Nutrient Dense, Low-Cost Foods Can Improve the Affordability and Quality of the New Zealand Diet—A Substitution Modeling Study
Abstract
:1. Introduction
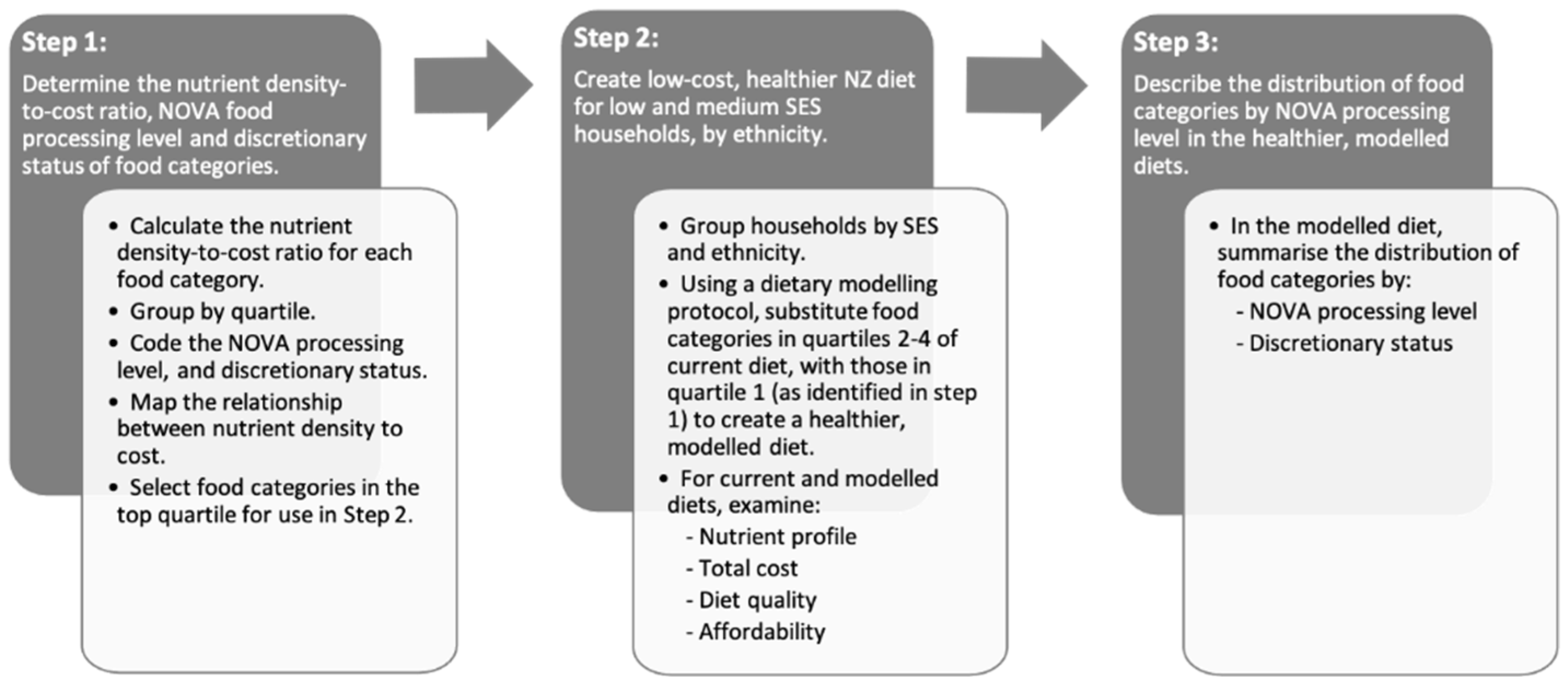
2. Materials and Methods
2.1. Nutrient and Food Price Databases
2.1.1. NZ Food and Nutrient Database and Selection of Representative Foods
2.1.2. Food Price of Selected Representative Foods
2.1.3. Dietary Intake Database
2.2. Classification of Each Food Category by NOVA Processing Level and Discretionary Status
2.3. Dietary Modeling Protocol
2.3.1. Diet Quality
2.3.2. Diet Cost and Affordability
2.4. Statistical Analyses
3. Results
3.1. Nutrient Density, Cost, and the Top Quartile of Nutrient Dense, Low-Cost NZ Food Categories
3.2. The Current NZ Diet for Māori, Pacific, and NZEO Households, from Low and Medium Socioeconomic Deciles
3.3. The Theoretical Healthier, Low-Cost Diet
3.4. Diet Quality of the Current and Healthier Modeled Diets
3.5. Distribution of NOVA Processing Levels and Food Categories in the Current and Healthier, Low-Cost Diets
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mackay, S.; Buch, T.; Vandevijvere, S.; Goodwin, R.; Korohina, E.; Funaki-Tahifote, M.; Lee, A.; Swinburn, B. Cost and Affordability of Diets Modelled on Current Eating Patterns and on Dietary Guidelines, for New Zealand Total Population, Māori and Pacific Households. Int. J. Environ. Res. Public Health 2018, 15, 1255. [Google Scholar] [CrossRef] [Green Version]
- National Health and Medical Research Council. Eat for Health: Australian Dietary Guidelines. Providing the Scientific Evidence for healthier Australian Diets; National Health and Medical Research Council: Canberra, ACT, Australia, 2013. [Google Scholar]
- Darmon, N.; Drewnowski, A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: A systematic review and analysis. Nutr. Rev. 2015, 73, 643–660. [Google Scholar] [CrossRef]
- Drewnowski, A. Obesity, diets, and social inequalities. Nutr. Rev. 2009, 67, S36–S39. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health. Longer, Healthier Lives: New Zealand’s Health 1990–2017; Ministry of Health: Wellington, New Zealand, 2020.
- Mackay, S.; Parnell, W.; Heath, A.-L.; Brown, R.; Wilson, N.; Gray, A.; Turley, M.; Weerasekera, D.; Fleming, L.; Thomson, C.; et al. A Focus on Nutrition: Key Findings of the 2008/09 New Zealand Adult Nutrition Survey; University of Otago and Ministry of Health: Wellington, New Zealand, 2011. [Google Scholar]
- Yeh, L.-C.; Timutimu, R.; Himona, P.; Talamaivao, N.; Searle, P.; Weerasekera, D.; Martinuseen, M. Tatau Kahukura: Māori Health Chart Book 2015, 3rd ed.; Ministry of Health: Wellington, New Zealand, 2015.
- Mackay, S.; Parnell, W.; Heath, A.-L.; Brown, R.; Wilson, N.; Gray, A.; Turley, M.; Weerasekera, D.; Fleming, L.; Thomson, C.; et al. A Focus on Pacific Nutrition: Findings from the 2008/09 New Zealand Adult Nutrition Survey; Ministry of Health: Wellington, New Zealand, 2012.
- Lewis, M.; Lee, A.J. Affording health during the COVID-19 pandemic and associated economic downturn. Aust. N. Z. J. Public Health 2020, 44, 519–520. [Google Scholar] [CrossRef]
- Metcalf, P.A.; Scragg, R.R.; Schaaf, D.; Dyall, L.; Black, P.N.; Jackson, R. Dietary intakes of European, Māori, Pacific and Asian adults living in Auckland: The diabetes, heart and health study. Aust. N. Z. J. Public Health 2008, 32, 454–460. [Google Scholar] [CrossRef] [PubMed]
- Annual Update of Key Results 2019/20: New Zealand Health Survey. Available online: https://www.health.govt.nz/publication/annual-update-key-results-2019-20-new-zealand-health-survey (accessed on 22 February 2021).
- New Zealand Health Survey Annual Data Explorer. Available online: https://minhealthnz.shinyapps.io/nz-health-survey-2018-19-annual-data-explorer/_w_c5d421d5/#!/home (accessed on 21 November 2020).
- Clinical Trials Research Unit. Enhancing Food Security and Physical Activity for Māori, Pacific and Low-Income Families/Whanau—An. Evidence Summary; Prepared for the Ministry of Health and the Health Research Council; Health Research Council of New Zealand and the Ministry of Health: Auckland, New Zealand, 2008. [Google Scholar]
- Drewnowski, A. The Nutrient Rich Foods Index helps to identify healthy, affordable foods. Am. J. Clin. Nutr. 2010, 91, 1095S–1101S. [Google Scholar] [CrossRef] [PubMed]
- Blumfield, M.; Starck, C.; Keighley, T.; Roesler, A.; Abbott, K.; Cassettari, T.; Marshall, S.; Fayet-Moore, F. Diet and economic modelling to improve the quality and affordability of the Australian diet for low and medium socioeconomic households. Int. J. Environ. Res. Public Health 2021, 18, 5771. [Google Scholar] [CrossRef]
- Wilson, N.; Nghiem, N.; Ni Mhurchu, C.; Eyles, H.; Baker, M.G.; Blakely, T. Foods and Dietary Patterns That Are Healthy, Low-Cost, and Environmentally Sustainable: A Case Study of Optimization Modeling for New Zealand. PLoS ONE 2013, 8, e59648. [Google Scholar] [CrossRef] [Green Version]
- Vandevijvere, S.; Young, N.; Mackay, S.; Swinburn, B.; Gahegan, M. Modelling the cost differential between healthy and current diets: The New Zealand case study. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 16. [Google Scholar] [CrossRef]
- Vandevijvere, S.; Mackay, S.; Waterlander, W. INFORMAS Protocol: Food Prices Module [Internet]. Available online: https://auckland.figshare.com/articles/journal_contribution/INFORMAS_Protocol_Food_Prices_Module/5627440/1 (accessed on 25 October 2020).
- Nga Tikanga Paihere. Available online: https://data.govt.nz/use-data/data-ethics/nga-tikanga-paihere/ (accessed on 25 October 2020).
- Husereau, D.; Drummond, M.; Petrou, S.; Carswell, C.; Moher, D.; Greenberg, D.; Augustovski, F.; Briggs, A.H.; Mauskopf, J.; Loder, E. Consolidated health economic evaluation reporting standards (CHEERS) statement. BMJ 2013, 11, 6. [Google Scholar] [CrossRef] [Green Version]
- NZ Food Composition Data. Available online: https://www.foodcomposition.co.nz/ (accessed on 25 October 2020).
- Monteiro, C.; Cannon, G.; Levy, R.; Moubarac, J.-C.; Jaime, P.; Martins, A.P.; Canella, D.; Louzada, M.; Parra, D. NOVA. The star shines bright. Position paper 2. World Nutr. 2016, 7, 28–38. [Google Scholar]
- Starck, C.; Blumfield, M.; Keighley, T.; Petocz, P.; Roesler, A.; Abbott, K.; Cassettari, T.; Marchall, S.; Fayet-Moore, F. 2020 NRAUS Australia New Zealand Food Category Cost Dataset. Dryad 2021. [Google Scholar] [CrossRef]
- Socioeconomic Deprivation Indexes: NZDep and NZiDep, Department of Public Health. Available online: https://www.otago.ac.nz/wellington/departments/publichealth/research/hirp/otago020194.html#2018 (accessed on 25 October 2020).
- Parnell, P.; Scragg, R.; Wilson, N.; Schaaf, D.; Fitzgerald, E. NZ Food NZ Children. Key results of the 2002 National Children’s Nutrition Survey; Ministry of Health: Wellington, New Zealand, 2003.
- Apply to Use Microdata for Research. Available online: https://www.stats.govt.nz/integrated-data/apply-to-use-microdata-for-research/ (accessed on 21 November 2020).
- Monteiro, C.A.; Levy, R.B.; Claro, R.M.; de Castro, I.R.R.; Cannon, G. A new classification of foods based on the extent and purpose of their processing. Cad. Saúde Pública 2010, 26, 2039–2049. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monteiro, C.; Cannon, G.; Levy, R.; Moubarac, J.-C.; Louzada, M.; Rauber, F.; Khandpur, N.; Cediel, G.; Neri, D.; Martinez Steele, E.; et al. Ultra-processed foods: What they are and how to identify them. Public Health Nutr. 2019, 22, 936–941. [Google Scholar] [CrossRef]
- Machado, P.P.; Steele, E.M.; Levy, R.B.; Sui, Z.; Rangan, A.; Woods, J.; Gill, T.; Scrinis, G.; Monteiro, C.A. Ultra-processed foods and recommended intake levels of nutrients linked to non-communicable diseases in Australia: Evidence from a nationally representative cross-sectional study. BMJ Open 2019, 9, e029544. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- 4363.0.55.001—Australian Health Survey: Users’ Guide, 2011–2013. Discretionary Foods. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4363.0.55.001Chapter65062011-13 (accessed on 10 December 2020).
- Fulgoni, V.L., III; Keast, D.R.; Drewnowski, A. Development and Validation of the Nutrient-Rich Foods Index: A Tool to Measure Nutritional Quality of Foods. J. Nutr. 2009, 139, 1549–1554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Household Income and Housing-Cost Statistics: Year Ended June 2019. Available online: https://www.stats.govt.nz/information-releases/household-income-and-housing-cost-statistics-year-ended-june-2019 (accessed on 25 October 2020).
- Nutrient Reference Values for Australia and New Zealand. Available online: https://www.nrv.gov.au/ (accessed on 23 October 2020).
- Ministry of Health. Eating and Activity Guidelines for New Zealand Adults; Ministry of Health: Wellington, New Zealand, 2015.
- National Health and Medical Research Council. Eat for Health -Educator’s Guide; National Health and Medical Research Council: Canberra, ACT, Australia, 2013. [Google Scholar]
- Ministry of Health. Eating and Activity Guidelines for New Zealand Adults; Updated 2020; Ministry of Health: Wellington, New Zealand, 2020.
- Roy, R.; Hebden, L.; Rangan, A.; Allman-Farinelli, M. The development, application, and validation of a Healthy eating index for Australian Adults (HEIFA-2013). Nutrition 2016, 32, 432–440. [Google Scholar] [CrossRef]
- Delshad, M.; Beck, K.L.; von Hurst, P.R.; Mugridge, O.; Conlon, C.A. The validity and reliability of the Dietary Index for a Child’s Eating in 2-8-year old children living in New Zealand. Matern. Child. Nutr. 2019, 15, e12758. [Google Scholar] [CrossRef] [Green Version]
- R: A language and Environment for Statistical Computing. Available online: https://www.R-project.org/. (accessed on 15 December 2020).
- Wickham, H.; Averick, M.; Bryan, J.; Chang, W.; D’Agostino McGowan, L.; Francois, R.; Grolemund, G.; Hayes, A.; Henry, L.; Hester, J.; et al. Welcome to the tidyverse. J. Open Source Softw. 2019, 4, 1686. [Google Scholar] [CrossRef]
- Ministry of Health. New Serving Size Advice; Ministry of Health: Wellington, New Zealand, 2020.
- Stevenson, S. Edible Impact. Food Security Policy: A Review of Literature and Synthesis of Key Recommendations for Toi Te Ora—Public Health Service; Public Health Service: Bay of Plenty, New Zealand, 2011. [Google Scholar]
- GST and Food. Available online: https://www.ato.gov.au/print-publications/gst-and-food/?=top_10_publications (accessed on 15 April 2021).
- GST Rate. Available online: https://www.govt.nz/browse/tax-benefits-and-finance/tax/gst-rate/ (accessed on 15 April 2021).
- Gupta, S.; Hawk, T.; Aggarwal, A.; Drewnowski, A. Characterizing Ultra-Processed Foods by Energy Density, Nutrient Density, and Cost. Front. Nutr. 2019, 6. [Google Scholar] [CrossRef] [Green Version]
- Drewnowski, A.; Gupta, S.; Darmon, N. An Overlap Between “Ultraprocessed” Foods and the Preexisting Nutrient Rich Foods Index? Nutr. Today 2020, 55, 75–81. [Google Scholar] [CrossRef]
- Jones, J.M. Food processing: Criteria for dietary guidance and public health? Proc. Nutr. Soc. 2019, 78, 4–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Healthy Active Learning. Available online: https://www.health.govt.nz/our-work/preventative-health-wellness/nutrition/healthy-active-learning (accessed on 12 April 2021).
- Ministry of Health. Healthy Food and Drink Guidance—Schools; Ministry of Health: Wellington, New Zealand, 2020.
- Ka Ora, Ka Ako. Healthy School Lunches Programme. Available online: https://www.education.govt.nz/our-work/overall-strategies-and-policies/wellbeing-in-education/free-and-healthy-school-lunches/ (accessed on 12 April 2021).
- Ministry of Education. Ka Ora, Ka Ako. Healthy School Lunches Programme Nutrition Guidelines; Ministry of Education: Wellington, New Zealand, 2020.
- Food Secure Communities. Available online: https://www.msd.govt.nz/what-we-can-do/community/food-secure-communities/index.html (accessed on 12 April 2021).
- Turley, M.; Ni Mhurchu, C.; Gorton, D.; Eyles, H.; Jull, A. Food and Nutrition Guidelines for Healthy Children and Young People (Aged 2–18 years). A Background Paper; Partial revision February 2015; Ministry of Health: Wellington, New Zealand, 2012.
- Vegetables and Fruit. Available online: https://nutritionfoundation.org.nz/nutrition-facts/food-groups/vegetables-and-fruit (accessed on 12 April 2021).
- Semnani-Azad, Z.; Khan, T.A.; Blanco Mejia, S.; de Souza, R.J.; Leiter, L.A.; Kendall, C.W.C.; Hanley, A.J.; Sievenpiper, J.L. Association of Major Food Sources of Fructose-Containing Sugars With Incident Metabolic Syndrome: A Systematic Review and Meta-analysis. JAMA Netw. Open 2020, 3, e209993. [Google Scholar] [CrossRef] [PubMed]
- Liska, D.; Kelley, M.; Mah, E. 100% Fruit Juice and Dental Health: A Systematic Review of the Literature. Front. Public Health 2019, 7, 190. [Google Scholar] [CrossRef] [Green Version]
- Ni Mhurchu, C.; Eyles, H.; Choi, Y.H. Effects of a Voluntary Front-of-Pack Nutrition Labelling System on Packaged Food Reformulation: The Health Star Rating System in New Zealand. Nutrients 2017, 9, 918. [Google Scholar] [CrossRef]


| Indicators 1 | Low SES Household | Medium SES Household | ||||||
|---|---|---|---|---|---|---|---|---|
| Māori | Pacific | NZEO | Total | Māori | Pacific | NZEO | Total | |
| 4-person reference household | 4-person reference household | |||||||
| Household member 2 | ||||||||
| Male (31–50 years) | ||||||||
| n | 70 | 81 | 39 | 190 | 20 | 14 | 54 | 88 |
| Age (y) | 39.5 (5.4) | 39.8 (4.8) | 38.9 (5.7) | 39.5 (5.2) | 42.0 (6.0) | 39.4 (6.9) | 40.0 (6.0) | 40.4 (6.1) |
| Height (cm) | 174.1 (6.5) | 175.2 (5.5) | 175.8 (8.7) | 174.9 (6.6) | 176.5 (7.4) | 177.6 (7.0) | 176.8 (6.6) | 176.8 (6.8) |
| Weight (kg) | 95.9 (22.6) | 105.1 (20.1) | 82.3 (16.3) | 97.0 (22.0) | 96.4 (16.5) | 109.1 (22.3) | 85.4 (14.0) | 91.7 (18.3) |
| BMI (kg/m2) | ||||||||
| Underweight (<18.5), n (%) | 0 (0.0%) | 1 (1.3%) | 1 (2.6%) | 2 (1.1%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Normal (18.5–24.9), n (%) | 8 (12.1%) | 3 (3.7%) | 15 (38.5%) | 26 (14.0%) | 1 (5.3%) | 1 (7.1%) | 14 (26.9%) | 16 (18.8%) |
| Overweight (25.0–29.9), n (%) | 28 (42.4%) | 15 (18.8%) | 16 (41.0%) | 59 (31.9%) | 7 (36.8%) | 2 (14.3%) | 27 (51.9%) | 36 (42.4%) |
| Obese (≥30.0), n (%) | 30 (45.5%) | 61 (76.2%) | 7 (17.9%) | 98 (53.0%) | 11 (57.9%) | 11 (78.6%) | 11 (21.2%) | 33 (38.8%) |
| Female (31–50 years) | ||||||||
| n | 128 | 96 | 52 | 276 | 29 | 19 | 67 | 115 |
| Age (y) | 38.9 (5.5) | 39.2 (5.4) | 40.4 (5.9) | 39.3 (5.6) | 38.9 (5.7) | 40.6 (4.9) | 40.7 (5.5) | 40.2 (5.5) |
| Height (cm) | 163.5 (5.2) | 163.9 (5.3) | 161.5 (6.0) | 163.3 (5.5) | 162.8 (5.6) | 164.6 (3.9) | 163.8 (6.9) | 163.7 (6.1) |
| Weight (kg) | 89.0 (24.4) | 95.4 (22.0) | 74.4 (17.6) | 88.3 (23.5) | 80.1 (18.7) | 94.2 (18.7) | 76.2 (17.0) | 80.2 (18.8) |
| BMI (kg/m2) | ||||||||
| Underweight (<18.5), n (%) | 1 (0.9%) | 0 (0.0%) | 0 (0.0%) | 1 (0.4%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Normal (18.5–24.9), n (%) | 18 (15.5%) | 4 (4.6%) | 13 (26.0%) | 35 (13.8%) | 5 (17.2%) | 1 (5.3%) | 21 (32.3%) | 27 (23.9%) |
| Overweight (25.0–29.9), n (%) | 27 (23.3%) | 22 (25.3%) | 23 (46.0%) | 72 (28.5%) | 15 (51.7%) | 4 (21.0%) | 23 (35.4%) | 42 (37.2%) |
| Obese (≥30.0), n (%) | 70 (60.3%) | 61 (70.1%) | 14 (28.0%) | 145 (57.3%) | 9 (31.0%) | 14 (73.7%) | 21 (32.3%) | 44 (38.9%) |
| Male (11–14 years) | ||||||||
| n | 67 | 110 | 17 | 194 | 36 | 13 | 46 | 95 |
| Age (y) | 12.4 (1.2) | 12.4 (1.1) | 12.5 (0.9) | 12.4 (1.1) | 12.4 (1.2) | 12.5 (1.1) | 12.4 (1.1) | 12.4 (1.2) |
| Height (cm) | 162.7 (11.6) | 161.7 (11.2) | 159.6 (8.5) | 161.9 (11.1) | 160.6 (11.6) | 160.5 (10.3) | 158.6 (11.6) | 159.6 (11.3) |
| Weight (kg) | 58.4 (19.4) | 65.4 (21.0) | 56.3 (11.5) | 62.2 (20.1) | 55.0 (15.6) | 58.1 (14.8) | 53.8 (12.8) | 54.8 (14.1) |
| BMI (kg/m2) | ||||||||
| Underweight (<18.5), n (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Normal (18.5–24.9), n (%) | 43 (68.3%) | 40 (38.1%) | 8 (53.3%) | 91 (49.7%) | 21 (65.6%) | 4 (33.3%) | 27 (62.8%) | 52 (59.8%) |
| Overweight (25.0–29.9), n (%) | 12 (19.0%) | 33 (31.4%) | 6 (40.0%) | 51 (27.9%) | 8 (25.0%) | 6 (50.0%) | 13 (30.2%) | 27 (31.0%) |
| Obese (≥30.0), n (%) | 8 (12.7%) | 32 (30.5%) | 1 (6.7%) | 41 (22.4%) | 3 (9.4%) | 2 (16.7%) | 3 (7.0%) | 8 (9.2%) |
| Female (7–10 years) | ||||||||
| n | 127 | 133 | 25 | 285 | 31 | 20 | 24 | 75 |
| Age (y) | 8.4 (1.2) | 8.6 (1.1) | 8.6 (1.2) | 8.5 (1.1) | 8.3 (1.2) | 8.6 (1.2) | 8.6 (1.2) | 8.5 (1.2) |
| Height (cm) | 135.6 (9.8) | 139.4 (9.9) | 135.1 (7.2) | 137.4 (9.8) | 136.4 (11.9) | 137.5 (10.2) | 135.0 (9.4) | 136.3 (10.6) |
| Weight (kg) | 36.5 (11.0) | 41.9 (13.0) | 32.9 (6.5) | 38.9 (12.1) | 37.3 (13.8) | 37.3 (10.9) | 35.1 (9.4) | 36.6 (11.7) |
| BMI (kg/m2) | ||||||||
| Underweight (<18.5), n (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Normal (18.5–24.9), n (%) | 59 (50.9%) | 50 (38.7%) | 17 (73.9%) | 126 (47.0%) | 14 (46.7%) | 9 (45.0%) | 12 (54.5%) | 35 (48.6%) |
| Overweight (25.0–29.9), n (%) | 35 (30.2%) | 34 (26.4%) | 4 (17.4%) | 73 (27.2%) | 9 (30.0%) | 9 (45.0%) | 8 (36.4%) | 26 (36.1%) |
| Obese (≥30.0), n (%) | 22 (19.0%) | 45 (34.9%) | 2 (8.7%) | 69 (25.7%) | 7 (23.3%) | 2 (10.0%) | 2 (9.1%) | 11 (15.3%) |
| SES Data | ||||||||
| Decile of socioeconomic deprivation (NZDep) 3 | 9–10 | 5–6 | ||||||
| Equivalised disposable household income 4 | $404/week | $775/week | ||||||
| Adjusted household income 5 | $808/week | $1550/week | ||||||
| Food Sub-Groups 1 | NRF 9.3/100 kcal | $/100 kcal | Nutrient Density-to-Cost Ratio 2 | Processing Level |
|---|---|---|---|---|
| Vegetables | ||||
| Other vegetables | 355.7 (162.8) | 1.3 (0.8) | 337.9 (179.9) | Unprocessed |
| Orange/yellow vegetables | 205.3 (88.1) | 0.9 (0.3) | 324.3 (335.0) | Unprocessed |
| Potatoes and red kumara, unprocessed | 96.4 (19.9) | 0.6 (0.3) | 196.1 (77.7) | Unprocessed |
| Vegetable dishes | 99.7 (90.8) | 0.6 (0.4) | 183.2 (192.9) | Ultra-processed |
| Fruit | ||||
| Fruit juices | 272.2 (105.8) | 0.7 (0.3) | 416.0 (102.7) | Processed |
| Fresh fruit | 116.6 (106.8) | 0.7 (0.4) | 159.1 (84.2) | Unprocessed |
| Dried fruit | 24.3 (4.2) | 0.2 (0.1) | 126.8 (46.0) | Unprocessed |
| Cereals and grain foods | ||||
| Hot porridge | 27.5 (9.8) | 0.2 (0.1) | 246.0 (153.6) | Unprocessed |
| Pasta and noodles | 14.2 (6.8) | 0.2 (0.2) | 180.9 (137.1) | Unprocessed |
| Breads and rolls, wholegrain, fortified | 19.4 (2.2) | 0.1 (0.0) | 150.5 (55.1) | Ultra-processed |
| Breakfast cereal, unfortified, sugars ≤15 g/100 g | 23.1 (0.0) | 0.2 (0.0) | 148.9 (3.5) | Ultra-processed |
| Breakfast cereal, fortified, sugars 15–30 g/100 g | 46.4 (19.8) | 0.3 (0.0) | 148.4 (58.4) | Ultra-processed |
| Rice and grains | 10.5 (6.3) | 0.1 (0.0) | 136.4 (70.3) | Unprocessed |
| Meat and alternatives | ||||
| Nuts and seeds | 35.5 (11.8) | 0.1 (0.0) | 303.6 (50.7) | Unprocessed |
| Other foods | ||||
| Oils | 2.9 (4.8) | 0.04 (0.0) | 138.5 (103.9) | Culinary processed |
| Discretionary foods | ||||
| Potatoes and red kumara, processed | 25.4 (10.3) | 0.2 (0.1) | 129.2 (81.4) | Ultra-processed |
| Current Diet 1 | Low SES Household | Medium SES Household | ||||
| Māori | Pacific | NZEO | Māori | Pacific | NZEO | |
| n | 391 | 420 | 133 | 116 | 66 | 190 |
| Total energy (kcal/day) | 7286.1 (111.5) | 7275.2 (103.4) | 6228.2 (126.4) | 6260.3 (159.6) | 6931.1 (236.3) | 6247.9 (130.5) |
| Food groups (servings/day) 2 | ||||||
| Vegetables (21.5 servings/day) | 7.0 (0.3) | 10.0 (0.4) | 6.6 (0.4) | 6.3 (0.5) | 9.2 (0.8) | 7.8 (0.4) |
| Fruit (8 servings/day) | 4.4 (0.2) | 5.5 (0.2) | 5.1 (0.3) | 6.6 (0.3) | 5.4 (0.4) | 5.9 (0.2) |
| Grains and cereals (22 servings/day) | 11.9 (0.4) | 15.5 (0.4) | 11.8 (0.5) | 10.9 (0.5) | 13.3 (0.9) | 14.4 (0.6) |
| Lean meats and alternatives (10 servings/day) | 5.5 (0.2) | 6.8 (0.2) | 3.9 (0.3) | 5.2 (0.4) | 5.5 (0.4) | 3.6 (0.2) |
| Dairy and alternatives (10.5 servings/day) | 3.1 (0.1) | 2.2 (0.1) | 3.5 (0.2) | 3.4 (0.2) | 2.7 (0.2) | 3.5 (0.1) |
| Discretionary foods (<11 servings/day) | 36.9 (0.8) | 31.6 (0.8) | 27.3 (0.9) | 27.4 (1.3) | 28.2 (1.6) | 23.9 (0.7) |
| Macronutrients (% of energy) 3 | ||||||
| Protein (15–25%) | 14.2 (0.2) | 14.9 (0.2) | 13.1 (0.3) | 13.2 (0.3) | 14.1 (0.4) | 13.1 (0.2) |
| Total fat (<35%) | 34.3 (0.3) | 31.5 (0.3) | 30.3 (0.4) | 31.6 (0.4) | 31.7 (0.7) | 28.7 (0.4) |
| Saturated fat (<10%) | 12.3 (0.1) | 11.0 (0.1) | 11.7 (0.2) | 11.7 (0.2) | 11.7 (0.3) | 11.2 (0.2) |
| Monounsaturated fat | 12.6 (0.1) | 11.6 (0.1) | 10.1 (0.2) | 11.0 (0.2) | 11.5 (0.3) | 9.6 (0.2) |
| Polyunsaturated fat | 5.5 (0.1) | 5.4 (0.1) | 5.1 (0.1) | 5.2 (0.1) | 5.0 (0.1) | 4.7 (0.1) |
| Total Carbohydrates (45–65%) | 49.7 (0.3) | 51.5 (0.3) | 54.6 (0.5) | 53.2 (0.5) | 52.3 (0.8) | 56.1 (0.4) |
| Total sugars | 20.0 (0.3) | 19.0 (0.3) | 24.4 (0.5) | 24.5 (0.6) | 20.1 (0.7) | 22.7 (0.4) |
| Added sugars (<10%) | 10.7 (0.2) | 8.8 (0.2) | 12.9 (0.4) | 12.0 (0.5) | 10.0 (0.5) | 11.2 (0.3) |
| Free sugars | 12.2 (0.2) | 10.2 (0.2) | 14.6 (0.5) | 14.4 (0.5) | 11.2 (0.5) | 13.0 (0.3) |
| Starch | 29.5 (0.3) | 32.3 (0.3) | 29.9 (0.5) | 28.5 (0.5) | 32.0 (0.8) | 33.2 (0.5) |
| Dietary fiber (g/day) 4 (100 g/day) | 67.6 (1.2) | 75.8 (1.2) | 65.9 (1.8) | 64.3 (1.7) | 70.8 (2.7) | 69.6 (1.5) |
| Cost and affordability | ||||||
| Cost of diet (NZD/week) | 191.0 (3.3) | 187.3 (2.9) | 155.7 (3.3) | 173.8 (6.0) | 184.9 (6.5) | 161.3 (3.5) |
| Diet affordability (%) 5 | 23.6 | 23.2 | 19.3 | 11.2 | 11.9 | 10.4 |
| Diet energy cost (NZD/100 kcal) | 2.7 (0.0) | 2.7 (0.0) | 2.6 (0.0) | 2.8 (0.1) | 2.7 (0.1) | 2.6 (0.0) |
| Total consumed food (g/day) | 5131.5 (72.1) | 5242.6 (71.7) | 4644.8 (94.8) | 4538.0 (98.3) | 5040.0 (168.4) | 4534.8 (77.8) |
| Healthier Modeled Diet 1,2 | Low SES Household | Medium SES Household | Statistical Comparisons (p-Value) 3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Current vs. Healthier Diet Low SES | Current vs. Healthier Diet Medium SES | |||||||||||
| Maori | Pacific | NZEO | Maori | Pacific | NZEO | Maori | Pacific | NZEO | Maori | Pacific | NZEO | |
| n | 391 | 420 | 133 | 116 | 66 | 190 | ||||||
| Total energy (kcal/day) | 7717.6 (131.2) | 7494.8 (105.7) | 6087.1 (131.8) | 6148.4 (165.8) | 6830.3 (232.7) | 6189.2 (125.8) | <0.011 | <0.001 | <0.001 | 0.030 | <0.001 | <0.001 |
| Food groups (servings/day) | ||||||||||||
| Vegetables (21.5 servings/day) | 14.9 (0.4) | 16.2 (0.4) | 13.7 (0.6) | 14.9 (0.8) | 16.7 (1.2) | 13.7 (0.5) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Fruit (8 servings/day) | 12.6 (0.3) | 13.9 (0.4) | 11.9 (0.4) | 13.4 (0.5) | 11.9 (0.5) | 11.4 (0.4) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Grains and cereals (22 servings/day) | 26.7 (0.6) | 28.1 (0.6) | 21.5 (0.6) | 19.9 (0.7) | 23.4 (1.0) | 23.6 (0.7) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Lean meats and alternatives (10 servings/day) | 8.0 (0.3) | 8.7 (0.2) | 5.4 (0.3) | 6.8 (0.4) | 7.6 (0.5) | 5.4 (0.2) | 0.001 | 0.017 | 0.061 | 0.869 | 0.017 | 0.694 |
| Dairy and alternatives (10.5 servings/day) | 5.4 (0.3) | 3.6 (0.2) | 5.1 (0.3) | 4.0 (0.2) | 4.1 (0.4) | 4.4 (0.2) | <0.001 | <0.001 | 0.001 | 0.113 | <0.001 | 0.010 |
| Discretionary foods (<11 servings/day) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Macronutrients (% of energy) | ||||||||||||
| Protein (15–25%) | 13.7 (0.1) | 13.2 (0.1) | 13.8 (0.2) | 13.1 (0.1) | 13.2 (0.2) | 13.7 (0.1) | <0.001 | <0.001 | 0.845 | 0.179 | 0.001 | 0.767 |
| Total fat (<35%) | 25.7 (0.4) | 25.8 (0.3) | 21.6 (0.5) | 22.9 (0.6) | 23.5 (0.8) | 20.7 (0.5) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Saturated fat (<10%) | 4.2 (0.1) | 4.2 (0.0) | 3.7 (0.1) | 3.8 (0.1) | 3.9 (0.1) | 3.6 (0.1) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Monounsaturated fat | 11.2 (0.2) | 11.4 (0.2) | 9.1 (0.3) | 9.9 (0.3) | 10.4 (0.4) | 8.8 (0.2) | <0.001 | <0.001 | <0.001 | 0.048 | <0.001 | 0.001 |
| Polyunsaturated fat | 8.7 (0.1) | 8.7 (0.1) | 7.3 (0.2) | 7.7 (0.2) | 7.8 (0.3) | 7.0 (0.2) | <0.001 | <0.001 | 0.012 | <0.001 | 0.007 | 0.001 |
| Total Carbohydrates (45–65%) | 56.4 (0.4) | 56.8 (0.3) | 60.4 (0.5) | 59.8 (0.6) | 59.2 (0.8) | 61.5 (0.5) | 0.358 | <0.001 | 0.714 | 0.036 | 0.578 | 0.913 |
| Total sugars | 23.1 (0.3) | 22.4 (0.3) | 25.9 (0.5) | 27.1 (0.7) | 22.3 (0.7) | 23.4 (0.4) | <0.001 | <0.001 | 0.019 | 0.003 | 0.001 | 0.010 |
| Added sugars (<10%) | 1.9 (0.1) | 1.9 (0.1) | 2.0 (0.1) | 1.7 (0.1) | 1.6 (0.1) | 1.9 (0.1) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Free sugars | 2.9 (0.1) | 2.7 (0.1) | 2.9 (0.1) | 3.7 (0.4) | 2.3 (0.2) | 2.9 (0.1) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Starch | 32.9 (0.4) | 34.1 (0.3) | 34.2 (0.5) | 32.4 (0.6) | 36.6 (0.9) | 37.8 (0.6) | <0.001 | <0.001 | 0.008 | 0.424 | <0.001 | 0.014 |
| Dietary fiber (g/day) (100 g/day) | 173.0 (3.1) | 169.9 (2.6) | 136.8 (3.2) | 141.8 (4.1) | 152.4 (5.9) | 137.4 (3.1) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Cost and affordability | ||||||||||||
| Cost of diet (NZD/week) | 138.9 (2.4) | 137.3 (2.2) | 120.3 (2.7) | 122.1 (3.5) | 133.0 (5.2) | 116.3 (2.3) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Diet affordability (%) 4 | 17.2 | 17.0 | 14.9 | 7.9 | 8.6 | 7.5 | ||||||
| Diet energy cost (NZD/100 kcal) | 2.0 (0.0) | 1.9 (0.0) | 2.1 (0.0) | 2.1 (0.0) | 2.0 (0.0) | 2.0 (0.0) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Total consumed food (g/day) | 5736.4.1 (120.1) | 5661.1 (96.4) | 5153.7 (122.4) | 4891.1 (140.7) | 5535.5 (220.5) | 4961.3 (98.6) | <0.001 | 0.001 | 0.007 | 0.076 | 0.202 | 0.003 |
| Category Distribution 1 | Low SES Household | Medium SES Household | Statistical Comparisons (p-Value) 2 | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Māori | Pacific | NZEO | Māori | Pacific | NZEO | Current vs. Healthier Diet Low SES | Current vs. Healthier Diet Medium SES | |||||||||||
| C | H | C | H | C | H | C | H | C | H | C | H | M | P | N | M | P | N | |
| Unprocessed | 27.7% (1.1) | 65.5% (1.3) | 35.7% (1.2) | 65.1% (1.2) | 31.4% (2.3) | 66.7% (2.3) | 29.0% (2.1) | 65.7% (2.1) | 34.9% (2.7) | 71.4% (2.9) | 33.2% (1.8) | 67.8% (1.6) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Potatoes and red kumara | 13.2% (1.3) | 13.0% (1.0) | 13.7% (1.2) | 11.6% (0.9) | 9.4% (1.9) | 7.5% (1.3) | 11.8% (2.1) | 13.1% (1.7) | 19.7% (3.4) | 17.0% (2.5) | 12.1% (1.9) | 10.7% (1.3) | 0.816 | 0.047 | 0.317 | 0.360 | 0.332 | 0.576 |
| Orange/yellow vegetables | 1.8% (0.4) | 4.6% (0.5) | 0.9% (0.2) | 4.2% (0.5) | 3.0% (0.8) | 5.6% (1.1) | 1.2% (0.4) | 6.0% (1.4) | 1.4% (0.8) | 4.6% (1.6) | 2.5% (0.6) | 3.8% (0.6) | <0.001 | <0.001 | 0.015 | <0.001 | 0.028 | 0.232 |
| Green leafy vegetables | 1.3% (0.4) | 0.0% (0.0) | 0.8% (0.3) | 0.0% (0.0) | 0.6% (0.3) | 0.0% (0.0) | 0.8% (0.4) | 0.0% (0.0) | 0.7% (0.4) | 0.0% (0.0) | 0.9% (0.3) | 0.0% (0.0) | <0.001 | 0.010 | 0.313 | 0.215 | 0.424 | 0.066 |
| Other vegetables | 6.1% (0.9) | 6.8% (0.7) | 11.7% (1.2) | 9.8% (0.8) | 8.4% (1.7) | 7.5% (1.3) | 4.8% (1.0) | 6.2% (1.0) | 5.6% (1.6) | 5.8% (1.1) | 7.8% (1.1) | 8.5% (1.1) | 0.354 | 0.040 | 0.849 | 0.332 | 0.893 | 0.480 |
| Fresh fruit | 19.7% (1.5) | 17.3% (1.0) | 19.8% (1.3) | 20.2% (1.1) | 23.9% (3.2) | 22.7% (2.5) | 26.8% (3.0) | 20.8% (2.1) | 27.0% (3.8) | 21.4% (2.8) | 25.0% (2.6) | 17.6% (1.5) | 0.144 | 0.816 | 0.616 | 0.034 | 0.095 | <0.001 |
| Dried fruit | 0.4% (0.4) | 10.0% (0.9) | 0.0% (0.0) | 8.7% (0.9) | 1.5% (0.9) | 9.9% (1.5) | 1.7% (0.8) | 12.6% (1.9) | 0.2% (0.2) | 5.0% (1.4) | 0.6% (0.3) | 9.0% (1.3) | <0.001 | <0.001 | <0.001 | <0.001 | 0.032 | <0.001 |
| Rice and grains | 3.3% (0.7) | 5.1% (0.7) | 11.3% (1.1) | 9.1% (0.8) | 12.2% (2.2) | 10.7% (1.4) | 1.4% (0.7) | 6.1% (1.4) | 11.4% (3.6) | 9.4% (2.3) | 11.6% (2.1) | 13.8% (1.8) | 0.052 | 0.009 | 0.626 | 0.009 | 0.484 | 0.075 |
| Pasta, plain | 1.0% (0.5) | 4.8% (0.7) | 0.7% (0.3) | 4.2% (0.7) | 2.5% (1.0) | 3.0% (0.7) | 1.2% (0.7) | 2.5% (0.8) | 0.3% (0.3) | 7.5% (2.0) | 3.0% (1.5) | 4.8% (1.0) | <0.001 | <0.001 | 0.997 | 0.410 | <0.001 | 0.180 |
| Hot porridge | 1.3% (0.4) | 7.4% (0.9) | 0.8% (0.3) | 4.4% (0.6) | 1.7% (1.4) | 6.0% (1.3) | 0.5% (0.4) | 6.5% (1.4) | 0.6% (0.6) | 4.8% (1.8) | 1.0% (0.5) | 6.0% (1.0) | <0.001 | <0.001 | 0.001 | <0.001 | 0.132 | <0.001 |
| Dairy milk full/reduced fat | 22.4% (1.7) | 0.0% (0.0) | 12.4% (1.1) | 0.0% (0.0) | 15.2% (2.4) | 0.0% (0.0) | 22.3% (3.1) | 0.0% (0.0) | 14.0% (2.8) | 0.0% (0.0) | 16.1% (2.1) | 0.0% (0.0) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Dairy milk skim | 0.7% (0.3) | 11.4% (0.8) | 0.9% (0.4) | 8.6% (0.5) | 2.1% (0.8) | 12.8% (1.2) | 1.1% (0.5) | 10.7% (1.2) | 0.2% (0.1) | 9.6% (2.1) | 2.6% (0.9) | 11.8% (1.0) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Yoghurt full fat | 1.1% (0.3) | 0.0% (0.0) | 1.2% (0.3) | 0.0% (0.0) | 0.5% (0.2) | 0.0% (0.0) | 2.5% (0.9) | 0.0% (0.0) | 0.2% (0.1) | 0.0% (0.0) | 1.3% (0.5) | 0.0% (0.0) | 0.008 | 0.002 | 0.500 | <0.001 | 0.888 | 0.037 |
| Nuts and seeds | 1.6% (0.4) | 19.5% (1.2) | 2.2% (0.4) | 19.0% (0.9) | 3.0% (1.1) | 14.2% (1.7) | 3.0% (1.2) | 15.5% (1.6) | 0.6% (0.3) | 14.8% (1.7) | 2.6% (0.6) | 14.0% (1.2) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Fish, meat, eggs and poultry | 26.1% (1.7) | 0.0% (0.0) | 23.7% (1.3) | 0.0% (0.0) | 15.9% (2.2) | 0.0% (0.0) | 20.8% (2.7) | 0.0% (0.0) | 18.1% (3.0) | 0.0% (0.0) | 12.8% (1.7) | 0.0% (0.0) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Processed culinary | 5.7% (0.5) | 5.4% (0.4) | 5.5% (0.4) | 5.3% (0.4) | 3.9% (0.5) | 3.8% (0.5) | 4.8% (0.8) | 4.4% (0.7) | 4.6% (0.9) | 4.6% (0.9) | 2.9% (0.4) | 2.7% (0.4) | <0.001 | 0.085 | 0.388 | <0.001 | 1.000 | 0.060 |
| Margarine | 65.8% (3.4) | 0.0% (0.0) | 68.6% (3.2) | 0.0% (0.0) | 68.3% (6.7) | 0.0% (0.0) | 64.1% (7.1) | 0.0% (0.0) | 75.4% (7.9) | 0.0% (0.0) | 69.8% (6.2) | 0.0% (0.0) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Oils | 0.5% (0.3) | 100.0% (0.0) | 0.9% (0.7) | 100.0% (0.0) | 5.2% (2.9) | 100.0% (0.0) | 1.9% (1.9) | 100.0% (0.0) | 2.8% (2.8) | 100.0% (0.0) | 1.1% (1.1) | 100.0% (0.0) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Discretionary fats | 33.6% (3.4) | 0.0% (0.0) | 30.5% (3.2) | 0.0% (0.0) | 26.6% (6.2) | 0.0% (0.0) | 34.0% (7.0) | 0.0% (0.0) | 21.8% (7.5) | 0.0% (0.0) | 29.1% (6.2) | 0.0% (0.0) | <0.001 | <0.001 | <0.001 | <0.001 | 0.013 | <0.001 |
| Processed | 2.8% (0.4) | 2.9% (0.2) | 3.8% (0.5) | 2.2% (0.2) | 4.3% (0.8) | 2.5% (0.3) | 5.2% (1.1) | 3.9% (1.0) | 3.8% (1.1) | 2.2% (0.4) | 5.6% (0.7) | 2.7% (0.3) | 0.995 | 0.002 | 0.087 | 0.232 | 0.245 | <0.001 |
| Fruit juices | 49.5% (5.3) | 100.0% (0.0) | 34.6% (4.7) | 100.0% (0.0) | 36.8% (7.5) | 100.0% (0.0) | 46.3% (8.4) | 100.0% (0.0) | 18.2% (9.3) | 100.0% (0.0) | 48.0% (5.8) | 100.0% (0.0) | 0.003 | <0.001 | <0.001 | 0.034 | <0.001 | <0.001 |
| Processed fruit | 4.2% (2.2) | 0.0% (0.0) | 0.7% (0.6) | 0.0% (0.0) | 2.7% (2.1) | 0.0% (0.0) | 2.8% (2.8) | 0.0% (0.0) | 0.0% (0.0) | 0.0% (0.0) | 3.8% (1.8) | 0.0% (0.0) | <0.001 | 0.263 | 0.373 | 0.156 | 1.000 | 0.439 |
| Cheese | 11.4% (3.5) | 0.0% (0.0) | 11.4% (3.0) | 0.0% (0.0) | 24.1% (6.4) | 0.0% (0.0) | 19.3% (6.5) | 0.0% (0.0) | 16.8% (9.0) | 0.0% (0.0) | 24.5% (5.2) | 0.0% (0.0) | <0.001 | <0.001 | <0.001 | 0.002 | 0.036 | <0.001 |
| Processed fish and meat alternatives | 8.3% (2.8) | 0.0% (0.0) | 18.3% (3.9) | 0.0% (0.0) | 21.9% (6.2) | 0.0% (0.0) | 4.1% (2.5) | 0.0% (0.0) | 20.8% (9.3) | 0.0% (0.0) | 9.7% (2.5) | 0.0% (0.0) | 0.748 | 0.002 | <0.001 | 0.906 | 0.470 | 0.024 |
| Processed meats | 26.7% (4.8) | 0.0% (0.0) | 35.0% (4.5) | 0.0% (0.0) | 14.6% (5.3) | 0.0% (0.0) | 27.5% (7.5) | 0.0% (0.0) | 44.1% (10.6) | 0.0% (0.0) | 14.0% (3.8) | 0.0% (0.0) | 0.007 | <0.001 | 0.324 | 0.087 | <0.001 | 0.195 |
| Ultra-processed | 63.7% (1.2) | 26.2% (1.1) | 55.1% (1.2) | 27.4% (1.1) | 60.5% (2.2) | 27.0% (2.1) | 61.0% (2.2) | 26.0% (1.9) | 56.7% (2.7) | 21.8% (2.6) | 58.3% (1.7) | 26.7% (1.6) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Vegetable dishes | 2.6% (0.4) | 18.3% (1.6) | 2.0% (0.4) | 14.7% (1.6) | 4.5% (1.1) | 19.6% (3.1) | 3.5% (1.0) | 14.7% (2.3) | 0.7% (0.5) | 8.1% (2.8) | 4.7% (0.9) | 20.9% (2.5) | <0.001 | <0.001 | <0.001 | <0.001 | 0.071 | <0.001 |
| Ultra-processed fruit | 0.3% (0.1) | 0.0% (0.0) | 0.1% (0.0) | 0.0% (0.0) | 1.0% (0.5) | 0.0% (0.0) | 0.5% (0.3) | 0.0% (0.0) | 1.5% (0.7) | 0.0% (0.0) | 0.3% (0.1) | 0.0% (0.0) | 0.233 | 0.544 | 0.003 | 0.081 | 0.008 | 0.271 |
| Cereal, fortified, sugars 15–30 g/100 g | 0.4% (0.2) | 16.7% (1.7) | 0.9% (0.4) | 17.2% (1.7) | 0.8% (0.4) | 19.7% (3.6) | 1.0% (0.6) | 19.0% (3.4) | 1.7% (1.2) | 20.6% (4.4) | 1.0% (0.5) | 16.9% (2.8) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Cereal, unfortified, sugars <15 g/100 g | 0.1% (0.1) | 13.4% (1.6) | 0.0% (0.0) | 12.3% (1.5) | 0.3% (0.2) | 10.8% (2.7) | 0.1% (0.1) | 16.2% (3.0) | 0.3% (0.3) | 19.7% (4.6) | 0.1% (0.1) | 21.5% (3.2) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Wholegrain bread, fortified | 2.7% (0.7) | 51.6% (2.3) | 2.8% (0.6) | 55.8% (2.3) | 3.8% (0.8) | 49.9% (4.3) | 4.3% (1.3) | 50.1% (4.0) | 4.8% (1.8) | 51.7% (5.3) | 5.6% (1.1) | 40.7% (3.3) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Cereal, fortified, sugars <15 g/100 g | 6.5% (0.7) | 0.0% (0.0) | 6.5% (0.8) | 0.0% (0.0) | 4.8% (1.2) | 0.0% (0.0) | 7.9% (1.2) | 0.0% (0.0) | 7.3% (2.2) | 0.0% (0.0) | 9.2% (1.6) | 0.0% (0.0) | <0.001 | <0.001 | <0.001 | <0.001 | 0.001 | <0.001 |
| Wholegrain bread, unfortified | 0.6% (0.2) | 0.0% (0.0) | 1.5% (0.5) | 0.0% (0.0) | 0.4% (0.3) | 0.0% (0.0) | 0.3% (0.3) | 0.0% (0.0) | 0.0% (0.0) | 0.0% (0.0) | 0.5% (0.2) | 0.0% (0.0) | 0.132 | <0.001 | 0.616 | 0.707 | 1.000 | 0.413 |
| Refined bread | 13.8% (1.2) | 0.0% (0.0) | 17.6% (1.3) | 0.0% (0.0) | 10.7% (2.0) | 0.0% (0.0) | 11.5% (1.8) | 0.0% (0.0) | 11.9% (2.7) | 0.0% (0.0) | 8.6% (1.4) | 0.0% (0.0) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Cereal, unfortified, sugars >15–30 g/100 g | 0.2% (0.1) | 0.0% (0.0) | 0.2% (0.2) | 0.0% (0.0) | 0.7% (0.4) | 0.0% (0.0) | 0.0% (0.0) | 0.0% (0.0) | 0.3% (0.3) | 0.0% (0.0) | 0.9% (0.4) | 0.0% (0.0) | 0.317 | 0.402 | 0.095 | 1.000 | 0.656 | 0.043 |
| Batter-based products | 0.6% (0.2) | 0.0% (0.0) | 1.2% (0.3) | 0.0% (0.0) | 0.7% (0.5) | 0.0% (0.0) | 0.2% (0.1) | 0.0% (0.0) | 1.2% (0.9) | 0.0% (0.0) | 0.7% (0.3) | 0.0% (0.0) | 0.051 | <0.001 | 0.231 | 0.795 | 0.073 | 0.094 |
| Pasta, with additions | 2.0% (0.4) | 0.0% (0.0) | 0.9% (0.3) | 0.0% (0.0) | 1.6% (0.6) | 0.0% (0.0) | 2.0% (1.1) | 0.0% (0.0) | 2.7% (1.4) | 0.0% (0.0) | 2.2% (0.6) | 0.0% (0.0) | <0.001 | 0.133 | 0.068 | 0.100 | 0.038 | <0.001 |
| Liquid/fortified breakfast | 0.3% (0.1) | 0.0% (0.0) | 0.5% (0.3) | 0.0% (0.0) | 0.4% (0.2) | 0.0% (0.0) | 0.6% (0.2) | 0.0% (0.0) | 0.7% (0.4) | 0.0% (0.0) | 0.6% (0.2) | 0.0% (0.0) | 0.080 | 0.003 | 0.324 | 0.125 | 0.132 | 0.095 |
| Yoghurt reduced fat | 0.4% (0.1) | 0.0% (0.0) | 0.3% (0.2) | 0.0% (0.0) | 0.5% (0.2) | 0.0% (0.0) | 0.4% (0.2) | 0.0% (0.0) | 0.6% (0.5) | 0.0% (0.0) | 0.7% (0.2) | 0.0% (0.0) | 0.040 | 0.084 | 0.186 | 0.628 | 0.094 | 0.004 |
| Flavored milk | 0.5% (0.2) | 0.0% (0.0) | 0.0% (0.0) | 0.0% (0.0) | 0.3% (0.2) | 0.0% (0.0) | 0.4% (0.3) | 0.0% (0.0) | 0.0% (0.0) | 0.0% (0.0) | 0.5% (0.2) | 0.0% (0.0) | <0.001 | 0.841 | 0.590 | 0.100 | 1.000 | 0.007 |
| Dairy milk substitutes | 0.0% (0.0) | 0.0% (0.0) | 0.0% (0.0) | 0.0% (0.0) | 0.2% (0.1) | 0.0% (0.0) | 0.0% (0.0) | 0.0% (0.0) | 0.4% (0.3) | 0.0% (0.0) | 0.5% (0.4) | 0.0% (0.0) | 0.953 | 1.000 | 0.808 | 1.000 | 0.297 | 0.038 |
| Cheese, ultra-processed | 0.0% (0.0) | 0.0% (0.0) | 0.1% (0.0) | 0.0% (0.0) | 0.0% (0.0) | 0.0% (0.0) | 0.0% (0.0) | 0.0% (0.0) | 0.0% (0.0) | 0.0% (0.0) | 0.0% (0.0) | 0.0% (0.0) | 0.599 | 0.037 | 1.000 | 1.000 | 1.000 | 0.448 |
| Discretionary | 69.0% (1.5) | 0.0% (0.0) | 65.6% (1.6) | 0.0% (0.0) | 69.5% (2.6) | 0.0% (0.0) | 67.3% (2.3) | 0.0% (0.0) | 66.1% (4.0) | 0.0% (0.0) | 63.7% (2.3) | 0.0% (0.0) | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Starck, C.S.; Blumfield, M.; Keighley, T.; Marshall, S.; Petocz, P.; Inan-Eroglu, E.; Abbott, K.; Cassettari, T.; Ali, A.; Wham, C.; et al. Nutrient Dense, Low-Cost Foods Can Improve the Affordability and Quality of the New Zealand Diet—A Substitution Modeling Study. Int. J. Environ. Res. Public Health 2021, 18, 7950. https://doi.org/10.3390/ijerph18157950
Starck CS, Blumfield M, Keighley T, Marshall S, Petocz P, Inan-Eroglu E, Abbott K, Cassettari T, Ali A, Wham C, et al. Nutrient Dense, Low-Cost Foods Can Improve the Affordability and Quality of the New Zealand Diet—A Substitution Modeling Study. International Journal of Environmental Research and Public Health. 2021; 18(15):7950. https://doi.org/10.3390/ijerph18157950
Chicago/Turabian StyleStarck, Carlene S., Michelle Blumfield, Tim Keighley, Skye Marshall, Peter Petocz, Elif Inan-Eroglu, Kylie Abbott, Tim Cassettari, Ajmol Ali, Carol Wham, and et al. 2021. "Nutrient Dense, Low-Cost Foods Can Improve the Affordability and Quality of the New Zealand Diet—A Substitution Modeling Study" International Journal of Environmental Research and Public Health 18, no. 15: 7950. https://doi.org/10.3390/ijerph18157950
APA StyleStarck, C. S., Blumfield, M., Keighley, T., Marshall, S., Petocz, P., Inan-Eroglu, E., Abbott, K., Cassettari, T., Ali, A., Wham, C., Kruger, R., Kira, G., & Fayet-Moore, F. (2021). Nutrient Dense, Low-Cost Foods Can Improve the Affordability and Quality of the New Zealand Diet—A Substitution Modeling Study. International Journal of Environmental Research and Public Health, 18(15), 7950. https://doi.org/10.3390/ijerph18157950









