A Comparison of the Survival, Place of Death, and Medical Utilization of Terminal Patients Receiving Hospital-Based and Community-Based Palliative Home Care: A Retrospective and Propensity Score Matching Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population and Settings
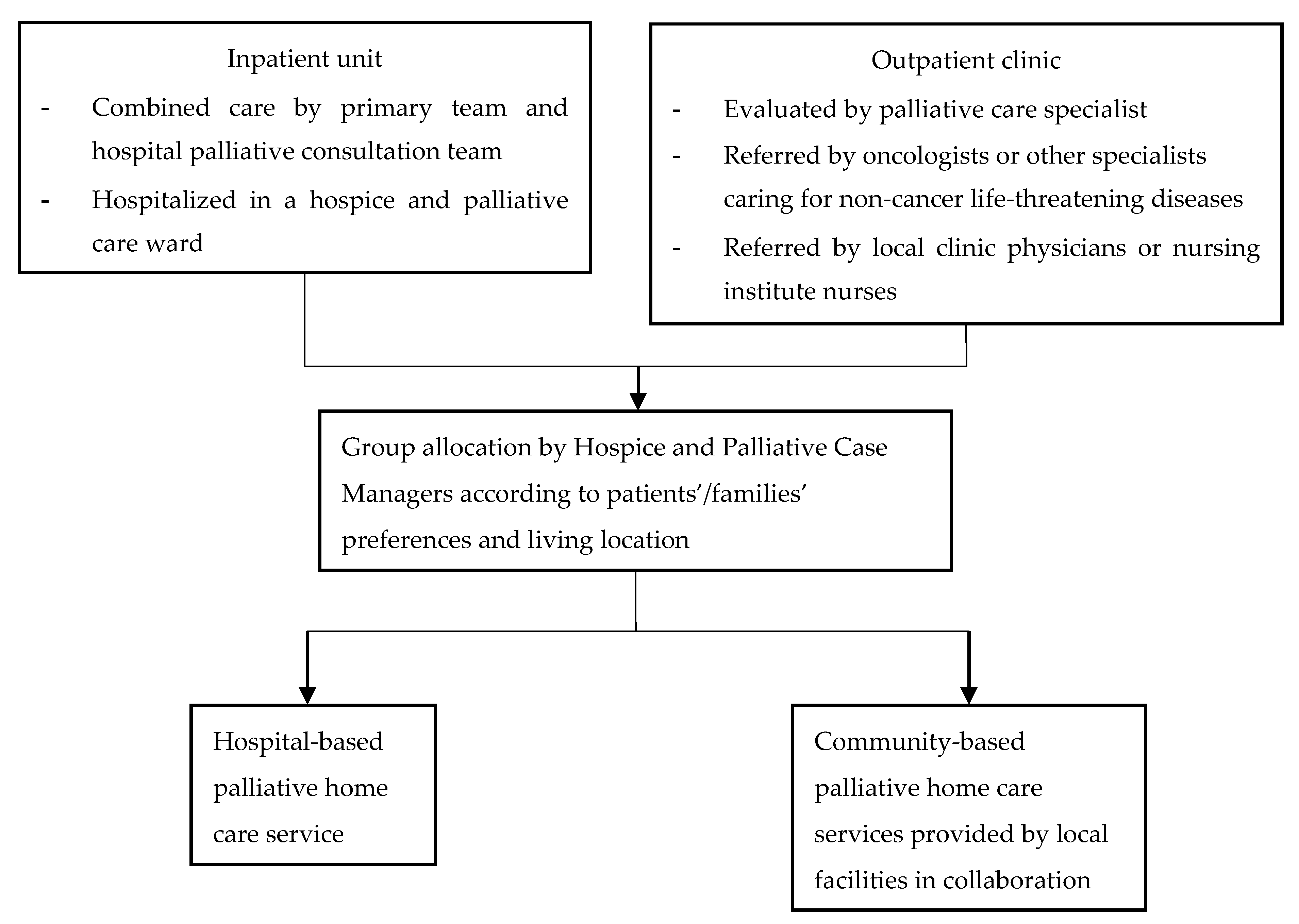
2.3. Group Allocation Process
2.4. Data Sources and Data Collection
2.5. Data Analysis
2.6. Ethical Consideration
3. Results
3.1. Participant Characteristics
3.2. Medical Utilization, Place of Death, and Survival Days
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations World Population Ageing 2019 Highlights; World Health Organization: New York, NY, USA, 2019.
- National Development Council Taiwan Projection on Population in Taiwan 2020–2070. Available online: https://www.ndc.gov.tw/Content_List.aspx?n=695E69E28C6AC7F3 (accessed on 6 May 2021).
- Sleeman, K.E.; Gomes, B.; de Brito, M.; Shamieh, O.; Harding, R. The burden of serious health-related suffering among cancer decedents: Global projections study to 2060. Palliat. Med. 2020, 35, 231–235. [Google Scholar] [CrossRef]
- Sleeman, K.E.; de Brito, M.; Etkind, S.; Nkhoma, K.; Guo, P.; Higginson, I.J.; Gomes, B.; Harding, R. The escalating global burden of serious health-related suffering: Projections to 2060 by world regions, age groups, and health conditions. Lancet Glob. Health 2019, 7, e883–e892. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization World Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2015.
- World Health Organization Europe Palliative Care for Older People: Better Practice; World Health Organization: Copenhagen, Denmark, 2011.
- Bone, A.E.; Evans, C.J.; Etkind, S.N.; Sleeman, K.E.; Gomes, B.; Aldridge, M.; Keep, J.; Verne, J.; Higginson, I.J. Factors associated with older people’s emergency department attendance towards the end of life: A systematic review. Eur. J. Public Health 2019, 29, 67–74. [Google Scholar] [CrossRef] [Green Version]
- Tan, W.S.; Bajpai, R.; Low, C.K.; Ho, A.H.Y.; Wu, H.Y.; Car, J. Individual, clinical and system factors associated with the place of death: A linked national database study. PLoS ONE 2019, 14, e0215566. [Google Scholar] [CrossRef]
- Riolfi, M.; Buja, A.; Zanardo, C.; Marangon, C.F.; Manno, P.; Baldo, V. Effectiveness of palliative home-care services in reducing hospital admissions and determinants of hospitalization for terminally ill patients followed up by a palliative home-care team: A retrospective cohort study. Palliat. Med. 2014, 28, 403–411. [Google Scholar] [CrossRef]
- Chen, C.Y.; Thorsteinsdottir, B.; Cha, S.S.; Hanson, G.J.; Peterson, S.M.; Rahman, P.A.; Naessens, J.M.; Takahashi, P.Y. Health care outcomes and advance care planning in older adults who receive home-based palliative care: A pilot cohort study. J. Palliat. Med. 2015, 18, 38–44. [Google Scholar] [CrossRef] [Green Version]
- Gomes, B.; Calanzani, N.; Curiale, V.; McCrone, P.; Higginson, I.J. Effectiveness and cost-effectiveness of home palliative care services for adults with advanced illness and their caregivers. Cochrane Database Syst. Rev. 2013, 6, CD007760-279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spilsbury, K.; Rosenwax, L. Community-based specialist palliative care is associated with reduced hospital costs for people with non-cancer conditions during the last year of life. BMC Palliat. Care 2017, 16, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spilsbury, K.; Rosenwax, L.; Arendts, G.; Semmens, J.B. The impact of community-based palliative care on acute hospital use in the last year of life is modified by time to death, age, and underlying cause of death. A population-based retrospective cohort study. PLoS ONE 2017, 12, e0185275. [Google Scholar] [CrossRef] [Green Version]
- Huang, C.M.; Shih, H.C.; Liu, C.J. Community hospice service analysis in Taipei City Hospital: Current status and future needs estimate. Taipei City Med. J. 2015, 12, 9–20. [Google Scholar]
- Huang, Y.-S.; Huang, S.-H. The obstacles of home hospice care in Taiwan. Taiwan J. Hosp. Palliat. Care 2017, 22, 180–191. [Google Scholar]
- Vandenbroucke, J.P.; Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Ann. Intern. Med. 2007, 147, 163–194. [Google Scholar] [CrossRef] [Green Version]
- Brumley, R.; Enguidanos, S.; Jamison, P.; Seitz, R.; Morgenstern, N.; Saito, S.; McIlwane, J.; Hillary, K.; Gonzalez, J. Increased satisfaction with care and lower costs: Results of a randomized trial of in-home palliative care. J. Am. Geriatr. Soc. 2007, 55, 993–1000. [Google Scholar] [CrossRef] [PubMed]
- Lustbader, D.; Mudra, M.; Romano, C.; Lukoski, E.; Chang, A.; Mittelberger, J.; Scherr, T.; Cooper, D. The impact of a home-based palliative care program in an accountable care organization. J. Palliat. Med. 2017, 20, 23–28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alonso-Babarro, A.; Astray-Mochales, J.; Domínguez-Berjón, F.; Gènova-Maleras, R.; Bruera, E.; Díaz-Mayordomo, A.; Centeno Cortes, C. The association between in-patient death, utilization of hospital resources and availability of palliative home care for cancer patients. Palliat. Med. 2012, 27, 68–75. [Google Scholar] [CrossRef]
- Costantini, M.; Higginson, I.J.; Boni, L.; Orengo, M.A.; Garrone, E.; Henriquet, F.; Bruzzi, P. Effect of a palliative home care team on hospital admissions among patients with advanced cancer. Palliat. Med. 2003, 17, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Miccinesi, G.; Crocetti, E.; Morino, P.; Fallai, M.; Piazza, M.; Cavallini, V.; Paci, E. Palliative home care reduces time spent in hospital wards: A population-based study in the Tuscany Region, Italy. Cancer Causes Control. 2003, 14, 971–977. [Google Scholar] [CrossRef]
- Phongtankuel, V.; Adelman, R.D.; Trevino, K.; Abramson, E.; Johnson, P.; Oromendia, C.; Henderson, C.R., Jr.; Reid, M.C. Association between nursing visits and hospital-related disenrollment in the home hospice population. Am. J. Hosp. Palliat. Med. 2018, 35, 316–323. [Google Scholar] [CrossRef]
- Cai, J.; Zhang, L.; Guerriere, D.; Coyte, P.C. Congruence between the preferred and actual place of death for those in receipt of home-based palliative care. J. Palliat. Med. 2020, 23, 1460–1467. [Google Scholar] [CrossRef]
- Fukui, S.; Kawagoe, H.; Masako, S.; Noriko, N.; Hiroko, N.; Toshie, M. Determinants of the place of death among terminally ill cancer patients under home hospice care in Japan. Palliat. Med. 2003, 17, 445–453. [Google Scholar] [CrossRef]
- Tang, S.T. Influencing factors of place of death among home care patients with cancer in Taiwan. Cancer Nurs. 2002, 25, 158–166. [Google Scholar] [CrossRef]
- Paramanandam, G.; Boohene, J.; Tran, K.; Volk-Craft, B.E. Impact of a hospital community-based palliative care partnership: Continuum from hospital to home. J. Palliat. Med. 2020, 23, 1599–1605. [Google Scholar] [CrossRef]
- Seow, H.; Brazil, K.; Sussman, J.; Pereira, J.; Marshall, D.; Austin, P.C.; Husain, A.; Rangrej, J.; Barbera, L. Impact of community-based, specialist palliative care teams on hospitalizations and emergency department visits late in life and hospital deaths: A pooled analysis. BMJ 2014, 348, g3496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, S.J.; Huang, C.Y.; Woung, L.C.; Lee, O.K.; Chu, D.C.; Huang, T.C.; Wang, Y.W.; Guo, P.; Harding, R.; Kellehear, A.; et al. The 2017 Taipei Declaration for health-promoting palliative care. J. Palliat. Med. 2018, 21, 581–582. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bennett, M.; Corcoran, G. The impact on community palliative care services of a hospital palliative care team. Palliat. Med. 1994, 8, 237–244. [Google Scholar] [CrossRef] [PubMed]
- de Graaf, E.; Zweers, D.; Valkenburg, A.C.; Uyttewaal, A.; Teunissen, S.C. Hospice assist at home: Does the integration of hospice care in primary healthcare support patients to die in their preferred location–a retrospective cross-sectional evaluation study. Palliat. Med. 2016, 30, 580–586. [Google Scholar] [CrossRef] [PubMed]
- Kamal, A.H.; Currow, D.C.; Ritchie, C.S.; Bull, J.; Abernethy, A.P. Community-based palliative care: The natural evolution for palliative care delivery in the US. J. Pain Symptom Manag. 2013, 46, 254–264. [Google Scholar] [CrossRef] [PubMed]


| Variables | Palliative Home Care Type (Before PSM) | p-Value | Palliative Home Care Type (After PSM) | p-Value | ||
|---|---|---|---|---|---|---|
| Hospital (n = 131) | Community (n = 43) | Hospital (n = 42) | Community (n = 42) | |||
| N (%)/Mean ± SD | N (%)/Mean ± SD | |||||
| Age | 74.38 ± 12.30 | 72.14 ± 12.81 | 0.31 | 71.33 ± 13.46 | 72.31 ± 12.92 | 0.74 |
| Gender | 0.60 | 0.66 | ||||
| Female | 79 (60.3%) | 24 (55.8%) | 22 (52.4%) | 24 (57.1%) | ||
| Male | 52 (39.7%) | 19 (44.2%) | 20 (47.6%) | 18 (42.9%) | ||
| Education | 0.99 | 0.52 | ||||
| ≦6 years | 70 (53.4%) | 23 (53.5%) | 18 (42.9%) | 23 (54.8%) | ||
| 7~12 years | 49 (37.4%) | 16 (37.2%) | 20 (47.6%) | 15 (35.7%) | ||
| >12 years | 12 (9.2%) | 4 (9.3%) | 4 (9.5%) | 4 (9.5%) | ||
| Marriage | 0.98 | 0.47 | ||||
| Single | 8 (6.1%) | 2 (4.7%) | 3 (7.1%) | 2 (4.8%) | ||
| Married | 68 (51.9%) | 22 (51.2%) | 27 (64.3%) | 21 (50.0%) | ||
| Widowed | 47 (35.9%) | 16 (37.20%) | 10 (23.8%) | 16 (38.1%) | ||
| Separated/ Divorced | 8 (6.1%) | 3 (7.0%) | 2 (4.8%) | 3 (7.1%) | ||
| Religion | 0.37 | 0.72 | ||||
| None | 33 (25.2%) | 10 (23.3%) | 12 (28.6%) | 10 (23.8%) | ||
| Buddhism | 43 (32.8%) | 12 (27.9%) | 12 (28.6%) | 12 (28.6%) | ||
| Christianity | 10 (7.6%) | 2 (4.7%) | 4 (9.5%) | 2 (4.8%) | ||
| Taoism/Folk religion | 45 (34.4%) | 18 (41.9%) | 14 (33.3%) | 18 (42.9%) | ||
| Other | 0 (0%) | 1 (2.3%) | 0 (0%) | 0 (0%) | ||
| ECOG | 0.23 | 0.25 | ||||
| 2 | 1 (0.8%) | 2 (4.7%) | 0 (0%) | 2 (4.8%) | ||
| 3 | 66 (50.4%) | 20 (46.5%) | 24 (57.1%) | 19 (45.2%) | ||
| 4 | 64 (48.9%) | 21 (48.8%) | 18 (42.9%) | 21 (50%) | ||
| Terminal Diagnosis | 0.64 | 0.99 | ||||
| Cancer | 117 (89.3%) | 42 (97.7%) | 41 (97.6%) | 41 (97.6%) | ||
| Brain disease | 7 (5.3%) | 1 (2.3%) | 1 (2.4%) | 1 (2.4%) | ||
| Organ failure | 6 (4.6%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| ALS | 1 (0.8%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Devices/Wounds/Infusion 1 | ||||||
| Nasogastric tube | 41 (31.3%) | 12 (27.9%) | 0.68 | 10 (23.8%) | 12 (28.6%) | 0.62 |
| Foley tube | 51 (38.9%) | 15 (34.9%) | 0.64 | 17 (40.5%) | 15 (35.7%) | 0.65 |
| Tracheostomy | 3 (2.3%) | 1 (2.3%) | 0.99 | 1 (2.4%) | 1 (2.4%) | 0.99 |
| Gastro-/Jejunostomy | 6 (4.6%) | 3 (7.0%) | 0.69 | 2 (4.8%) | 3 (7.1%) | 0.99 |
| Colostomy | 13 (9.9%) | 3 (7.0%) | 0.76 | 3 (7.1%) | 3 (7.1%) | 0.99 |
| Intravenous Fluid | 8 (6.1%) | 0 (0%) | 0.20 | 3 (7.1%) | 0 (0%) | 0.24 |
| Wound | 42 (32.1%) | 14 (32.6%) | 0.95 | 13 (31.0%) | 14 (33.3%) | 0.82 |
| Distance from nursing institution to patient’s home (km) | 3.92 ± 2.12 | 8.21 ± 5.23 | <0.01 | 3.71 ± 1.92 | 7.90 ± 4.86 | <0.01 |
| Distance from hospital to patient’s home (km) | 3.92 ± 2.23 | 9.29 ± 7.35 | <0.01 | 3.71 ± 1.92 | 8.72 ± 6.39 | <0.01 |
| Variables | Palliative Home Care Type (Before PSM) | p-Value | Palliative Home Care Type (After PSM) | p-Value | ||
|---|---|---|---|---|---|---|
| Hospital (n = 131) | Community (n = 43) | Hospital (n = 42) | Community (n = 42) | |||
| N (%)/Mean ± SD | N (%)/Mean ± SD | |||||
| Number of physician visits | 5.18 ± 5.46 | 3.09 ± 2.39 | <0.01 | 5.17 ± 6.56 | 3.14 ± 2.40 | 0.07 |
| Physician visit interval (day/time) | 15.59± 9.40 | 18.28 ± 15.63 | 0.29 | 15.00 ± 9.32 | 18.6 ± 15.61 | 0.20 |
| Number of nurse visits | 5.91 ± 5.93 | 9.98 ± 9.97 | 0.01 | 5.57 ± 6.95 | 10.19 ± 9.99 | 0.02 |
| Nurse visit interval (day/time) | 13.07± 8.66 | 6.30 ± 3.65 | <0.01 | 14.19 ± 9.25 | 6.40 ± 3.63 | <0.01 |
| Total days of care | 82.12 ± 95.38 | 61.30 ± 64.40 | 0.18 | 71.76 ± 95.5 | 62.71 ± 64.5 | 0.61 |
| The wait time between referral and acceptance to PHC | 9.53 ± 5.87 | 6.47 ± 5.41 | <0.01 | 9.45 ± 6.43 | 6.40 ± 5.46 | 0.02 |
| Ever been to ED after referred to PHC but not yet received PHC | 0.06 | 0.04 | ||||
| Yes | 21 (16%) | 2 (4.7%) | 8 (19.0%) | 2 (4.8%) | ||
| No | 110 (84%) | 41 (95.3%) | 34 (81.0%) | 40 (95.2%) | ||
| The total number of ED visits after referred to PHC but not yet received PHC | 0.18 ± 0.420 | 0.07 ± 0.33 | 0.10 | 0.21 ± 0.47 | 0.07 ± 0.34 | 0.12 |
| Ever been to the ED | 0.049 | 0.01 | ||||
| Yes | 86 (65.6%) | 21 (48.8%) | 31 (73.8%) | 20 (47.6%) | ||
| No | 45 (34.4%) | 22 (51.2%) | 11 (26.2%) | 22 (52.4%) | ||
| Number of ED visits | 0.90 ± 0.927 | 0.58 ± 0.698 | 0.04 | 1.07 ±0.92 | 0.57 ±0.70 | <0.01 |
| Ever been hospitalized | 0.73 | 0.36 | ||||
| Yes | 80 (61.1%) | 25 (58.1%) | 29 (69.0%) | 25 (59.5%) | ||
| No | 51 (38.9%) | 18 (41.9%) | 13 (31.0%) | 17 (40.5%) | ||
| Number of hospitalizations | 0.78 ± 0.797 | 0.77 ± 0.782 | 0.94 | 0.90 ± 0.85 | 0.79 ± 0.72 | 0.51 |
| The total length of hospital stays | 9.92 ± 13.59 | 7.23 ± 10.71 | 0.24 | 10.40 ± 12.54 | 7.40 ± 10.78 | 0.24 |
| The average length of hospital stay | 7.84 ± 10.12 | 5.03 ± 6.12 | 0.03 | 8.42 ± 10.32 | 5.15 ± 6.14 | 0.08 |
| Place of death | 0.13 | 0.02 | ||||
| Home | 47 (35.9%) | 22 (51.2%) | 12 (28.6%) | 22 (52.4%) | ||
| Nursing/residential home | 8 (6.1%) | 1 (2.3%) | 3 (7.1%) | 1 (2.4%) | ||
| Palliative care unit/inpatient hospice | 63 (48.1%) | 16 (37.2%) | 24 (57.1%) | 16 (38.1%) | ||
| General wards | 3 (2.3%) | 3 (7.0%) | 0 (0%) | 3 (7.1%) | ||
| Emergency department | 10 (7.6%) | 1 (2.3%) | 3 (7.1%) | 0 (0%) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, C.-P.; Tsay, M.-S.; Chang, Y.-H.; Chen, H.-C.; Wang, C.-Y.; Chuang, Y.-S.; Wu, C.-Y. A Comparison of the Survival, Place of Death, and Medical Utilization of Terminal Patients Receiving Hospital-Based and Community-Based Palliative Home Care: A Retrospective and Propensity Score Matching Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 7272. https://doi.org/10.3390/ijerph18147272
Lin C-P, Tsay M-S, Chang Y-H, Chen H-C, Wang C-Y, Chuang Y-S, Wu C-Y. A Comparison of the Survival, Place of Death, and Medical Utilization of Terminal Patients Receiving Hospital-Based and Community-Based Palliative Home Care: A Retrospective and Propensity Score Matching Cohort Study. International Journal of Environmental Research and Public Health. 2021; 18(14):7272. https://doi.org/10.3390/ijerph18147272
Chicago/Turabian StyleLin, Cheng-Pei, Min-Shiow Tsay, Yi-Hui Chang, Hung-Cheng Chen, Ching-Yu Wang, Yun-Shiuan Chuang, and Chien-Yi Wu. 2021. "A Comparison of the Survival, Place of Death, and Medical Utilization of Terminal Patients Receiving Hospital-Based and Community-Based Palliative Home Care: A Retrospective and Propensity Score Matching Cohort Study" International Journal of Environmental Research and Public Health 18, no. 14: 7272. https://doi.org/10.3390/ijerph18147272
APA StyleLin, C.-P., Tsay, M.-S., Chang, Y.-H., Chen, H.-C., Wang, C.-Y., Chuang, Y.-S., & Wu, C.-Y. (2021). A Comparison of the Survival, Place of Death, and Medical Utilization of Terminal Patients Receiving Hospital-Based and Community-Based Palliative Home Care: A Retrospective and Propensity Score Matching Cohort Study. International Journal of Environmental Research and Public Health, 18(14), 7272. https://doi.org/10.3390/ijerph18147272






