Demographics, Socioeconomic Status, Social Distancing, Psychosocial Factors and Psychological Well-Being among Undergraduate Students during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Participants
2.3. Sample Size
2.4. Data Collection
2.5. Measures
2.5.1. Psychological Well-Being
2.5.2. Psychosocial Factors
2.5.3. Demographics and Socioeconomic Status
2.5.4. Social Distancing Factors
2.6. Data Analysis
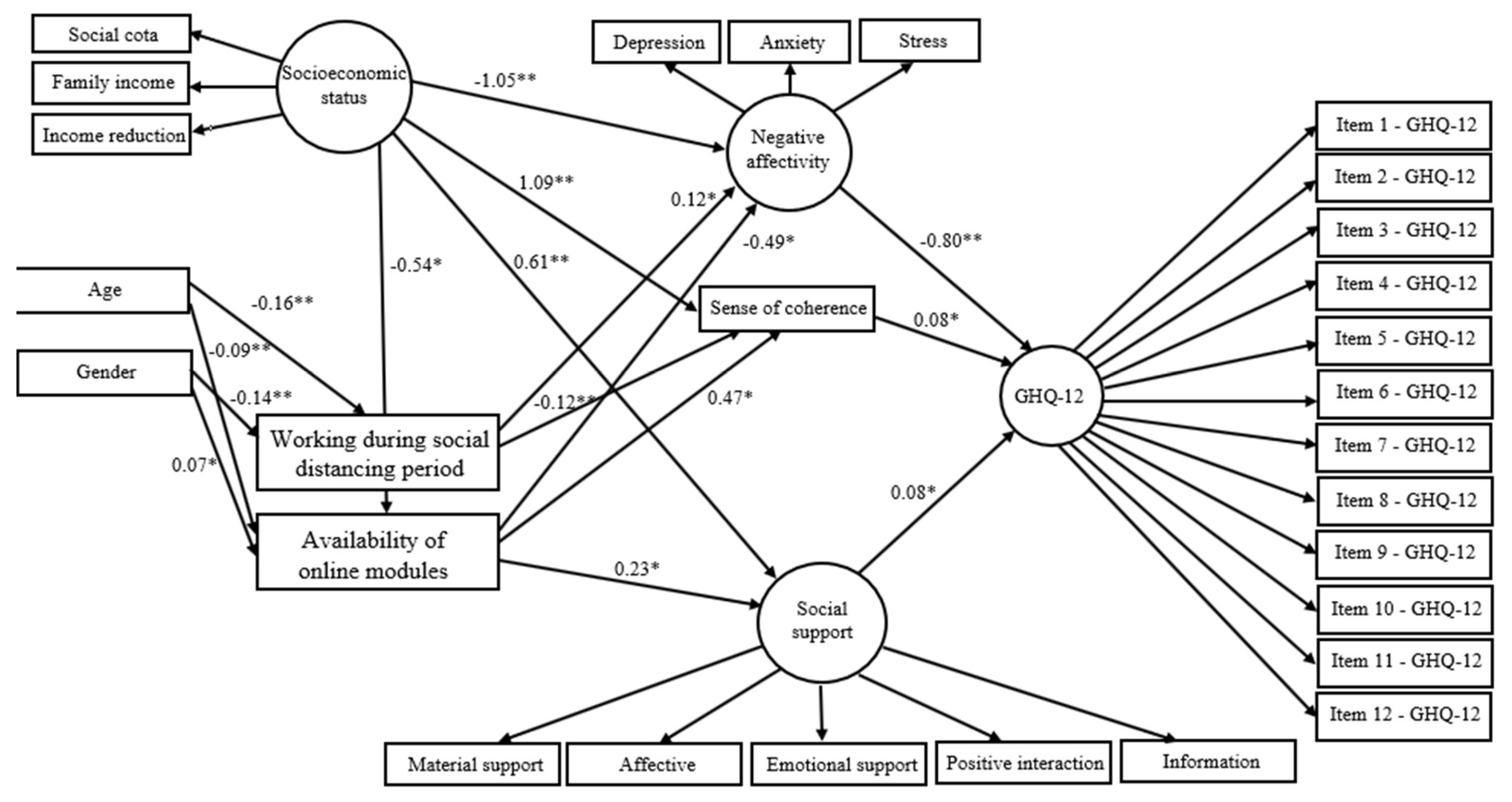
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bao, Y.; Sun, Y.; Meng, S.; Shi, J.; Lu, L. 2019-nCoV epidemic: Address mental health care to empower society. Lancet 2020, 395, e37–e38. [Google Scholar] [CrossRef] [Green Version]
- WHO (World Health Organization). R&D Blueprint and COVID-19. Available online: https://www.who.int/teams/blueprint/covid-19 (accessed on 10 March 2021).
- Sahu, P. Closure of universities due to coronavírus disease 2019 (covid-19): Impact on Education and mental health of students and academic staff. Cureus 2020, 12, e7541. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- UNESCO. COVID-19 Educational Disruption and Response. Available online: https://en.unesco.org/themes/education-emergencies/coronavirus-school-closures (accessed on 25 March 2020).
- MEC (Ministry of Education). Coronavírus. Monitoramento das Instituições de Ensino. Available online: http://por-tal.mec.gov.br/coronavirus/ (accessed on 15 March 2020).
- Frajerman, A.; Morvan, Y.; Krebs, M.O.; Gorwood, P.; Chaumette, B. Burnout in medical students before residency: A systematic review and meta-analysis. Eur. Psychiatry 2019, 55, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Tung, Y.J.; Lo, K.K.H.; Ho, R.C.M.; Tam, W.S.W. Prevalence of depression among nursing students: A systematic review and meta-analysis. Nurse Educ. Today 2018, 63, 119–129. [Google Scholar] [CrossRef] [PubMed]
- Demenech, L.M.; Oliveira, A.T.; Neiva-Silva, L.; Dumith, S.C. Prevalence of anxiety, depression and suicidal behaviors among Brazilian undergraduate students: A systematic review and meta-analysis. J. Affect. Disord. 2021, 282, 147–159. [Google Scholar] [CrossRef]
- Bíró, E.; Balajti, I.; Adany, R.; Kosa, K. Mental health and behaviour of students of public health and their correlation with social support: A cross-sectional study. BMC Public Health 2011, 11, 871. [Google Scholar] [CrossRef] [Green Version]
- Bashir, M.B.A.; Mohamed, S.O.A.; Nkfusai, C.N.; Bede, F.; Oladimeji, O.; Tsoka-Gwegweni, J.M.; Cumber, S.N. Assessment of minor psychiatric morbidity, stressors, and barriers of seeking help among medical students at the University of Khartoum, Khartoum, Sudan. Pan Afr. Med. J. 2020, 35, 87. [Google Scholar] [CrossRef]
- Deasy, C.; Coughlan, B.; Pironom, J.; Jourdan, D.; Mannix-McNamara, P. Psychological Distress and Coping amongst Higher Education Students: A Mixed Method Enquiry. PLoS ONE 2014, 9, e115193. [Google Scholar] [CrossRef] [Green Version]
- Warbah, L.; Sathiyaseelan, M.; Vijayakumar, C.; Vasantharaj, B.; Russell, S.; Jacob, K.S. Psychological distress, personality and adjustment among nursing students. Nurse Educ. Today 2007, 27, 597–601. [Google Scholar] [CrossRef]
- Deasy, C.; Coughlan, B.; Pironom, J.; Jourdan, D.; Mannix-McNamara, P. Predictors of health of pre-registration nursing and midwifery students: Findings from a cross-sectional survey. Nurse Educ. Today 2016, 36, 427–433. [Google Scholar] [CrossRef]
- Gorter, R.; Freeman, R.; Hammen, S.; Murtomaa, H.; Blinkhorn, A.; Humphris, G. Psychological stress and health in undergradate dental students: Fifth year outcomes compared with first year baseline results from five European dental schools. Eur. J. Den. Educ. 2008, 12, 61–68. [Google Scholar] [CrossRef]
- Bastos, J.L.; Barros, A.J.D.; Celeste, R.K.; Paradies, Y.; Faerstein, E. Age, class and race discrimination: Their interactions and associations with mental health among Brazilian university students. Cad. Saude Publica 2014, 30, 175–186. [Google Scholar] [CrossRef] [Green Version]
- Gibbons, C. Stress, coping and burn-out in nursing students. Int. J. Nurs. Stud. 2011, 47, 1299–1309. [Google Scholar] [CrossRef] [PubMed]
- Clay, J.M.; Parker, M.O. Alcohol use and misuse during the COVID-19 pandemic: A potential public health crisis? Lancet Public Health 2020, 5, e259. [Google Scholar] [CrossRef]
- Shigemura, J.; Ursano, R.J.; Morganstein, J.C.; Kurosawa, M.; Benedek, D.M. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin. Neurosci. 2020, 74, 281–282. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Zhong, B.L.; Chiu, H.F. Prevalence of depressive symptoms among Chinese university students amid the COVID-19 pandemic: A systematic review and meta-analysis. Epidemiol. Psychiatr. Sci. 2021, 30, e31. [Google Scholar] [CrossRef]
- Kecojevic, A.; Basch, C.H.; Sullivan, M.; Davi, N.K. The impact of the COVID-19 epidemic on mental health of undergraduate students in New Jersey, cross-sectional study. PLoS ONE 2020, 15, e0239696. [Google Scholar] [CrossRef] [PubMed]
- Deng, J.; Zhou, F.; Hou, W.; Silver, Z.; Wong, C.Y.; Chang, O.; Drakos, A.; Zuo, Q.K.; Huang, E. The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2021, 301, 113863. [Google Scholar] [CrossRef] [PubMed]
- Bradburn, N.M. The Structure of Psychological Well Being; Aldine Publishing Company: Chicago, IL, USA, 1969; p. 318. [Google Scholar]
- Suh, E.; Diener, E.; Fujita, F. Events and subjective well-being: Only recent matter. J. Personal. Soc. Psychol. 1996, 70, 1091–1102. [Google Scholar] [CrossRef]
- Lazarus, R.S. Stress and Emotion: A New Synthesis; Springer Publishing Company: New York, NY, USA, 2006; p. 340. [Google Scholar]
- Ryff, C.D. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J. Personal. Soc. Psychol. 1989, 57, 1069–1081. [Google Scholar] [CrossRef]
- Liu, T.; Wang, Z.; Zhou, C.; Li, T. Affect and Self-Esteem as Mediators between Trait Resilience and Psychological Adjustment. Personal. Individ. Differ. 2014, 66, 92–97. [Google Scholar] [CrossRef]
- Liébana-Presa, C.; Fernández-Martínez, E.; Gándara, A.R.; Muñoz-Villanueva, M.C.; Vázquez-Casares, A.M.; Rodríguez-Borrego, M.A. Psychological distress in health sciences college students and its relationship with academic engagement. Rev. Esc. Enferm. USP 2014, 48, 715–722. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Antonovsky, A. Unraveling Mystery of Health. How People Manage Stress and Stay Well, 1st ed.; Jossey-Bass Inc. Pub: San Francisco, CA, USA, 1987; pp. 15–32. [Google Scholar]
- Antonovsky, A. Health, Stress and Coping, 1st ed.; Jossey-Bass Inc. Pub: San Francisco, CA, USA, 1979; pp. 70–97. [Google Scholar]
- Cobb, S. Social support as a moderator of life stress. Psychosom. Med. 1976, 38, 300–314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caplan, G. The family as social support. In Support Systems and Mutual Help: Multidisciplinary Explorations; Caplan, G., Killilea, M., Eds.; Grune & Stratton: New York, NY, USA, 1976; pp. 19–36. [Google Scholar]
- UFF (Fluminense Federal University). UFF em Números. Available online: http://www.uff.br/?q=uff-em-numeros-0 (accessed on 5 January 2021).
- Westland, J.C. Lower bounds on sample size in structural equation modeling. Electron. Commer. Res. Appl. 2010, 9, 476–487. [Google Scholar] [CrossRef]
- Goldberg, D.P. The Detection of Psychiatric Illness by Questionnaire; Oxford University Press: London, UK, 1972. [Google Scholar]
- Mari, J.J.; Williams, P. A comparison of the validity of two psychiatric screening questionnaires (GHQ-12 and SRQ-20) in Brazil, using relative operating characteristic (ROC) analysis. Psychol. Med. 1985, 15, 651–659. [Google Scholar] [CrossRef]
- Lovibond, S.H.; Lovibond, P.F. Manual for the Depression Anxiety Stress Scales, 2nd ed.; Psychology Foundation: Sydney, Australia, 1995. [Google Scholar]
- Vignola, R.C.B.; Tucci, A.M. Adaptation and validation of the Depression, Anxiety and Stress Scale (DASS) to Brazilian portuguese. J. Affect. Disord. 2014, 155, 104–109. [Google Scholar] [CrossRef]
- Bonanato, K.; Barbabela, D.; Mota, J.P.T.; Ramos-Jorge, M.L.; Kaeppler, K.C.; Paiva, S.M.; Pordeus, I.A.; Kaeppler, K.C. Trans-cultural adaptation and psychometric properties of the ‘Sense of Coherence Scale’ in mothers of preschool children. Interam. J. Psychol. 2007, 41, 22–29. [Google Scholar]
- Sherbourne, C.D.; Stewart, A.L. The MOS social support survey. Soc. Sci. Med. 1991, 32, 705–714. [Google Scholar] [CrossRef]
- Chor, D.; Griep, R.H.; Lopes, C.S.; Faerstein, E. Social network and social support measures from the Pró-Saúde Study: Pre-tests and pilot study. Cad. Saúde Pública 2001, 17, 887–896. [Google Scholar] [CrossRef] [Green Version]
- Drissi, N.; Alhmoudi, A.; Nuaimi, H.A.; Alkhyeli, M.; Alsalami, S.; Ouhbi, S. Investigating the Impact of COVID-19 Lockdown on the Psychological Health of University Students and Their Attitudes Toward Mobile Mental Health Solutions: Two-Part Questionnaire Study. JMIR Form. Res. 2020, 4, e19876. [Google Scholar] [CrossRef] [PubMed]
- MacKinnon, D.P.; Lockwood, C.M.; Hoffman, J.M.; West, S.G.; Sheets, V.A. Comparison of methods to test mediation and other intervening variable effects. Psychol. Methods 2002, 7, 83–104. [Google Scholar] [CrossRef]
- Hu, L.-T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Modeling Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Teixeira, L.A.C.; Costa, R.A.; Mattos, R.M.P.R.; Pimentel, D. Brazilian medical students’ mental health during coronavirus disease 2019 pandemic. J. Bras. Psiquiatr. 2021, 70, 21–29. [Google Scholar] [CrossRef]
- Tamarit, A.; de la Barrera, U.; Mónaco, E.; Schoeps, K.; Montoya-Castilla, I. Psychological impact of COVID-19 pandemic in Spanish adolescents: Risk and protective factors of emotional symptom. Rev. Psicol. Clín. Niños Adolesc. 2020, 7, 73–80. [Google Scholar] [CrossRef]
- Carlén, K.; Suominen, S.; Lindmark, U.; Saarinen, M.M.; Aromaa, M.; Rautava, P.; Sillanpää, M. Sense of coherence predicts adolescent mental health. J. Affect. Disord. 2020, 274, 1206–1210. [Google Scholar] [CrossRef]
- Nilsson, K.W.; Leppert, J.; Simonsson, B.; Starrin, B. Sense of coherence and psychological well-being: Improvement with age. J. Epidemiol. Community Health 2010, 64, 347–352. [Google Scholar] [CrossRef]
- Ma, Z.; Zhao, J.; Li, Y.; Chen, D.; Wang, T.; Zhang, Z.; Chen, Z.; Yu, Q.; Jiang, J.; Fan, F.; et al. Mental health problems and correlates among 746,217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol. Psychiatr. Sci. 2020, 29, e181. [Google Scholar] [CrossRef] [PubMed]
- Rafael, R.M.R.; Correia, L.M.; Mello, A.S.; Prata, J.A.; Depret, D.G.; Santo, T.B.E.; Silva, F.V.C.; Acioli, A. Psychological distress in the COVID-19 pandemic: Prevalence and associated factors at a nursing college. Rev. Bras. Enferm. 2021, 74 (Suppl. S1), e20210023. [Google Scholar] [CrossRef]
- Sun, S.; Goldberg, S.B.; Lin, D.; Qiao, S.; Operario, D. Psychiatric symptoms, risk, and protective factors among university students in quarantine during the COVID-19 pandemic in China. Glob. Health 2021, 17, 15. [Google Scholar] [CrossRef] [PubMed]
- Elmer, T.; Mepham, K.; Stadtfeld, C. Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE 2020, 15, e0236337. [Google Scholar] [CrossRef] [PubMed]
- Thoits, P.A. Stress, coping and social support processes: Where are we? What next? J. Health Soc. Behav. 1995, 53–79. [Google Scholar] [CrossRef] [Green Version]
- Kawachi, I.; Berkman, L.F. Social ties and mental health. J. Urban Health 2001, 78, 458–467. [Google Scholar] [CrossRef] [Green Version]
- Atri, A.; Sharma, M.; Cottrell, R. Role of social support, hardiness, and acculturation as predictors of mental health among international students of Asian Indian origin. Int. Q. Community Health Educ. 2007, 27, 59–73. [Google Scholar] [CrossRef]
- Kinderman, P. A psychological model of mental disorder. Harv. Rev. Psychiatry 2005, 13, 206–217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Braun-Lewensohn, O.; Sagy, S.; Roth, G. Coping strategies as mediators of the relationship between sense of coherence and stress reactions: Israeli adolescents under missile attacks. Anxiety Stress Coping 2011, 24, 327–341. [Google Scholar] [CrossRef]
- Geckova, A.M.; Tavel, P.; van Dijk, J.; Abel, T.; Reijneveld, S. Factors associated with educational aspirations among adolescents: Cues to counteract socioeconomic differences? BMC Public Health 2010, 10, 154. [Google Scholar] [CrossRef] [Green Version]
- Hefner, J.; Eisenberg, D. Social support and mental health among college students. Am. J. Orthopsychiatry 2009, 79, 491–499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lo, R. A longitudinal study of perceived level of stress, coping and self-esteem of undergraduate nursing students: An Australian case study. J. Adv. Nurs. 2002, 39, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Sagy, S.; Antonovsky, A. Adolescents’ reaction to the evacuation of the Sinai settlements: A longitudinal study. J. Psychol. 1986, 120, 543–556. [Google Scholar] [CrossRef]
- Díaz-Jiménez, R.M.; Caravaca-Sánchez, F.; Martín-Cano, M.C.; De la Fuente-Robles, Y.M. Anxiety levels among social work students during the COVID-19 lockdown in Spain. Soc. Work Health Care 2020, 59, 681–693. [Google Scholar] [CrossRef]
- González-Carrasco, M.; Casas, F.; Malo, S.; Viñas, F.; Dinisman, T. Changes with age in subjective well-being through the adolescent years: Differences by gender. J. Happiness Stud. 2017, 18, 63–88. [Google Scholar] [CrossRef]
- Costa, E.F.O.; Rocha, M.M.V.; Santos, A.T.R.A.; Melo, E.V.; Martins, L.A.N.; Andrade, T.M. Common mental disorders and associated factors among final-year healthcare students. Rev. Assoc. Med. Bras. 2014, 60, 525–530. [Google Scholar] [CrossRef] [Green Version]
- Silva, A.G.; Ramos-Cerqueira, A.T.A.; Lima, M.C.P. Social support and common mental disorder among medical students. Rev. Bras. Epidemiol. 2014, 17, 229–242. [Google Scholar] [CrossRef] [PubMed]
- Prado, A.S.; Freitas, J.L. Social distancing during pandemics: Suicide risk and prevention in the face of psychosocial impacts of COVID-19. Estud. Psicol. 2020, 25, 157–166. [Google Scholar] [CrossRef]
- Arvidsdotter, T.; Marklund, B.; Taft, C.; Kylén, S. Quality of life, sense of coherence and experiences with three different treatments in patients with psychological distress in primary care: A mixed-methods study. BMC Complement. Altern. Med. 2015, 15, 132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kähönen, K.; Näätänen, P.; Tolvanen, A.; Salmela-Aro, K. Development of sense of coherence during two group interventions. Scand. J. Psychol. 2012, 53, 523–527. [Google Scholar] [CrossRef]
- Lattie, E.G.; Adkins, E.C.; Winquist, N.; Stiles-Shields, C.; Wafford, Q.E.; Graham, A.K. Digital Mental Health Interventions for Depression, Anxiety and Enhancement of Psychological Well-Being Among College Students: Systematic Review. J. Med. Internet Res. 2019, 21, e12869. [Google Scholar] [CrossRef]


| Variables | Total (n = 620) | Psychological Well-Being | ||
|---|---|---|---|---|
| Severe Case Score Category (n = 279/45%) | High-Risk Score Category (n = 287/46.3%) | Normal State Score Category (n = 54/8.7%) | ||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
| Age, mean (SD) | 23.0 (3.7) | 23.2 (4.1) | 22.8 (3.5) | 22.8 (2.2) |
| N (%) | N (%) | N (%) | N (%) | |
| Gender | ||||
| Female | 484 (78) | 229 (82) | 222 (77) | 33 (61) |
| Male | 136 (22) | 50 (18) | 65 (23) | 21 (39) |
| Admission through social quotas | ||||
| Yes | 262 (42) | 124 (44) | 115 (40) | 23 (43) |
| No | 358 (58) | 155 (56) | 172 (60) | 31 (57) |
| Monthly Family income | ||||
| Up to 3 BMWs | 236 (38) | 118 (42) | 101 (35) | 17 (32) |
| 3–6 BMWs | 194 (31) | 98 (35) | 77 (27) | 19 (31) |
| >6 BMWs | 190 (31) | 63 (23) | 109 (38) | 18 (33) |
| Reduction of family income during the social distancing period | ||||
| Yes | 377 (61) | 180 (65) | 168 (59) | 29 (54) |
| No | 243 (39) | 99 (36) | 119 (42) | 25 (46) |
| Working during the social distancing period | ||||
| No | 496 (80) | 231 (83) | 227 (79) | 38 (70) |
| Yes | 124 (20) | 48 (17) | 60 (21) | 16 (30) |
| Availability of online modules | ||||
| No | 279 (45) | 141 (50) | 119 (42) | 19 (35) |
| Yes | 341 (55) | 138 (50) | 168 (59) | 35 (65) |
| City of origin is different from the city of the campus | ||||
| No | 353 (57) | 156 (56) | 167 (58) | 30 (56) |
| Yes | 267 (43) | 123 (45) | 120 (42) | 24 (44) |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
| Negative affectivity | 34.1 (14.9) | 44.6 (10.2) | 27.7 (11.8) | 13.9 (8.9) |
| Depression | 11.5 (5.8) | 15.8 (4.0) | 8.8 (4.4) | 3.9 (3.5) |
| Anxiety | 9.0 (5.8) | 12.3 (5.1) | 7.0 (5.0) | 3.2 (3.5) |
| Stress | 13.5 (5.2) | 16.6 (3.8) | 11.9 (4.7) | 6.8 (4.2) |
| SOC | 37.0 (8.2) | 31.5 (6.4) | 40.4 (6.1) | 47.1 (6.2) |
| Social support | 57.1 (17.1) | 50.5 (17.8) | 61.2 (14.5) | 69.2 (9.4) |
| Material support | 13.3 (3.6) | 12.6 (4.1) | 13.8 (3.0) | 14.5 (3.2) |
| Affective support | 9.7 (3.0) | 8.7 (3.4) | 10.3 (2.5) | 11.3 (1.5) |
| Emotional support | 14.3 (2.8) | 9.2 (4.7) | 12.0 (4.1) | 14.3 (2.8) |
| Positive social interaction | 11.9 (4.6) | 10.3 (4.7) | 12.8 (3.9) | 14.7 (2.6) |
| Information support | 11.3 (4.4) | 9.6 (4.5) | 12.3 (3.9) | 14.6 (2.1) |
| Pathways | β | 95% CI | p |
|---|---|---|---|
| Direct Effects | |||
| Negative affectivity → psychological well-being | −0.80 | −0.92/−0.68 | 0.003 ** |
| SOC → psychological well-being | 0.08 | 0.05/0.20 | 0.016 * |
| Social support → psychological well-being | 0.08 | 0.02/0.14 | 0.014 * |
| SES → Negative affectivity | −1.05 | −2.00/−0.87 | 0.002 ** |
| Working during the social distancing period → Negative affectivity | 0.12 | 0.03/0.19 | 0.013 * |
| Availability of online teaching → Negative affectivity | −0.49 | −1.72/−0.03 | 0.038 * |
| SES → SOC | 1.09 | 0.93/2.08 | 0.001 ** |
| Working during the social distancing period → SOC | −0.12 | −0.19/−0.05 | 0.005 ** |
| Availability of online teaching → SOC | 0.47 | 0.01/1.74 | 0.040 * |
| SES → social support | 0.61 | 0.49/1.02 | 0.002 ** |
| Availability of online teaching → social support | 0.23 | 0.04/0.87 | 0.009 ** |
| Age → working during the social distancing period | −0.16 | −0.26/−0.07 | 0.002 ** |
| Gender → working during the social distancing period | −0.14 | −0.23/−0.05 | 0.002 ** |
| SES → availability of online teaching | −0.54 | −0.90/−0.13 | 0.019 * |
| Age → availability of online teaching | −0.09 | −0.16/−0.03 | 0.004 ** |
| Gender → availability of online teaching | 0.07 | 0.01/0.14 | 0.032 * |
| Indirect effects | |||
| SES → psychological well-being | 0.73 | 4.05/27.29 | 0.001 ** |
| Gender → psychological well-being | 0.05 | 0.01/0.16 | 0.001 ** |
| Working during the social distancing period → psychological well-being | −0.10 | −0.21/−0.04 | 0.01 * |
| Availability of online teaching → psychological well-being | 0.45 | 0.02/1.56 | 0.042 * |
| SES → Negative affectivity | 0.27 | 1.22/4.51 | 0.018 * |
| Gender → Negative affectivity | −0.05 | −2.68/−0.22 | 0.001 ** |
| SES → SOC | −0.25 | −4.61/−0.43 | 0.036 * |
| Gender → SOC | 0.05 | 0.32/2.86 | 0.001 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, A.N.d.; Guedes, C.R.; Santos-Pinto, C.D.B.; Miranda, E.S.; Ferreira, L.M.; Vettore, M.V. Demographics, Socioeconomic Status, Social Distancing, Psychosocial Factors and Psychological Well-Being among Undergraduate Students during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 7215. https://doi.org/10.3390/ijerph18147215
Silva ANd, Guedes CR, Santos-Pinto CDB, Miranda ES, Ferreira LM, Vettore MV. Demographics, Socioeconomic Status, Social Distancing, Psychosocial Factors and Psychological Well-Being among Undergraduate Students during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2021; 18(14):7215. https://doi.org/10.3390/ijerph18147215
Chicago/Turabian StyleSilva, Andréa Neiva da, Carla Ribeiro Guedes, Cláudia Du Bocage Santos-Pinto, Elaine Silva Miranda, Larissa Machado Ferreira, and Mario Vianna Vettore. 2021. "Demographics, Socioeconomic Status, Social Distancing, Psychosocial Factors and Psychological Well-Being among Undergraduate Students during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 18, no. 14: 7215. https://doi.org/10.3390/ijerph18147215
APA StyleSilva, A. N. d., Guedes, C. R., Santos-Pinto, C. D. B., Miranda, E. S., Ferreira, L. M., & Vettore, M. V. (2021). Demographics, Socioeconomic Status, Social Distancing, Psychosocial Factors and Psychological Well-Being among Undergraduate Students during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 18(14), 7215. https://doi.org/10.3390/ijerph18147215






