Effects of Exercise Training on Cardiopulmonary Function and Quality of Life in Elderly Patients with Pulmonary Fibrosis: A Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Registration
2.2. Literature Search Strategy
2.3. Selection Criteria
2.3.1. Inclusion Criteria
2.3.2. Exclusion Criteria
2.4. Reported Methodological Quality Assessment
2.5. Data Management
2.5.1. Outcomes
2.5.2. Statistical Analysis
3. Results
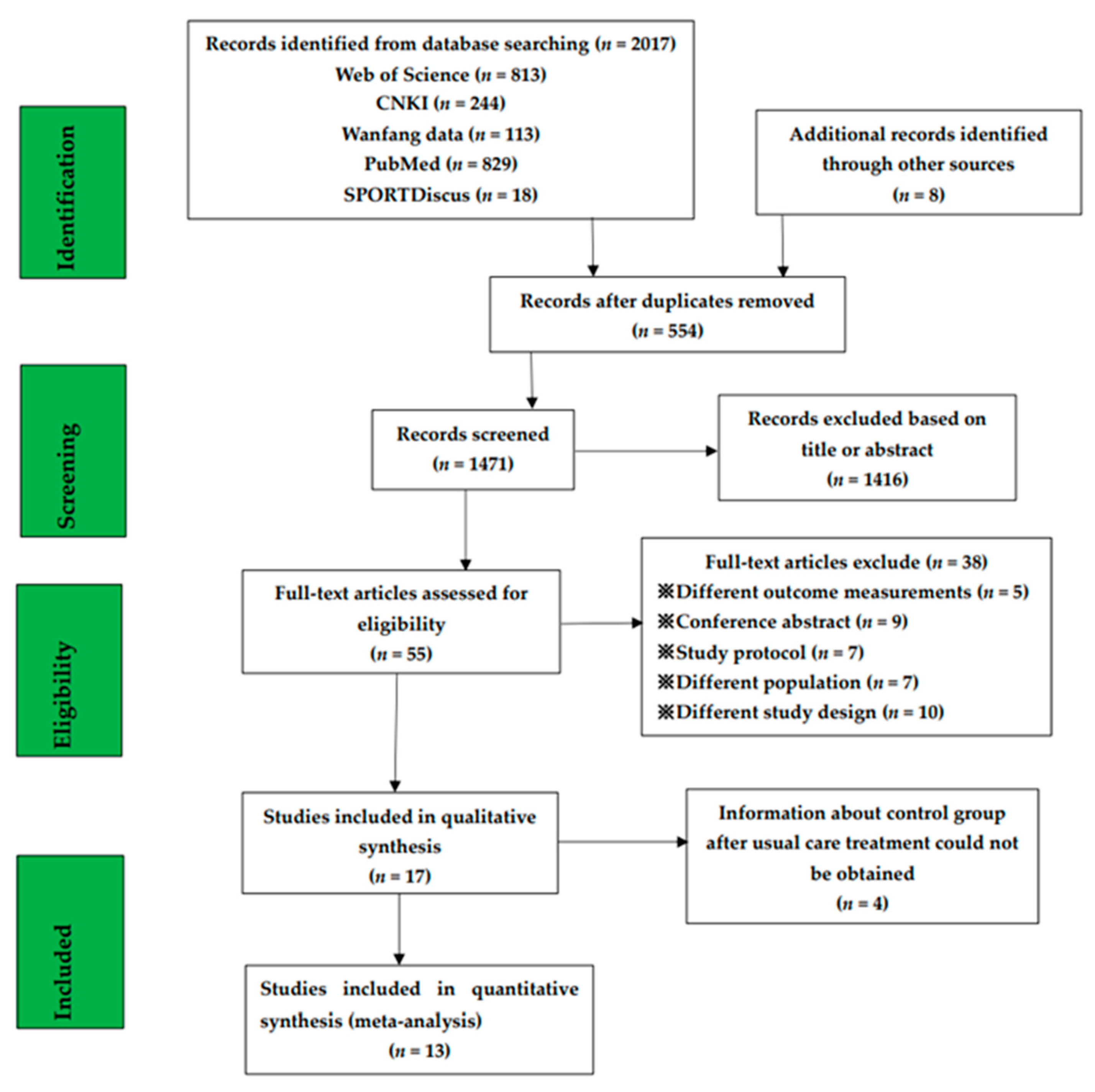
3.1. Search Results and Reported Quality
3.2. Cardiopulmonary Function
- 6MWD: The 6MWD was evaluated in eleven studies (nine GQ [16,17,19,24,26,28,29,30,31], two FQ [32,33]). The effect sizes were calculated according to Cohen’s d. The difference of the 6MWD between two conditions supported PF patients in exercise training (Cohen’s d = 0.77, MD: 34.04; 95% CI: 26.50 to 41.58; Z = 8.85, p < 0.01) (Figure 2). According to the information (exercise frequency, intensity, type, duration, age and BMI), we conducted the subgroup analysis (Table 3). This showed significant differences in frequency, intensity, type, and age on the 6MWD results (Table 3). Compared with the high frequency group (>60 min × 2/week; Cohen’ d = 0.82, p = 0.001), the 6MWD in the low frequency group (≤60 min × 2; Cohen’s d = 0.62) was higher. The 6MWD was higher at moderate exercise intensity (Cohen’s d = 0.78) than at light exercise intensity (Cohen’s d = 0.77, p = 0.004). Seven studies evaluated aerobic–resistance exercise (five GQ [17,24,28,30,31], two FQ [32,33]; Cohen’s d = 0.77, p < 0.01); one GQ study [29] evaluated aerobic–flexibility exercise (Cohen’s d = 0.13, p = 0.76); and three GQ studies [16,19,26] evaluated aerobic–resistance–flexibility–breathing exercise (Cohen’s d = 0.92, p < 0.01). Combined aerobic–resistance–flexibility–breathing exercise produced higher 6MWD (p = 0.0008). Three GQ studies [19,26,30] evaluated a long duration (Cohen’s d = 0.77, p < 0.01), and ten studies (eight GQ [16,17,19,24,28,29,30,31], two FQ [32,33]) evaluated a short duration (Cohen’s d = 0.78, p < 0.01). Although the exercise duration difference between subgroups was significant (p = 0.04), the confidence intervals overlapped. Hence, we concluded that there was no difference between exercise duration subgroups. Four GQ studies [17,29,31,33] evaluated subjects older than 70 (Cohen’s d = 0.45, p = 0.14), seven studies (six GQ [16,19,24,26,28,30], one FQ [32]) evaluated those 70 or younger (Cohen’s d = 0.86, p < 0.01). The 6MWD differences between the age subgroups (p < 0.01) suggested that the group aged under 70 derived more benefits from exercise training. Pertaining to BMI, five studies (four GQ [16,19,26,30], one FQ [33]) evaluated high BMI groups (Cohen’s d = 1.03, p < 0.01) and one GQ study [28] evaluated a low BMI group (Cohen’s d = 0.38, p = 0.30). Differences were not observed between two BMI levels (p = 0.62).
- Peak VO2: Peak VO2 was evaluated in four GQ studies [16,19,26,27]. The difference of the peak VO2 between two conditions supported PF patients engaging in exercise training (Cohen’s d = 0.45, MD: 1.13; 95% CI: 0.45 to 1.82; Z = 3.23, p = 0.0001) (Figure 3). Due to the high heterogeneity (I2 = 68%), a subgroup analysis of exercise duration was performed (Table 3). It that showed two GQ studies [26,27] focused on long durations (Cohen’s d = 0.74, p = 0.84) and three GQ studies [16,27,29] focused on short durations (Cohen’s d = 0.05, p < 0.01). Although the exercise duration difference between subgroups was significant (p = 0.03), the confidence intervals overlapped. Accordingly, we conclude that exercise duration has no effect on peak VO2.
- FVC% pred: FVC% pred was evaluated in three GQ studies [16,19,26]. The synthesized FVC% pred encouraged patients with PF to engage in exercise training (Cohen’s d = 0.42, MD: 3.94; 95% CI: 0.91 to 6.96; Z = 2.55, p = 0.01) (Figure 4). No difference was observed when we compared two exercise duration subgroups (p = 0.35) (Table 3).
- DLCO% pred: Five studies were included in the meta-analysis to provide DLCO% pred numerical data (four GQ [16,19,26,30], one FQ [32]). The combined DLCO% pred did not support patients with PF engaging in exercise training (Cohen’s d = 0.16, MD: 1.86; 95% CI: −0.37 to 4.09; Z = 1.63, p = 0.10) (Figure 5). Exercise frequency, duration, intensity and type subgroups had no significant difference in DLCO% pred results (p = 0.93, 0.84, 0.86, 0.86) (Table 3).
- TLC% pred: TLC% pred was evaluated in two GQ studies [16,26]. The difference of the TLC% pred between two conditions did not support patients with PF engaging in exercise training (Cohen’s d = 0.02, MD: 0.07; 95% CI: −6.53 to 6.67; Z = 0.02, p = 0.98) (Figure 6). There was no significant difference between the two exercise duration subgroups (p = 0.90) (Table 3).
3.3. Quality of Life
- SGRQ: SGRQ was evaluated in nine studies (eight GQ [2,16,19,26,27,28,30,31], one FQ [33]). The synthesized SGRQ in this study encouraged patients with PF to engage in exercise training (Cohen’s d = 0.89, MD: −8.79; 95% CI: −10.37 to −7.21; Z = 10.93, p < 0.01) (Figure 7). According to the relevant information (exercise frequency, intensity, type, duration, age and BMI), we conducted the subgroup analysis (Table 3). The results showed that SGRQ scores were not affected by exercise frequency, intensity, duration, type, age or BMI. Five studies (four GQ [28,29,30,31], one FQ [33]) evaluated aerobic–resistance exercise (Cohen’s d = 0.67, p = 0.0005), and four GQ studies [16,19,26,27] evaluated aerobic–resistance–flexibility–breathing exercise (Cohen’s d = 1.35, p < 0.01). There were no differences in exercise type between subgroups (p = 0.97). Two GQ studies [19,26] evaluated long duration (Cohen’s d = 1.00, p < 0.01), eight studies (seven GQ [2,16,19,27,28,30,31], one FQ [33]) evaluated short durations (Cohen’s d = 0.82, p < 0.01). There were no differences in exercise duration between subgroups (p = 0.43). Three studies (two GQ [2,31], one FQ [33]) evaluated subjects older than 70 (Cohen’s d = 0.63, p = 0.003); six GQ studies [16,19,26,27,28,30] evaluated those 70 or younger (Cohen’s d = 0.94, p < 0.01). There were no differences in age between subgroups (p = 0.33). Six studies (five GQ [16,19,26,27,30], one FQ [33]) evaluated high BMI (Cohen’s d = 1.00, p < 0.01), and one GQ study [28] evaluated low BMI (Cohen’s d = 0.30, p = 0.41). There were no differences in BMI between subgroups (p = 0.71).
- mMRC: mMRC was evaluated in three GQ studies [19,24,27]. The difference in the mMRC between two conditions supported patients with PF engaging in exercise training (Cohen’s d = 0.64, MD: −0.58; 95% CI: −0.79 to −0.36; Z = 5.21, p < 0.01) (Figure 8). Due to the high heterogeneity (I2 = 67%), subgroup analysis on exercise intensity, type and duration was performed (Table 3). The subgroup analysis showed significant differences in intensity and type on the mMRC. Although the exercise duration difference between subgroups was significant (p = 0.02), the confidence intervals overlapped. Hence, we conclude that there is no difference between exercise duration subgroups. The mMRC was higher at light exercise intensity (Cohen’s d = 1.11) and aerobic–resistance–flexibility–breathing exercise (Cohen’s d = 1.11) than at moderate exercise intensity (Cohen’s d = 0.30) and aerobic–resistance exercise (Cohen’s d = 0.30, p = 0.004).
3.4. Publication Bias
4. Discussion
4.1. Cardiopulmonary Function
4.1.1. Cardiopulmonary Endurance
4.1.2. Pulmonary Function
4.2. Quality of Life
4.3. Advantages and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Oldham, J.M.; Noth, I. Idiopathic pulmonary fibrosis: Early detection and referral. Respir. Med. 2014, 108, 819–829. [Google Scholar] [CrossRef] [Green Version]
- Gaunaurd, I.A.; Gómez-Marín, O.W.; Ramos, C.F.; Sol, C.M.; Cohen, M.I.; Cahalin, L.P.; Cardenas, D.D.; Jackson, R.M. Physical activity and quality of life improvements of patients with idiopathic pulmonary fibrosis completing a pulmonary rehabilitation program. Respir. Care 2014, 59, 1872–1879. [Google Scholar] [CrossRef] [Green Version]
- Gribbin, J.; Hubbard, R.B.; Le Jeune, I.; Smith, C.J.; West, J.; Tata, L.J. Incidence and mortality of idiopathic pulmonary fibrosis and sarcoidosis in the UK. Thorax 2006, 61, 980–985. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fell, C.D.; Martinez, F.J.; Liu, L.X.; Murray, S.; Han, M.K.; Kazerooni, E.A.; Gross, B.H.; Myers, J.; Travis, W.D.; Colby, T.V.; et al. Clinical predictors of a diagnosis of idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 2010, 181, 832–837. [Google Scholar] [CrossRef] [PubMed]
- Sheng, G.; Chen, P.; Wei, Y.; Yue, H.; Chu, J.; Zhao, J.; Wang, Y.; Zhang, W.; Zhang, H.L. Viral infection increases the risk of idiopathic pulmonary fibrosis: A meta-analysis. Chest 2020, 157, 1175–1187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atabati, E.; Dehghani-Samani, A.; Mortazavimoghaddam, S.G. Association of COVID-19 and other viral infections with interstitial lung diseases, pulmonary fibrosis, and pulmonary hypertension: A narrative review. Can. J. Respir. Ther. CJRT Rev. 2020, 56, 1. [Google Scholar]
- Xie, L.; Liu, Y.; Xiao, Y.; Tian, Q.; Fan, B.; Zhao, H.; Chen, W. Follow-up study on pulmonary function and lung radiographic changes in rehabilitating severe acute respiratory syndrome patients after discharge. Chest 2005, 127, 2119–2124. [Google Scholar] [CrossRef] [Green Version]
- Hui, D.S.; Joynt, G.M.; Wong, K.T.; Gomersall, C.D.; Li, T.S.; Antonio, G.; Ko, F.W.; Chan, M.C.; Chan, D.P.; Tong, M.W.; et al. Impact of severe acute respiratory syndrome (SARS) on pulmonary function, functional capacity and quality of life in a cohort of survivors. Thorax 2005, 60, 401–409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, P.; Qie, S.; Liu, Z.; Ren, J.; Li, K.; Xi, J. Clinical characteristics of hospitalized patients with SARS-CoV-2 infection: A single arm meta-analysis. J. Med. Virol. 2020, 92, 612–617. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nathan, S.D.; Albera, C.; Bradford, W.Z.; Costabel, U.; Glaspole, I.; Glassberg, M.K.; Kardatzke, D.R.; Daigl, M.; Kirchgaessler, K.U.; Lancaster, L.H.; et al. Effect of pirfenidone on mortality: Pooled analyses and meta-analyses of clinical trials in idiopathic pulmonary fibrosis. Lancet Respir. Med. 2017, 5, 33–41. [Google Scholar] [CrossRef]
- Richeldi, L.; Du Bois, R.M.; Raghu, G.; Azuma, A.; Brown, K.K.; Costabel, U.; Cottin, V.; Flaherty, K.R.; Hansell, D.M.; Inoue, Y.; et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. New Engl. J. Med. 2014, 370, 2071–2082. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borie, R.; Justet, A.; Beltramo, G.; Manali, E.D.; Pradère, P.; Spagnolo, P.; Crestani, B. Pharmacological management of IPF. Respirology 2016, 21, 615–625. [Google Scholar] [PubMed] [Green Version]
- Hanada, M.; Kasawara, K.T.; Mathur, S.; Rozenberg, D.; Kozu, R.; Hassan, S.A.; Reid, W.D. Aerobic and breathing exercises improve dyspnea, exercise capacity and quality of life in idiopathic pulmonary fibrosis patients: Systematic review and meta-analysis. J. Thorac. Dis. 2020, 12, 1041. [Google Scholar] [CrossRef]
- Suresh, M.; Chandrashekar, M. The Effect Of Short, Intermediate And Long Duration Of Swimming On Pulmonary Function Tests. IOSR J. Pharm. Biol. Sci. 2012, 44, 2278–3008. [Google Scholar]
- Vainshelboim, B. Exercise training in idiopathic pulmonary fibrosis: Is it of benefit? Breathe 2016, 12, 130–138. [Google Scholar] [CrossRef] [Green Version]
- Vainshelboim, B.; Oliveira, J.; Yehoshua, L.; Weiss, I.; Fox, B.D.; Fruchter, O.; Kramer, M.R. Exercise training-based pulmonary rehabilitation program is clinically beneficial for idiopathic pulmonary fibrosis. Respiration 2014, 88, 378–388. [Google Scholar] [CrossRef]
- Dowman, L.; Hill, C.J.; May, A.; Holland, A.E. Pulmonary rehabilitation for interstitial lung disease. Cochrane Database Syst. Rev. 2021. [Google Scholar] [CrossRef]
- Dale, M.T.; McKeough, Z.J.; Munoz, P.A.; Corte, P.; Bye, P.T.; Alison, J.A. Exercise training for asbestos-related and other dust-related respiratory diseases: A randomised controlled trial. BMC Pulm. Med. 2014, 14, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Vainshelboim, B.; Fox, B.D.; Kramer, M.R.; Izhakian, S.; Gershman, E.; Oliveira, J. Short-term improvement in physical activity and body composition after supervised exercise training program in idiopathic pulmonary fibrosis. Arch. Phys. Med. Rehabil. 2016, 97, 788–797. [Google Scholar] [CrossRef]
- Ryerson, C.J.; Cayou, C.; Topp, F.; Hilling, L.; Camp, P.G.; Wilcox, P.G.; Khalil, N.; Collard, H.R.; Garvey, C. Pulmonary rehabilitation improves long-term outcomes in interstitial lung disease: A prospective cohort study. Respir. Med. 2014, 108, 203–210. [Google Scholar] [CrossRef] [Green Version]
- Holland, A.E.; Hill, C.J.; Glaspole, I.; Goh, N.; McDonald, C.F. Predictors of benefit following pulmonary rehabilitation for interstitial lung disease. Respir. Med. 2012, 106, 429–435. [Google Scholar] [CrossRef] [Green Version]
- Orimo, H.; Ito, H.; Suzuki, T.; Araki, A.; Hosoi, T.; Sawabe, M. Reviewing the definition of “elderly”. Geriatr. Gerontol. Int. 2006, 6, 149–158. [Google Scholar] [CrossRef]
- Dowman, L.M.; McDonald, C.F.; Hill, C.J.; Lee, A.L.; Barker, K.; Boote, C.; Glaspole, I.; Goh, N.S.; Southcott, A.M.; Burge, A.T.; et al. The evidence of benefits of exercise training in interstitial lung disease: A randomised controlled trial. Thorax 2017, 72, 610–619. [Google Scholar] [CrossRef] [Green Version]
- Holland, A.E.; Hill, C.J.; Conron, M.; Munro, P.; McDonald, C.F. Short term improvement in exercise capacity and symptoms following exercise training in interstitial lung disease. Thorax 2008, 63, 549–554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vainshelboim, B.; Oliveira, J.; Fox, B.D.; Soreck, Y.; Fruchter, O.; Kramer, M.R. Long-term effects of a 12-week exercise training program on clinical outcomes in idiopathic pulmonary fibrosis. Lung 2015, 193, 345–354. [Google Scholar] [CrossRef]
- Vainshelboim, B.; Kramer, M.R.; Fox, B.D.; Izhakian, S.; Sagie, A.; Oliveira, J. Supervised exercise training improves exercise cardiovascular function in idiopathic pulmonary fibrosis. Eur. J. Phys. Rehabil. Med. 2016, 53, 209–218. [Google Scholar]
- Nishiyama, O.; Kondoh, Y.; Kimura, T.; Kato, K.; Kataoka, K.; Ogawa, T.; Watanabe, F.; Arizono, S.; Nishimura, K.; Taniguchi, H. Effects of pulmonary rehabilitation in patients with idiopathic pulmonary fibrosis. Respirology 2008, 13, 394–399. [Google Scholar] [CrossRef]
- Jackson, R.M.; Gómez-Marín, O.W.; Ramos, C.F.; Sol, C.M.; Cohen, M.I.; Gaunaurd, I.A.; Cahalin, L.P.; Cardenas, D.D. Exercise limitation in IPF patients: A randomized trial of pulmonary rehabilitation. Lung 2014, 192, 367–376. [Google Scholar] [CrossRef]
- Arizono, S.; Taniguchi, H.; Sakamoto, K.; Kondoh, Y.; Kimura, T.; Kataoka, K.; Ogawa, T.; Watanabe, F.; Nishiyama, O.; Nishimura, K.; et al. Endurance time is the most responsive exercise measurement in idiopathic pulmonary fibrosis. Respir. Care 2014, 59, 1108–1115. [Google Scholar] [CrossRef] [Green Version]
- Perez-Bogerd, S.; Wuyts, W.; Barbier, V.; Demeyer, H.; Van Muylem, A.; Janssens, W.; Troosters, T. Short and long-term effects of pulmonary rehabilitation in interstitial lung diseases: A randomised controlled trial. Respir. Res. 2018, 19, 1–10. [Google Scholar] [CrossRef]
- Yuen, H.K.; Lowman, J.D.; Oster, R.A.; De Andrade, J.A. Home-based pulmonary rehabilitation for patients with idiopathic pulmonary fibrosis: A pilot study. J. Cardiopulm. Rehabil. Prev. 2019, 39, 281–284. [Google Scholar] [CrossRef]
- Wapenaar, M.; Bendstrup, E.; Molina-Molina, M.; Stessel, M.K.; Huremovic, J.; Bakker, E.W.; Kardys, I.; Aerts, J.G.; Wijsenbeek, M.S. The effect of the walk-bike on quality of life and exercise capacity in patients with idiopathic pulmonary fibrosis: A feasibility study. Sarcoidosis Vasc. Diffus. Lung Dis. 2020, 37, 192. [Google Scholar]
- Lee, D.C.; Artero, E.G.; Sui, X.; Blair, S.N. Mortality trends in the general population: The importance of cardiorespiratory fitness. J. Psychopharmacol. 2010, 24 (Suppl. 4), 27–35. [Google Scholar] [CrossRef]
- Sui, X.; LaMonte, M.J.; Blair, S.N. Cardiorespiratory fitness as a predictor of nonfatal cardiovascular events in asymptomatic women and men. Am. J. Epidemiol 2007, 165, 1413–1423. [Google Scholar] [CrossRef] [PubMed]
- Kodama, S.; Saito, K.; Tanaka, S.; Maki, M.; Yachi, Y.; Asumi, M.; Sugawara, A.; Totsuka, K.; Shimano, H.; Ohashi, Y.; et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis. JAMA 2009, 301, 2024–2035. [Google Scholar] [CrossRef] [Green Version]
- Blair, S.N.; Kohl, H.W.; Paffenbarger, R.S.; Clark, D.G.; Cooper, K.H.; Gibbons, L.W. Physical fitness and all-cause mortality: A prospective study of healthy men and women. JAMA 1989, 262, 2395–2401. [Google Scholar] [CrossRef] [PubMed]
- Wells, A.U. Forced vital capacity as a primary end point in idiopathic pulmonary fibrosis treatment trials: Making a silk purse from a sow’ s ear. BMJ J. Thorax 2013, 68, 309–310. [Google Scholar] [CrossRef] [Green Version]
- Yu, X.; Li, X.; Wang, L.; Liu, R.; Xie, Y.; Li, S.; Li, J. Pulmonary rehabilitation for exercise tolerance and quality of life in IPF patients: A systematic review and meta-analysis. BioMed Res. Int. 2019, 2019, 8498603. [Google Scholar] [CrossRef] [Green Version]
- Holland, A.E.; Spruit, M.A.; Troosters, T.; Puhan, M.A.; Pepin, V.; Saey, D.; McCormack, M.C.; Carlin, B.W.; Sciurba, F.C.; Pitta, F.; et al. An official European Respiratory Society/American Thoracic Society technical standard: Field walking tests in chronic respiratory disease. Eur. Respir. J. 2014, 44, 1428–1446. [Google Scholar] [CrossRef] [PubMed]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef]
- Jones, P.W.; Quirk, F.H.; Baveystock, C.M.; Littlejohns, P. A self-complete measure of health status for chronic airflow limitation. Am. Rev. Respir. Dis. 1992, 145, 1321–1327. [Google Scholar] [CrossRef]
- Jones, P.W. Quality of life measurement for patients with diseases of the airways. Thorax 1991, 46, 676. [Google Scholar] [CrossRef] [Green Version]
- Jones, P.W.; Quirk, F.H.; Baveystock, C.M. The St George’ s Respiratory Questionnaire. Respir. Med. 1991, 85, 25–31. [Google Scholar] [CrossRef]
- Ferrer, M.; Villasante, C.; Alonso, J.; Sobradillo, V.; Gabriel, R.; Vilagut, G.; Masa, J.F.; Viejo, J.L.; Jimenez-Ruiz, C.A.; Miravitlles, M. Interpretation of quality of life scores from the St George’ s Respiratory Questionnaire. Eur. Respir. J. 2002, 19, 405–413. [Google Scholar] [CrossRef] [PubMed]
- Mahler, D.A.; Wells, C.K. Evaluation of clinical methods for rating dyspnea. Chest 1988, 93, 580–586. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bestall, J.C.; Paul, E.A.; Garrod, R.; Garnham, R.; Jones, P.W.; Wedzicha, J.A. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax 1999, 54, 581–586. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andrade, C. Mean difference, standardized mean difference (SMD), and their use in meta-analysis: As simple as it gets. J. Clin. Psychiatry 2020, 81. [Google Scholar] [CrossRef]
- Cohen, J. Statistical power analysis for the behavioral sciences. In Statistical Power Analysis for the Behavioral Sciences; Academic Press: Cambridge, MA, USA, 2013. [Google Scholar]
- Follmann, D.; Elliott, P.; Suh, I.L.; Cutler, J. Variance imputation for overviews of clinical trials with continuous response. J. Clin. Epidemiol. 1992, 45, 769–773. [Google Scholar] [CrossRef]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.; Rothstein, H.R. Introduction to Meta-Analysis; John Wiley & Sons: Hoboken, NJ, USA, 2021. [Google Scholar]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.M.; Nieman, D.C.; Swain, D.P. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef]
- Kemmler, W.; Von Stengel, S. Exercise frequency, health risk factors, and diseases of the elderly. Arch. Phys. Med. Rehabil. 2013, 94, 2046–2053. [Google Scholar] [CrossRef]
- Sial, S.; Coggan, A.R.; Carroll, R.; Goodwin, J.; Klein, S. Fat and carbohydrate metabolism during exercise in elderly and young subjects. Am. J. Physiol. Endocrinol. Metab. 1996, 271, E983–E989. [Google Scholar] [CrossRef] [PubMed]
- Greig, C.A.; Young, A.; Skelton, D.A.; Pippet, E.; Butler, F.M.M.; Mahmud, S.M. Exercise studies with elderly volunteers. Age Ageing 1994, 23, 185–189. [Google Scholar] [CrossRef]
- Ohta, T.; Nagashima, J.; Sasai, H.; Ishii, N. Relationship of cardiorespiratory fitness and body mass index with the incidence of dyslipidemia among Japanese women: A cohort study. Int. J. Environ. Res. Public Health 2019, 16, 4647. [Google Scholar] [CrossRef] [Green Version]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [Green Version]
- McElroy, P.A.; Janicki, J.S.; Weber, K.T. Cardiopulmonary exercise testing in congestive heart failure. Am. J. Cardiol. 1988, 62, 35A–40A. [Google Scholar] [CrossRef]
- Galloza, J.; Castillo, B.; Micheo, W. Benefits of Exercise in the Older Population. Phys. Med. Rehabil. Clin. N. Am. 2017, 28, 659–669. [Google Scholar] [CrossRef]
- Vagetti, G.C.; Barbosa, V.C.; Moreira, N.B.; Oliveira, V.D.; Mazzardo, O.; Campos, W.D. Association between physical activity and quality of life in the elderly: A systematic review, 2000–2012. Braz. J. Psychiatr. 2014, 36, 76–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nelson, M.E.; Rejeski, W.J.; Blair, S.N.; Duncan, P.W.; Judge, J.O.; King, A.C.; Macera, C.A.; Castaneda-Sceppa, C. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Circulation 2007, 116, 1094. [Google Scholar] [CrossRef] [Green Version]
- Department of Healtj and Human Services. Physical Activity Guidelines Advisory Committee report, 2008. To the Secretary of Health and Human Services. Part A: Ex-ecutive summary. Nutr. Rev. 2009, 67, 114–120. [Google Scholar]
- Roman, M.A.; Rossiter, H.B.; Casaburi, R. Exercise, ageing and the lung. Eur. Respir. J. 2016, 48, 1471–1486. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nathan, S.D.; Yang, M.; Morgenthien, E.A.; Stauffer, J.L. FVC variability in patients with idiopathic pulmonary fibrosis and role of 6-min walk test to predict further change. Eur. Respir. J. 2020, 55, 1902151. [Google Scholar] [CrossRef] [PubMed]
- LeVert, S. The Lungs; Marshall Cavendish: New York, NY, USA, 2002. [Google Scholar]
- Babb, T.G.; Long, K.A.; Rodarte, J.R. The relationship between maximal expiratory flow and increases of maximal exercise capacity with exercise training. Am. J. Respir. Crit. Care Med. 1997, 156, 116–121. [Google Scholar] [CrossRef]
- Raghu, G.; Collard, H.R.; Egan, J.J.; Martinez, F.J.; Behr, J.; Brown, K.K.; Colby, T.V.; Cordier, J.F.; Flaherty, K.R.; Lasky, J.A.; et al. An official ATS/ERS/JRS/ALAT statement: Idiopathic pulmonary fibrosis: Evidence-based guidelines for diagnosis and management. Am. J. Respir. Crit. Care Med. 2011, 183, 788–824. [Google Scholar] [CrossRef]
- Paterniti, M.O.; Bi, Y.; Rekić, D.; Wang, Y.; Karimi-Shah, B.A.; Chowdhury, B.A. Acute exacerbation and decline in forced vital capacity are associated with increased mortality in idiopathic pulmonary fibrosis. Ann. Am. Thorac. Soc. 2017, 14, 1395–1402. [Google Scholar] [CrossRef] [PubMed]
- Durheim, M.T.; Collard, H.R.; Roberts, R.S.; Brown, K.K.; Flaherty, K.R.; King, T.E., Jr.; Palmer, S.M.; Raghu, G.; Snyder, L.D.; Anstrom, K.J.; et al. Association of hospital admission and forced vital capacity endpoints with survival in patients with idiopathic pulmonary fibrosis: Analysis of a pooled cohort from three clinical trials. Lancet Respir. Med. 2015, 3, 388–396. [Google Scholar] [CrossRef] [Green Version]
- Enright, P. Office-based DLCO tests help pulmonologists to make important clinical decisions. Respir. Investig. 2016, 54, 305–311. [Google Scholar] [CrossRef]
- Yao, W.; Han, X.; Wang, G. Effect of lung function factors on diffusing capacity in patients with chronic bronchitis and emphysema. Mod. Rehabil. 2001, 403, 104–105. [Google Scholar]
- Zach, M.S.; Purrer, B.; Oberwaldner, B. Effect of swimming on forced expiration and sputum clearance in cystic fibrosis. Lancet 1981, 318, 1201–1203. [Google Scholar] [CrossRef]
- Farber, H.W.; Miller, D.P.; McGoon, M.D.; Frost, A.E.; Benton, W.W.; Benza, R.L. Predicting outcomes in pulmonary arterial hypertension based on the 6-minute walk distance. J. Heart Lung Transplant. 2015, 34, 362–368. [Google Scholar] [CrossRef] [Green Version]
- Swigris, J.J.; Brown, K.K.; Make, B.J.; Wamboldt, F.S. Pulmonary rehabilitation in idiopathic pulmonary fibrosis: A call for continued investigation. Respir. Med. 2008, 102, 1675–1680. [Google Scholar] [CrossRef] [Green Version]
- Swigris, J.J.; Kuschner, W.G.; Jacobs, S.S.; Wilson, S.R.; Gould, M.K. Health-related quality of life in patients with idiopathic pulmonary fibrosis: A systematic review. Thorax 2005, 60, 588–594. [Google Scholar] [CrossRef] [Green Version]
- King, T.E., Jr.; Bradford, W.Z.; Castro-Bernardini, S.; Fagan, E.A.; Glaspole, I.; Glassberg, M.K.; Gorina, E.; Hopkins, P.M.; Kardatzke, D.; Lancaster, L.; et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. New Engl. J. Med. 2014, 370, 2083–2092. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puetz, T.W. Physical activity and feelings of energy and fatigue. Sports Med. 2006, 36, 767–780. [Google Scholar] [CrossRef]
- Bartholomew, J.B.; Morrison, D.; Ciccolo, J.T. Effects of acute exercise on mood and well-being in patients with major depressive disorder. Med. Sci. Sports Exerc. 2005, 37, 2032. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwai-Sang, Y.M. Tai Chi exercise and the improvement of health and well-being in older adults. Med. Sport Sci. 2008, 52, 155–165. [Google Scholar]
- Larson, E.B.; Wang, L.I.; Bowen, J.D.; McCormick, W.C.; Teri, L.; Crane, P.; Kukull, W. Exercise is associated with reduced risk for incident dementia among persons 65 years of age and older. Ann. Int. Med. 2006, 144, 73–81. [Google Scholar] [CrossRef]
- Paterson, D.H.; Warburton, D.E.R. Physical activity and functional limitations in older adults: A systematic review related to Canada’ s Physical Activity Guidelines. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 1–22. [Google Scholar] [CrossRef] [Green Version]
- Weuve, J.; Kang, J.H.; Manson, J.E.; Breteler, M.M.; Ware, J.H.; Grodstein, F. Physical activity, including walking, and cognitive function in older women. JAMA 2004, 292, 1454–1461. [Google Scholar] [CrossRef] [Green Version]
- Yaffe, K.; Fiocco, A.J.; Lindquist, K.; Vittinghoff, E.; Simonsick, E.M.; Newman, A.B.; Satterfield, S.; Rosano, C.; Rubin, S.M.; Ayonayon, H.N.; et al. Predictors of maintaining cognitive function in older adults: The Health ABC study. Neurology 2009, 72, 2029–2035. [Google Scholar] [CrossRef] [Green Version]







| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Score | Quality | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Vainshelboim, 2014 | Yes | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | good |
| Vainshelboim, 2015 | Yes | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | good |
| Vainshelboim, 2016 | Yes | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | good |
| Vainshelboim, 2017 | Yes | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | good |
| Perez-Bogerd, 2018 | Yes | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | good |
| Nishiyama, 2008 | Yes | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | good |
| Yuen, 2019 | Yes | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 5 | fair |
| Jackson, 2014 | Yes | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | good |
| Gaunaurd 2014 | Yes | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | good |
| Dowman 2017 | Yes | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 8 | good |
| Holland, 2008 | Yes | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 8 | good |
| Arizono, 2014 | Yes | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 | fair |
| Wapenaar, 2020 | Yes | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 | good |
| Study | Country Study Design | Sample Size (n) | Age (Year) | Male (%) | BMI (kg/m2) | Frequency (/Week) | Intensity | Duration (Months) | Type | Outcomes |
|---|---|---|---|---|---|---|---|---|---|---|
| Vainshelboim, 2014 [16] | Israel RCT | OG: 15 CG: 17 | OG: 68.8 (6) CG: 66 (9) | OG: 67% CG: 65% | OG: 28.3 (3.5) CG: 28.8 (3.5) | 60 min × 2 | Light | 3 | OG: A–R–F–B CG: RC | ①②③ ④⑤⑥ |
| Vainshelboim, 2015 [26] | Israel RCT | OG: 14 CG: 14 | OG: 68.8 (6) CG: 66 (9) | OG: 67% CG: 65% | OG: 28.3 (3.5) CG: 28.8 (3.5) | 60 min × 2 | Light | 11 | OG: A–R–F–B CG: RC | ①②③ ④⑤⑥ |
| Vainshelboim, 2016 [19] | Israel RCT | OG: 15 CG: 17 | OG: 68.8 (6) CG: 66 (9) | OG: 67% CG: 65% | OG: 28.3 (3.5) CG: 28.8 (3.5) | 60 min × 2 | Light | 3, 11 | OG: A–R–F–B CG: RC | ①②③ ④⑥⑦ |
| Vainshelboim, 2017 [27] | Israel RCT | OG: 15 CG: 17 | OG: 68.8 (6) CG: 66 (9) | OG: 67% CG: 65% | OG: 28.3 (3.5) CG: 28.8 (3.5) | 60 min × 2 | Light | 3 | OG: A–R–F–B CG: RC | ②⑥⑦ |
| Perez-Bogerd, 2018 [30] | Belgium RCT | OG: 30 CG: 30 | OG: 64 (13) CG: 64 (8) | OG: 73% CG: 50% | OG: 28 (4) CG: 26 (5) | 3 (1–3 months) 2 (4–12 months) | Moderate | 3, 6, 12 | OG: A–R CG: RC | ①④⑥ |
| Nishiyama, 2008 [28] | Japan RCT | OG: 13 CG: 15 | OG: 68.1 (8.9) CG: 64.5 (9.1) | OG: 92% CG: 60% | OG: 23 (3.8) CG: 22.9 (2.8) | 2 | Moderate | 2.5 | OG: A–R CG: RC | ①⑥ |
| Yuen 2019 [33] | America RCT | OG: 10 CG: 10 | OG: 67.4 (7.4) CG: 72.2 (8.4) | OG: 50% CG: 80% | OG: 28.0 (4.6) CG: 28.4 (4.3) | 30 min × 3 | Light | 3 | OG: A–R CG: RC | ①⑥ |
| Jackson, 2014 [29] | America RCT | OG: 11 CG: 10 | OG: 71 (6) CG: 66 (7) | NC | NC | 120 min × 2 | Moderate | 3 | OG: A–F CG: RC | ① |
| Gaunaurd, 2014 [2] | America RCT | OG: 11 CG: 10 | OG: 71 (6) CG: 66 (7) | NC | NC | 90 min × 2 | Moderate | 3 | OG: A–R CG: RC | ⑥ |
| Dowman, 2017 [17] | Australia RCT | OG: 32 CG: 29 | OG: 70 (10) CG: 73 (9) | OG: 66% CG: 69% | NC | 2 | Moderate | 2.25 | OG: A–R CG: RC | ① |
| Holland, 2008 [24] | Australia RCT | OG: 30 CG: 27 | OG: 70 (8) CG: 67 (13) | NC | NC | 2 | Moderate | 2.25, 6.5 | OG: A–R CG: RC | ①⑦ |
| Arizono, 2014 [32] | Japan Pre-post | OG: 24 CG: 24 | OG: 69 (7) CG: 69 (6) | OG: 67% CG: 67% | NC | 90 min × 2 | Moderate | 2.5 | OG: A–R CG: RC | ①④ |
| Wapenaar, 2020 [31] | Netherlands Pre-post | OG: 10 CG: 10 | OG: 71 (7) CG: 71 (7) | OG: 80% CG: 80% | NC | 60 min × 6 | Light | 2 | OG: A–R CG: RC | ①⑥ |
| Group Standard | Study Quantity | Sample Size (n) | Mean Difference (95% CI) | Cohen’s d | Z | I2 | pa | pb | |
|---|---|---|---|---|---|---|---|---|---|
| 6MWD | 0.77 | ||||||||
| Frequency | >60 min × 2 | 4 | OG:75/CG:74 | 15.09 (2.74, 27.43) | 0.62 | 2.40 | 79% | 0.02 | 0.0001 |
| ≤60 min × 2 | 11 | OG:234/CG:233 | 45.32 (35.80, 54.85) | 0.82 | 9.33 | 56% | <0.00001 | ||
| Intensity | Light | 6 | OG:79/CG:85 | 19.64 (7.17, 32.11) | 0.77 | 3.09 | 79% | 0.002 | 0.004 |
| Moderate | 9 | OG:230/CG:222 | 42.34 (32.87, 51.81) | 0.78 | 8.76 | 59% | <0.00001 | ||
| Type | A–R | 10 | OG:239/CG:232 | 30.71 (22.72, 38.71) | 0.77 | 7.53 | 78% | <0.00001 | 0.0008 |
| A–F | 1 | OG:11/CG:10 | 9.10 (−48.73, 66.93) | 0.13 | 0.31 | 0.76 | |||
| A–R–F–B | 4 | OG:74/CG:82 | 70.38 (45.66, 95.10) | 0.92 | 5.58 | 0% | <0.00001 | ||
| Duration | >3 months | 5 | OG:119/CG:118 | 48.07 (32.98, 63.17) | 0.77 | 6.24 | 74% | <0.00001 | 0.04 |
| ≤3 months | 10 | OG:190/CG:189 | 29.37 (20.67, 38.08) | 0.78 | 6.61 | 72% | <0.00001 | ||
| Age | >70 | 4 | OG:58/CG:51 | 9.54 (−3.19, 22.28) | 0.45 | 1.47 | 51% | 0.14 | <0.00001 |
| ≤70 | 11 | OG:246/CG:248 | 47.26 (37.90, 56.62) | 0.86 | 9.90 | 57% | <0.00001 | ||
| BMI | >25 | 8 | OG:159/CG:165 | 68.01 (54.41, 81.60) | 1.03 | 9.8 | 0% | <0.00001 | 0.62 |
| ≤25 | 1 | OG:13/CG:15 | 46.00 (−40.28, 132.28) | 0.38 | 1.04 | 0.3 | |||
| Peak VO2 | 0.45 | ||||||||
| Duration | >3 months | 2 | OG:29/CG:31 | 0.12 (−1.01, 1.25) | 0.74 | 0.2 | 0 | 0.84 | 0.03 |
| ≤3 months | 3 | OG:45/CG:51 | 1.73 (0.87, 2.60) | 0.05 | 3.92 | 74% | <0.00001 | ||
| FVC% pred | 0.42 | ||||||||
| Duration | >3 months | 1 | OG:15/CG:17 | 1.00 (−5.83, 7.83) | 0.11 | 0.29 | 0.77 | 0.35 | |
| ≤3 months | 3 | OG:94/CG:98 | 4.65 (1.28, 8.02) | 0.51 | 2.70 | 0% | 0.007 | ||
| DLCO% pred | 0.16 | ||||||||
| Frequency | >60 min × 2 | 2 | OG:54/CG:54 | 1.68 (−2.80, 6.15) | 0.15 | 0.73 | 0% | 0.46 | 0.93 |
| ≤60 min × 2 | 6 | OG:119/CG:125 | 1.92 (−0.65, 4.49) | 0.17 | 1.46 | 0% | 0.14 | ||
| Intensity | Light | 4 | OG:59/CG:65 | 1.66 (−1.42, 4.75) | 0.15 | 1.06 | 0% | 0.29 | 0.86 |
| Moderate | 4 | OG:114/CG:114 | 2.07 (−1.15, 5.30) | 0.17 | 1.26 | 0% | 0.21 | ||
| Type | A–R | 4 | OG:114/CG:114 | 2.07 (−1.15, 5.30) | 0.17 | 1.26 | 0% | 0.21 | 0.86 |
| A–R–F–B | 4 | OG:59/CG:65 | 1.66 (−1.42, 4.75) | 0.15 | 1.06 | 0% | 0.29 | ||
| Duration | >3 months | 3 | OG:75/CG:77 | 1.27 (−2.94, 5.47) | 0.11 | 0.59 | 0% | 0.55 | 0.84 |
| ≤3 months | 5 | OG:98/CG:102 | 1.78 (−0.86, 4.41) | 0.18 | 1.32 | 0% | 0.19 | ||
| TLC% pred | 0.02 | ||||||||
| Duration | >3 months | 1 | OG:14/CG:14 | 0.00 (−6.69, 6.69) | 0.00 | 0.00 | 1.00 | 0.90 | |
| ≤3 months | 1 | OG:15/CG:17 | 2.60 (−37.18, 42.28) | 0.04 | 0.13 | 0.90 | |||
| SGRQ | 0.89 | ||||||||
| Frequency | >60 min × 2 | 2 | OG:40/CG:40 | −7.81 (−12.18, −3.44) | 0.65 | 3.50 | 0% | 0.0005 | 0.64 |
| ≤60 min × 2 | 10 | OG:168/CG:177 | −8.94 (−10.63, −7.25) | 0.95 | 10.36 | 31% | <0.00001 | ||
| Intensity | Light | 7 | OG:94/CG:102 | −8.34 (−10.07, −6.61) | 1.15 | 9.43 | 28% | <0.00001 | 0.22 |
| Moderate | 5 | OG:114/CG:115 | −10.96 (−14.76, −7.16) | 0.71 | 5.65 | 0% | <0.00001 | ||
| Type | A–R | 7 | OG:134/CG:135 | −8.75 (−11.70, −5.79) | 0.67 | 5.80 | 43% | <0.00001 | 0.97 |
| A–R–F–B | 5 | OG:74/CG:82 | −8.81 (−10.67, −6.94) | 1.35 | 9.26 | 0% | <0.00001 | ||
| Duration | >3 months | 4 | OG:104/CG:108 | −9.65 (−12.27, −7.02) | 1.00 | 7.2 | 0% | <0.00001 | 0.43 |
| ≤3 months | 8 | OG:104/CG:109 | −8.31 (−10.28, −6.34) | 0.82 | 8.26 | 28% | <0.00001 | ||
| Age | >70 | 3 | OG:31/CG:30 | −6.72 (−11.20, −2.24) | 0.63 | 2.94 | 72% | 0.003 | 0.33 |
| ≤70 | 9 | OG:177/CG:187 | −9.09 (−10.77, −7.40) | 0.94 | 10.57 | 0% | <0.00001 | ||
| BMI | >25 | 9 | OG:174/CG:182 | −8.73 (−10.40, −7.06) | 1.00 | 10.27 | 27% | <0.00001 | 0.71 |
| ≤25 | 1 | OG:13/CG:15 | −6.00 (−20.34, 8.34) | 0.30 | 0.82 | 0.41 | |||
| mMRC | 0.64 | ||||||||
| Intensity | Light | 3 | OG:45/CG:54 | −0.91 (−1.21, −0.60) | 1.11 | 5.73 | 30% | <0.00001 | 0.004 |
| Moderate | 2 | OG:60/CG:54 | −0.26 (−0.56, 0.04) | 0.30 | 1.68 | 0% | 0.09 | ||
| Type | A–R | 2 | OG:60/CG:54 | −0.26 (−0.56, 0.04) | 0.30 | 1.68 | 0% | 0.09 | 0.004 |
| A–R–F–B | 3 | OG:45/CG:54 | −0.91 (−1.21, −0.60) | 1.11 | 5.73 | 30% | <0.00001 | ||
| Duration | >3 months | 2 | OG:45/CG:44 | −0.25 (−0.60, 0.10) | 0.29 | 1.42 | 16% | 0.16 | 0.02 |
| ≤3 months | 3 | OG:60/CG:61 | −0.78 (−1.06, −0.50) | 0.93 | 5.52 | 65% | <0.00001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, X.; Yu, R.; Wang, P.; Wang, A.; Huang, H. Effects of Exercise Training on Cardiopulmonary Function and Quality of Life in Elderly Patients with Pulmonary Fibrosis: A Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 7643. https://doi.org/10.3390/ijerph18147643
Li X, Yu R, Wang P, Wang A, Huang H. Effects of Exercise Training on Cardiopulmonary Function and Quality of Life in Elderly Patients with Pulmonary Fibrosis: A Meta-Analysis. International Journal of Environmental Research and Public Health. 2021; 18(14):7643. https://doi.org/10.3390/ijerph18147643
Chicago/Turabian StyleLi, Xiaohan, Rongfang Yu, Ping Wang, Aiwen Wang, and Huiming Huang. 2021. "Effects of Exercise Training on Cardiopulmonary Function and Quality of Life in Elderly Patients with Pulmonary Fibrosis: A Meta-Analysis" International Journal of Environmental Research and Public Health 18, no. 14: 7643. https://doi.org/10.3390/ijerph18147643
APA StyleLi, X., Yu, R., Wang, P., Wang, A., & Huang, H. (2021). Effects of Exercise Training on Cardiopulmonary Function and Quality of Life in Elderly Patients with Pulmonary Fibrosis: A Meta-Analysis. International Journal of Environmental Research and Public Health, 18(14), 7643. https://doi.org/10.3390/ijerph18147643






