The Positive Role of Tai Chi in Responding to the COVID-19 Pandemic
Abstract
:1. Introduction
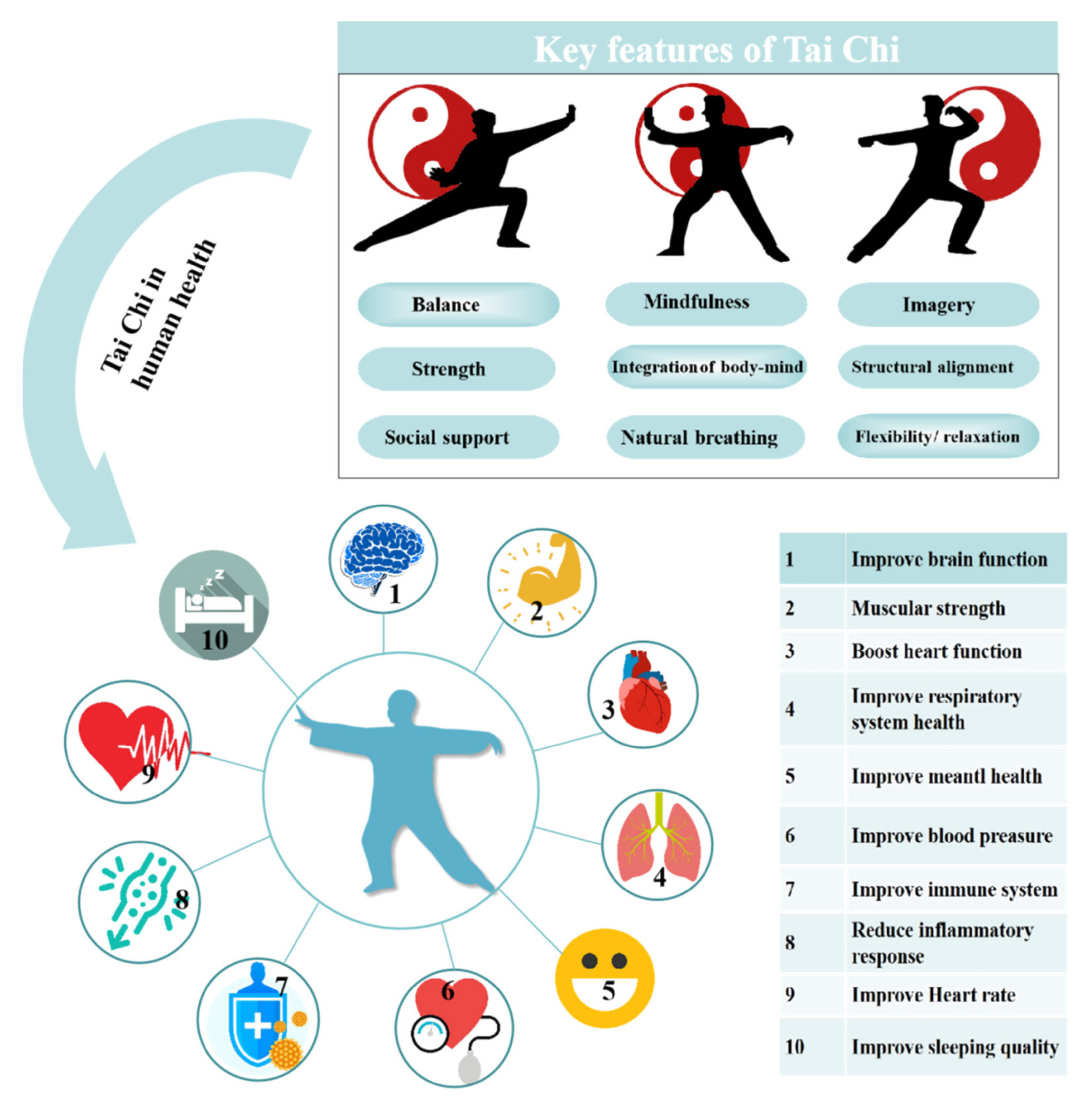
2. The Benefits of Tai Chi on Human Health
3. Effect of Tai Chi Practice on Immune Function and Inflammation
4. Application of Tai Chi to Rehabilitation in Pulmonary Function
5. Effects of Tai Chi Intervention on Negative Emotions (Anxiety and Depression)
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Jiang, X.; Niu, Y.; Li, X.; Li, L.; Cai, W.; Chen, Y.; Wang, E. Is a 14-day quarantine period optimal for effectively controlling coronavirus disease 2019 (COVID-19)? MedRxiv 2020. [Google Scholar] [CrossRef]
- Yarımkaya, E.; Esentürk, O.K. Promoting physical activity for children with autism spectrum disorders during Coronavirus outbreak: Benefits, strategies, and examples. Int. J. Dev. Disabil. 2020. [Google Scholar] [CrossRef]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Hoekelmann, A. Effects of COVID-19 home confinement on eating behaviour and physical activity: Results of the ECLB-COVID19 international online survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef]
- Kunstler, B.; Slattery, P.; Grundy, E.; Goodwin, D.; Saeri, A.K. Physical activity and sedentary behaviour during the COVID-19 pandemic: An Australian population study. OSF Prepr. 2020. [Google Scholar] [CrossRef]
- Qin, F.; Song, Y.; Nassis, G.P.; Zhao, L.; Cui, S.; Lai, L.; Zhao, J. Prevalence of insufficient physical activity, sedentary screen time and emotional well-being during the early days of the 2019 novel coronavirus (COVID-19) outbreak in China: A national cross-sectional study. Preprints 2020, 17, 5170. [Google Scholar] [CrossRef]
- Stanton, R.; To, Q.G.; Khalesi, S.; Williams, S.L.; Alley, S.J.; Thwaite, T.L.; Vandelanotte, C. Depression, anxiety and stress during COVID-19: Associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int. J. Environ. Res. Public Health 2020, 17, 4065. [Google Scholar] [CrossRef]
- Ammar, A.; Trabelsi, K.; Brach, M.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Batatia, H. Effects of home confinement on mental health and lifestyle behaviours during the COVID-19 outbreak: Insights from the ECLB-COVID19 multicentre study. Biol. Sport. 2021, 38, 9–21. [Google Scholar] [CrossRef] [PubMed]
- Buman, M.P.; Winkler, E.A.; Kurka, J.M.; Hekler, E.B.; Baldwin, C.M.; Owen, N.; Gardiner, P.A. Reallocating time to sleep, sedentary behaviors, or active behaviors: Associations with cardiovascular disease risk biomarkers, NHANES 2005–2006. Am. J. Epidemiol. 2014, 179, 323–334. [Google Scholar] [CrossRef]
- Chau, J.Y.; Grunseit, A.; Midthjell, K.; Holmen, J.; Holmen, T.L.; Bauman, A.E.; Van der Ploeg, H.P. Sedentary behaviour and risk of mortality from all-causes and cardiometabolic diseases in adults: Evidence from the HUNT3 population cohort. Br. J. Sports Med. 2015, 49, 737–742. [Google Scholar] [CrossRef]
- Koster, A.; Caserotti, P.; Patel, K.V.; Matthews, C.E.; Berrigan, D.; Van Domelen, D.R.; Harris, T.B. Association of sedentary time with mortality independent of moderate to vigorous physical activity. PLoS ONE 2012, 7, e37696. [Google Scholar] [CrossRef] [PubMed]
- Thorp, A.A.; Owen, N.; Neuhaus, M.; Dunstan, D.W. Sedentary behaviors and subsequent health outcomes in adults: A systematic review of longitudinal studies, 1996–2011. Am. J. Prev. Med. 2011, 41, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Wilmot, E.G.; Edwardson, C.L.; Achana, F.A.; Davies, M.J.; Gorely, T.; Gray, L.J.; Biddle, S.J. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: Systematic review and meta-analysis. Diabetologia 2012, 55, 2895–2905. [Google Scholar] [CrossRef]
- Galea, S.; Merchant, R.M.; Lurie, N. The mental health consequences of COVID-19 and physical distancing: The need for prevention and early intervention. JAMA Intern. Med. 2020, 180, 817–818. [Google Scholar] [CrossRef] [Green Version]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry 2020, 33, e100213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hawryluck, L.; Gold, W.L.; Robinson, S.; Pogorski, S.; Galea, S.; Styra, R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004, 10, 120–1212. [Google Scholar] [CrossRef]
- Reynolds, D.L.; Garay, J.R.; Deamond, S.L.; Moran, M.K.; Gold, W.; Styra, R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol. Infect. 2008, 136, 997–1007. [Google Scholar] [CrossRef] [PubMed]
- Bentlage, E.; Ammar, A.; How, D.; Ahmed, M.; Trabelsi, K.; Chtourou, H.; Brach, M. Practical recommendations for maintaining active lifestyle during the COVID-19 pandemic: A systematic literature review. Int. J. Environ. Res. Public Health 2020, 17, 6265. [Google Scholar] [CrossRef]
- Wang, M.; Baker, J.S.; Quan, W.; Shen, S.; Fekete, G.; Gu, Y. A preventive role of exercise across the coronavirus 2 (SARS-CoV-2) pandemic. Front. Physiol. 2020, 11, 572718. [Google Scholar] [CrossRef]
- Wayne, P.M.; Fuerst, M. The Harvard Medical School Guide to Tai Chi: 12 Weeks to a Healthy Body, Strong Heart, and Sharp Mind; Shambhala Publications: Boulder, CO, USA, 2013. [Google Scholar]
- Polero, P.; Rebollo-Seco, C.; Adsuar, J.C.; Pérez-Gómez, J.; Rojo-Ramos, J.; Manzano-Redondo, F.; Carlos-Vivas, J. Physical activity recommendations during COVID-19: Narrative review. Int. J. Environ. Res. Public Health 2021, 18, 65. [Google Scholar] [CrossRef]
- Easwaran, K.; Gopalasingam, Y.; Green, D.D.; Lach, V.; Melnyk, J.A.; Wan, C.; Bartlett, D.J. Effectiveness of Tai Chi for health promotion for adults with health conditions: A scoping review of meta-analyses. Disabil. Rehabil. 2020, 1–12. [Google Scholar] [CrossRef]
- Lan, C.; Chen, S.Y.; Lai, J.S.; Wong, A.M.K. Tai Chi Chuan in medicine and health promotion. Evid-Based Complalt. 2013, 2013, 502131. [Google Scholar] [CrossRef]
- Liu, J.; Chen, P.; Wang, R.; Yuan, Y.; Li, C. Effect of Tai Chi exercise on immune function in middle-aged and elderly women. J. Sports Med. Doping Stud. 2012, 2, 2161-0673. [Google Scholar] [CrossRef]
- Oh, B.; Bae, K.; Lamoury, G.; Eade, T.; Boyle, F.; Corless, B.; Back, M. The effects of tai chi and qigong on immune responses: A systematic review and meta-analysis. Medicines 2020, 7, 39. [Google Scholar] [CrossRef]
- Yang, Y.; Verkuilen, J.; Rosengren, K.S.; Mariani, R.A.; Reed, M.; Grubisich, S.A.; Woods, J.A. Effects of a Taiji and Qigong intervention on the antibody response to influenza vaccine in older adults. Am. J. Chin. Med. 2007, 35, 597–607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oh, B.; Butow, P.N.; Mullan, B.A.; Clarke, S.J.; Beale, P.J.; Pavlakis, N.; Vardy, J. Effect of medical Qigong on cognitive function, quality of life, and a biomarker of inflammation in cancer patients: A randomized controlled trial. Support Care Cancer 2012, 20, 1235–1242. [Google Scholar] [CrossRef]
- Campo, R.A.; Light, K.C.; O’Connor, K.; Nakamura, Y.; Lipschitz, D.; LaStayo, P.C.; Kinney, A.Y. Blood pressure, salivary cortisol, and inflammatory cytokine outcomes in senior female cancer survivors enrolled in a tai chi chih randomized controlled trial. J. Cancer Surviv. 2015, 9, 115–125. [Google Scholar] [CrossRef] [Green Version]
- Irwin, M.R.; Olmstead, R.; Breen, E.C.; Witarama, T.; Carrillo, C.; Sadeghi, N.; Cole, S. Cognitive behavioral therapy and tai chi reverse cellular and genomic markers of inflammation in late-life insomnia: A randomized controlled trial. Biol. Psychiatry 2015, 78, 721–729. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robins, J.L.; ElswickJr, R.K.; Sturgill, J.; McCain, N.L. The effects of tai chi on cardiovascular risk in women. Am. J. Health Promot. 2016, 30, 613–622. [Google Scholar] [CrossRef] [Green Version]
- Libby, P. Inflammatory mechanisms: The molecular basis of inflammation and disease. Nutr. Rev. 2007, 65, S140–S146. [Google Scholar] [CrossRef]
- Jose, R.J.; Manuel, A. COVID-19 cytokine storm: The interplay between inflammation and coagulation. Lancet Respir. Med. 2020, 8, 46–47. [Google Scholar] [CrossRef]
- Stebbing, J.; Phelan, A.; Griffin, I.; Tucker, C.; Oechsle, O.; Smith, D.; Richardson, P. COVID-19: Combining antiviral and anti-inflammatory treatments. Lancet Infect. Dis. 2020, 20, 400–402. [Google Scholar] [CrossRef]
- Zhang, L.; Li, C.; Zhou, Y.; Wang, B.; Zhang, J. Persistent viral shedding lasting over 60 days in a mild COVID-19 patient with ongoing positive SARS-CoV-2. Quant. Imaging Med. Surg. 2020, 10, 1141. [Google Scholar] [CrossRef]
- Ratarasarn, K.; Kundu, A. Yoga and Tai Chi: A mind–body approach in managing respiratory symptoms in obstructive lung diseases. Curr. Opin. Pulm. Med. 2020, 26, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Leung, R.W.; McKeough, Z.J.; Alison, J.A. Tai Chi as a form of exercise training in people with chronic obstructive pulmonary disease. Expert Rev. Respir. Med. 2013, 7, 587–592. [Google Scholar] [CrossRef]
- Moy, M.L.; Wayne, P.M.; Litrownik, D.; Beach, D.; Klings, E.S.; Davis, R.B.; Yeh, G.Y. Long-term Exercise After Pulmonary Rehabilitation (LEAP): Design and rationale of a randomized controlled trial of Tai Chi. Contemp. Clin. Trials. 2015, 45, 458–467. [Google Scholar] [CrossRef] [Green Version]
- Jerath, R.; Edry, J.W.; Barnes, V.A.; Jerath, V. Physiology of long pranayamic breathing: Neural respiratory elements may provide a mechanism that explains how slow deep breathing shifts the autonomic nervous system. Med. Hypotheses 2006, 67, 566–571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pal, G.K.; Velkumary, S. Effect of short-term practice of breathing exercises on autonomic functions in normal human volunteers. Indian J. Med. Res. 2004, 120, 115. [Google Scholar]
- Peng, C.K.; Mietus, J.E.; Liu, Y.; Khalsa, G.; Douglas, P.S.; Benson, H.; Goldberger, A.L. Exaggerated heart rate oscillations during two meditation techniques. Int. J. Cardiol. 1999, 70, 101–107. [Google Scholar] [CrossRef]
- Ngai, S.P.; Jones, A.Y.; San Tam, W.W. Tai Chi for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst. Rev. 2016, 6, 1–74. [Google Scholar] [CrossRef]
- Li, P.; Liu, J.; Lu, Y.; Liu, X.; Wang, Z.; Wu, W. Effects of long-term home-based Liuzijue exercise combined with clinical guidance in elderly patients with chronic obstructive pulmonary disease. Clin. Interv. Aging. 2018, 13, 1391. [Google Scholar] [CrossRef] [Green Version]
- Lan, C.; Chen, S.Y.; Lai, J.S. Relative exercise intensity of Tai Chi Chuan is similar in different ages and gender. Am. J. Chinese Med. 2004, 32, 151–160. [Google Scholar] [CrossRef]
- Lu, X.; Hui-Chan, C.W.; Tsang, W.W. Tai Chi, arterial compliance, and muscle strength in older adults. Eur. J. Prev. Cardiol. 2013, 20, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Bannuru, R.; Ramel, J.; Kupelnick, B.; Scott, T.; Schmid, C.H. Tai Chi on psychological well-being: Systematic review and meta-analysis. BMC Complement. Altern. 2010, 10, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.; Schmid, C.H.; Fielding, R.A.; Harvey, W.F.; Reid, K.F.; Price, L.L.; McAlindon, T. Effect of tai chi versus aerobic exercise for fibromyalgia: Comparative effectiveness randomized controlled trial. BMJ 2018, 360, k851. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Ni, X.; Chen, P. Study about the effects of different fitness sports on cognitive function and emotion of the aged. Cell Biochem. Biophys. 2014, 70, 1591–1596. [Google Scholar] [CrossRef] [PubMed]
- Zheng, S.; Kim, C.; Lal, S.; Meier, P.; Sibbritt, D.; Zaslawski, C. The Effects of Twelve Weeks of Tai Chi Practice on Anxiety in Stressed But Healthy People Compared to Exercise and Wait-List Groups–A Randomized Controlled Trial. J. Clin. Psychol. 2018, 74, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann-Smith, K.A.; Ma, A.; Yeh, C.T.; DeGuire, N.L.; Smith, J.P. The effect of tai chi in reducing anxiety in an ambulatory population. J. Complement. Integr. Med. 2009, 6, 1–14. [Google Scholar]
- Zhang, S.; Zou, L.; Chen, L.Z.; Yao, Y.; Loprinzi, P.D.; Siu, P.M.; Wei, G.X. The Effect of Tai Chi Chuan on negative emotions in non-clinical populations: A meta-analysis and systematic review. Int. J. Environ. Res. Public Health 2019, 16, 3033. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siu, J.Y.M. Coping with future epidemics: T ai chi practice as an overcoming strategy used by survivors of severe acute respiratory syndrome (SARS) in post-SARS H ong K ong. Health Expect. 2016, 19, 762–772. [Google Scholar] [CrossRef]
- Goyal, M.; Singh, S.; Sibinga, E.M.; Gould, N.F.; Rowland-Seymour, A.; Sharma, R.; Haythornthwaite, J.A. Meditation programs for psychological stress and well-being: A systematic review and meta-analysis. JAMA Intern. Med. 2014, 174, 357–368. [Google Scholar] [CrossRef] [Green Version]
- Stonerock, G.L.; Hoffman, B.M.; Smith, P.J.; Blumenthal, J.A. Exercise as treatment for anxiety: Systematic review and analysis. Ann. Behav. Med. 2015, 49, 542–556. [Google Scholar] [CrossRef] [Green Version]
- Zou, L.; Yeung, A.; Quan, X.; Hui, S.S.C.; Hu, X.; Chan, J.S.; Wang, H. Mindfulness-based Baduanjin exercise for depression and anxiety in people with physical or mental illnesses: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2018, 15, 321. [Google Scholar] [CrossRef] [Green Version]
- Appelhans, B.M.; Luecken, L.J. Heart rate variability as an index of regulated emotional responding. Rev. Gen. Psychol. 2006, 10, 229–240. [Google Scholar] [CrossRef] [Green Version]
- Mather, M.; Thayer, J.F. How heart rate variability affects emotion regulation brain networks. Curr. Opin. Behav. Sci. 2018, 19, 98–104. [Google Scholar] [CrossRef]
- Wei, G.X.; Li, Y.F.; Yue, X.L.; Ma, X.; Chang, Y.K.; Yi, L.Y.; Zuo, X.N. Tai Chi Chuan modulates heart rate variability during abdominal breathing in elderly adults. PsyCh J. 2016, 5, 69–77. [Google Scholar] [CrossRef]
- Chen, S.; Jiang, H.; Liu, Y.; Hou, Z.; Yue, Y.; Zhang, Y.; Yuan, Y. Combined serum levels of multiple proteins in tPA-BDNF pathway may aid the diagnosis of five mental disorders. Sci. Rep. 2017, 7, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hosang, G.M.; Shiles, C.; Tansey, K.E.; McGuffin, P.; Uher, R. Interaction between stress and the BDNF Val66Met polymorphism in depression: A systematic review and meta-analysis. BMC Med. 2014, 12, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sungkarat, S.; Boripuntakul, S.; Kumfu, S.; Lord, S.R.; Chattipakorn, N. Tai Chi improves cognition and plasma BDNF in older adults with mild cognitive impairment: A randomized controlled trial. Neurorehabilit. Neural Repair. 2018, 32, 142–149. [Google Scholar] [CrossRef]
- Xianjian, C.; Datao, X. Effects of Tai Chi Chuan on the Physical and Mental Health of the Elderly: A Systematic Review. Phys. Act. Health 2021, 5, 21–27. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, S.; Baker, J.S.; Ren, F. The Positive Role of Tai Chi in Responding to the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 7479. https://doi.org/10.3390/ijerph18147479
Xu S, Baker JS, Ren F. The Positive Role of Tai Chi in Responding to the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2021; 18(14):7479. https://doi.org/10.3390/ijerph18147479
Chicago/Turabian StyleXu, Suodi, Julien S. Baker, and Feng Ren. 2021. "The Positive Role of Tai Chi in Responding to the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 18, no. 14: 7479. https://doi.org/10.3390/ijerph18147479
APA StyleXu, S., Baker, J. S., & Ren, F. (2021). The Positive Role of Tai Chi in Responding to the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 18(14), 7479. https://doi.org/10.3390/ijerph18147479






