Acute and Delayed Effects of Time-Matched Very Short “All Out” Efforts in Concentric vs. Eccentric Cycling
Abstract
:1. Introduction
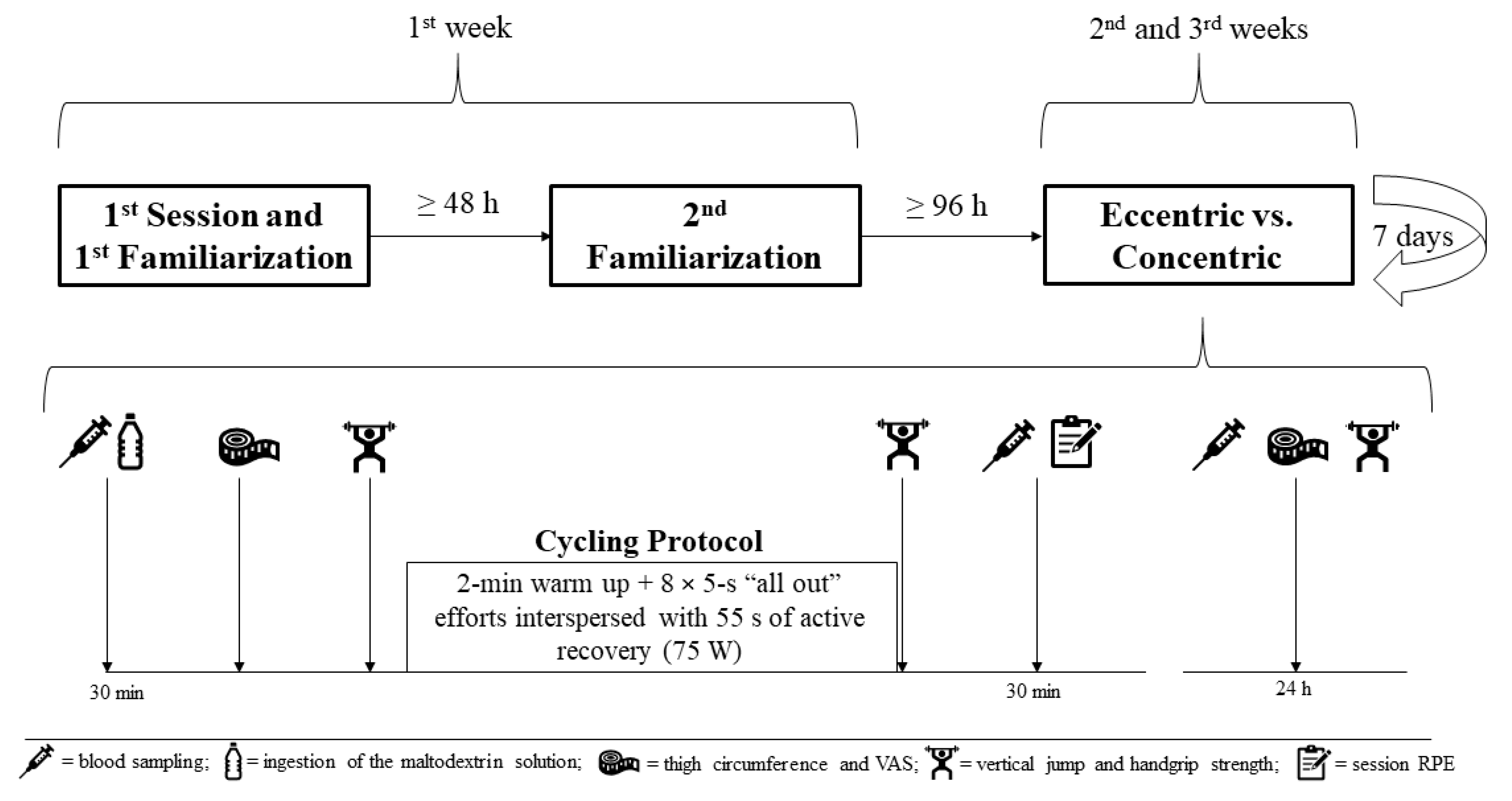
2. Materials and Methods
3. Results
3.1. Graded Exercise Test
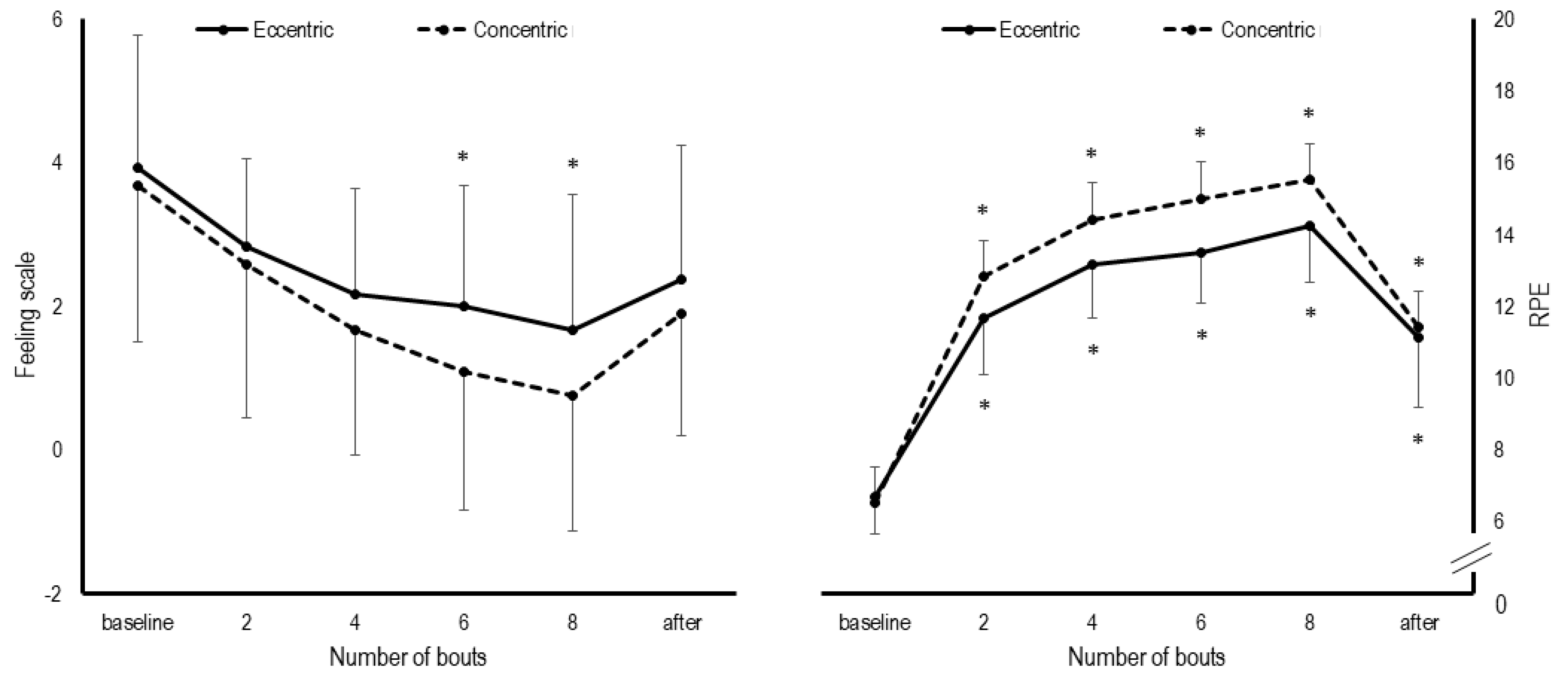
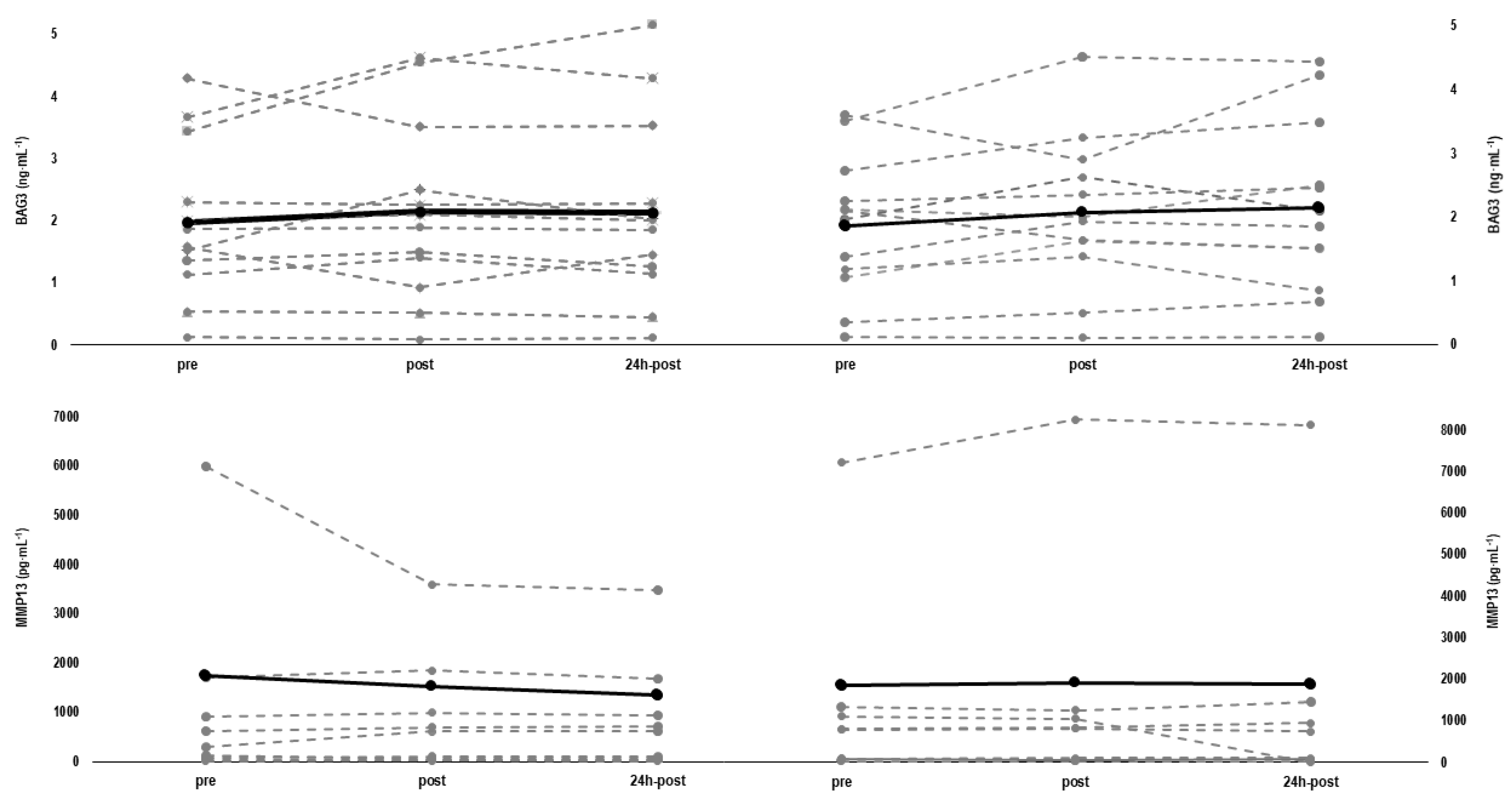
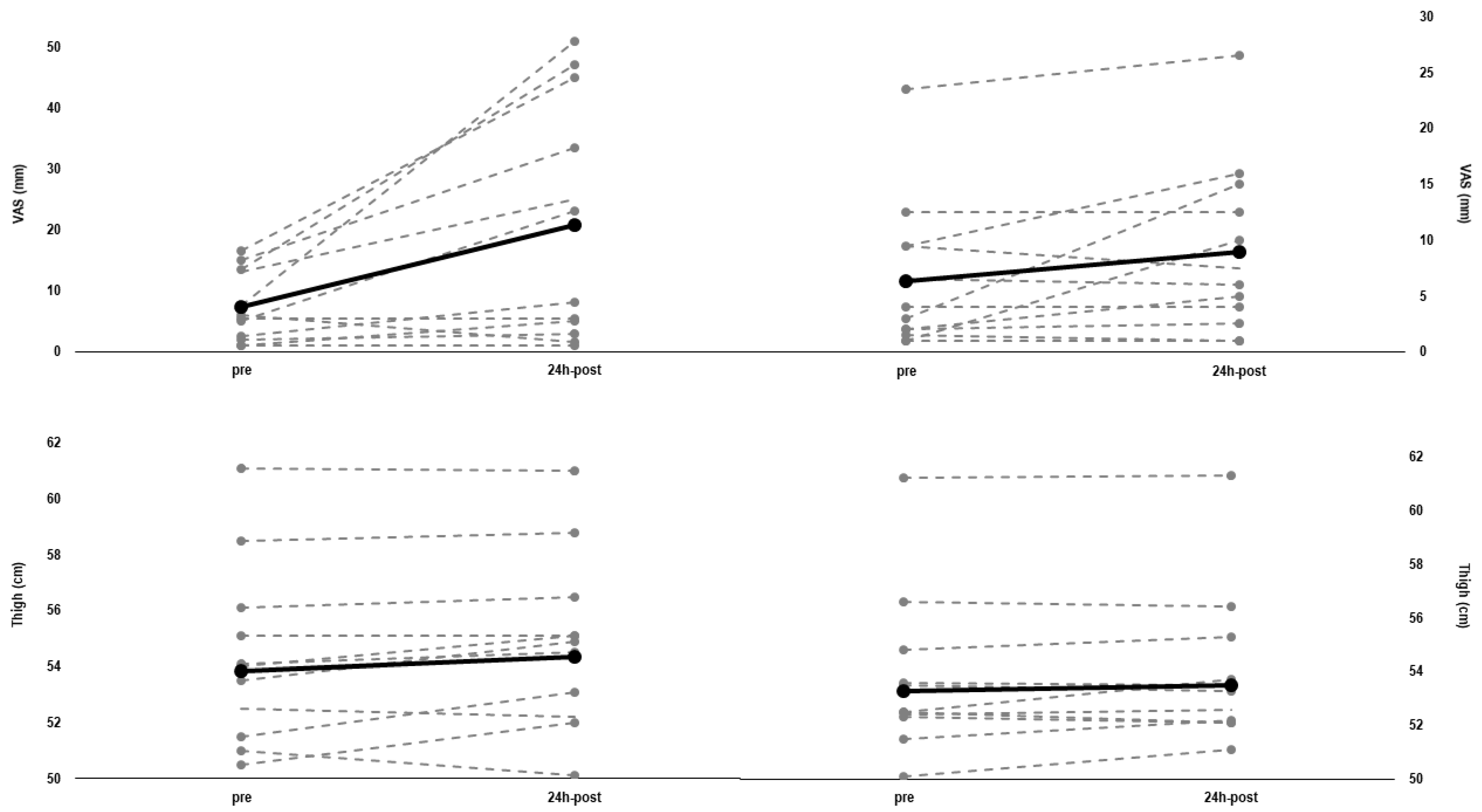
3.2. Comparisons between Protocols
3.3. Relationships between Parameters
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- MacInnis, M.J.; Gibala, M.J. Physiological adaptations to interval training and the role of exercise intensity. J. Physiol. 2017, 595, 2915–2930. [Google Scholar] [CrossRef] [Green Version]
- Burgomaster, K.A.; Hughes, S.C.; Heigenhauser, G.J.; Bradwell, S.N.; Gibala, M.J. Six sessions of sprint interval training increases muscle oxidative potential and cycle endurance capacity in humans. J. Appl. Physiol. 2005, 98, 1985–1990. [Google Scholar] [CrossRef]
- Vollaard, N.; Metcalfe, R.; Williams, S. Effect of number of sprints in an SIT session on change in VO2max: A meta-analysis. Med. Sci. Sports Exerc. 2017, 49, 1147–1156. [Google Scholar] [CrossRef]
- Biddle, S.J.; Batterham, A.M. High-intensity interval exercise training for public health: A big HIT or shall we HIT it on the head? Int. J. Behav. Nutr. Phys. Act. 2015, 12, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Saanijoki, T.; Nummenmaa, L.; Eskelinen, J.J.; Savolainen, A.M.; Vahlberg, T.; Kalliokoski, K.K.; Hannukainen, J.C. Affective Responses to Repeated Sessions of High-Intensity Interval Training. Med. Sci. Sports Exerc. 2015, 47, 2604–2611. [Google Scholar] [CrossRef]
- Vollaard, N.B.; Metcalfe, R.S. Research into the Health Benefits of Sprint Interval Training Should Focus on Protocols with Fewer and Shorter Sprints. Sport. Med. 2017, 47, 2443–2451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McKie, G.L.; Islam, H.; Townsend, L.K.; Robertson-Wilson, J.; Eys, M.; Hazell, T.J. Modified sprint interval training protocols: Physiological and psychological responses to 4 weeks of training. Appl. Physiol. Nutr. Metab. 2018, 43, 595–601. [Google Scholar] [CrossRef]
- Peñailillo, L.; Blazevich, A.J.; Nosaka, K. Factors contributing to lower metabolic demand of eccentric compared with concentric cycling. J. Appl. Physiol. 2017, 123, 884–893. [Google Scholar] [CrossRef]
- Ritter, O.; Isacco, L.; Rakobowchuk, M.; Tordi, N.; Laroche, D.; Bouhaddi, M.; Degano, B.; Mourot, L. Cardiorespiratory and Autonomic Nervous System Responses to Prolonged Eccentric Cycling. Int. J. Sports Med. 2019, 40, 453–461. [Google Scholar] [CrossRef]
- Brughelli, M.; Van Leemputte, M. Reliability of Power Output During Eccentric Sprint Cycling. J. Strength Cond. Res. 2013, 27, 76–82. [Google Scholar] [CrossRef]
- Lipski, M.; Abbiss, C.R.; Nosaka, K. Oxygen consumption, rate of perceived exertion and enjoyment in high-intensity interval eccentric cycling. Eur. J. Sport Sci. 2018, 18, 1390–1397. [Google Scholar] [CrossRef]
- Mavropalias, G.; Koeda, T.; Barley, O.R.; Poon, W.C.K.; Fisher, A.J.; Blazevich, A.J.; Nosaka, K. Comparison between high- and low-intensity eccentric cycling of equal mechanical work for muscle damage and the repeated bout effect. Eur. J. Appl. Physiol. 2020, 120, 1015–1025. [Google Scholar] [CrossRef]
- Barreto, R.V.; de Lima, L.C.R.; Denadai, B.S. Moving forward with backward pedaling: a review on eccentric cycling. Eur. J. Appl. Physiol. 2021, 121, 381–407. [Google Scholar] [CrossRef]
- Hody, S.; Croisier, J.L.; Bury, T.; Rogister, B.; Leprince, P. Eccentric muscle contractions: Risks and benefits. Front. Physiol. 2019, 10, 536. [Google Scholar] [CrossRef]
- Margaritelis, N.V.; Theodorou, A.A.; Chatzinikolaou, P.N.; Kyparos, A.; Nikolaidis, M.G.; Paschalis, V. Eccentric exercise per se does not affect muscle damage biomarkers: Early and late phase adaptations. Eur. J. Appl. Physiol. 2020, 121, 549–559. [Google Scholar] [CrossRef] [PubMed]
- Iguchi, M.; Shields, R.K. Quadriceps low-frequency fatigue and muscle pain are contraction-type-dependent. Muscle Nerve 2010, 42, 230–238. [Google Scholar] [CrossRef] [PubMed]
- Hill, E.C.; Housh, T.J.; Smith, C.M.; Keller, J.L.; Schmidt, R.J.; Johnson, G.O. Eccentric and concentric blood flow restriction resistance training on indices of delayed onset muscle soreness in untrained women. Eur. J. Appl. Physiol. 2019, 119, 2363–2373. [Google Scholar] [CrossRef]
- Penailillo, L.; Santander, M.; Zbinden-Foncea, H.; Jannas-Vela, S. Metabolic Demand and Indirect Markers of Muscle Damage after Eccentric Cycling with Blood Flow Restriction. Res. Q. Exerc. Sport 2020, 91, 705–712. [Google Scholar] [CrossRef]
- Chen, T.C.; Huang, G.L.; Hsieh, C.C.; Tseng, K.W.; Tseng, W.C.; Chou, T.Y.; Nosaka, K. Comparison among three different intensities of eccentric contractions of the elbow flexors resulting in the same strength loss at one day post-exercise for changes in indirect muscle damage markers. Eur. J. Appl. Physiol. 2020, 120, 267–279. [Google Scholar] [CrossRef]
- Nishikawa, K.C.; Lindstedt, S.L.; LaStayo, P.C. Basic science and clinical use of eccentric contractions: History and uncertainties. J. Sport Health Sci. 2018, 7, 265–274. [Google Scholar] [CrossRef]
- Sonkodi, B.; Berkes, I.; Koltai, E. Have We Looked in the Wrong Direction for More Than 100 Years? Delayed Onset Muscle Soreness Is, in Fact, Neural Microdamage Rather Than Muscle Damage. Antioxidants 2020, 9, 212. [Google Scholar] [CrossRef] [Green Version]
- Morawetz, D.; Blank, C.; Koller, A.; Arvandi, M.; Siebert, U.; Schobersberger, W. Sex-Related Differences After a Single Bout of Maximal Eccentric Exercise in Response to Acute Effects: A Systematic Review and Meta-analysis. J. Strength Cond. Res. 2020, 34, 2697–2707. [Google Scholar] [CrossRef]
- Lei, H.; Leong, D.; Smith, L.R.; Barton, E.R. Matrix metalloproteinase 13 is a new contributor to skeletal muscle regeneration and critical for myoblast migration. Am. J. Physiol. Physiol. 2013, 305, C529–C538. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marzullo, L.; Turco, M.C.; De Marco, M. The multiple activities of BAG3 protein: Mechanisms. Biochim. Biophys. Acta Gen. Subj. 2020, 1864, 129628. [Google Scholar] [CrossRef]
- Ulbricht, A.; Gehlert, S.; Leciejewski, B.; Schiffer, T.; Bloch, W.; Höhfeld, J. Induction and adaptation of chaperone-assisted selective autophagy CASA in response to resistance exercise in human skeletal muscle. Autophagy 2015, 11, 538–546. [Google Scholar] [CrossRef] [Green Version]
- Green, D.J.; Thomas, K.; Ross, E.Z.; Green, S.C.; Pringle, J.S.; Howatson, G. Torque, power and muscle activation of eccentric and concentric isokinetic cycling. J. Electromyogr. Kinesiol. 2018, 40, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, H.; Monahan, K.D.; Seals, D.R. Age-predicted maximal heart rate revisited. J. Am. Coll. Cardiol. 2001, 37, 153–156. [Google Scholar] [CrossRef] [Green Version]
- Benítez-Flores, S.; de Sousa, A.F.M.; da Cunha Totó, E.C.; Rosa, T.S.; Del Rosso, S.; Foster, C.; Boullosa, D. Shorter sprints elicit greater cardiorespiratory and mechanical responses with less fatigue during time-matched sprint interval training (SIT) sessions. Kinesiology 2018, 50, 137–148. [Google Scholar] [CrossRef]
- Scherr, J.; Wolfarth, B.; Christle, J.W.; Pressler, A.; Wagenpfeil, S.; Halle, M. Associations between Borg’s rating of perceived exertion and physiological measures of exercise intensity. Eur. J. Appl. Physiol. 2013, 113, 147–155. [Google Scholar] [CrossRef]
- Hardy, C.J.; Rejeski, W.J. Not What, but How One Feels: The Measurement of Affect during Exercise. J. Sport Exerc. Psychol. 1989, 11, 304–317. [Google Scholar] [CrossRef]
- Foster, C.; Florhaug, J.A.; Franklin, J.; Gottschall, L.; Hrovatin, L.A.; Parker, S.; Doleshal, P.; Dodge, C. A New Approach to Monitoring Exercise Training. J. Strength Cond. Res. 2001, 15, 109–115. [Google Scholar] [CrossRef]
- Boullosa, D.; Abreu, L.; de Conceição, F.A.; Cordero, Y.C.; Jimenez-Reyes, P. The influence of training background on different rate of force calculations during countermovement jump. Kinesiology 2018, 50, 90–95. [Google Scholar]
- Cronin, J.; Lawton, T.; Harris, N.; Kilding, A.; McMaster, D.T. A brief review of handgrip strength and sport performance. J. Strength Cond. Res. 2017, 31, 3187–3217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coren, S. The lateral preference inventory for measurement of handedness, footedness, eyedness, and earedness: Norms for young adults. Bull. Psychon. Soc. 1993, 31, 1–3. [Google Scholar] [CrossRef]
- Lau, W.Y.; Muthalib, M.; Nosaka, K. Visual analog scale and pressure pain threshold for delayed onset muscle soreness assessment. J. Musculoskelet. Pain 2013, 21, 320–326. [Google Scholar] [CrossRef]
- Benítez-Flores, S.; Medeiros, A.R.; Voltarelli, F.A.; Iglesias-Soler, E.; Doma, K.; Simões, H.G.; Rosa, T.S.; Boullosa, D.A. Combined effects of very short “all out” efforts during sprint and resistance training on physical and physiological adaptations after 2 weeks of training. Eur. J. Appl. Physiol. 2019, 119, 1337–1351. [Google Scholar] [CrossRef]
- McDaniel, J.; Behjani, N.S.; Elmer, S.J.; Brown, N.A.; Martin, J.C. Joint-Specific Power-Pedaling Rate Relationships During Maximal Cycling. J. Appl. Biomech. 2014, 30, 423–430. [Google Scholar] [CrossRef]
- Kordi, M.; Folland, J.; Goodall, S.; Barratt, P.; Howatson, G. Isovelocity vs. Isoinertial Sprint Cycling Tests for Power- and Torque-cadence Relationships. Int. J. Sports Med. 2019, 40, 897–902. [Google Scholar] [CrossRef]
- Rodger, S.M.; Plews, D.J.; Mcquillan, J.; Driller, M.W. Evaluation of the Cyclus ergometer and the Stages power meter against the SRM crankset for measurement of power output in cycling. J. Sci. Cycl. 2016, 5, 16–22. [Google Scholar]
- Foster, C.; Boullosa, D.; McGuigan, M.; Fusco, A.; Cortis, C.; Arney, B.E.; Orton, B.; Dodge, C.; Jaime, S.; Radtke, K.; et al. 25 Years of Session Rating of Perceived Exertion: Historical Perspective and Development. Int. J. Sports Physiol. Perform. 2021, 16, 612–621. [Google Scholar] [CrossRef] [PubMed]
- Peñailillo, L.; Blazevich, A.; Numazawa, H.; Nosaka, K. Rate of force development as a measure of muscle damage. Scand. J. Med. Sci. Sports 2015, 25, 417–427. [Google Scholar] [CrossRef]
- Boullosa, D.; Del Rosso, S.; Behm, D.G.; Foster, C. Post-activation potentiation (PAP) in endurance sports: A review. Eur. J. Sport Sci. 2018, 18, 595–610. [Google Scholar] [CrossRef]
- Boullosa, D.A.; Tuimil, J.L.; Alegre, L.M.; Iglesias, E.; Lusquiños, F. Concurrent fatigue and potentiation in endurance athletes. Int. J. Sports Physiol. Perform. 2011, 6, 82–93. [Google Scholar] [CrossRef] [Green Version]
- Hyldahl, R.D.; Chen, T.C.; Nosaka, K. Mechanisms and Mediators of the Skeletal Muscle Repeated Bout Effect. Exerc. Sport Sci. Rev. 2017, 45, 24–33. [Google Scholar] [CrossRef]
- González-Bartholin, R.; Mackay, K.; Valladares, D.; Zbinden-Foncea, H.; Nosaka, K.; Peñailillo, L. Changes in oxidative stress, inflammation and muscle damage markers following eccentric versus concentric cycling in older adults. Eur. J. Appl. Physiol. 2019, 119, 2301–2312. [Google Scholar] [CrossRef]
- Smith, L.R.; Kok, H.J.; Zhang, B.; Chung, D.; Spradlin, R.A.; Rakoczy, K.D.; Lei, H.; Boesze-Battaglia, K.; Barton, E.R. Matrix metalloproteinase 13 from satellite cells is required for efficient muscle growth and regeneration. Cell. Physiol. Biochem. 2020, 54, 333–353. [Google Scholar] [CrossRef] [PubMed]
- Lavender, A.P.; Nosaka, K. Comparison between old and young men for changes in makers of muscle damage following voluntary eccentric exercise of the elbow flexors. Appl. Physiol. Nutr. Metab. 2006, 31, 218–225. [Google Scholar] [CrossRef] [Green Version]
- Lavender, A.P.; Nosaka, K. Responses of old men to repeated bouts of eccentric exercise of the elbow flexors in comparison with young men. Eur. J. Appl. Physiol. 2006, 97, 619–626. [Google Scholar] [CrossRef]
- Dedrick, M.E.; Clarkson, P.M. The effects of eccentric exercise on motor performance in young and older women. Eur. J. Appl. Physiol. Occup. Physiol. 1990, 60, 183–186. [Google Scholar] [CrossRef] [PubMed]
| Variable | Concentric Protocol (Mean ± SD) | Eccentric Protocol (Mean ± SD) | Between-Group (p-Value) | Cohen’s d |
|---|---|---|---|---|
| Mean HR (bpm) | 129.7 ± 11.2 | 96.5 ± 12.2 | <0.001 | 2.841 |
| Mean HR (% HRmax) | 68.8 ± 6.6 | 51.3 ± 5.7 | <0.001 | 2.818 |
| Peak HR (bpm) | 154.3 ± 12.2 | 116.2 ± 14.1 | <0.001 | 2.897 |
| Peak HR (% HRmax) | 81.8 ± 4.6 | 61.8 ± 6.6 | <0.001 | 2.897 |
| Mean Power (W) | 137 ± 11 | 101 ± 15 | <0.001 | 2.812 |
| Mean Power (% PPO) | 31.6 ± 2.8 | 23.3 ± 3.8 | <0.001 | 2.493 |
| Sprint Peak Power (W) | 1112 ± 153 | 782 ± 112 | <0.001 | 2.465 |
| Sprint Peak Power (% PPO) | 254.6 ± 22.9 | 179.9 ± 27.3 | <0.001 | 2.966 |
| Total Work (J) | 82,824 ± 6350 | 60,602 ± 8904 | <0.001 | 2.874 |
| Peak Lactate (mmol·L−1) | 4.9 ± 2.1 | 1.8 ± 0.6 | <0.001 | 2.042 |
| Variable | Concentric Protocol (Mean ± SD) | Eccentric Protocol (Mean ± SD) | Between-Groups (Cohen’s d) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | 24-h | Pre | Post | 24-h | Pre | Post | 24-h | |
| Jumping height (cm) | 31.5 ± 5.0 | 33.3 ± 5.0 * | 32.0 ± 4.7 | 30.8 ± 5.4 | 31.7 ± 5.1 | 31.5 ± 5.2 | 0.135 | 0.317 | 0.101 |
| PP (W·kg-1) | 26.7 ± 4.0 | 27.9 ± 3.8 * | 26.8 ± 3.8 | 26.7 ± 4.6 | 27.0 ± 4.6 | 26.3 ± 4.0 | 0.000 | 0.213 | 0.128 |
| Kvert (N·m-1·kg-1) | 56.8 ± 7.1 | 57.7 ± 8.4 | 57.1 ± 8.6 | 59.5 ± 12.9 | 56.9 ± 10.6 | 55.2 ± 8.6 | 0.259 | 0.084 | 0.221 |
| Handgrip strength (kgf) | 53.8 ± 5.3 | 53.8 ± 3.7 | 53.6 ± 4.7 | 55.7 ± 6.3 | 55.5 ± 5.9 | 53.7 ± 5.0 | 0.326 | 0.345 | 0.021 |
| Variable | Concentric Protocol (Mean ± SD) | Eccentric Protocol (Mean ± SD) | ICC | CV |
|---|---|---|---|---|
| BAG3 (ng∙mL−1) | 1.9 ± 1.1 | 2.0 ± 1.3 | 0.952 | 8.3% |
| MMP-13 (pg∙mL−1) | 1281 ± 2285 | 1087 ± 1922 | 0.980 | 19.4% |
| CK (U∙L−1) | 228 ± 154 | 215 ± 133 | 0.942 | 8.5% |
| VAS (mm) | 6.3 ± 6.4 | 7.4 ± 5.4 | 0.642 | 26.1% |
| Thigh circumference (cm) | 53.3 ± 3.1 | 53.9 ± 3.4 | 0.977 | 0.8% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boullosa, D.; Dragutinovic, B.; Deutsch, J.-P.; Held, S.; Donath, L.; Bloch, W.; Schumann, M. Acute and Delayed Effects of Time-Matched Very Short “All Out” Efforts in Concentric vs. Eccentric Cycling. Int. J. Environ. Res. Public Health 2021, 18, 7968. https://doi.org/10.3390/ijerph18157968
Boullosa D, Dragutinovic B, Deutsch J-P, Held S, Donath L, Bloch W, Schumann M. Acute and Delayed Effects of Time-Matched Very Short “All Out” Efforts in Concentric vs. Eccentric Cycling. International Journal of Environmental Research and Public Health. 2021; 18(15):7968. https://doi.org/10.3390/ijerph18157968
Chicago/Turabian StyleBoullosa, Daniel, Boris Dragutinovic, Jan-Philip Deutsch, Steffen Held, Lars Donath, Wilhelm Bloch, and Moritz Schumann. 2021. "Acute and Delayed Effects of Time-Matched Very Short “All Out” Efforts in Concentric vs. Eccentric Cycling" International Journal of Environmental Research and Public Health 18, no. 15: 7968. https://doi.org/10.3390/ijerph18157968






