Association of Rotating Night Shift Work with Body Fat Percentage and Fat Mass Index among Female Steelworkers in North China
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Anthropometric Measurements
2.3. Assessment of Night Shift Work
2.4. Assessment of Covariates
2.5. Statistical Analysis
3. Results
3.1. General Characteristics of the Participants
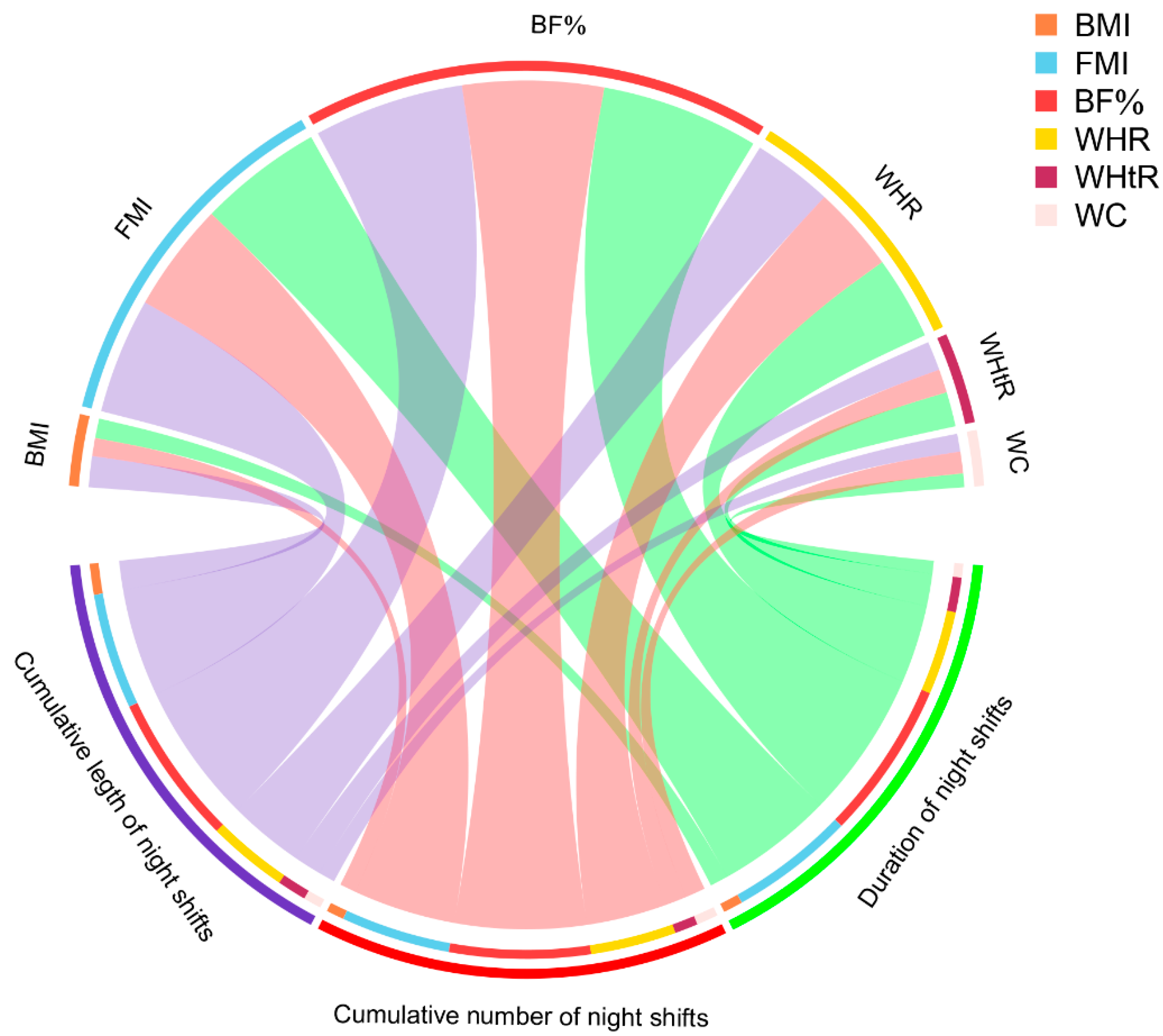
3.2. Different Exposure Metrics of Night Shift Work and Anthropometric Measures
3.3. Sensitivity Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Guo, Y.; Liu, Y.; Huang, X.; Rong, Y.; He, M.; Wang, Y.; Yuan, J.; Wu, T.; Chen, W. The Effects of Shift Work on Sleeping Quality, Hypertension and Diabetes in Retired Workers. PLoS ONE 2013, 8, e71107. [Google Scholar] [CrossRef]
- Sun, M.; Feng, W.; Wang, F.; Li, P.; Li, Z.; Li, M.; Tse, G.; Vlaanderen, J.; Vermeulen, R.; Tse, L.A. Meta-analysis on shift work and risks of specific obesity types. Obes. Rev. 2018, 19, 28–40. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Chair, S.Y.; Lo, S.H.S.; Chau, J.P.-C.; Schwade, M.; Zhao, X. Association between shift work and obesity among nurses: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2020, 112, 103757. [Google Scholar] [CrossRef]
- Haslam, D.W.; James, W.P. Obesity. Lancet 2005, 366, 1197–1209. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, L.; Qu, W. New national data show alarming increase in obesity and noncommunicable chronic diseases in China. Eur. J. Clin. Nutr. 2017, 71, 149–150. [Google Scholar] [CrossRef] [PubMed]
- Poirier, P.; Giles, T.D.; Bray, G.A.; Hong, Y.; Stern, J.S.; Pi-Sunyer, F.X.; Eckel, R.H. Obesity and Cardiovascular Disease: Pathophysiology, Evaluation, and Effect of Weight Loss: An update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation 2006, 113, 898–918. [Google Scholar] [CrossRef] [PubMed]
- Lauby-Secretan, B.; Scoccianti, C.; Loomis, D.; Grosse, Y.; Bianchini, F.; Straif, K. International Agency for Research on Cancer Handbook Working Group. Body Fatness and Cancer—Viewpoint of the IARC Working Group. N. Engl. J. Med. 2016, 375, 794–798. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Ambrosi, J.; Silva, C.; Galofré, J.C.; Escalada, J.; Santos, S.; Millán, D.; Vila, N.; Ibañez, P.; Gil, M.J.; Valentí, V.; et al. Body mass index classification misses subjects with increased cardiometabolic risk factors related to elevated adiposity. Int. J. Obes. 2012, 36, 286–294. [Google Scholar] [CrossRef]
- VanItallie, T.B.; Yang, M.U.; Heymsfield, S.B.; Funk, R.C.; Boileau, R.A. Height-normalized indices of the body’s fat-free mass and fat mass: Potentially useful indicators of nutritional status. Am. J. Clin. Nutr. 1990, 52, 953–959. [Google Scholar] [CrossRef]
- Liu, P.; Ma, F.; Lou, H.; Liu, Y. The utility of fat mass index vs. body mass index and percentage of body fat in the screening of metabolic syndrome. BMC Public Health 2013, 13, 629. [Google Scholar] [CrossRef]
- Ramírez-Vélez, R.; Correa-Bautista, J.E.; Sanders-Tordecilla, A.; Ojeda-Pardo, M.L.; Cobo-Mejía, E.A.; Castellanos-Vega, R.D.P.; García-Hermoso, A.; González-Jiménez, E.; Schmidt-RioValle, J.; González-Ruíz, K. Percentage of Body Fat and Fat Mass Index as a Screening Tool for Metabolic Syndrome Prediction in Colombian University Students. Nutrients 2017, 9, 1009. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.-C.; Arthur, R.; Iyengar, N.M.; Kamensky, V.; Xue, X.; Wassertheil-Smoller, S.; Allison, M.A.; Shadyab, A.H.; Wild, R.A.; Sun, Y.; et al. Association between regional body fat and cardiovascular disease risk among postmenopausal women with normal body mass index. Eur. Heart J. 2019, 40, 2849–2855. [Google Scholar] [CrossRef] [PubMed]
- Vyas, M.V.; Garg, A.X.; Iansavichus, A.V.; Costella, J.; Donner, A.; Laugsand, L.E.; Janszky, I.; Mrkobrada, M.; Parraga, G.; Hackam, D.G. Shift work and vascular events: Systematic review and meta-analysis. BMJ 2012, 345, e4800. [Google Scholar] [CrossRef]
- Torquati, L.; Mielke, G.I.; Brown, W.J.; Kolbe-Alexander, T. Shift work and the risk of cardiovascular disease. A systematic review and meta-analysis including dose–response relationship. Scand. J. Work Environ. Health 2017, 44, 229–238. [Google Scholar] [CrossRef]
- Schiavo-Cardozo, D.; Lima, M.M.O.; Pareja, J.C.; Geloneze, B. Appetite-regulating hormones from the upper gut: Disrupted control of xenin and ghrelin in night workers. Clin. Endocrinol. 2013, 79, 807–811. [Google Scholar] [CrossRef] [PubMed]
- Souza, B.B.; Monteze, N.M.; de Oliveira, F.L.P.; De Oliveira, J.M.; De Freitas, S.N.; Neto, R.M.D.N.; Sales, M.L.; Souza, G.G.L. Lifetime shift work exposure: Association with anthropometry, body composition, blood pressure, glucose and heart rate variability. Occup. Environ. Med. 2015, 72, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Peplonska, B.; Bukowska, A.; Sobala, W. Association of Rotating Night Shift Work with BMI and Abdominal Obesity among Nurses and Midwives. PLoS ONE 2015, 10, e0133761. [Google Scholar] [CrossRef]
- Zhang, S.; Wang, Y.; Wang, Z.; Wang, H.; Xue, C.; Li, Q.; Guan, W.; Yuan, J. Rotating night shift work and non-alcoholic fatty liver disease among steelworkers in China: A cross-sectional survey. Occup. Environ. Med. 2020, 77, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Wang, Y.; Li, Q.; Wang, Z.; Wang, H.; Xue, C.; Zhu, Y.; Guan, W.; Yuan, J. Different exposure metrics of rotating night shift work and hyperhomocysteinaemia among Chinese steelworkers: A cross-sectional study. BMJ Open 2020, 10, e041576. [Google Scholar] [CrossRef]
- Zhang, S.; Wang, Y.; Zhu, Y.; Li, X.; Song, Y.; Yuan, J. Rotating Night Shift Work, Exposure to Light at Night, and Glomerular Filtration Rate: Baseline Results from a Chinese Occupational Cohort. Int. J. Environ. Res. Public Health 2020, 17, 9035. [Google Scholar] [CrossRef]
- Xiao, M.Y.; Wang, Z.Y.; Fan, H.M.; Che, C.L.; Lu, Y.; Cong, L.X.; Gao, X.J.; Liu, Y.J.; Yuan, J.X.; Li, X.M.; et al. Relationship between shift work and overweight/obesity in male steel workers. Zhonghua Liu Xing Bing Xue Za Zhi = Zhonghua Liuxingbingxue Zazhi 2016, 37, 1468–1472. [Google Scholar]
- He, H.; Pan, L.; Pa, L.; Cui, Z.; Ren, X.; Wang, D.; Liu, F.; Wang, X.; Du, J.; Wang, H.; et al. Data Resource Profile: The China National Health Survey (CNHS). Int. J. Epidemiol. 2018, 47, 1734–1735f. [Google Scholar] [CrossRef] [PubMed]
- Zhou, B.-F. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults—study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed. Environ. Sci. 2002, 15, 83–96. [Google Scholar]
- Garde, A.H.; Hansen, J.; Kolstad, H.A.; Larsen, A.D.; Hansen, Å.M. How do different definitions of night shift affect the exposure assessment of night work? Chronobiol. Int. 2016, 33, 595–598. [Google Scholar] [CrossRef] [PubMed]
- Rimm, E.B.; Giovannucci, E.L.; Stampfer, M.J.; Colditz, G.A.; Litin, L.B.; Willett, W.C. Reproducibility and Validity of an Expanded Self-Administered Semiquantitative Food Frequency Questionnaire among Male Health Professionals. Am. J. Epidemiol. 1992, 135, 1114–1126. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Heianza, Y.; Sun, D.; Huang, T.; Ma, W.; Rimm, E.B.; Manson, J.E.; Hu, F.B.; Willett, W.C.; Qi, L. Improving adherence to healthy dietary patterns, genetic risk, and long term weight gain: Gene-diet interaction analysis in two prospective cohort studies. BMJ 2018, 360, j5644. [Google Scholar] [CrossRef]
- Celis-Morales, C.A.; Perez-Bravo, F.; Ibañez, L.; Salas, C.; Bailey, M.E.S.; Gill, J.M.R. Objective vs. Self-Reported Physical Activity and Sedentary Time: Effects of Measurement Method on Relationships with Risk Biomarkers. PLoS ONE 2012, 7, e36345. [Google Scholar] [CrossRef] [PubMed]
- Soldatos, C.R.; Dikeos, D.G.; Paparrigopoulos, T.J. Athens Insomnia Scale: Validation of an instrument based on ICD-10 criteria. J. Psychosom. Res. 2000, 48, 555–560. [Google Scholar] [CrossRef]
- Stamatakis, E.; Davis, M.; Stathi, A.; Hamer, M. Associations between multiple indicators of objectively-measured and self-reported sedentary behaviour and cardiometabolic risk in older adults. Prev. Med. 2012, 54, 82–87. [Google Scholar] [CrossRef]
- McFadden, E.; Jones, M.; Schoemaker, M.; Ashworth, A.; Swerdlow, A. The Relationship Between Obesity and Exposure to Light at Night: Cross-Sectional Analyses of Over 100,000 Women in the Breakthrough Generations Study. Am. J. Epidemiol. 2014, 180, 245–250. [Google Scholar] [CrossRef]
- Davis, S.; Mirick, D.K.; Stevens, R.G. Night shift work, light at night, and risk of breast cancer. J. Natl. Cancer Inst. 2001, 93, 1557–1562. [Google Scholar] [CrossRef] [PubMed]
- Tingley, D.; Teppei, H.; Mit, Y.; Keele, L.; Imai, K. Mediation: R Package for Causal Mediation Analysis. J. Stat. Softw. 2014, 59. [Google Scholar] [CrossRef]
- Xu, T.; Liu, J.; Liu, J.; Zhu, G.; Han, S. Relation between metabolic syndrome and body compositions among Chinese adolescents and adults from a large-scale population survey. BMC Public Health 2017, 17, 337. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.C.; Hoe, V.C.W.; Darus, A.; Bhoo-Pathy, N. Association between night-shift work, sleep quality and metabolic syndrome. Occup. Environ. Med. 2018, 75, 716–723. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, K.; Sakuraya, A.; Kawakami, N.; Imamura, K.; Ando, E.; Asai, Y.; Eguchi, H.; Kobayashi, Y.; Nishida, N.; Arima, H.; et al. Work-related psychosocial factors and metabolic syndrome onset among workers: A systematic review and meta-analysis. Obes. Rev. 2018, 19, 1557–1568. [Google Scholar] [CrossRef]
- Oliveros, E.; Somers, V.K.; Sochor, O.; Goel, K.; Lopez-Jimenez, F. The Concept of Normal Weight Obesity. Prog. Cardiovasc. Dis. 2014, 56, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Borruel, S.; Moltó, J.F.; Alpañés, M.; Fernández-Durán, E.; Álvarez-Blasco, F.; Luque-Ramírez, M.; Escobar-Morreale, H.F. Surrogate Markers of Visceral Adiposity in Young Adults: Waist Circumference and Body Mass Index Are More Accurate than Waist Hip Ratio, Model of Adipose Distribution and Visceral Adiposity Index. PLoS ONE 2014, 9, e114112. [Google Scholar] [CrossRef]
- Hall, A.L.; Franche, R.L.; Koehoorn, M. Examining Exposure Assessment in Shift Work Research: A Study on Depression Among Nurses. Ann. Work Expo. Health 2018, 62, 182–194. [Google Scholar] [CrossRef]
- Ramin, C.; Devore, E.E.; Wang, W.; Pierre-Paul, J.; Wegrzyn, L.R.; Schernhammer, E.S. Night shift work at specific age ranges and chronic disease risk factors. Occup. Environ. Med. 2015, 72, 100–107. [Google Scholar] [CrossRef]
- Kogi, K. International research needs for improving sleep and health of workers. Ind. Health 2005, 43, 71–79. [Google Scholar] [CrossRef][Green Version]
- Leproult, R.; Van Cauter, E. Role of Sleep and Sleep Loss in Hormonal Release and Metabolism. Endocr. Dev. 2009, 17, 11–21. [Google Scholar] [CrossRef]
- Schmid, S.M.; Hallschmid, M.; Jauch-Chara, K.; Born, J.; Schultes, B. A single night of sleep deprivation increases ghrelin levels and feelings of hunger in normal-weight healthy men. J. Sleep Res. 2008, 17, 331–334. [Google Scholar] [CrossRef]
- Taheri, S.; Lin, L.; Austin, D.; Young, T.; Mignot, E. Short Sleep Duration Is Associated with Reduced Leptin, Elevated Ghrelin, and Increased Body Mass Index. PLoS Med. 2004, 1, e62. [Google Scholar] [CrossRef]
- Van Cauter, E.; Spiegel, K.; Tasali, E.; Leproult, R. Metabolic consequences of sleep and sleep loss. Sleep Med. 2008, 9, S23–S28. [Google Scholar] [CrossRef]
- Crispim, C.A.; Waterhouse, J.; Dâmaso, A.R.; Zimberg, I.Z.; Padilha, H.G.; Oyama, L.M.; Tufik, S.; de Mello, M.T. Hormonal appetite control is altered by shift work: A preliminary study. Metabolism 2011, 60, 1726–1735. [Google Scholar] [CrossRef] [PubMed]
- James, S.M.; Honn, K.A.; Gaddameedhi, S.; Van Dongen, H.P. Shift Work: Disrupted Circadian Rhythms and Sleep—Implications for Health and Well-being. Curr. Sleep Med. Rep. 2017, 3, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Mukherji, A.; Bailey, S.M.; Staels, B.; Baumert, T.F. The circadian clock and liver function in health and disease. J. Hepatol. 2019, 71, 200–211. [Google Scholar] [CrossRef]
- Adamovich, Y.; Rousso-Noori, L.; Zwighaft, Z.; Neufeld-Cohen, A.; Golik, M.; Kraut-Cohen, J.; Wang, M.; Han, X.; Asher, G. Circadian Clocks and Feeding Time Regulate the Oscillations and Levels of Hepatic Triglycerides. Cell Metab. 2014, 19, 319–330. [Google Scholar] [CrossRef]
- Longo, V.D.; Mattson, M.P. Fasting: Molecular Mechanisms and Clinical Applications. Cell Metab. 2014, 19, 181–192. [Google Scholar] [CrossRef]
- Chaix, A.; Zarrinpar, A.; Miu, P.; Panda, S. Time-Restricted Feeding Is a Preventative and Therapeutic Intervention against Diverse Nutritional Challenges. Cell Metab. 2014, 20, 991–1005. [Google Scholar] [CrossRef]
- Currenti, W.; Godos, J.; Castellano, S.; Mogavero, M.P.; Ferri, R.; Caraci, F.; Grosso, G.; Galvano, F. Time restricted feeding and mental health: A review of possible mechanisms on affective and cognitive disorders. Int. J. Food Sci. Nutr. 2020, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Hatori, M.; Vollmers, C.; Zarrinpar, A.; DiTacchio, L.; Bushong, E.A.; Gill, S.; Leblanc, M.; Chaix, A.; Joens, M.; Fitzpatrick, J.A.; et al. Time-Restricted Feeding without Reducing Caloric Intake Prevents Metabolic Diseases in Mice Fed a High-Fat Diet. Cell Metab. 2012, 15, 848–860. [Google Scholar] [CrossRef] [PubMed]
- Ward, L.C. Bioelectrical impedance analysis for body composition assessment: Reflections on accuracy, clinical utility, and standardisation. Eur. J. Clin. Nutr. 2019, 73, 194–199. [Google Scholar] [CrossRef] [PubMed]

| Variables | Total | Day Work | Night Shift Work | |
|---|---|---|---|---|
| n = 435 | n = 91 | n = 344 | p Value | |
| * Age (years), mean ± SD | 44.1 ± 5.0 | 44.1 ± 5.0 | 44.1 ± 5.0 | 0.937 a |
| Marital status, n (%) | 0.329 b | |||
| Married/Cohabitating | 406 (93.3) | 87 (95.6) | 319 (92.7) | |
| Single/Divorced/Widow | 29 (6.7) | 4 (4.4) | 25 (7.3) | |
| Smoking status, n (%) | 0.036 b | |||
| Nonsmoker | 390 (89.7) | 87 (95.6) | 303 (88.1) | |
| Pre-/Current smoker | 45 (10.3) | 4 (4.4) | 41 (11.9) | |
| Drinking status, n (%) | 0.053 b | |||
| Nondrinker | 399 (91.7) | 88 (96.7) | 311 (90.4) | |
| Pre-/Current drinker | 36 (8.3) | 3 (3.3) | 33 (9.6) | |
| Education level, n (%) | 0.162 b | |||
| High school or below | 339 (77.9) | 66 (72.5) | 273 (79.4) | |
| University or college | 96 (22.1) | 25 (27.5) | 71 (20.6) | |
| Ethnicity, n (%) | 0.018 b | |||
| Han | 413 (94.4) | 82 (90.1) | 331 (96.2) | |
| Others | 22 (5.1) | 9 (9.9) | 13 (3.8) | |
| Bedroom ambient light level, n (%) | 0.603 b | |||
| Darkest level | 198 (45.5) | 40 (44.0) | 158 (45.9) | |
| Middle level | 199 (45.8) | 45 (49.5) | 154 (44.8) | |
| Lightest level | 38 (8.7) | 6 (6.6) | 32 (9.3) | |
| Physical activity (MET-h/week), median (IQR) | 103.8 (82.9–126.9) | 103.8 (84.5–131.7) | 103.8 (78.9–125.8) | 0.421c |
| DASH score, mean ± SD | 22.9 ± 2.1 | 22.5 ± 2.1 | 23.0 ± 2.1 | 0.044 a |
| Sedentary behavior (h), median (IQR) | 4.0 (2.4–5.5) | 3.0 (1.6–4.6) | 4.3 (2.6–5.5) | <0.001 c |
| Sleep duration (h), mean ± SD | 6.8 ± 1.2 | 7.2 ± 1.2 | 6.7 ± 1.2 | <0.001 a |
| Insomnia, n (%) | 154 (35.4) | 33 (36.3) | 121 (35.2) | 0.847 b |
| BMI (kg/m2), mean ± SD | 23.8 ± 3.2 | 23.8 ± 3.1 | 23.8 ± 3.2 | 0.919a |
| WC (cm), mean ± SD | 83.2 ± 11.0 | 83.7 ± 11.4 | 83.0 ± 11.0 | 0.571 a |
| HC (cm), mean ± SD | 98.8 ± 7.5 | 98.3 ± 7.7 | 99.1 ± 7.5 | 0.413 a |
| WHR, mean ± SD | 0.84 ± 0.07 | 0.85 ± 0.07 | 0.84 ± 0.07 | 0.111 a |
| WHtR, mean ± SD | 0.50 ± 0.06 | 0.50 ± 0.06 | 0.51 ± 0.06 | 0.069 a |
| BF%, mean ± SD | 29.1 ± 7.9 | 27.4 ± 7.5 | 29.6 ± 7.9 | 0.022 a |
| FMI (kg/m2), mean ± SD | 7.3 ± 2.7 | 6.8 ± 2.4 | 7.7 ± 2.8 | 0.039 a |
| Menopausal status, n (%) | 0.746 b | |||
| Premenopausal | 413 (94.9) | 87 (95.6) | 326 (94.8) | |
| Postmenopausal | 22 (5.1) | 4 (4.4) | 18 (5.2) | |
| Current use of oral contraceptives, n (%) | 0.225 b | |||
| No | 409 (94.0) | 88 (96.7) | 321 (93.3) | |
| Yes | 26 (6.0) | 3 (3.3) | 23 (6.7) |
| Exposure Metrics | BMI | FMI | PBF (%) | |||
|---|---|---|---|---|---|---|
| β | p | β | p | β | p | |
| Duration of night shifts (years) | ||||||
| Day work | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) |
| Q1 (1–13) | −0.337 | 0.492 | −0.051 | 0.904 | 0.103 | 0.932 |
| Q2 (14–20) | −0.045 | 0.929 | 0.596 | 0.166 | 2.078 | 0.092 |
| Q3 (21–26) | −0.427 | 0.378 | 0.496 | 0.235 | 1.494 | 0.211 |
| Q4 (27–38) | −0.130 | 0.799 | 1.028 | 0.020 * | 3.761 | 0.003 * |
| p trend | 0.743 | 0.009 * | 0.002 * | |||
| Cumulative number of night shifts (nights) | ||||||
| Day work | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) |
| Q1 (43–1157) | −0.380 | 0.437 | -0.071 | 0.866 | 0.062 | 0.959 |
| Q2 (1158–1790) | −0.033 | 0.947 | 0.590 | 0.167 | 2.118 | 0.083 |
| Q3 (1791–2411) | −0.387 | 0.428 | 0.622 | 0.140 | 1.820 | 0.131 |
| Q4 (2412–3580) | −0.152 | 0.768 | 0.928 | 0.038 * | 3.440 | 0.007 * |
| p trend | 0.783 | 0.011 * | 0.003 * | |||
| Cumulative length of night shifts (hours) | ||||||
| Day work | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) |
| Q1 (344–9681) | −0.280 | 0.544 | 0.053 | 0.899 | 0.377 | 0.755 |
| Q2 (9682–14600) | 0.042 | 0.932 | 0.361 | 0.393 | 1.425 | 0.239 |
| Q3 (14601–19941) | −0.540 | 0.274 | 0.708 | 0.097 | 2.479 | 0.043 * |
| Q4 (19942–42960) | −0.204 | 0.691 | 0.961 | 0.031 * | 3.108 | 0.015 * |
| p trend | 0.599 | 0.011 * | 0.004 * | |||
| Average frequency of night shifts (nights/month) | ||||||
| Day work | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) |
| <3 | −0.161 | 0.725 | 0.296 | 0.438 | 0.987 | 0.386 |
| 3–7 | −0.113 | 0.841 | 0.778 | 0.093 | 2.043 | 0.146 |
| >7 | −0.343 | 0.426 | 0.862 | 0.013 * | 2.252 | 0.036 * |
| p trend | 0.429 | 0.007 * | 0.030 * | |||
| Percentage of hours on night shifts | ||||||
| Day work | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) | 0 (Ref) |
| <20% | −0.149 | 0.779 | 0.240 | 0.588 | 0.778 | 0.556 |
| 20–30% | −0.554 | 0.314 | 0.136 | 0.765 | 0.504 | 0.712 |
| >30% | −0.175 | 0.675 | 0.916 | 0.006 * | 2.464 | 0.018 * |
| p trend | 0.670 | 0.038 * | 0.013 * | |||
| Exposure Metrics | Obesity-BMI | Obesity-BF% | ||
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | |||
| Unadjusted | Adjusted | Unadjusted | Adjusted | |
| Duration of night shifts (years) | ||||
| Day work | 1.00 | 1.00 | 1.00 | 1.00 |
| Q1 (1–13) | 0.70 (0.24–2.06) | 0.71 (0.22–2.24) | 0.87 (0.34–2.22) | 0.90 (0.34–2.39) |
| Q2 (14–20) | 1.41 (0.55–3.60) | 1.66 (0.58–4.70) | 2.50 (1.12–5.58) | 2.64 (1.12–6.22) |
| Q3 (21–26) | 1.04 (0.39–2.75) | 1.06 (0.37–3.04) | 1.74 (0.77–3.97) | 1.58 (0.67–3.74) |
| Q4 (27–38) | 1.14 (0.44–2.95) | 0.95 (0.32–2.84) | 4.21 (1.97–9.02) | 3.48 (1.50–8.08) |
| p trend | 0.599 | 0.795 | <0.001 | 0.002 |
| Cumulative number of night shifts (nights) | ||||
| Day work | 1.00 | 1.00 | 1.00 | 1.00 |
| Q1 (43–1157) | 0.68 (0.23–2.01) | 0.69 (0.22–2.19) | 0.96 (0.38–2.38) | 0.99 (0.38–2.58) |
| Q2 (1158–1790) | 1.34 (0.53–3.40) | 1.60 (0.56–4.55) | 2.35 (1.06–5.23) | 2.53 (1.07–5.96) |
| Q3 (1791–2411) | 1.20 (0.46–3.11) | 1.15 (0.41–3.25) | 2.06 (0.92–4.64) | 1.80 (0.77–4.19) |
| Q4 (2412–3580) | 1.07 (0.40–2.82) | 0.89 (0.29–2.73) | 3.90 (1.80–8.42) | 3.11 (1.33–7.27) |
| p trend | 0.578 | 0.786 | <0.001 | 0.003 |
| Cumulative length of night shifts (hours) | ||||
| Day work | 1.00 | 1.00 | 1.00 | 1.00 |
| Q1 (344–9681) | 0.81 (0.29–2.27) | 0.80 (0.26–2.44) | 1.07 (0.44–2.61) | 1.07 (0.42–2.71) |
| Q2 (9682–14600) | 1.18 (0.46–3.07) | 1.35 (0.47–3.82) | 1.90 (0.84–4.29) | 1.93 (0.81–4.56) |
| Q3 (14601–19941) | 1.22 (0.47–3.15) | 1.18 (0.41–3.37) | 2.39 (1.07–5.31) | 2.09 (0.90–4.86) |
| Q4 (19942–42960) | 1.07 (0.40–2.82) | 0.92 (0.30–2.83) | 3.90 (1.80–8.42) | 3.35 (1.43–7.81) |
| p trend | 0.647 | 0.821 | <0.001 | 0.001 |
| Average frequency of night shifts (nights/month) | ||||
| Day work | 1.00 | 1.00 | 1.00 | 1.00 |
| <3 | 1.13 (0.45–2.81) | 1.15 (0.44–3.03) | 1.34 (0.60–3.04) | 1.34 (0.56–3.14) |
| 3–7 | 1.14 (0.38–3.40) | 1.22 (0.37–4.05) | 2.31 (0.95–5.60) | 2.25 (0.87–5.81) |
| >7 | 1.01 (0.43–2.34) | 0.94 (0.36–2.44) | 2.78 (1.37–5.64) | 2.50 (1.17–5.35) |
| p trend | 0.935 | 0.784 | 0.001 | 0.008 |
| Percentage of hours on night shifts | ||||
| Day work | 1.00 | 1.00 | 1.00 | 1.00 |
| <20% | 0.81 (0.26–2.56) | 0.81 (0.24–2.71) | 1.26 (0.49–3.25) | 1.23 (0.46–3.31) |
| 20–30% | 0.89 (0.28–2.82) | 0.99 (0.29–3.38) | 1.21 (0.46–3.23) | 1.25 (0.45–3.47) |
| >30% | 1.18 (0.53–2.62) | 1.17 (0.47–2.92) | 2.79 (1.40–5.59) | 2.55 (1.21–5.39) |
| p trend | 0.550 | 0.596 | 0.001 | 0.005 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, S.; Wang, H.; Wang, Y.; Yu, M.; Yuan, J. Association of Rotating Night Shift Work with Body Fat Percentage and Fat Mass Index among Female Steelworkers in North China. Int. J. Environ. Res. Public Health 2021, 18, 6355. https://doi.org/10.3390/ijerph18126355
Zhang S, Wang H, Wang Y, Yu M, Yuan J. Association of Rotating Night Shift Work with Body Fat Percentage and Fat Mass Index among Female Steelworkers in North China. International Journal of Environmental Research and Public Health. 2021; 18(12):6355. https://doi.org/10.3390/ijerph18126355
Chicago/Turabian StyleZhang, Shengkui, Han Wang, Yongbin Wang, Miao Yu, and Juxiang Yuan. 2021. "Association of Rotating Night Shift Work with Body Fat Percentage and Fat Mass Index among Female Steelworkers in North China" International Journal of Environmental Research and Public Health 18, no. 12: 6355. https://doi.org/10.3390/ijerph18126355
APA StyleZhang, S., Wang, H., Wang, Y., Yu, M., & Yuan, J. (2021). Association of Rotating Night Shift Work with Body Fat Percentage and Fat Mass Index among Female Steelworkers in North China. International Journal of Environmental Research and Public Health, 18(12), 6355. https://doi.org/10.3390/ijerph18126355






