Effectiveness of Community Nutrition-Specific Interventions on Improving Malnutrition of Children under 5 Years of Age in the Eastern Mediterranean Region: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
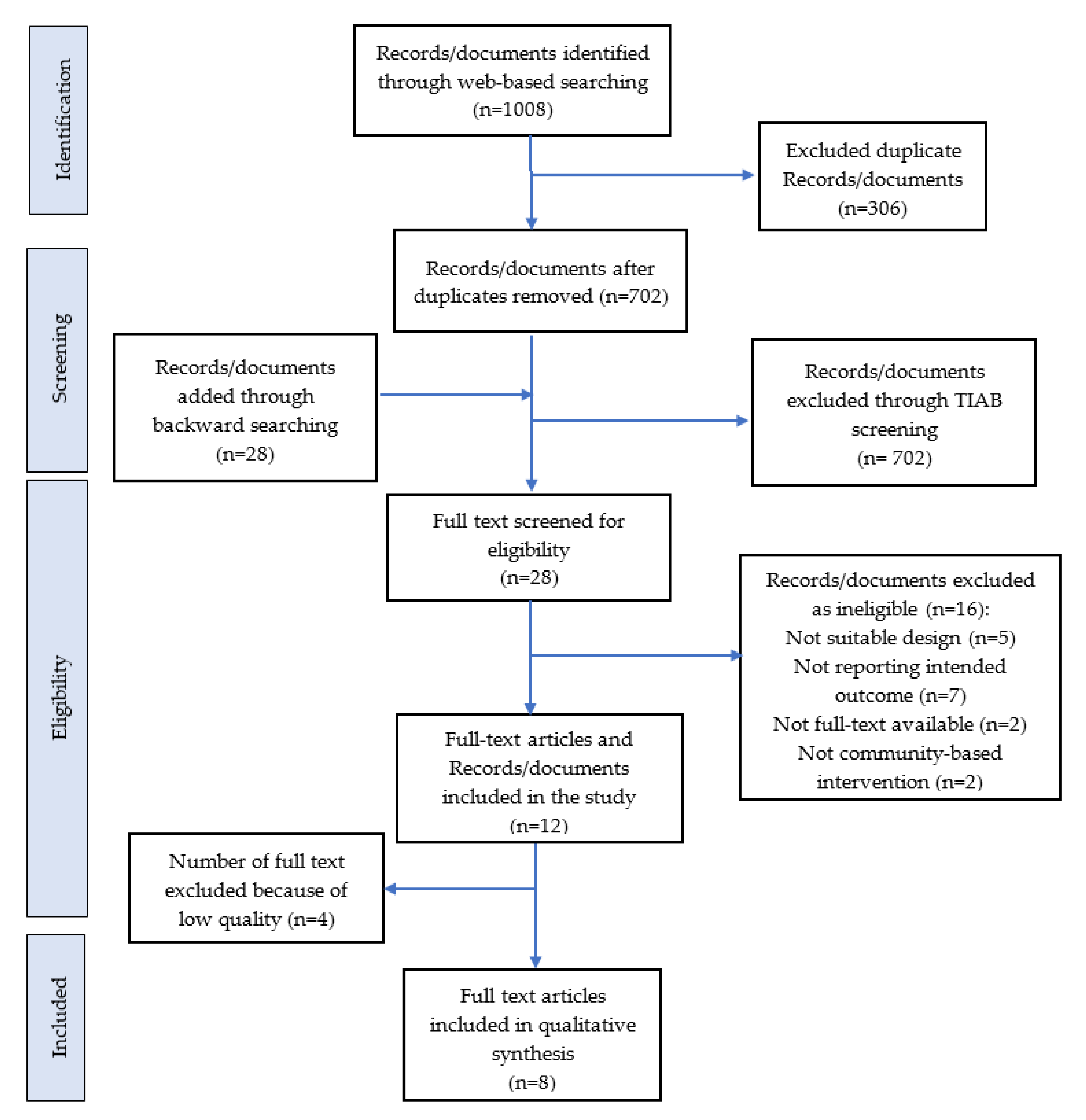
2. Materials and Methods
2.1. Search Strategy
2.2. Study Eligibility Criteria
2.3. Article Screening and Data Extraction
2.4. Risk of Bias Assessment
2.5. Data Synthesis and Meta-Analysis
2.6. Meta-Regression
2.7. Statistical Analysis
3. Results
3.1. Descriptive Systematic Literature Review
3.1.1. Nutrition Education/Nutrition Counselling
3.1.2. Food Distribution through Different Modalities
3.2. Meta-Analysis
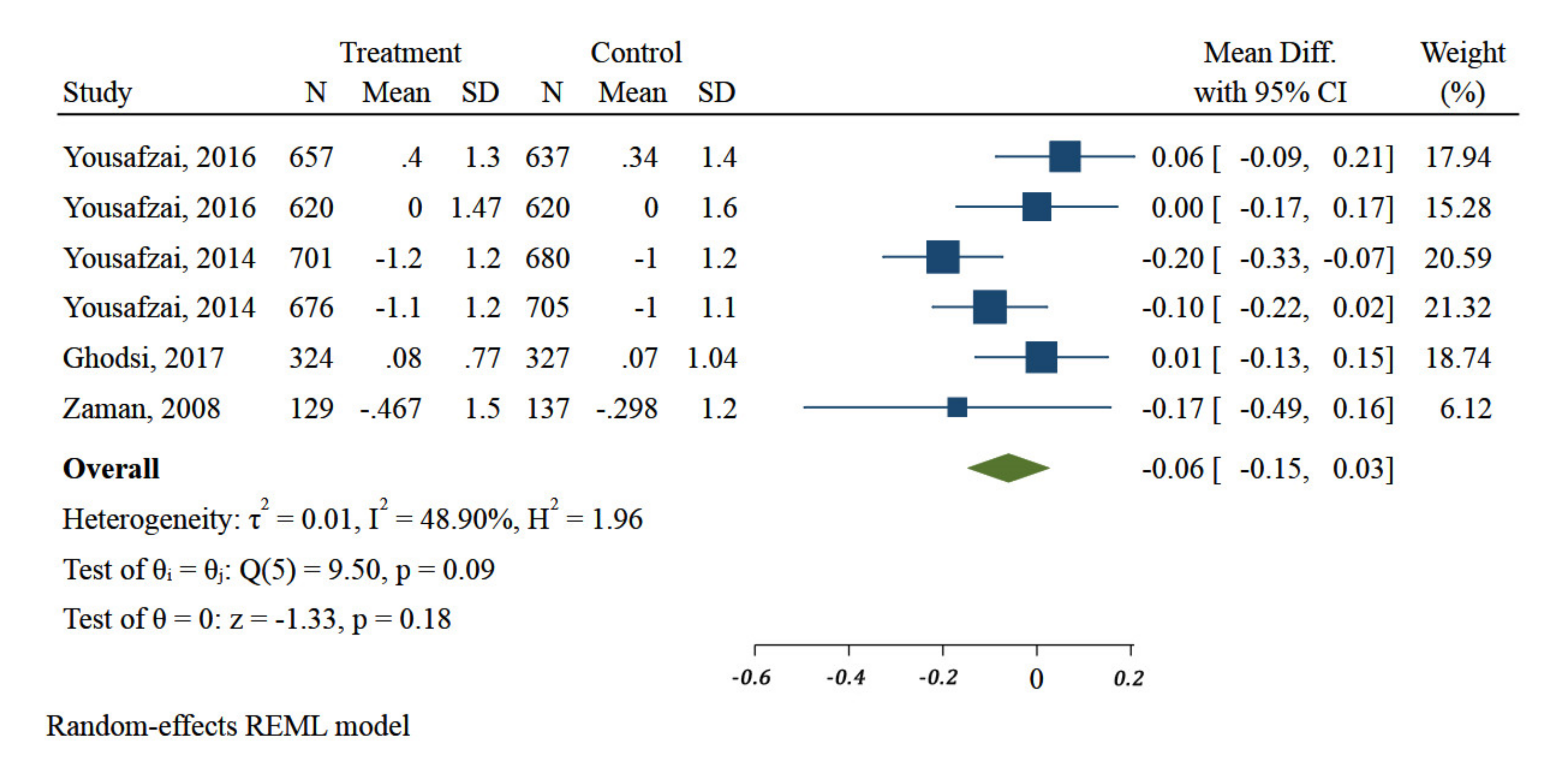
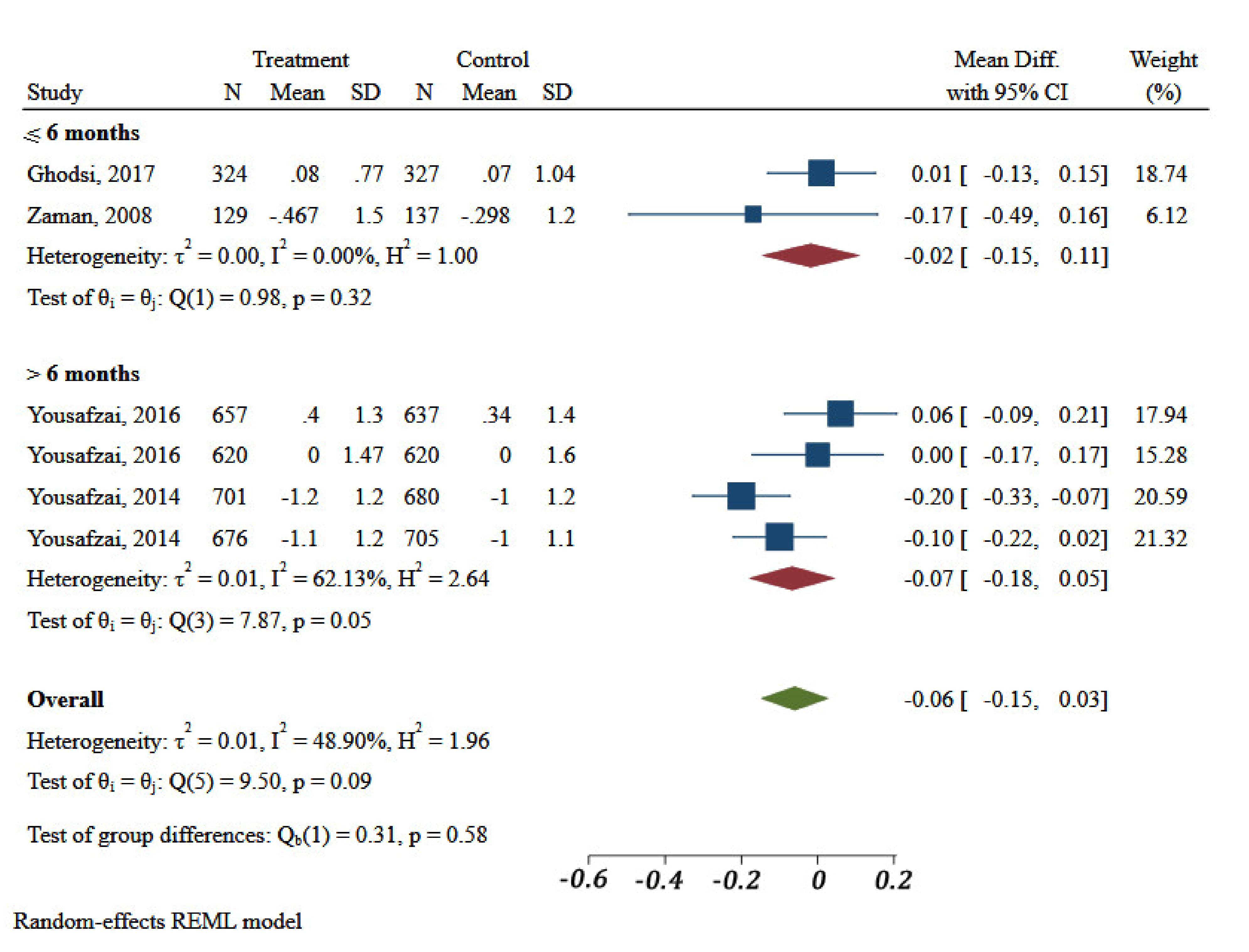
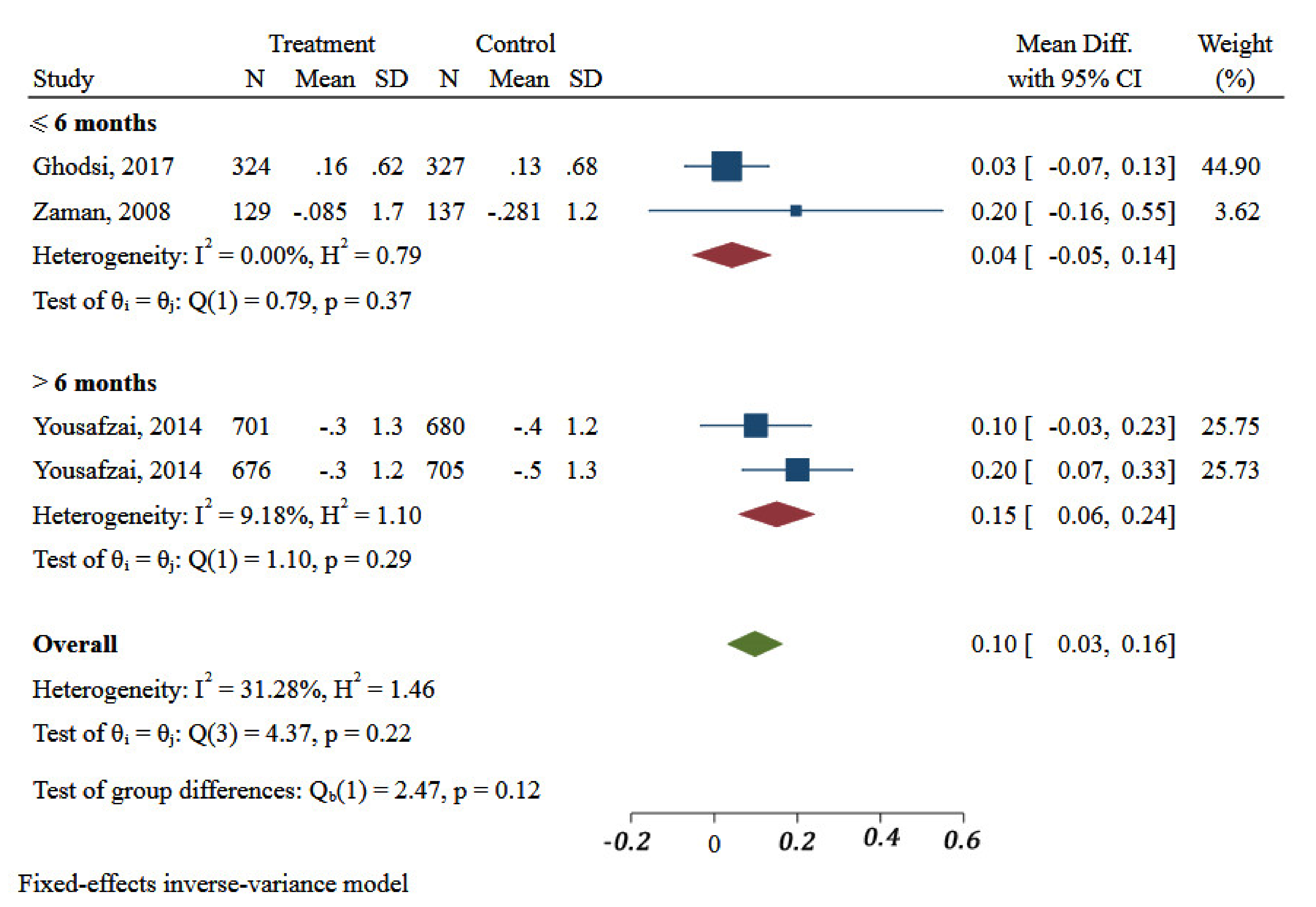
3.2.1. Impact of Different Nutrition-Specific Interventions on HAZ
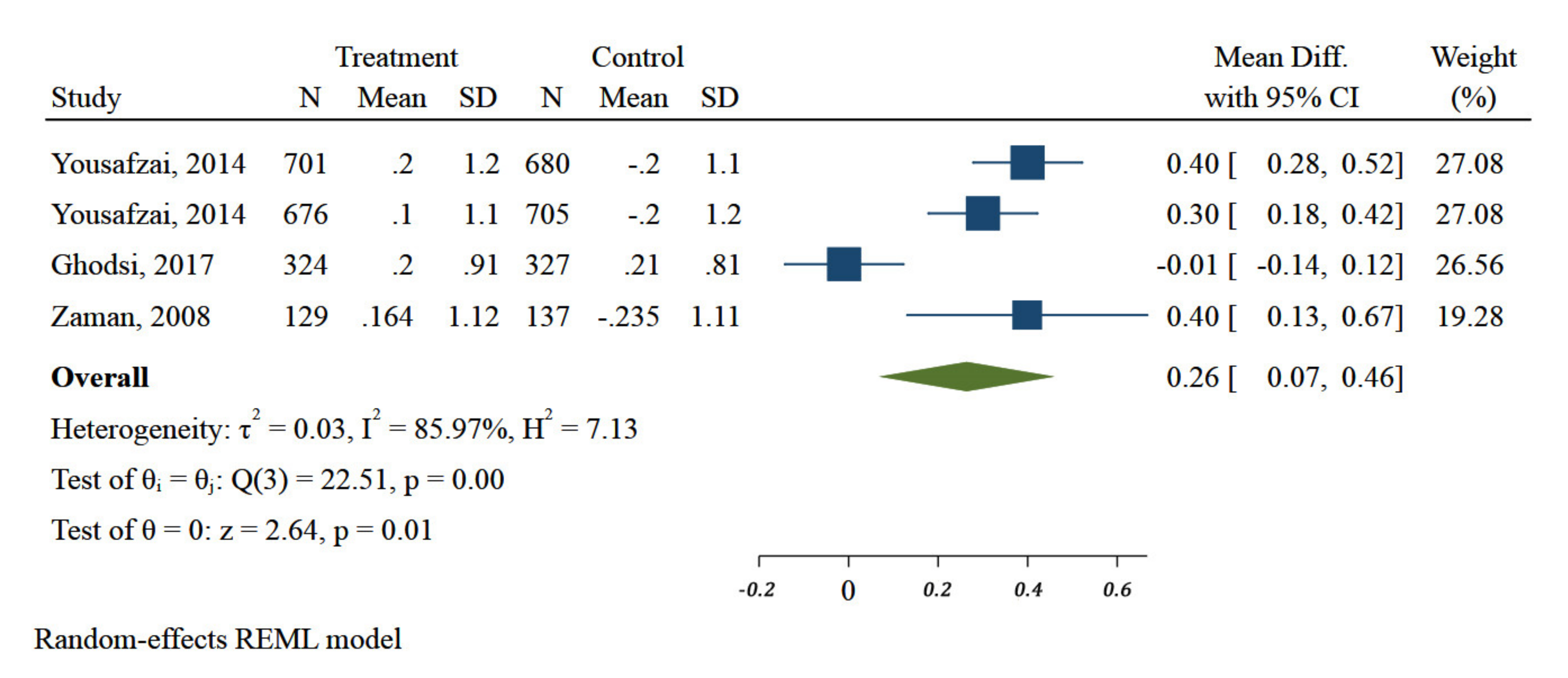
3.2.2. Impact of Different Nutrition-Specific Interventions on WAZ
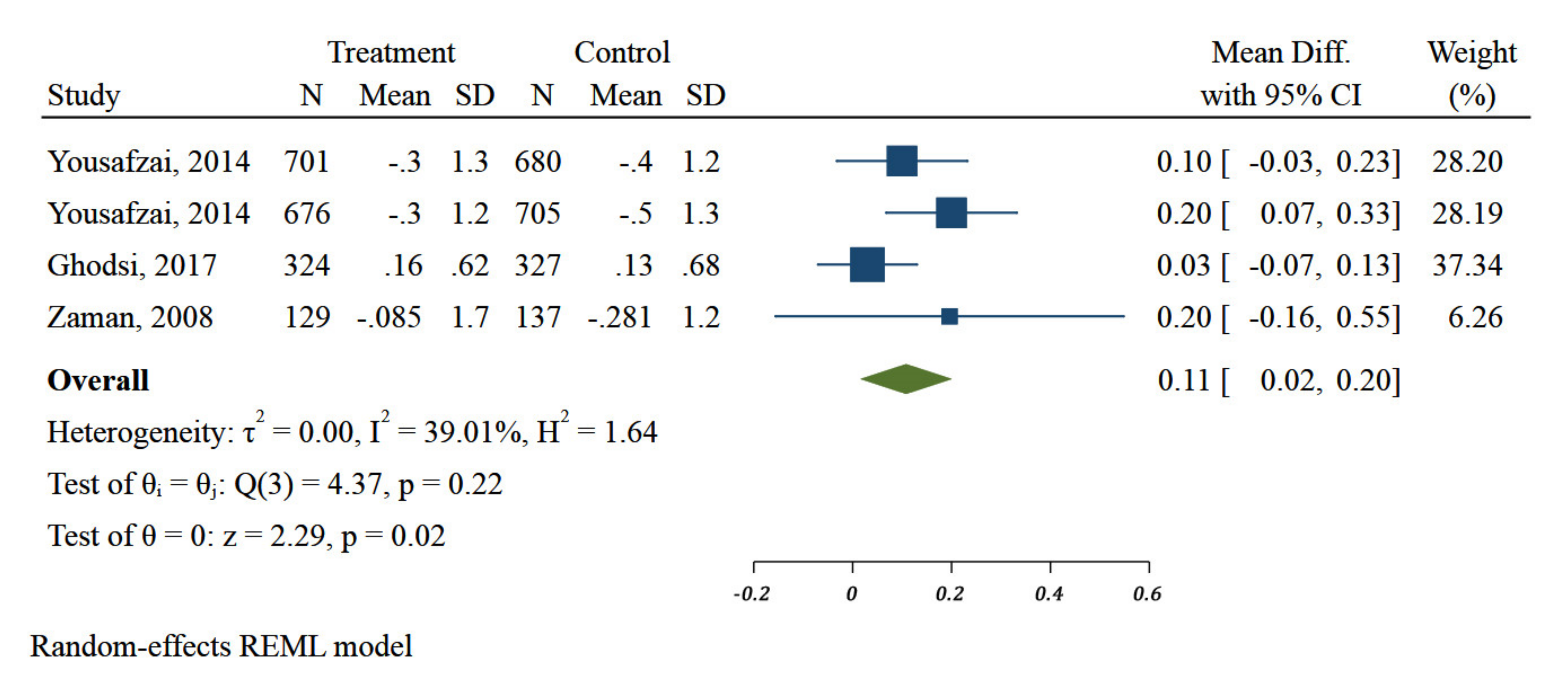
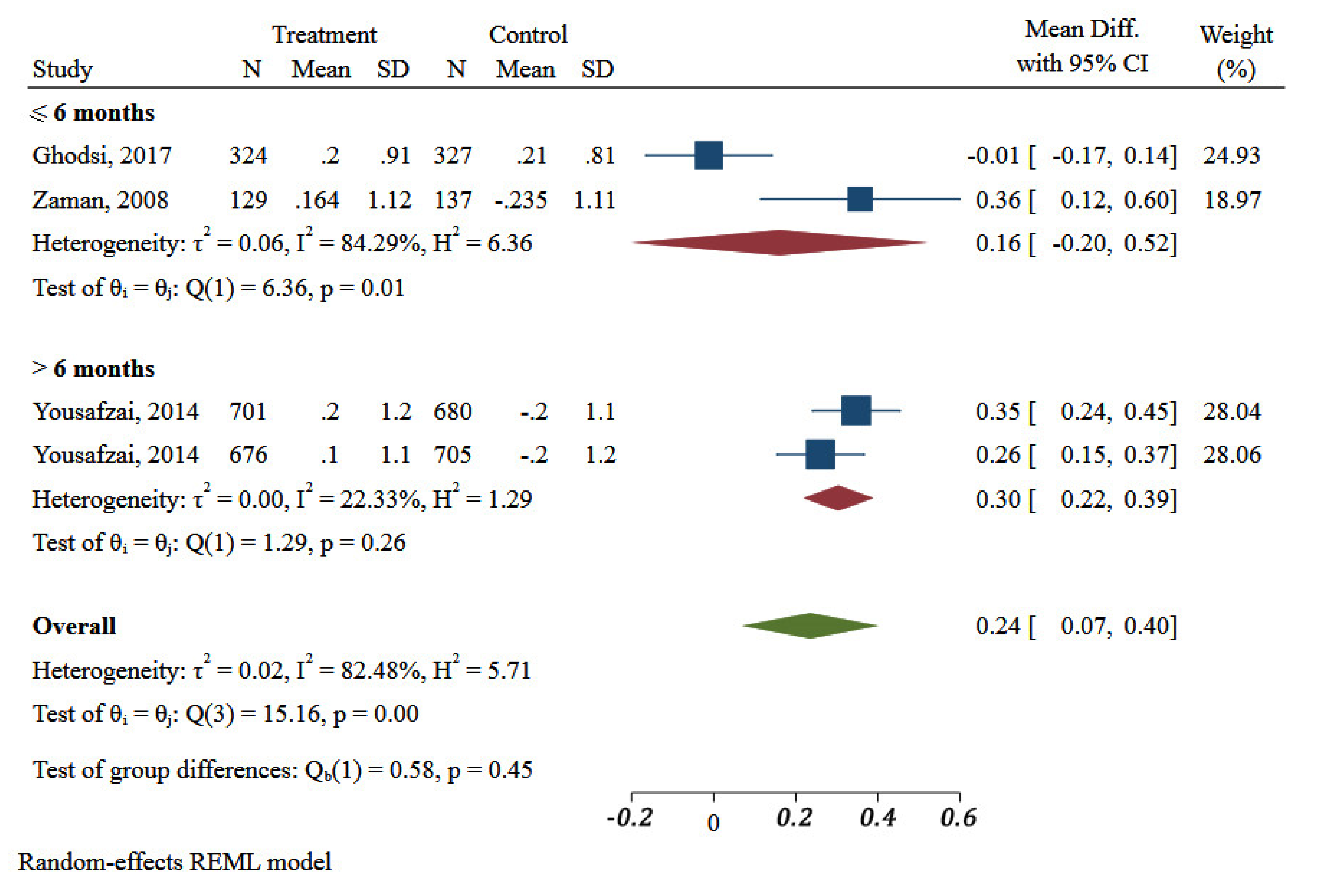
3.2.3. Impact of Different Nutrition-Specific Interventions on WHZ
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ssentongo, P.; Ssentongo, A.E.; Ba, D.M.; Ericson, J.E.; Na, M.; Gao, X.; Fronterre, C.; Chinchilli, V.M.; Schiff, S.J. Global, regional and national epidemiology and prevalence of child stunting, wasting and underweight in low- and middle-income countries, 2006–2018. Sci. Rep. 2021, 11, 1–12. [Google Scholar] [CrossRef]
- Ruel, M.T.; Hoddinott, J. Investing in Early Childhood Nutrition; IFPRI Policy Brief; International Food Policy Research Institute: Washington, DC, USA, 2008; No 8. [Google Scholar]
- United Nations. SDG Indicators: Revised List of Global Sustainable Development Goal Indicators; United Nations: New York, NY, USA, 2017. [Google Scholar]
- Lentz, E.C.; Barrett, C. The economics and nutritional impacts of food assistance policies and programs. Food Policy 2013, 42, 151–163. [Google Scholar] [CrossRef]
- Leroy, J.L.; Olney, D.; Ruel, M. Tubaramure, a Food-Assisted Integrated Health and Nutrition Program in Burundi, Increases Maternal and Child Hemoglobin Concentrations and Reduces Anemia: A Theory-Based Cluster-Randomized Controlled Intervention Trial. J. Nutr. 2016, 146, 1601–1608. [Google Scholar] [CrossRef] [PubMed]
- Alderman, H.; Behrman, J.R.; Glewwe, P.; Fernald, L.; Walker, S. Evidence of impact of interventions on growth and devel-opment during early and middle childhood. Child Adolesc. Health Dev. 2017, 8, 1790. [Google Scholar]
- Black, R.e.; Victora, C.g.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Ruel, M.T.; Alderman, H. Maternal and Child Nutrition Study Group Nutrition-sensitive interventions and programmes: How can they help to accelerate progress in improving maternal and child nutrition. Lancet 2013, 382, 536–551. [Google Scholar] [CrossRef]
- Bhutta, Z.A.; Das, J.K.; Rizvi, A.; Gaffey, M.F.; Walker, N.; Horton, S.; Webb, P.; Lartey, A.; Black, R.E. Evidence-based interventions for improvement of maternal and child nutrition: What can be done and at what cost? Lancet 2013, 382, 452–477. [Google Scholar] [CrossRef]
- Haddad, L.; Achadi, E.; Bendech, M.A.; Ahuja, A.; Bhatia, K.; Bhutta, Z.; Blössner, M.; Borghi, E.; Colecraft, E.; de Onis, M.; et al. The Global Nutrition Report 2014: Actions and accountability to accelerate the world’s progress on nutrition. J. Nutr. 2015, 145, 663–671. [Google Scholar] [CrossRef]
- Djazayery, A. Regional overview of maternal and child malnutrition: Trends, interventions and outcomes. EMHJ East. Mediterr. Health J. 2004, 10, 731–736. [Google Scholar]
- Technical Paper. Regional Strategy on Nutrition 2010–2019. Regional Committee for the Eastern Mediterranean. Fifty-Seventh Session. Agenda Item 4 (b) [Internet]. 2010. Available online: http://applications.emro.who.int/docs/EM_RC57_4_en.pdf?ua=1 (accessed on 13 November 2020).
- Nasreddine, L.M.; Kassis, A.N.; Ayoub, J.J.; Naja, F.A.; Hwalla, N.C. Nutritional status and dietary intakes of children amid the nutrition transition: The case of the Eastern Mediterranean Region. Nutr. Res. 2018, 57, 12–27. [Google Scholar] [CrossRef]
- UNICEF. United Nations Children’s Fund. The State of the World’s Children; Oxford University Press (with Additional Calculations): Oxford, UK, 1994. [Google Scholar]
- UNICEF. United Nations Children’s Fund. The State of the World’s Children; Oxford University Press (with Additional Calculations): Oxford, UK, 2004. [Google Scholar]
- UNICEF. United Nations Children’s Fund. The State of the World’s Children; Oxford University Press (with Additional Calculations): Oxford, UK, 2012. [Google Scholar]
- Musaiger, A.O.; Hassan, A.S.; Obeid, O. The Paradox of Nutrition-Related Diseases in the Arab Countries: The Need for Action. Int. J. Environ. Res. Public Health 2011, 8, 3637–3671. [Google Scholar] [CrossRef] [PubMed]
- Galal, O.M. The nutrition transition in Egypt: Obesity, undernutrition and the food consumption context. Public Health Nutr. 2002, 5, 141–148. [Google Scholar] [CrossRef]
- Kelishadi, R.; Amiri, M.; Motlagh, M.E.; Taslimi, M.; Ardalan, G.; Rouzbahani, R.; Poursafa, P. Growth Disorders among 6-Year-Old Iranian Children. Iran. Red Crescent Med. J. 2014, 16, e6761. [Google Scholar] [CrossRef] [PubMed]
- Sibai, A.; Nasreddine, L.; Mokdad, A.H.; Adra, N.; Tabet, M.; Hwalla, N. Nutrition Transition and Cardiovascular Disease Risk Factors in Middle East and North Africa Countries: Reviewing the Evidence. Ann. Nutr. Metab. 2010, 57, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Al-Senaeai, A.A.A.A. Health Crisis in Yemen during War. Int. J. Sci. Res. 2019, 7, 2734–2741. [Google Scholar]
- Giacaman, R.; Khatib, R.; Shabaneh, L.; Ramlawi, A.; Sabri, B.; Sabatinelli, G.; Khawaja, M.; Laurance, T. Health status and health services in the occupied Palestinian territory. Lancet 2009, 373, 837–849. [Google Scholar] [CrossRef]
- Van Berlaer, G.; Elsafti, A.M.; Al Safadi, M.; Saeed, S.S.; Buyl, R.; Debacker, M.; Redwan, A.; Hubloue, I. Diagnoses, infections and injuries in Northern Syrian children during the civil war: A cross-sectional study. PLoS ONE 2017, 12, e0182770. [Google Scholar] [CrossRef]
- Al-Jawaldeh, A.; Abul-Fadl, A. Assessment of the baby friendly hospital initiative implementation in the eastern Mediterra-nean region. Children 2018, 5, 41. [Google Scholar] [CrossRef] [PubMed]
- Allen, L.H.; Gillespie, S.R. What Works? A Review of the Efficacy and Effectiveness of Nutrition Interventions; Asian Development Bank: Mandaluyong, Philippines, 2001. [Google Scholar]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Yousafzai, A.K.; Obradović, J.; Rasheed, M.A.; Rizvi, A.; Portilla, X.A.; Tirado-Strayer, N.; Siyal, S.; Memon, U. Effects of responsive stimulation and nutrition interventions on children’s development and growth at age 4 years in a disadvantaged population in Pakistan: A longitudinal follow-up of a cluster-randomised factorial effectiveness trial. Lancet Glob. Health 2016, 4, e548–e558. [Google Scholar] [CrossRef]
- Yousafzai, A.K.; Rasheed, M.A.; Rizvi, A.; Armstrong, R.; Bhutta, Z.A. Effect of integrated responsive stimulation and nutrition interventions in the Lady Health Worker programme in Pakistan on child development, growth, and health outcomes: A cluster-randomised factorial effectiveness trial. Lancet 2014, 384, 1282–1293. [Google Scholar] [CrossRef]
- Saleem, A.F.; Mahmud, S.; Baig-Ansari, N.; Zaidi, A.K. Impact of Maternal Education about Complementary Feeding on Their Infants’ Nutritional Outcomes in Low- and Middle-income Households: A Community-based Randomized Interventional Study in Karachi, Pakistan. J. Health Popul. Nutr. 2014, 32, 623–633. [Google Scholar] [PubMed]
- Ghodsi, D.; Omidvar, N.; Rashidian, A.; Eini-Zinab, H.; Raghfar, H.; Aghayan, M. Effectiveness of the national food supplementary program on children growth and nutritional status in Iran. Matern. Child Nutr. 2018, 14, e12591. [Google Scholar] [CrossRef] [PubMed]
- Abolfotouh, M.A.; Nofal, L.M.; Safwat, H.; Abolfotouh, M.A.; Nofal, L.M.; Safwat, H. Growth and nutritional status of preschool children attending the well-baby clinics. J. Egypt. Public Health Assoc. 1990, 65, 485–507. [Google Scholar]
- Agha, S.Y. Supplementary feeding of malnourished children in northern Iraq. EMHJ East. Mediterr. Health J. 2005, 10, 12–18. [Google Scholar]
- Jabbari Beirami, H.; Bakhshian, F.; Vahidi, R. Assessment of the effectiveness of health care on children under five years through the health system in East Azarbaijan and Zanjan provinces. Med. Sci. J. Islamic Azad Univ. 2007, 17, 17–22. [Google Scholar]
- Zavoshy, R.; Noroozi, M.; Jahanihashemi, H.; Kiamiri, D. Nutritional Intervention on Malnutrition in 3-6 Years Old Rural Children in Qazvin Province, Iran. Pak. J. Biol. Sci. 2012, 15, 347–352. [Google Scholar] [CrossRef]
- Morikawa, M.; Polanc, A.; Becker, S. Continuous weight and height gain among at-risk children discharged from a supplementary feeding center in Kabul, Afghanistan. ICAN Infant Child Adolesc. Nutr. 2013, 5, 97–99. [Google Scholar] [CrossRef][Green Version]
- Lin, A.; Salehi, A.S. Stimulating demand: Effects of a conditional cash transfer programme on increasing maternal and child health-service utilisation in Afghanistan, a quasi-experimental study. Lancet 2013, 381, S84. [Google Scholar] [CrossRef]
- Doocy, S.; Tappis, H.; Paul, A.; Klemm, R.; Funna, S. Preventing malnutrition in children under two (PM2A): A case study in the food insecure context of South Sudan. World Health Popul. 2013, 14, 12–22. [Google Scholar] [CrossRef] [PubMed]
- Campbell, L. Cross-Sector Cash Assistance for Syrian Refugees and Host Communities in Lebanon: An IRC Programme; The Cash Learning Partnership. 2014. Available online: http://hdl.handle.net/10546/322214 (accessed on 1 February 2019).
- Slaymaker, T. Save the Children (UK) South Sudan Programme; Internal Report; Water Policy Programme Overseas Development Institute: London, UK, 2004. [Google Scholar]
- Fenn, B.; Sangrasi, G.M.; Puett, C.; Trenouth, L.; Pietzsch, S. The REFANI Pakistan study--A cluster randomized controlled trial of the effectiveness and cost-effectiveness of cash-based transfer programmes on child nutrition status: Study protocol. BMC Public Health 2015, 15, 1044. [Google Scholar] [CrossRef] [PubMed]
- Rouhani, S.; Yazdani, J.; Rostami, F.; Roushan, S.; Rahimian, R. Assessment of nutritional support delivered by Imam Khomaini Relif Fundation on improvement of growth-retaded children aged 1–6 years in Neka. J. Knowl. Health Basic Med. Sci. 2010, 5, 85. [Google Scholar]
- Al-Mudhwahi, A.A. Role of Integrated Outreach Activities in Improving Nutritional Status among Under-Five Children in Yemen. J. Nutr. Sci. Vitaminol. 2015, 61, 60–62. [Google Scholar] [CrossRef] [PubMed]
- Omidvar, N.; Ghodsi, D.; Eini-Zinab, H.; Rashidian, A.; Raghfar, H. Impact of the national food supplementary program for children on household food security and maternal weight status in Iran. Int. J. Prev. Med. 2016, 7, 108. [Google Scholar] [CrossRef] [PubMed]
- Abedzadeh Zavareh, M.S.; Hasani, M.; Darabi, M.; Mirzaei, A.; Khorshidi, A.; Saeidi, A.; Momeni, K.; Jalilian, M. Growth indicators and nutritional supplement evaluation in 6–12 months year old children’s: A perspective From Ilam. Electron. J. Gen. Med. 2018, 15, em17. [Google Scholar]
- Ghodsi, D.; Rashidian, A.; Omidvar, N.; Eini-Zinab, H.; Raghfar, H.; Ebrahimi, M. Process evaluation of a national, communitybased, food supplementary programme for improving the nutritional status of children in Iran. Public Health Nutr. 2018, 21, 2811–2818. [Google Scholar] [CrossRef]
- Fenn, B.; Colbourn, T.; Dolan, C.; Pietzsch, S.; Sangrasi, M.; Shoham, J. Impact evaluation of different cash-based intervention modalities on child and maternal nutritional status in Sindh Province, Pakistan, at 6 mo and at 1 y: A cluster randomised controlled trial. PLoS Med. 2017, 14, e1002305. [Google Scholar] [CrossRef] [PubMed]
- Trenouth, L.; Colbourn, T.; Fenn, B.; Pietzsch, S.; Myatt, M.; Puett, C. The cost of preventing undernutrition: Cost, cost-efficiency and cost-effectiveness of three cash-based interventions on nutrition outcomes in Dadu, Pakistan. Health Policy Plan. 2018, 33, 743–754. [Google Scholar] [CrossRef] [PubMed]
- Froozani, M.; Permehzadeh, K.; Motlagh, A.; Golestan, B. Effect of breastfeeding education on the feeding pattern and health of infants in their first 4 months in the Islamic Republic of Iran. Bull. World Health Organ. 1999, 77, 381. [Google Scholar]
- Bakhtiari, Z.; Rostami, S.; Keikhaei, B.; Cheraghian, B. The Effects of Training Mothers about Complementary Feeding on Growth Indicators of Infants in Dezful, Iran. Indo Am. J. Pharm. Sci. 2017, 4, 3907–3912. [Google Scholar]
- Zaman, S.; Ashraf, R.N.; Martines, J. Training in Complementary Feeding Counselling of Healthcare Workers and Its Influence on Maternal Behaviours and Child Growth: A Cluster-randomized Controlled Trial in Lahore, Pakistan. J. Health Popul. Nutr. 2008, 26, 210–222. [Google Scholar]
- Brown, N.; Finch, J.; Obradović, J.; Yousafzai, A. Maternal care mediates the effects of nutrition and responsive stimulation interventions on young children’s growth. Child Care Health Dev. 2017, 43, 577–587. [Google Scholar] [CrossRef] [PubMed]
- Malekafzali, H.; Abdollahi, Z.; Mafi, A.; Naghavi, M. Community-based nutritional intervention for reducing malnutrition among children under 5 years of age in the Islamic Republic of Iran. EMHJ East. Mediterr. Health J. 2001, 6, 238–245. [Google Scholar]
- Sheikholeslam, R.; Kimiagar, M.; Siasi, F.; Abdollahi, Z.; Jazayeri, A.; Keyghobadi, K.; Ghaffarpoor, M.; Noroozi, F.; Kalantari, M.; Minaei, N.; et al. Multidisciplinary intervention for reducing malnutrition among children in the Islamic Republic of Iran. EMHJ East. Mediterr. Health J. 2004, 10, 844–852. [Google Scholar]
- Hossain, M.; Choudhury, N.; Abdullah, K.A.B.; Mondal, P.; Jackson, A.A.; Walson, J.; Ahmed, T. Evidence-based approaches to childhood stunting in low and middle income countries: A systematic review. Arch. Dis. Child. 2017, 102, 903–909. [Google Scholar] [CrossRef] [PubMed]
- Majamanda, J.; Maureen, D.; Munkhondia, T.M.; Carrier, J. The Effectiveness of Community-Based Nutrition Education on the Nutrition Status of Under-five Children in Developing Countries. A Systematic Review. Malawi Med. J. 2014, 26, 115–118. [Google Scholar]
- Black, R.E.; Allen, L.H.; Bhutta, Z.A.; Caulfield, L.E.; De Onis, M.; Ezzati, M.; Mathers, C.; Rivera, J.; Maternal and Child Undernutrition Study Group. Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet 2008, 371, 243–260. [Google Scholar] [CrossRef]
- Lassi, Z.S.; Zahid, G.; Das, J.K.; Bhutta, Z.A. Systematic Review of Complementary Feeding Strategies amongst Children Less Than Two Years of Age; Division of Women and Child Health, The Aga Khan University: Karachi City, Pakistan, 2013. [Google Scholar]
- Sunguya, B.F.; Poudel, K.C.; Mlunde, L.B.; Urassa, D.P.; Yasuoka, J.; Jimba, M. Nutrition Training Improves Health Workers’ Nutrition Knowledge and Competence to Manage Child Undernutrition: A Systematic Review. Front. Public Health 2013, 1, 37. [Google Scholar] [CrossRef]
- Dewey, K.G.; Adu-Afarwuah, S. Systematic review of the efficacy and effectiveness of complementary feeding interventions in developing countries. Matern. Child Nutr. 2008, 4, 24–85. [Google Scholar] [CrossRef] [PubMed]
- Ghodsi, D. A Study of Program Analysis, Effectiveness and Cost Analysis of “Multidisciplinary Interventional Program for Improvement of Nutritional Status of Children in Iran; Shahid Beheshti University of Medical Sciences: Tehran, Iran, 2016. [Google Scholar]
- Fernald, L.C.H.; Gertler, P.J.; Neufeld, L.M. 10-year effect of Oportunidades, Mexico’s conditional cash transfer programme, on child growth, cognition, language, and behaviour: A longitudinal follow-up study. Lancet 2009, 374, 1997–2005. [Google Scholar] [CrossRef]
- Fernald, L.C.; Gertler, P.J.; Neufeld, L.M. Role of cash in conditional cash transfer programmes for child health, growth, and development: An analysis of Mexico’s Oportunidades. Lancet 2008, 371, 828–837. [Google Scholar] [CrossRef]
- World Health Organization. Technical Note: Supplementary Foods for the Management of Moderate Acute Malnutrition in Infants and Children 6–59 Months of Age; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Vasquez, N.A.; Daher, J. Do nutrition and cash-based interventions and policies aimed at reducing stunting have an impact on economic development of low-and-middle-income countries? A systematic review. BMC Public Health 2019, 19, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Das, J.; Do, Q.-T.; Özler, B. Reassessing Conditional Cash Transfer Programs. World Bank Res. Obs. 2005, 20, 57–80. [Google Scholar] [CrossRef]
- Afghanistan Ministry of Public Health; UNICEF. National Nutrition Survey Afghanistan: Survey Report; Afghanistan Ministry of Public Health: Kabul, Afghanistan, 2013.
- World Health Organization. UNICEF/WHO/The World Bank Group Joint Child Malnutrition Estimates—Levels and Trends; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Dureab, F.; Al-Falahi, E.; Ismail, O.; Al-Marhali, L.; Al Jawaldeh, A.; Nuri, N.N.; Safary, E.; Jahn, A. An Overview on Acute Malnutrition and Food Insecurity among Children during the Conflict in Yemen. Children 2019, 6, 77. [Google Scholar] [CrossRef] [PubMed]
- Cargo, M.; Harris, J.; Pantoja, T.; Booth, A.; Harden, A.; Hannes, K.; Cargo, M.; Thomas, J. Cochrane Qualitative and Implementation Methods Group guidance series—Paper 4: Methods for assessing evidence on intervention implementation. J. Clin. Epidemiol. 2018, 97, 59–69. [Google Scholar] [CrossRef]
- WHO. Global Nutrition Policy Review 2016–2017: Country Progress in Creating Enabling Policy Environments for Promoting Healthy Diets and Nutrition; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- UNSCN. United Nations Decade of Action on Nutrition. 2016. Available online: https://www.unscn.org/en/topics/un-decade-of-action-on-nutrition (accessed on 22 January 2021).
- World Health Organization. Regional Office for the Eastern Mediterranean. Strategy on Nutrition for the Eastern Mediterranean Region 2020–2030. 2019. Available online: https://apps.who.int/iris/handle/10665/330059 (accessed on 22 January 2021).
| Author/Country/Year | Reason for Exclusion |
|---|---|
| Abolfotouh et al./Egypt/1999 [31] | It was a cross-sectional study and not a community-based intervention |
| Djazayery A./Iran/2004 [11] | It was a report on the nutrition intervention in the region, there was no data regarding the children’ anthropometry and it was not a randomized trial. |
| Agha SY./Iraq/2004 [32] | It was a before-after study with no control group. |
| Jabbari-Beirami et al./Iran/2007 [33] | It was a cross-sectional study and not a community-based intervention |
| Zavoshy et al./Iran/2012 [34] | It was a before-after study without a control group. |
| Morikawa et al./Afghanistan/2013 [35] | It was a before-after study with no control group and the primary outcomes were not reported properly. |
| Lin and Salehi/Afghanistan/2013 [36] | It was an abstract without full text and there were no data regarding children’ anthropometry. |
| Doocy et al./South Sudan/2013 [37] | There were not any data regarding children anthropometric outcomes. |
| Cambell L./Lebanon/2014 [38] | Not relevant, as there was not any anthropometric outcome of children, thus the study was beyond the scope of this review. |
| Soly-maker T/South Sudan/2004 [39] | There was no data regarding children’ anthropometry |
| Fenn et al., Pakistan/2015 [40] | It was a protocol study |
| Rouhani et al., Iran/2015 [41] | It was a poster and the full-text was not available. |
| AL-Mudhwahi A., Yemen/2015 [42] | It was a descriptive study, not a controlled trial. |
| Ghodsi et al., Iran/2016 [43] | There was no data regarding the children’ anthropometry and it was not a randomized trial. |
| Zavareh et al., Iran/2017 [44] | A descriptive-analytical study |
| Ghodsi et al., Iran/2018 [45] | There were not any data regarding children anthropometric outcomes. |
| Author | Selection Bias: Allocation Concealment | Performance Bias: Blinding of Participants and Personnel | Detection Bias: Blinding of Outcome Assessment | Attrition Bias: Incomplete Outcome Data | Reporting Bias: Selective Reporting | Overall RoB Judgment |
|---|---|---|---|---|---|---|
| Ghodsi et al., 2018 [30] | L | S | L | L | L | S |
| Fenn et al., 2017 [46] | L | S | L | L | L | S |
| Trenouth et al., 2018 [47] | L | S | L | L | L | S |
| Forozani, et al., 1999 [48] | L | S | S | S | H | H |
| Saleem et al., 2014 [29] | L | S | S | L | L | S |
| Bakhtiari et al., 2017 [49] | H | S | S | H | L | H |
| Zaman et al., 2008 [50] | L | S | S | L | L | L |
| Yousafzai et al., 2014 [28] | L | S | L | L | L | L |
| Yousafzai et al., 2016 [27] | L | S | L | L | L | L |
| Brown et al., 2017 [51] | L | S | L | L | L | L |
| Malekafzali et al., 2000 [52] | S | H | H | H | H | H |
| Sheikholeslam et al., 2004 [53] | H | S | H | H | L | H |
| Author/Year | Country/Region | Design | Type(s) of Intervention | Subjects (n)/ Age/Duration | Outcome(s) |
|---|---|---|---|---|---|
| 1. Interventions used nutrition education/nutrition counselling | |||||
| Zaman et al., 2008 | Pakistan/urban | Cluster randomized controlled trial | Mother’s nutrition counselling using locally adapted of Pakistan’s IMCI ‘feeding counselling card’ by Lady Health Workers regarding the recommended foods and frequency of feeding according to age of the child | Mother and 6–24 mo child pairs. Interventions: n = 189 Controls: n = 186/ 6.5m intervention | Baseline: WAZ: I:−1.089 ± 1.22 C: −1.439 ± 1.22, p = 0.125 HAZ: I: −1.115 ± 1.36 C: −1.407 ± 1.22, p = 0.167 WHZ: I: −0.450 ± 1.01 C: −0.559 ± 1.08, p = 0.451 End of the study: WAZ: I: −1.174 ± 1.94 C: −1.720 ± 1.27, p = 0.012 HAZ: I: −1.582 ± 1.58 (p = 0.55) C: −1.705 ± 1.24 WHZ: I: −0.286 ± 1.22 C: −0.794 ± 1.15 (p = 0.004) |
| Saleem et al., 2014 | Pakistan/peri-urban | cluster-randomized interventional trial | Intervention group received maternal educational on importance of breastfeeding (BF), its continuation for the first two years of life and the importance of complementary feeding (CF) initiation at 6 m., age-related complementary food, and hand washing and general hygiene promoting protein-based and iron-rich foods. The control group received advice about BF according to national guidelines | Mothers of infants aged 10–20 weeks. Interventions: n = 118 Controls: n = 94/ 6 m intervention | Intervention group had a higher mean weight of 350 g (p = 0.001); and length of 0.66 cm (p = 0.001) (p = 0.002) compared to the controls; proportionate reduction of stunting and underweight were 10% (84% vs. 74%; OR adj 8.36 (5.6–12.42) and 5% (25% vs. 20%; OR adj 0.75 (0.4–1.79) in the intervention compared to the control group. |
| Yousafzai et al., 2014 (Yousafzai et al., 2014) | Pakistan/rural | factorial, cluster-randomized effectiveness trial | Pakistan Early Child Development Scale-Up (PEDS): 1: Enhanced Nutrition (EN) group received nutrition education regarding association of good nutrition and health, additional advice on responsive feeding, and problem solving about feeding and a multiple micronutrient powder which contains iron, folic acid, Vit A, and Vit C. 2: Responsive Stimulation (RS) group: a local adaptation of the Care for Child Development approach developed by UNICEF and WHO) 3.Combined responsive stimulation and enhanced nutrition (RS&EN) 4. Controls: routine health and nutrition services | Infants up to 2.5 month divided to four groups and received intervention till age 24 m: EN: n = 364 RS: n = 383 RS&EN: n = 374 Controls: n = 368/Up to 24 m. | HAZ 6 m: EN: −1.2 ± 1.3 vs. no EN: −1.4 ± 1.2, p < 0.0001; 18 m: EN: −2.2 ± 1.2 vs. no EN: −2.4 ± 1.1, p = 0.02. Not significant differ in mean WAZ between the groups at 6, 12, 18, or 24 m. |
| Yousafzai et al., 2016 | Pakistan/rural | Follow-up study of the initial cluster-randomized effectiveness trial | Pakistan Early Child Development Scale-Up (PEDS): 1: Enhanced Nutrition (EN) 2: Responsive Stimulation (RS) 3: Combined responsive stimulation and enhanced nutrition (RS&EN) 4: Controls (C) | 1302 mother–child dyads (87% of the dyads in the original enrolment) followed up at 4 years of age 1-EN: n = 311 2-RS: n = 345 3-RS&EN: n = 315 4-C: n = 331 testing differences between exposures to the two interventions (RS (n = 657) vs. no RS (n = 638) and EN (n = 620) vs. no EN (n = 675))/ 4 years follow up study | RS (data are mean (%95CI)): WAZ: 0.8 (−0.9 to −0.7) HAZ: −0.9 (−1.0 to −0.7). WHZ: −0.5 (−0.5 to −0.4) no RS WAZ: −0.9(−0.9 to −0.8) HAZ: −0.09(−1.0 to −0.7) WHZ: −0.5 (−0.6 to −0.4) EN: WAZ:−0.8 (−0.9 to −0.7) underweight: 11% HAZ: −0.8 (−1.0 to −0.7) WHA: −0.4 (−0.5 to −0.3) No EZ: WAZ: −0.9 (−1.0 to −0.8) HAZ: −0.9 (−1.0 to −0.8) WHZ: −0.5 (−0.6 to −0.4) |
| Brown et al., 2017 | Pakistan/rural | factorial, cluster-randomized effectiveness trial | Pakistan Early Child Development Scale-Up (PEDS): 1: Enhanced Nutrition (EN) 2: Responsive Stimulation (RS) 3: Combined responsive stimulation and enhanced nutrition (RS&EN) 4: Controls (C) | 1302 mother–child dyads at 4 years of age 1-EN: n = 364 2-RS: n = 383 3-RS&EN:n = 374 4-C: n = 368/ 2 years (indicators related to measures at ages 2 and 4) | Mother–child interaction quality mediated the effects of both EN and RS on HAZ at 4 years via its longitudinal stability from 2 years of age (β = 0.016, p = 0.005; β = 0.048, p < 0.001, respectively). |
| 2. Interventions used food distribution through different modalities | |||||
| Fenn et al., 2017 | Pakistan/rural area | Cost, cost-efficiency, and cost-effectiveness study, cluster randomized controlled trial | Research on Food Assistance for Nutritional Impact (REFANI): Monthly cash-based interventions (CBIs) for 6 months: 1: Standard cash (SC) (PKR 1500, USD 14) 2: Double cash (DC), (PKR 3000); 3: Fresh food voucher (FFV) of PKR 1500 (USD 14, could be exchanged for specified fresh foods (fruits, vegetables, milk, and meat) in nominated shops) | 6–48mo.children Controls: n = 852 DC: n = 839 FFV: n = 866, SC: n = 905/ 6 mo. CBIs distribution and follow-up on 12 mo | Mean WHZ significantly improved in both the FFV and DC arms at 6mo (FFV: z-score = 0.16; 95% CI 0.05, 0.26; p = 0.004; DC: z-score = 0.11; 95% CI 0.00, 0.21; p = 0.05) compared to the CG. All three intervention groups showed similar significantly lower odds of being stunted (HAZ < −2) at 6 mo (DC: OR = 0.39; 95% CI 0.24, 0.64; p < 0.001; FFV: OR = 0.41; 95% CI 0.25, 0.67; p < 0.001; SC: OR = 0.36; 95% CI 0.22, 0.59; p < 0.001) and at 1 y (DC: OR = 0.53; 95% CI 0.35, 0.82; p = 0.004; FFV: OR = 0.48; 95% CI 0.31, 0.73; p = 0.001; SC: OR = 0.54; 95% CI 0.36, 0.81; p = 0.003) compared to the CG. |
| Ghodsi et al., 2018 | Iran/urban and rural area | Quasi-experimental and mixed-methods | Monthly in-kind food/food voucher/cash transfer for buying specified food items (cheese, honey, spaghetti, oil, sugar, bean, lentil, eggs, milk, and chicken) from nominated shops | under 5yr. child Controls: n = 409, Interventions: n = 362/ 6 m intervention | Significant differences (p < 0.001) were seen within each group in each index at the end of the study. Mean difference of indices in Intervention group after 6 mo.: WAZ: 0.16 ± 0.62 HAZ: 0.08 ± 0.77 WHZ: 0.2 ± 0.91 Mean of difference in controls: WAZ: 0.13 ± 0.68 HAZ: 0.07 ± 1.04 WHZ: 0.2 ± 0.81 |
| Trenouth et al., 2018 | Pakistan/rural area | Cluster randomized controlled trial and mixed-methods process evaluation | Research on Food Assistance for Nutritional Impact (REFANI): Monthly cash-based interventions (CBIs): 1: Standard cash (SC) (PKR 1500, USD14) 2: Double cash (DC),(PKR 3000; 3: Fresh food voucher (FFV) of PKR 1500 (14 USD, could be exchanged for specified fresh foods (fruits, vegetables, milk, and meat) in nominated shops) | 6–48 mo. children Controls: n = 852 DC: n = 839 FFV: n = 866, SC: n = 905/ 6 mo. CBIs distribution and follow-up on 12 mo. | TCTRs: DC: USD 1.82, SC: USD 2.82, and FFV: USD 2.73. The total cost per beneficiary household: SC: USD 193, FFV: USD 220, and DC: USD 284 Operational costs per recipient household: SC: USD 105, DC: USD 109, and FFV: USD 132 The cost per child in a household receiving cash or vouchers: DC: USD 203, SC:USD 135, FFV: USD 160 The cost per case of stunting averted: DC: USD 1290, SC: USD 882, FFV: USD 883. The cost per DALY averted *: DC: USD 64, SC: USD 434, and FFV: USD 563 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghodsi, D.; Omidvar, N.; Nikooyeh, B.; Roustaee, R.; Shakibazadeh, E.; Al-Jawaldeh, A. Effectiveness of Community Nutrition-Specific Interventions on Improving Malnutrition of Children under 5 Years of Age in the Eastern Mediterranean Region: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 7844. https://doi.org/10.3390/ijerph18157844
Ghodsi D, Omidvar N, Nikooyeh B, Roustaee R, Shakibazadeh E, Al-Jawaldeh A. Effectiveness of Community Nutrition-Specific Interventions on Improving Malnutrition of Children under 5 Years of Age in the Eastern Mediterranean Region: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2021; 18(15):7844. https://doi.org/10.3390/ijerph18157844
Chicago/Turabian StyleGhodsi, Delaram, Nasrin Omidvar, Bahareh Nikooyeh, Roshanak Roustaee, Elham Shakibazadeh, and Ayoub Al-Jawaldeh. 2021. "Effectiveness of Community Nutrition-Specific Interventions on Improving Malnutrition of Children under 5 Years of Age in the Eastern Mediterranean Region: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 18, no. 15: 7844. https://doi.org/10.3390/ijerph18157844
APA StyleGhodsi, D., Omidvar, N., Nikooyeh, B., Roustaee, R., Shakibazadeh, E., & Al-Jawaldeh, A. (2021). Effectiveness of Community Nutrition-Specific Interventions on Improving Malnutrition of Children under 5 Years of Age in the Eastern Mediterranean Region: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 18(15), 7844. https://doi.org/10.3390/ijerph18157844







