Association between Residence Location and Pre-Hospital Delay in Patients with Heart Failure
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Sample
2.2. Procedure
2.3. Measurement
2.4. Data Analysis
3. Results
3.1. Sample Characteristics
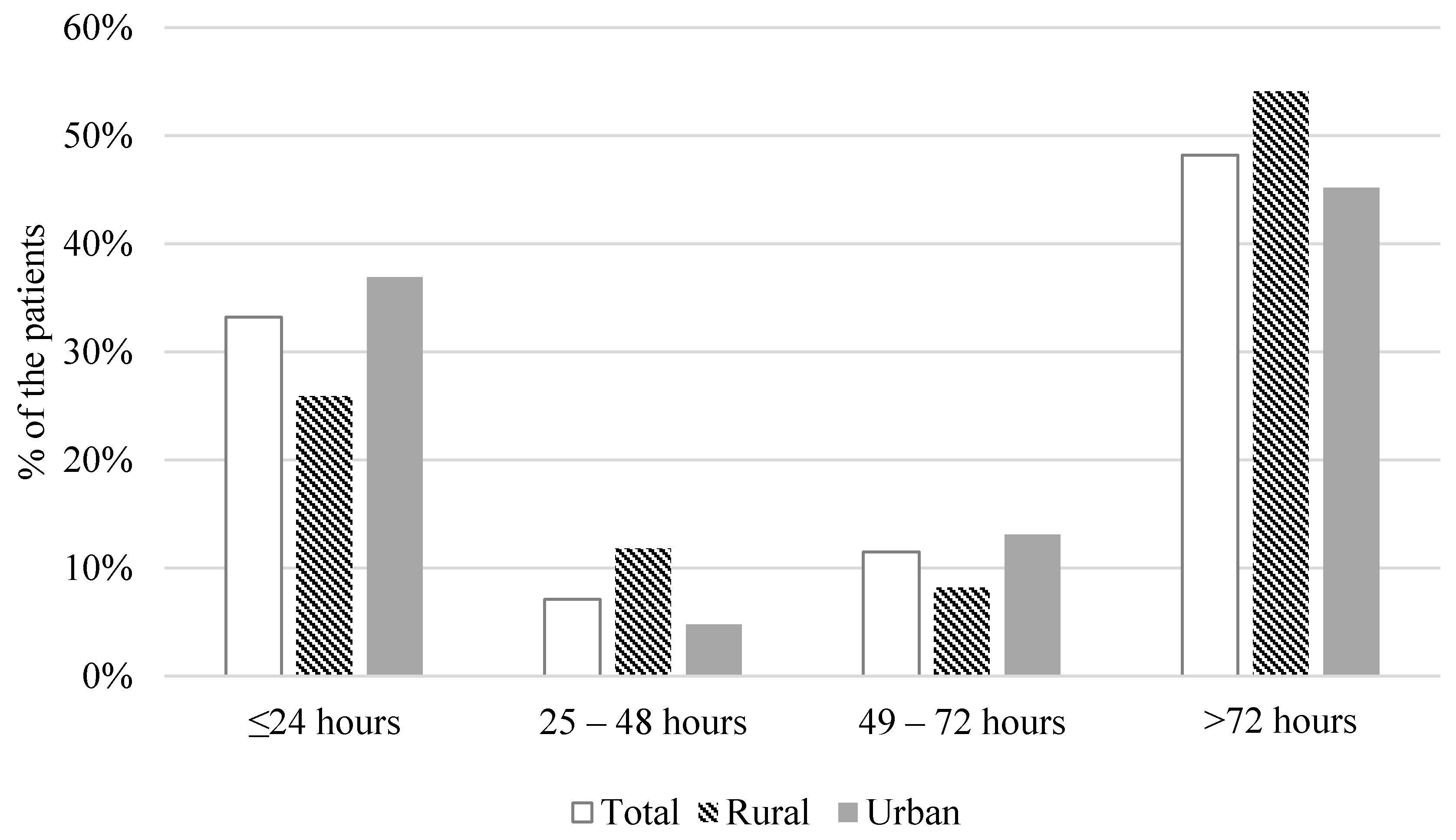
3.2. Duration of Pre-Hospital Delay
3.3. Symptom Experience before Seeking Medical Care
3.4. Interpretation and Response to Worsening of Symptoms by Patients
3.5. Factors Associated with a Pre-Hospital Delay
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Allen, L.A.; Gheorghiade, M.; Reid, K.J.; Dunlay, S.M.; Chan, P.S.; Hauptman, P.J.; Zannad, F.; Konstam, M.A.; Spertus, J.A. Identifying patients hospitalized with heart failure at risk for unfavorable future quality of life. Circ. Cardiovasc. Qual. Outcomes 2011, 4, 389–398. [Google Scholar] [CrossRef]
- Lesyuk, W.; Kriza, C.; Kolominsky-Rabas, P. Cost-of-illness studies in heart failure: A systematic review 2004–2016. BMC Cardiovasc. Disord. 2018, 18, 74. [Google Scholar] [CrossRef] [PubMed]
- Pham, P.N.; Xiao, H.; Sarayani, A.; Chen, M.; Brown, J.D. Risk Factors Associated With 7- Versus 30-Day Readmission Among Patients with Heart Failure Using the Nationwide Readmission Database. Med. Care 2019, 57, 1–7. [Google Scholar] [CrossRef]
- Darling, C.; Saczynski, J.S.; McManus, D.D.; Lessard, D.; Spencer, F.A.; Goldberg, R.J. Delayed hospital presentation in acute decompensated heart failure: Clinical and patient reported factors. Heart Lung 2013, 42, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, R.; Sullivan, A.; Hales, S.; Gillies, G.; Burke, R.; Tofler, G. Symptom patterns, duration and responses in newly diagnosed patients with heart failure. Int. J. Nurs. Pract. 2012, 18, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Okada, A.; Tsuchihashi-Makaya, M.; Kang, J.; Aoki, Y.; Fukawa, M.; Matsuoka, S. Symptom Perception, Evaluation, Response to Symptom, and Delayed Care Seeking in Patients with Acute Heart Failure: An Observational Study. J. Cardiovasc. Nurs. 2019, 34, 36–43. [Google Scholar] [CrossRef]
- Sethares, K.A.; Sosa, M.E.; Fisher, P.; Riegel, B. Factors Associated with Delay in Seeking Care for Acute Decompensated Heart Failure. J. Cardiovasc. Nurs. 2014, 29, 429–438. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.R.; Lee, K.S.; Dekker, R.D.; Welsh, J.D.; Song, E.K.; Abshire, D.A.; Lennie, T.A.; Moser, D.K. Prehospital Delay, Precipitants of Admission, and Length of Stay in Patients with Exacerbation of Heart Failure. Am. J. Crit. Care 2016, 26, 62–69. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Humphreys, J.S.; Solarsh, G. Populations at special health risk: Rural populations. In International Encyclopedia of Public Health; Heggenhougen, H.K.(Kris), Ed.; Academic Press: Oxford, UK, 2008; pp. 242–253. [Google Scholar] [CrossRef]
- Gamble, J.M.; Eurich, D.T.; Ezekowitz, J.A.; Kaul, P.; Quan, H.; McAlister, F.A. Patterns of care and outcomes differ for urban versus rural patients with newly diagnosed heart failure, even in a universal healthcare system. Circ. Heart Fail. 2011, 4, 317–323. [Google Scholar] [CrossRef]
- Munoz, M.A.; Garcia, R.; Navas, E.; Duran, J.; Del Val-Garcia, J.L.; Verdu-Rotellar, J.M. Relationship between the place of living and mortality in patients with advanced heart failure. BMC Fam. Pract. 2020, 21, 145. [Google Scholar] [CrossRef]
- Teng, T.H.; Katzenellenbogen, J.M.; Hung, J.; Knuiman, M.; Sanfilippo, F.M.; Geelhoed, E.; Hobbs, M.; Thompson, S.C. Rural-urban differentials in 30-day and 1-year mortality following first-ever heart failure hospitalisation in Western Australia: A population-based study using data linkage. BMJ Open 2014, 4, e004724. [Google Scholar] [CrossRef]
- Kim, H. Interlinking open government data in Korea using administrative district knowledge graph. J. Inf. Sci. Theory Pract. 2018, 6, 18–30. [Google Scholar]
- Lee, K.S.; Moser, D.K. Heart failure symptom measures: Critical review. Eur. J. Cardiovasc. Nurs. 2013, 12, 418–428. [Google Scholar] [CrossRef] [PubMed]
- Reeder, K.M.; Ercole, P.M.; Peek, G.M.; Smith, C.E. Symptom Perceptions and Self-care Behaviors in Patients Who Self-manage Heart Failure. J. Cardiovasc. Nurs. 2015, 30, E1–E7. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Lee, K.S.; Oh, S. An Integrative Review of the Symptom Perception Process in Heart Failure. J. Cardiovasc. Nurs. 2020. [Google Scholar] [CrossRef]
- Friedman, M.M.; Quinn, J.R. Heart Failure Patients’ Time, Symptoms, and Actions Before a Hospital Admission. J. Cardiovasc. Nurs. 2008, 23, 506–512. [Google Scholar] [CrossRef]
- Clark, A.M.; Freydberg, C.N.; McAlister, F.A.; Tsuyuki, R.T.; Armstrong, P.W.; Strain, L.A. Patient and informal caregivers’ knowledge of heart failure: Necessary but insufficient for effective self-care. Eur. J. Heart Fail. 2009, 11, 617–621. [Google Scholar] [CrossRef] [PubMed]
- Chan, L.; Hart, L.G.; Goodman, D.C. Geographic access to health care for rural Medicare beneficiaries. J. Rural Health 2006, 22, 140–146. [Google Scholar] [CrossRef]
- Verdejo, H.E.; Ferreccio, C.; Castro, P.F. Heart Failure in Rural Communities. Heart Fail. Clin. 2015, 11, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Yi, Y.J.; Kim, E.J. The effects of accessibility to medical facilities and public transportation on perceived health of urban and rural elderly: Using generalized ordered logic model. J. Korean Reg. Dev. Assoc. 2015, 27, 65–88. [Google Scholar]
| Characteristic | Total | Rural Residents (n = 85) | Urban Residents (n = 168) | p-Value | |
|---|---|---|---|---|---|
| Mean (SD) or Frequency (%) | |||||
| Age (years) | 71.5 (12.7) | 74 (11.1) | 70 (13.3) | 0.018 | |
| Gender | Male | 117 (46.2%) | 39 (45.9%) | 78 (46.4%) | 0.934 |
| Female | 136 (53.8%) | 46 (54.1%) | 90 (53.6%) | ||
| Body mass index (kg/m2) | 23.9 (4.1) | 23.1 (4.0) | 24.4 (4.1) | 0.021 | |
| Education level | ≥High school graduate | 72 (28.5%) | 16 (18.8%) | 56 (33.3%) | 0.016 |
| Marital status | Single/widowed/divorced | 50 (19.8%) | 20 (23.5%) | 30 (17.9%) | 0.285 |
| Married | 203 (80.2%) | 65 (76.5%) | 138 (82.1%) | ||
| Charlson comorbidity index | 2.8 (1.7) | 2.6 (1.5) | 3.0 (1.8) | 0.086 | |
| Left ventricular ejection fraction | <40 | 129 (51.0%) | 46 (54.1%) | 83 (49.4%) | 0.479 |
| ≥40 | 124 (49.0%) | 39 (45.9%) | 8 (50.6%) | ||
| Etiology of heart failure | Ischemic | 90 (35.6%) | |||
| Non-ischemic | 163 (64.4%) | ||||
| Years since HF diagnosis | 2.8 (3.4) | 3.3 (3.9) | 2.5 (3.1) | 0.072 | |
| NT-pro BNP (n = 214) | 7266.5 (8625.7) | 6361.3 (7435.2) | 7744.9 (9182.1) | 0.265 | |
| NYHA functional class on admission | II | 55 (21.7%) | 12 (14.1%) | 43 (25.6%) | 0.037 |
| III/IV | 198 (78.3%) | 73 (85.9%) | 125 (74.4%) | ||
| Prior admission due to HF exacerbation within 3 months | 36 (14.2%) | 11 (12.9%) | 25 (14.9%) | 0.677 | |
| Number of medications | 6.9 (3.1) | 6.6 (2.7) | 7.2 (3.3) | 0.117 | |
| ACEi/ARB | 184 (72.7%) | 62 (74.7%) | 122 (74.4%) | 0.958 | |
| Beta blockers | 211 (83.4%) | 70 (84.3%) | 141 (86.0%) | 0.730 | |
| Diuretics | 225 (88.9%) | 75 (90.4%) | 150 (91.5%) | 0.774 | |
| Admission route | Emergency room | 174 (68.8%) | 58 (68.2%) | 116 (69.0%) | 0.895 |
| Clinic | 79 (31.2%) | 27 (31.8%) | 52 (31.0%) | 0.895 | |
| Admission vital sign | Systolic blood pressure | 138.6 (31.7) | 132.8 (29.5) | 141.6 (32.5) | 0.038 |
| Diastolic blood pressure | 81.0 (17.4) | 80.1 (16.8) | 81.4 (17.8) | 0.585 | |
| Heart rate | 97.1 (24.2) | 91.8 (21.7) | 99.7 (25.0) | 0.014 | |
| Respiration | 24.6 (6.0) | 24.6 (5.9) | 24.7 (6.0) | 0.877 | |
| Saturation | 95.0 (5.4) | 95.1 (6.2) | 95.0 (5.0) | 0.879 | |
| Time interval from onset to the admission (hours) 1 | 379.8 (1125.6) | 410.2 (930.7) | 364.5 (1214.7) | 0.114 | |
| Median: 72 (IQR: 17.25–240.00) | Median: 96 (IQR 24.0–324.0) | Median: 72 (IQR 11.25–240.0) | |||
| Total | Rural Residents | Urban Residents | p-Value | |
|---|---|---|---|---|
| Mean (SD) or Frequency (%) | ||||
| Symptom experience | ||||
| Total number of symptoms experienced before the admission | 2.6 (1.6) | 2.6 (1.6) | 2.7 (1.7) | 0.807 |
| Shortness of breath | 218 (86.2%) | 74 (87.1%) | 144 (85.7%) | 0.770 |
| Shortness of breath with activity | 68 (26.9%) | 27 (31.8%) | 41 (24.4%) | 0.212 |
| Lower extremity swelling | 45 (17.8%) | 8 (9.4%) | 37 (22.0%) | 0.013 |
| Coughing | 42 (16.6%) | 9 (10.6%) | 33 (19.6%) | 0.068 |
| Chest pain | 40 (15.8%) | 13 (15.3%) | 27 (16.1%) | 0.873 |
| Shortness of breath when lying flat | 37 (14.6%) | 10 (11.8%) | 27 (16.1%) | 0.360 |
| Poor appetite | 19 (7.5%) | 8 (9.4%) | 11 (6.5%) | 0.414 |
| Difficulty in sleeping | 16 (6.3%) | 6 (7.1%) | 10 (6.0%) | 0.733 |
| Palpitations | 14 (5.5%) | 5 (5.9%) | 9 (5.4%) | 0.863 |
| Weight gain | 13 (5.1%) | 2 (2.4%) | 11 (6.5%) | 0.229 |
| Dizziness | 11 (4.3%) | 6 (7.1%) | 5 (3.0%) | 0.133 |
| Abdominal bloating | 3 (1.2%) | 0 (0.0%) | 3 (1.8%) | 0.553 |
| Fatigue | 3 (1.2%) | 2 (2.4%) | 1 (0.6%) | 0.262 |
| Nausea and vomiting | 3 (1.2%) | 0 (0.0%) | 3 (1.2%) | 0.049 |
| Worrying | 1 (0.4%) | 1 (1.2%) | 0 (0.0%) | 0.336 |
| Feeling sad or depressed | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | N/A |
| Difficulty in concentrating or forgetfulness | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | N/A |
| Precipitating factors of symptoms identified by patients | N/A | |||
| Unable to identify | 171 (67.6%) | 60 (70.6%) | 111 (66.1%) | |
| Exacerbation of comorbid conditions | 67 (26.5%) | 18 (21.2%) | 49 (29.2%) | |
| Non-adherence to medication | 12 (4.7%) | 5 (5.9%) | 7 (4.2%) | |
| Psychological stress | 2 (0.8%) | 1 (1.2%) | 1 (0.6%) | |
| Loss of clinic appointment | 1 (0.4%) | 1 (1.2%) | 0 (0%) | |
| Actions taken to decrease symptoms before the hospitalization 1 | N/A | |||
| Doing nothing | 128 (50.6%) | 42 (49.4%) | 86 (51.2%) | |
| Went to clinic other than cardiology clinic | 62 (24.5%) | 25 (29.4%) | 37 (22.0%) | |
| Call to family | 69 (27.3%) | 23 (27.1%) | 46 (27.4%) | |
| Call to the doctor | 24 (9.5%) | 9 (10.6%) | 15 (8.9%) | |
| Took unrelated medication or actions irrelevant to HF | 5 (2.0%) | 1 (1.2%) | 4 (2.4%) | |
| Took an extra diuretic | 1 (0.4%) | 0 | 1 (0.6%) | |
| Variables | Unstandardized Coefficients | Standardized Coefficients | p-Value | 95% Confidence Interval |
|---|---|---|---|---|
| Urban residence (vs. rural residence) | −0.563 | −0.126 | 0.034 | −1.082, −0.043 |
| Age (years) | −0.003 | −0.016 | 0.806 | −0.025, 0.019 |
| Female (vs. male) | 0.120 | 0.028 | 0.635 | −0.377, 0.616 |
| Body mass index (kg/m2) | 0.061 | 0.118 | 0.061 | −0.003, 0.124 |
| ≥High school graduation (vs. <high school education) | 0.283 | 0.061 | 0.343 | −0.304, 0.87 |
| Married (vs. single/divorced/widowed) | −0.576 | −0.109 | 0.059 | −1.176, 0.023 |
| Preserved ejection fraction (vs. reduced rejection fraction) | −0.292 | −0.069 | 0.227 | −0.766, 0.183 |
| NYHA functional class III/IV (vs. II) | 0.289 | 0.057 | 0.348 | −0.317, 0.895 |
| Charlson comorbidity index | −0.088 | −0.072 | 0.232 | −0.232, 0.056 |
| Admission via clinic (vs. emergency department) | 1.286 | 0.283 | 0.000 | 0.755, 1.816 |
| Prior admission experience due to HF exacerbation | −0.326 | −0.054 | 0.346 | −1.007, 0.354 |
| Did nothing to relieve symptoms before seeking care (vs. did something) | 0.771 | 0.183 | 0.002 | 0.294, 1.248 |
| Shortness of breath | 0.388 | 0.064 | 0.283 | −0.322, 1.099 |
| Shortness of breath with activity | 0.387 | 0.082 | 0.178 | −0.178. 0.952 |
| Lower extremity swelling | 0.722 | 0.131 | 0.027 | 0.084, 1.359 |
| Coughing | 0.891 | 0.157 | 0.007 | 0.24, 1.541 |
| Chest pain | −0.778 | −0.135 | 0.023 | −1.450, −0.107 |
| Shortness of breath when lying flat | 0.093 | 0.352 | 0.791 | −0.600, 0.787 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, K.S.; Lee, H.; Park, J.-H. Association between Residence Location and Pre-Hospital Delay in Patients with Heart Failure. Int. J. Environ. Res. Public Health 2021, 18, 6679. https://doi.org/10.3390/ijerph18126679
Lee KS, Lee H, Park J-H. Association between Residence Location and Pre-Hospital Delay in Patients with Heart Failure. International Journal of Environmental Research and Public Health. 2021; 18(12):6679. https://doi.org/10.3390/ijerph18126679
Chicago/Turabian StyleLee, Kyoung Suk, Hyeongsuk Lee, and Jae-Hyeong Park. 2021. "Association between Residence Location and Pre-Hospital Delay in Patients with Heart Failure" International Journal of Environmental Research and Public Health 18, no. 12: 6679. https://doi.org/10.3390/ijerph18126679
APA StyleLee, K. S., Lee, H., & Park, J.-H. (2021). Association between Residence Location and Pre-Hospital Delay in Patients with Heart Failure. International Journal of Environmental Research and Public Health, 18(12), 6679. https://doi.org/10.3390/ijerph18126679






