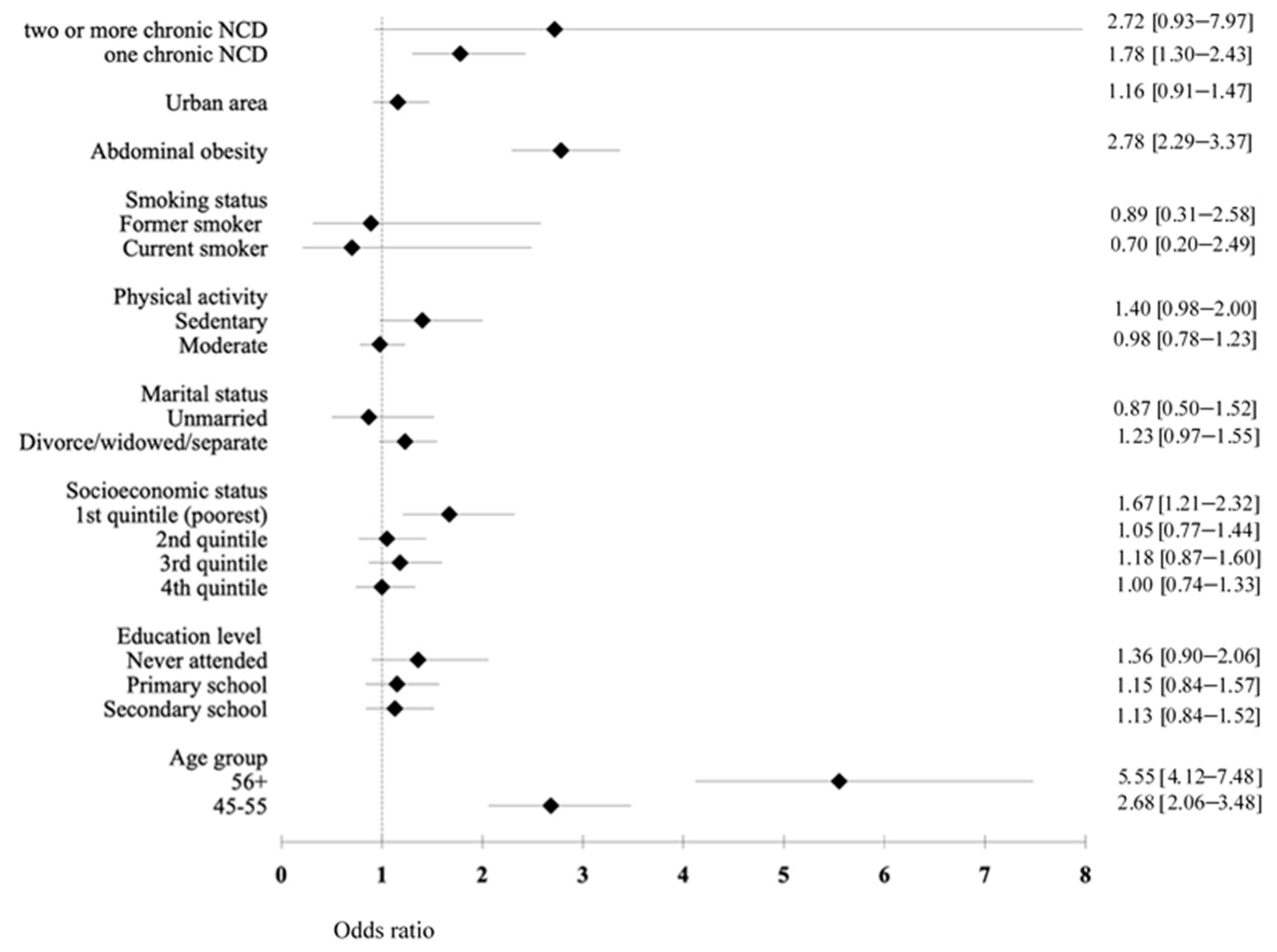
3. Results
4. Discussion
4.1. Gender Differences and Determinants of Hypertension
4.1.1. Biomedical Factors
4.1.2. Behavioral Factors
4.1.3. Sociodemographic Factors
4.2. Public Health Implications
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Noncommunicable Diseases Country Profiles. 2018. Available online: https://www.who.int/nmh/publications/ncd-profiles-2018/en/ (accessed on 26 October 2020).
- WHO. The Top 10 Causes of Death. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 26 October 2020).
- Haldar, R.N. Global Brief on Hypertension: Silent Killer, Global Public Health Crisis. Indian J. Phys. Med. Rehabil. 2013, 24, 2. [Google Scholar] [CrossRef]
- Oliva, R.V. A review on the status of hypertension in six Southeast Asian Countries. Hypertens. J. 2019, 5, 45–48. [Google Scholar] [CrossRef]
- Ministry of Health of Indonesia. Riset Kesehatan Dasar 2013 (Basic Health Research 2013). Available online: https://www.kemkes.go.id/resources/download/general/Hasil%20Riskesdas%202013.pdf (accessed on 28 October 2020).
- Everett, B.; Zajacova, A. Gender Differences in Hypertension and Hypertension Awareness Among Young Adults. Biodemogr. Soc. Biol. 2015, 61, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.M.; Kim, H.C.; Kang, D.R. Sex differences in hypertension prevalence and control: Analysis of the 2010-2014 Korea National Health and Nutrition Examination Survey. PLoS ONE 2017, 12, e0178334. [Google Scholar] [CrossRef] [PubMed]
- Santosa, A.; Zhang, Y.; Weinehall, L.; Zhao, G.; Wang, N.; Zhao, Q.; Wang, W.; Ng, N. Gender differences and determinants of prevalence, awareness, treatment and control of hypertension among adults in China and Sweden. BMC Public Health 2020, 20, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.J.L.; Jones, D.W.; Materson, B.J.; Oparil, S.; Wright, J.J.T.; et al. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003, 42, 1206–1252. [Google Scholar] [CrossRef] [PubMed]
- Ridha, A.; Hanim, D.; Suminah, S. Relationship between intake of fruits and vegetables toward hypertension among elderly in Yogyakarta. Bali Med. J. 2019, 8, 773–777. [Google Scholar] [CrossRef]
- Pangastuti, H.S.; Perdana, M.; Wati, D.A.; Melati, H.I.T.; Latifah, R. The Difference of Sodium Intake, Physical Activities and Psychological Problems of Patients Suffering from Hypertension in Rural and Urban Areas. Indones. Nurs. J. Educ. Clin. 2018, 3, 71–78. [Google Scholar] [CrossRef]
- Bantas, K.; Gayatri, D. Gender and Hypertension (Data analysis of The Indonesia Basic Health Research 2007). J. Epidemiol. Kesehat. Indones. 2019, 3, 7–18. [Google Scholar] [CrossRef]
- Hussain, M.A.; Al Mamun, A.; Reid, C.; Huxley, R.R. Prevalence, Awareness, Treatment and Control of Hypertension in Indonesian Adults Aged ≥40 Years: Findings from the Indonesia Family Life Survey (IFLS). PLoS ONE 2016, 11, e0160922. [Google Scholar] [CrossRef]
- Peltzer, K.; Pengpid, S. The Prevalence and Social Determinants of Hypertension among Adults in Indonesia: A Cross-Sectional Population-Based National Survey. Int. J. Hypertens. 2018, 2018, 1–9. [Google Scholar] [CrossRef]
- Dewi, F.S.; Choiriyyah, I.; Indriyani, C.; Wahab, A.; Lazuardi, L.; Nugroho, A.; Susetyowati, S.; Harisaputra, R.K.; Santi, R.; Lestari, S.K.; et al. Designing and collecting data for a longitudinal study: The Sleman Health and Demographic Surveillance System (HDSS). Scand. J. Public Health 2017, 46, 704–710. [Google Scholar] [CrossRef]
- Setyopranoto, I.; Bayuangga, H.F.; Panggabean, A.S.; Alifaningdyah, S.; Lazuardi, L.; Dewi, F.S.T.; Malueka, R.G. Prevalence of Stroke and Associated Risk Factors in Sleman District of Yogyakarta Special Region, Indonesia. Stroke Res. Treat. 2019, 2019, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Filmer, D.; Pritchett, L.H. Estimating Wealth Effects Without Expenditure Data--Or Tears: An Application to Educational Enrollments in States of India. Demography 2001, 38, 115–132. [Google Scholar] [CrossRef] [PubMed]
- Vyas, S.; Kumaranayake, L. Constructing socio-economic status indices: How to use principal components analysis. Health Policy Plan. 2006, 21, 459–468. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Physical Activity Questionnaire (GPAQ) Analysis Guide. Available online: https://www.who.int/ncds/surveillance/steps/resources/GPAQ_Analysis_Guide.pdf (accessed on 10 November 2020).
- Jiang, S.-Z.; Lu, W.; Zong, X.-F.; Ruan, H.-Y.; Liu, Y. Obesity and hypertension. Exp. Ther. Med. 2016, 12, 2395–2399. [Google Scholar] [CrossRef] [PubMed]
- Khader, Y.; Batieha, A.; Jaddou, H.; Rawashdeh, S.I.; El-Khateeb, M.; Hyassat, D.; Khader, A.; Ajlouni, K. Hypertension in Jordan: Prevalence, Awareness, Control, and Its Associated Factors. Int. J. Hypertens. 2019, 2019, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Van, N.B.; Vo, H.-L.; Van, T.B.; Anh, H.N.S.; Minh, H.T.; Nam, K.D.; Tri, T.N.; Show, P.L.; Nga, V.T.; Raj, D.B.T.G.; et al. Prevalence and Risk Factors of Hypertension in the Vietnamese Elderly. High Blood Press. Cardiovasc. Prev. 2019, 26, 239–246. [Google Scholar] [CrossRef]
- Lee, H.S.; Park, Y.-M.; Han, K.; Yang, J.-H.; Lee, S.; Lee, S.; Yoo, S.; Kim, S.R. Obesity-related hypertension: Findings from The Korea National Health and Nutrition Examination Survey 2008–2010. PLoS ONE 2020, 15, e0230616. [Google Scholar] [CrossRef]
- Ghosh, S.; Mukhopadhyay, S.; Barik, A. Sex differences in the risk profile of hypertension: A cross-sectional study. BMJ Open 2016, 6, e010085. [Google Scholar] [CrossRef]
- Li, G.; Wang, H.; Wang, K.; Wang, W.; Dong, F.; Qian, Y.; Gong, H.; Hui, C.; Xu, G.; Li, Y.; et al. The association between smoking and blood pressure in men: A cross-sectional study. BMC Public Health 2017, 17, 797. [Google Scholar] [CrossRef]
- Daştan, I.; Erem, A.; Çetinkaya, V. Urban and rural differences in hypertension risk factors in Turkey. Anatol. J. Cardiol. 2017, 18, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Slovic, P. What does it mean to know a cumulative risk?: Adolescents’ perceptions of short-term and long-term consequences of smoking. J. Behav. Decis. Mak. 2000, 13, 259–266. [Google Scholar] [CrossRef]
- Kale, D.; Gilbert, H.M.; Sutton, S. Are predictors of making a quit attempt the same as predictors of 3-month abstinence from smoking? Findings from a sample of smokers recruited for a study of computer-tailored smoking cessation advice in primary care. Addiction 2015, 110, 1653–1664. [Google Scholar] [CrossRef] [PubMed]
- Leng, B.; Jin, Y.; Li, G.; Chen, L.; Jin, N. Socioeconomic status and hypertension: A meta-analysis. J. Hypertens. 2015, 33, 221–229. [Google Scholar] [CrossRef] [PubMed]
- Brummett, B.H.; Babyak, M.A.; Jiang, R.; Huffman, K.M.; Kraus, W.E.; Singh, A.; Hauser, E.R.; Siegler, I.C.; Williams, R.B. Systolic Blood Pressure and Socioeconomic Status in a large multi-study population. SSM Popul. Health 2019, 9, 100498. [Google Scholar] [CrossRef] [PubMed]
- Falah, F. Javanese women in hybridism (a cross-cultural feminist psychology). J. Psikol. Proy. 2009, 4, 15–28. [Google Scholar]
- Tuoyire, D.A.; Ayetey, H. Gender differences in the association between marital status and hypertension in Ghana. J. Biosoc. Sci. 2018, 51, 313–334. [Google Scholar] [CrossRef]
- Nyarko, S.H. Prevalence and Sociodemographic Determinants of Hypertension History among Women in Reproductive Age in Ghana. Int. J. Hypertens. 2016, 2016, 1–6. [Google Scholar] [CrossRef]
- Ramezankhani, A.; Azizi, F.; Hadaegh, F. Associations of marital status with diabetes, hypertension, cardiovascular disease and all-cause mortality: A long term follow-up study. PLoS ONE 2019, 14, e0215593. [Google Scholar] [CrossRef]
- Nisak, S.; Sugiharti, L. Gender inequality and women poverty in Indonesia. Int. J. Innov. Creat. Chang. 2020, 11, 375–387. [Google Scholar]
- Parker, L. The theory and context of the stigmatisation of widows and divorcees (janda) in Indonesia. Indones. Malay World 2015, 44, 7–26. [Google Scholar] [CrossRef]
- WHO. Global Action Plan for the Prevention and Control of NCDs 2013–2020. Available online: https://www.who.int/publications/i/item/9789241506236 (accessed on 26 October 2020).
- Jeet, G.; Thakur, J.S.; Prinja, S.; Singh, M. Community health workers for non-communicable diseases prevention and control in developing countries: Evidence and implications. PLoS ONE 2017, 12, e0180640. [Google Scholar] [CrossRef] [PubMed]
- Allen, L.N.; Nicholson, B.D.; Yeung, B.Y.T.; Goiana-Da-Silva, F. Implementation of non-communicable disease policies: A geopolitical analysis of 151 countries. Lancet Glob. Health 2020, 8, e50–e58. [Google Scholar] [CrossRef]
- WHO. Multisectoral Coordination Mechanisms and Responses to Noncommunicable Diseases in South-East Asia: Where are We in 2018? Available online: https://apps.who.int/iris/handle/10665/326082 (accessed on 4 January 2021).


| Characteristics | Total. N (%) | Men. N (%) | Women N (%) | p-Value |
|---|---|---|---|---|
| Age group | ||||
| 18–39 years | 867 (20) | 282 (16.9) | 585 (22) | 0.000 |
| 40–55 years | 1881 (43.5) | 696 (41.8) | 1185 (44.5) | |
| ≥56 years | 1580 (36.5) | 689 (41.3) | 891 (33.5) | |
| Marital status | ||||
| Married | 3469 (80.2) | 1395 (83.7) | 2074 (77.9) | 0.000 |
| Divorce | 663 (15.3) | 148 (8.9) | 515 (19.4) | |
| Unmarried | 196 (4.5) | 124 (7.4) | 72 (2.7) | |
| Education level | ||||
| University/diploma | 642 (14.8) | 252 (15.1) | 390 (14.7) | 0.000 |
| Secondary school | 1618 (37.4) | 669 (40.1) | 949 (35.7) | |
| Primary school | 1715 (39.6) | 656 (39.4) | 1059 (39.8) | |
| Never attended school | 353 (8.2) | 90 (5.4) | 263 (9.9) | |
| Socioeconomic status | ||||
| Q5 (richest group) | 778 (18) | 310 (18.6) | 468 (17.6) | 0.918 |
| Q4 | 911 (21.1) | 351 (21.1) | 560 (21) | |
| Q3 | 915 (21.1) | 354 (21.2) | 561 (21.1) | |
| Q2 | 856 (19.8) | 324 (19.4) | 532 (20) | |
| Q1 (poorest group) | 868 (20.1) | 328 (19.7) | 540 (20.3) | |
| Physical activity | ||||
| High | 3197 (73.9) | 1175 (70.5) | 2022 (76) | 0.000 |
| Moderate | 765 (17.7) | 289 (17.3) | 476 (17.9) | |
| Low | 366 (8.5) | 203 (12.2) | 163 (6.1) | |
| Smoking status | ||||
| Never smoke | 3036 (70.2) | 403 (24.2) | 2633 (99) | 0.000 |
| Current smoker | 888 (20.5) | 876 (52.6) | 12 (0.5) | |
| Former smoker | 404 (9.3) | 388 (23.3) | 16 (0.6) | |
| Abdominal Obesity | 2197 (50.8) | 446 (26.8) | 1751 (65.8) | 0.000 |
| Urban area | 3611 (83.4) | 1370 (82.2) | 2241 (84.2) | 0.080 |
| Chronic NCD | ||||
| None | 3923 (90.6) | 1489 (89.3) | 2434 (91.5) | 0.038 |
| One chronic NCD | 366 (8.5) | 158 (9.5) | 208 (7.8) | |
| Two or more chronic NCDs | 39 (0.9) | 20 (1.2) | 19 (0.7) | |
| Hypertension | 1705 (39.4) | 692 (41.5) | 1013 (38.1) | 0.024 |
| Characteristics | Without Hypertension (N = 2623) | With Hypertension (N = 1705) | p-Value |
|---|---|---|---|
| Age group | |||
| 18–39 years | 722 (27.5) | 145 (8.5) | 0.000 |
| 40–55 years | 1192 (45.4) | 689 (40.4) | |
| ≥56 years | 709 (27) | 871 (51.1) | |
| Marital status | |||
| Married | 2177 (83) | 1292 (75.8) | 0.000 |
| Divorced | 310 (11.8) | 353 (20.7) | |
| Unmarried | 136 (5.2) | 60 (3.5) | |
| Education level | |||
| University | 403 (15.4) | 239 (14) | 0.000 |
| Secondary | 1061 (40.5) | 557 (32.7) | |
| Primary | 985 (37.6) | 730 (42.8) | |
| Never attended school | 174 (6.6) | 179 (10.5) | |
| Socioeconomic status | |||
| Q5 (richest group) | 473 (18) | 305 (17.9) | 0.011 |
| Q4 | 566 (21.6) | 345 (20.2) | |
| Q3 | 557 (21.2) | 358 (21) | |
| Q2 | 544 (20.7) | 312 (18.3) | |
| Q1 (poorest group) | 483 (18.4) | 385 (22.6) | |
| Physical activity | |||
| High | 1987 (75.8) | 1210 (71) | 0.000 |
| Moderate | 450 (17.2) | 315 (18.5) | |
| Low | 186 (7.1) | 180 (10.6) | |
| Smoking status | |||
| Never smoke | 1851 (70.6) | 1185 (69.5) | 0.000 |
| Current smoker | 575 (21.9) | 313 (18.4) | |
| Former smoker | 197 (7.5) | 207 (12.1) | |
| Abdominal Obesity | 1151 (43.9) | 1046 (61.4) | 0.000 |
| Urban area | 2171 (82.8) | 1440 (84.5) | 0.144 |
| Chronic NCD | |||
| None | 2454 (93.6) | 1469 (86.2) | 0.000 |
| One chronic NCD | 157 (6) | 209 (12.3) | |
| Two or more chronic NCDs | 12 (0.5) | 27 (1.6) | |
| Variables | Adjusted OR (95% CI) |
|---|---|
| Men | 1.77 (1.40–2.23) *** |
| Age group | |
| 40–55 years | 2.67 (2.16–3.29) *** |
| ≥56 years | 5.18 (4.11–6.53) *** |
| Education level | |
| Secondary school | 1.01 (0.81–1.25) |
| Primary school | 0.99 (0.78–1.26) |
| Never attended school | 1.06 (0.76–1.47) |
| Socioeconomic status | |
| 4th quintile (richest) | 1.07 (0.86–1.34) |
| 3rd quintile | 1.19 (0.95–1.50) |
| 2nd quintile | 1.12 (0.88–1.43) |
| 1st quintile (poorest) | 1.41 (1.09–1.81) ** |
| Marital status | |
| Divorced/widowed/separated | 1.29 (1.06–1.56) ** |
| Unmarried | 1.16 (0.82–1.64) |
| Physical activity | |
| Moderate | 1.06 (0.89–1.26) |
| Low | 1.23 (0.97–1.56) |
| Smoking status | |
| Current smoker | 0.76 (0.59–0.98) * |
| Former smoker | 1.15 (0.87–1.54) |
| Abdominal obesity | 2.64 (2.27–3.06) *** |
| Urban area | 1.15 (0.96–1.38) |
| Presence of chronic NCD | |
| One chronic NCD | 1.68 (1.33–2.12) *** |
| Two or more chronic NCDs | 2.31 (1.13–4.71) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Defianna, S.R.; Santosa, A.; Probandari, A.; Dewi, F.S.T. Gender Differences in Prevalence and Risk Factors for Hypertension among Adult Populations: A Cross-Sectional Study in Indonesia. Int. J. Environ. Res. Public Health 2021, 18, 6259. https://doi.org/10.3390/ijerph18126259
Defianna SR, Santosa A, Probandari A, Dewi FST. Gender Differences in Prevalence and Risk Factors for Hypertension among Adult Populations: A Cross-Sectional Study in Indonesia. International Journal of Environmental Research and Public Health. 2021; 18(12):6259. https://doi.org/10.3390/ijerph18126259
Chicago/Turabian StyleDefianna, Selly Ruth, Ailiana Santosa, Ari Probandari, and Fatwa Sari Tetra Dewi. 2021. "Gender Differences in Prevalence and Risk Factors for Hypertension among Adult Populations: A Cross-Sectional Study in Indonesia" International Journal of Environmental Research and Public Health 18, no. 12: 6259. https://doi.org/10.3390/ijerph18126259
APA StyleDefianna, S. R., Santosa, A., Probandari, A., & Dewi, F. S. T. (2021). Gender Differences in Prevalence and Risk Factors for Hypertension among Adult Populations: A Cross-Sectional Study in Indonesia. International Journal of Environmental Research and Public Health, 18(12), 6259. https://doi.org/10.3390/ijerph18126259






