Effect of the Use of Metronome Feedback on the Quality of Pediatric Cardiopulmonary Resuscitation
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Setting and Population
2.3. Sample Size Calculation
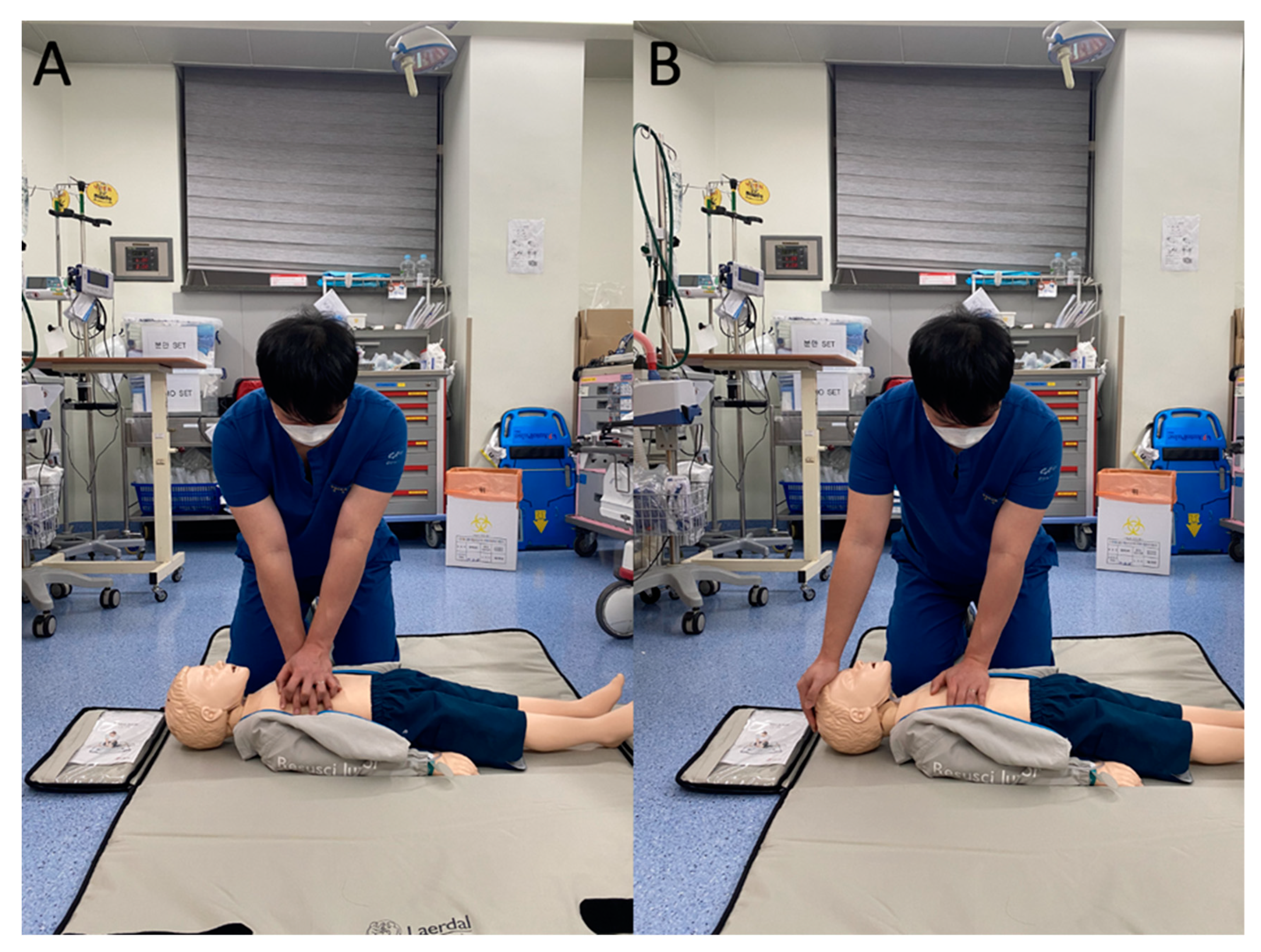
2.4. Study Protocol
2.5. Outcome Variables
2.6. Statistical Analysis
3. Results
3.1. Participant Characteristics
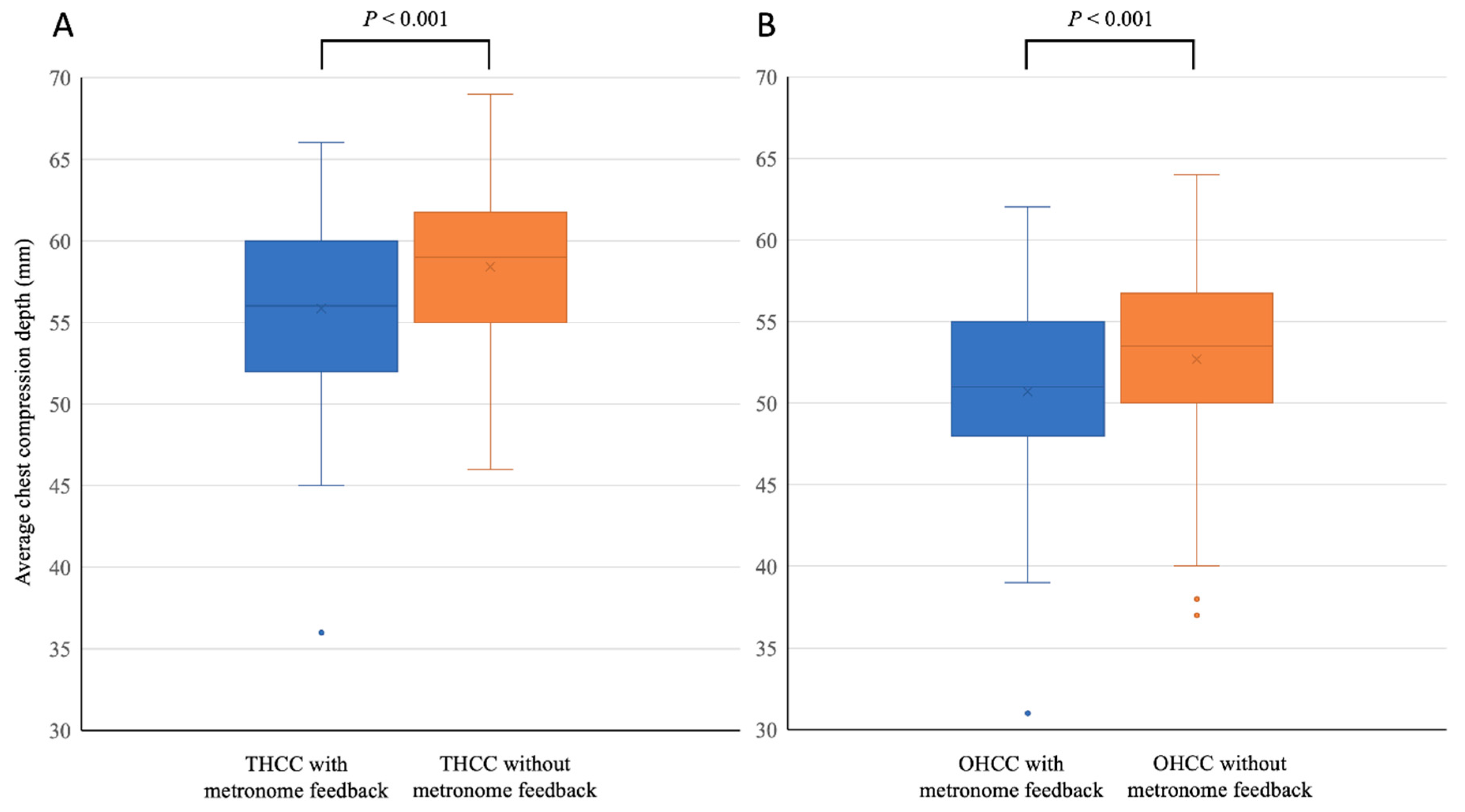
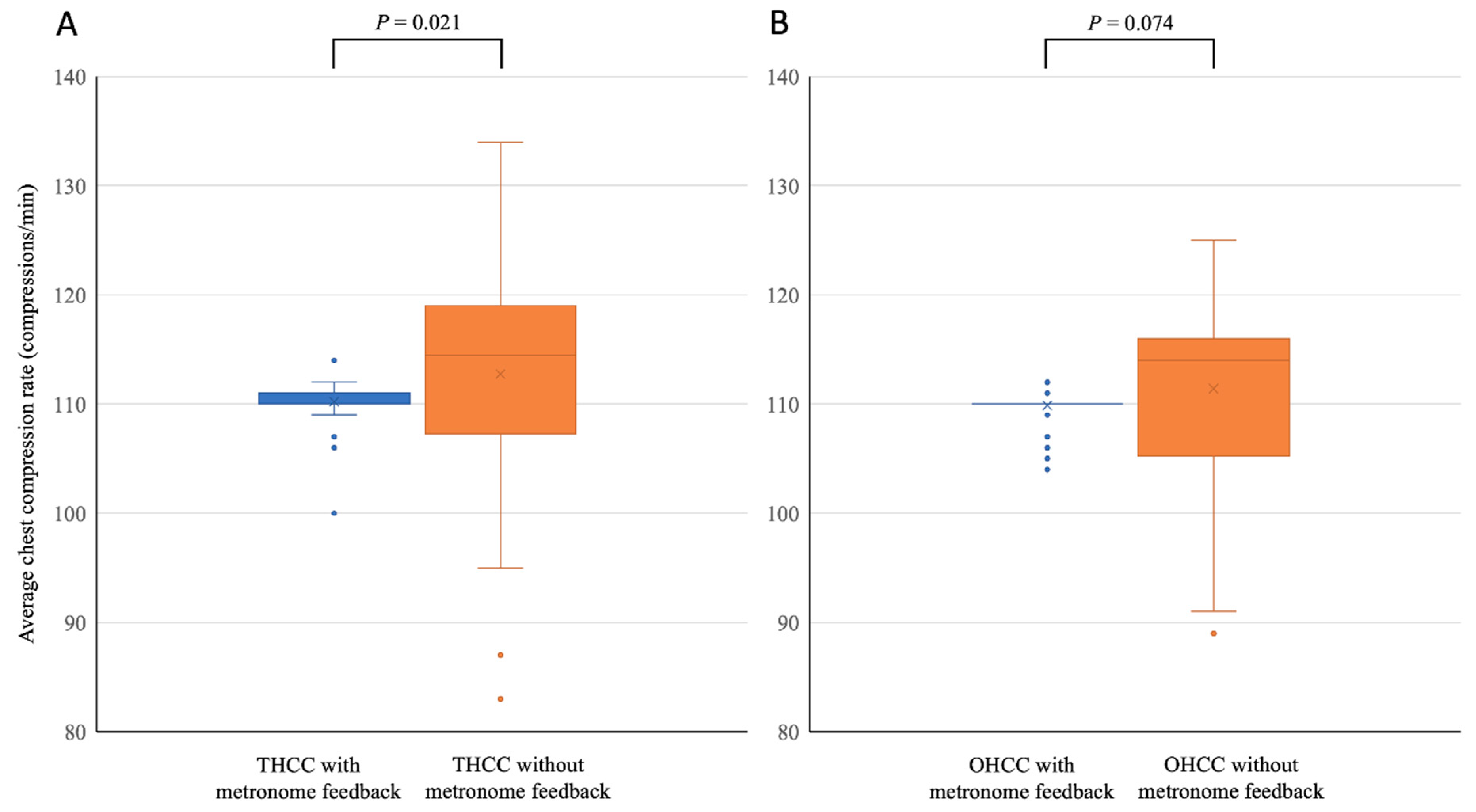
3.2. Comparisons of Variable Values for CPR Performed with and without Metronome Feedback
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Topjian, A.A.; Raymond, T.T.; Atkins, D.; Chan, M.; Duff, J.P.; Joyner, B.L., Jr.; Lasa, J.J.; Lavonas, E.J.; Levy, A.; Mahgoub, M.; et al. Part 4: Pediatric Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S469–S523. [Google Scholar] [CrossRef] [PubMed]
- Van de Voorde, P.; Turner, N.M.; Djakow, J.; de Lucas, N.; Martinez-Mejias, A.; Biarent, D.; Bingham, R.; Brissaud, O.; Hoffmann, F.; Johannesdottir, G.B.; et al. European Resuscitation Council Guidelines 2021: Paediatric Life Support. Resuscitation 2021, 161, 327–387. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Kim, D.K.; Kang, E.K.; Kim, J.T.; Na, J.Y.; Park, B.; Yeom, S.R.; Oh, J.S.; Jhang, W.K.; Jeong, S.I.; et al. 2020 Korean Guidelines for Cardiopulmonary Resuscitation. Part 6. Pediatric basic life support. Clin. Exp. Emerg. Med. 2021, 8, S65–S80. [Google Scholar] [CrossRef]
- Abella, B.S.; Alvarado, J.P.; Myklebust, H.; Edelson, D.P.; Barry, A.; O’Hearn, N.; Vanden Hoek, T.L.; Becker, L.B. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA 2005, 293, 305–310. [Google Scholar] [CrossRef]
- Wik, L.; Kramer-Johansen, J.; Myklebust, H.; Sorebo, H.; Svensson, L.; Fellows, B.; Steen, P.A. Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrest. JAMA 2005, 293, 299–304. [Google Scholar] [CrossRef]
- Kirkbright, S.; Finn, J.; Tohira, H.; Bremner, A.; Jacobs, I.; Celenza, A. Audiovisual feedback device use by health care professionals during CPR: A systematic review and meta-analysis of randomised and non-randomised trials. Resuscitation 2014, 85, 460–471. [Google Scholar] [CrossRef]
- Cheng, A.; Magid, D.J.; Auerbach, M.; Bhanji, F.; Bigham, B.L.; Blewer, A.L.; Dainty, K.N.; Diederich, E.; Lin, Y.; Leary, M.; et al. Part 6: Resuscitation Education Science: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S551–S579. [Google Scholar] [CrossRef]
- Greif, R.; Lockey, A.; Breckwoldt, J.; Carmona, F.; Conaghan, P.; Kuzovlev, A.; Pflanzl-Knizacek, L.; Sari, F.; Shammet, S.; Scapigliati, A.; et al. European Resuscitation Council Guidelines 2021: Education for resuscitation. Resuscitation 2021, 161, 388–407. [Google Scholar] [CrossRef]
- Lee, M.J.; Shin, T.Y.; Lee, C.H.; Moon, J.D.; Roh, S.G.; Kim, C.W.; Park, H.E.; Woo, S.H.; Lee, S.J.; Shin, S.L.; et al. 2020 Korean Guidelines for Cardiopulmonary Resuscitation. Part 9. Education and system implementation for enhanced chain of survival. Clin. Exp. Emerg. Med. 2021, 8, S116–S124. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, E.; Cohen, N.; Maniaci, V.; Pena, B.; Lozano, J.M.; Linares, M. Use of a Metronome in Cardiopulmonary Resuscitation: A Simulation Study. Pediatrics 2015, 136, 905–911. [Google Scholar] [CrossRef]
- Park, S.O.; Hong, C.K.; Shin, D.H.; Lee, J.H.; Hwang, S.Y. Efficacy of metronome sound guidance via a phone speaker during dispatcher-assisted compression-only cardiopulmonary resuscitation by an untrained layperson: A randomised controlled simulation study using a manikin. Emerg. Med. J. 2013, 30, 657–661. [Google Scholar] [CrossRef] [PubMed]
- Rawlins, L.; Woollard, M.; Williams, J.; Hallam, P. Effect of listening to Nellie the Elephant during CPR training on performance of chest compressions by lay people: Randomised crossover trial. BMJ 2009, 339, b4707. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.H.; Lee, S.J.; Kim, S.E.; Lee, K.J.; Choe, J.W.; Kim, C.W. Effects of audio tone guidance on performance of CPR in simulated cardiac arrest with an advanced airway. Resuscitation 2008, 79, 273–277. [Google Scholar] [CrossRef]
- Hostler, D.; Everson-Stewart, S.; Rea, T.D.; Stiell, I.G.; Callaway, C.W.; Kudenchuk, P.J.; Sears, G.K.; Emerson, S.S.; Nichol, G.; Resuscitation Outcomes Consortium, I. Effect of real-time feedback during cardiopulmonary resuscitation outside hospital: Prospective, cluster-randomised trial. BMJ 2011, 342, d512. [Google Scholar] [CrossRef] [PubMed]
- Sample Size Estimation. Centre for Clinical Research and Biostatistics, the Chinese University of Hong Kong. Available online: http://www2.ccrb.cuhk.edu.hk/stat/mean/tsmc_equality.htm (accessed on 13 September 2020).
- Wagner, M.; Bibl, K.; Hrdliczka, E.; Steinbauer, P.; Stiller, M.; Gropel, P.; Goeral, K.; Salzer-Muhar, U.; Berger, A.; Schmolzer, G.M.; et al. Effects of Feedback on Chest Compression Quality: A Randomized Simulation Study. Pediatrics 2019. [Google Scholar] [CrossRef]
- Cheng, A.; Brown, L.L.; Duff, J.P.; Davidson, J.; Overly, F.; Tofil, N.M.; Peterson, D.T.; White, M.L.; Bhanji, F.; Bank, I.; et al. Improving cardiopulmonary resuscitation with a CPR feedback device and refresher simulations (CPR CARES Study): A randomized clinical trial. JAMA Pediatr. 2015, 169, 137–144. [Google Scholar] [CrossRef]
- Handley, A.J. In-hospital chest compressions—The patient on a bed. Resuscitation 2012, 83, 795–796. [Google Scholar] [CrossRef]
- Sherren, P.B.; Lewinsohn, A.; Wijayatilake, D.S. Effects of bed height on the performance of chest compressions: Clinical application of results. Emerg. Med. J. 2011, 28, 171. [Google Scholar] [CrossRef]
- Cho, J.; Oh, J.H. The importance of the bed height during in-hospital cardiopulmonary resuscitation. Resuscitation 2011, 82, 634. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.; Oh, J.H.; Park, Y.S.; Park, I.C.; Chung, S.P. Effects of bed height on the performance of chest compressions. Emerg. Med. J. 2009, 26, 807–810. [Google Scholar] [CrossRef]
- Park, T.S.; Oh, J.H.; Kim, C.W.; Lee, D.H.; Hong, J.Y.; Kim, S.E. Development of a standardized in-hospital cardiopulmonary resuscitation set-up. Signa Vitae 2017, 13, 49–53. [Google Scholar] [CrossRef][Green Version]
- Park, M.R.; Lee, D.S.; In Kim, Y.; Ryu, J.H.; Cho, Y.M.; Kim, H.B.; Yeom, S.R.; Min, M.K. The effect of hydraulic bed movement on the quality of chest compressions. Am. J. Emerg. Med. 2017, 35, 1075–1077. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.H. Effect of bed frame deflection on chest compression quality during cardiopulmonary resuscitation. Am. J. Emerg. Med. 2017, 35, 1368. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.H.; Kim, C.W.; Kim, S.E.; Lee, D.H. Does the bed frame deflection occur along with mattress deflection during in-hospital cardiopulmonary resuscitation? An experiment using mechanical devices. Hong Kong J. Emerg. Med. 2016, 23, 35–41. [Google Scholar] [CrossRef]
- Kim, M.J.; Lee, H.S.; Kim, S.; Park, Y.S. Optimal chest compression technique for paediatric cardiac arrest victims. Scand. J. Trauma Resusc. Emerg. Med. 2015, 23, 36. [Google Scholar] [CrossRef][Green Version]
- Stevenson, A.G.; McGowan, J.; Evans, A.L.; Graham, C.A. CPR for children: One hand or two? Resuscitation 2005, 64. [Google Scholar] [CrossRef] [PubMed]

| Variables | THCC with Metronome Feedback | THCC without Metronome Feedback | p Value |
|---|---|---|---|
| Rate of use of correct hand position (%) | 100.0 (100.0, 100.0) | 100.0 (100.0, 100.0) | 0.955 |
| Total compressions (number) | 160.2 ± 8.8 | 161.1 ± 15.5 | 0.596 |
| Average CCD (mm) | 55.8 ± 5.6 | 58.4 ± 4.9 | <0.001 |
| Adequate CCD achievement rate (%) | 99.0 (95.5, 100.0) | 100.0 (99.0, 100.0) | 0.003 |
| Complete-recoil achievement rate (%) | 96.0 (68.0, 100.0) | 97.5 (86.0, 100.0) | 0.006 |
| Average rate (compressions/min) | 110.0 (110.0, 111.0) | 114.5 (107.5, 119.0) | 0.021 |
| Adequate CCR achievement rate (%) | 100.0 (98.5, 100.0) | 91.0 (34.5, 98.5) | <0.001 |
| Hands-off time (sec) | 8.0 (7.0, 9.0) | 8.0 (7.5, 9.0) | 0.050 |
| Total ventilation (number) | 10.0 (9.5, 10.0) | 10.0 (9.0, 10.0) | 0.796 |
| Average ventilation volume (mL) | 159.1 ± 40.3 | 158.7 ± 45.7 | 0.891 |
| Variables | OHCC with Metronome Feedback | OHCC without Metronome Feedback | p Value |
| Rate of use of correct hand position (%) | 100.0 (100.0, 100.0) | 100.0 (100.0, 100.0) | 0.223 |
| Total compressions (number) | 161.6 ± 8.7 | 161.0 ± 13.8 | 0.698 |
| Average CCD (mm) | 51.0 (48.0, 55.0) | 53.5 (50.0, 56.5) | <0.001 |
| Adequate CCD achievement rate (%) | 95.0 (23.5, 99.5) | 98.5 (77.5, 100.0) | 0.004 |
| Complete-recoil achievement rate (%) | 100.0 (97.5, 100.0) | 100.0 (97.5, 100.0) | 0.674 |
| Average rate (compressions/min) | 110.0 (110.0, 110.0) | 114.0 (105.5, 116.0) | 0.074 |
| Adequate CCR achievement rate (%) | 100.0 (99.0, 100.0) | 94.0 (69.0, 99.0) | <0.001 |
| Hands-off time (sec) | 8.0 (7.0, 9.0) | 8.0 (7.0, 9.0) | 0.015 |
| Total ventilation (number) | 10.0 (9.5, 10.0) | 10.0 (9.0, 10.0) | 0.563 |
| Average ventilation volume (mL) | 164.0 (133.0, 185.5) | 162.0 (122.5, 184.5) | 0.256 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, D.; Lee, W.; Oh, J. Effect of the Use of Metronome Feedback on the Quality of Pediatric Cardiopulmonary Resuscitation. Int. J. Environ. Res. Public Health 2021, 18, 8087. https://doi.org/10.3390/ijerph18158087
Yang D, Lee W, Oh J. Effect of the Use of Metronome Feedback on the Quality of Pediatric Cardiopulmonary Resuscitation. International Journal of Environmental Research and Public Health. 2021; 18(15):8087. https://doi.org/10.3390/ijerph18158087
Chicago/Turabian StyleYang, Dongjun, Wongyu Lee, and Jehyeok Oh. 2021. "Effect of the Use of Metronome Feedback on the Quality of Pediatric Cardiopulmonary Resuscitation" International Journal of Environmental Research and Public Health 18, no. 15: 8087. https://doi.org/10.3390/ijerph18158087
APA StyleYang, D., Lee, W., & Oh, J. (2021). Effect of the Use of Metronome Feedback on the Quality of Pediatric Cardiopulmonary Resuscitation. International Journal of Environmental Research and Public Health, 18(15), 8087. https://doi.org/10.3390/ijerph18158087







