Biopsychosocial Factors during the Perinatal Period: Risks, Preventative Factors, and Implications for Healthcare Professionals
Abstract
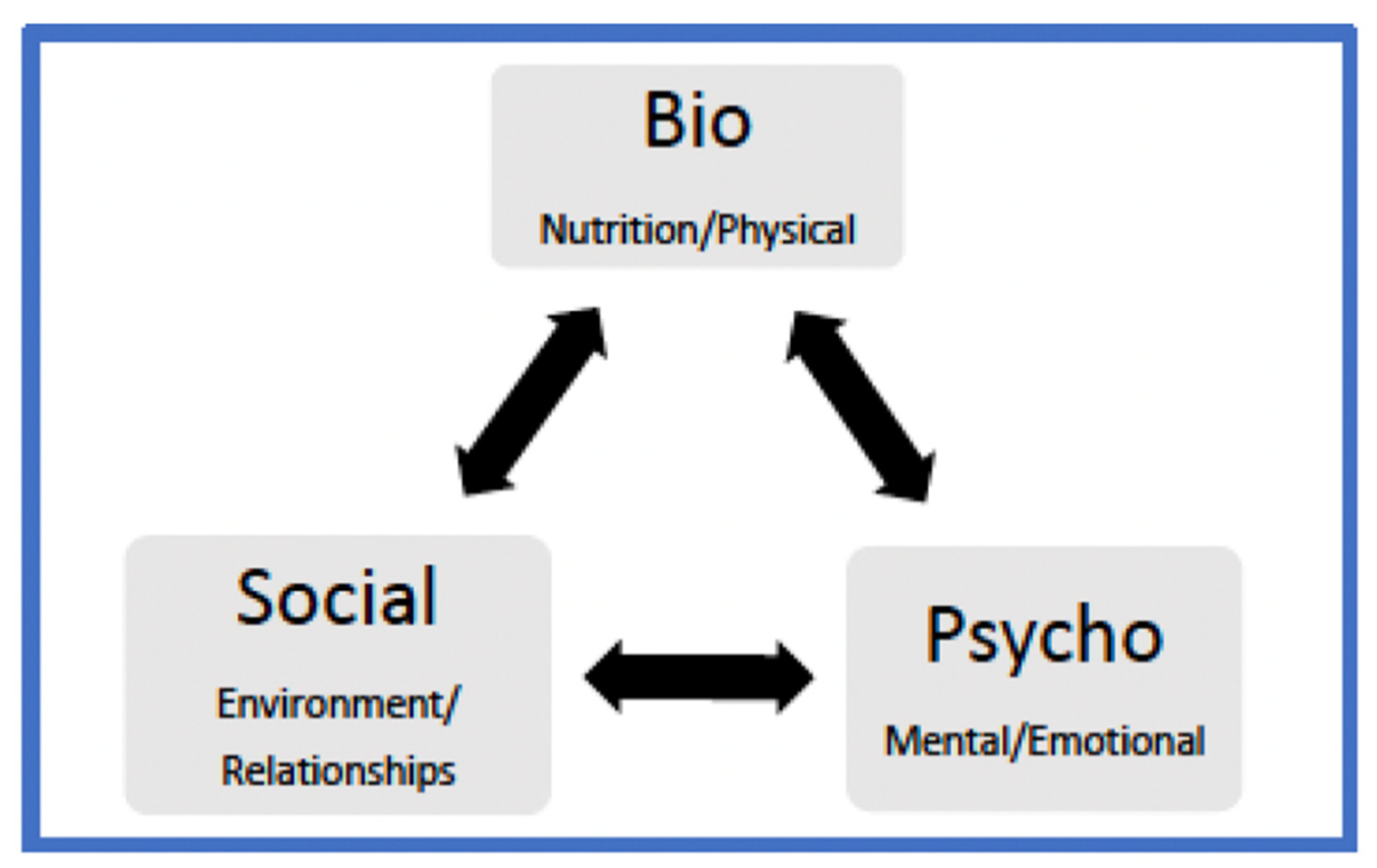
:1. Introduction
2. Biopsychosocial Risk Factors within the Perinatal Period Literature Review
2.1. Biological Risk Factors
2.1.1. Physical Concerns
2.1.2. Nutritional Concerns
2.1.3. Neurobiological Concerns
2.1.4. Adverse Childhood Events (ACE)
2.2. Psychological Risk Factors
2.2.1. Peri-Partum Factors
2.2.2. Post-Partum Factors
2.2.3. Stressors
2.2.4. Transgenerational Trauma
2.3. Sociological Risk Factors
2.3.1. Income/Poverty
2.3.2. Discrimination
2.3.3. Race
2.3.4. Relational Aspects
2.3.5. Access to Insurance/Quality Healthcare Services
3. Discussion
3.1. Implications for Healthcare Professionals
3.1.1. Culturally Responsive Services
3.1.2. Advocacy Role
3.1.3. Patient Assertiveness
4. Limitations of the Literature Review
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Srinivasan, K.; Satyanarayana, V.A.; Lukose, A. Maternal mental health in pregnancy and child behavior. Indian J. Psychiatry 2011, 53, 351. [Google Scholar] [CrossRef] [PubMed]
- International Health Conference. Constitution of the World Health Organization. 1946. Bull. World Health Organ. 2002, 80, 981–984. Available online: https://apps.who.int/iris/handle/10665/268688 (accessed on 12 July 2021).
- Buultjens, M.; Murphy, G.; Robinson, P.; Milgrom, J. The perinatal period: A literature review from the biopsychosocial perspective. Clin. Nurs. Stud. 2013, 1, 19–31. [Google Scholar] [CrossRef] [Green Version]
- Engel, G. The need for a new medical model: A challenge for biomedicine. Science 1977, 196, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Yehudah, S.B.; Lorelle, S. Black birth outcomes and implications for counseling. J. Prof. Couns. 2020, 47, 46–60. [Google Scholar] [CrossRef]
- Moya, J.; Phillips, L.; Sanford, J.; Wooton, M.; Gregg, A.; Schuda, L. A review of physiological and behavioral changes during pregnancy and lactation: Potential exposure factors and data gaps. J. Expo Sci. Environ. Epidemiol. 2014, 24, 449–458. [Google Scholar] [CrossRef] [Green Version]
- Zhang, N.; Zhang, F.; Chen, S.; Han, F.; Lin, G.; Zhai, Y. Associations between hydration state and pregnancy complications, maternal-infant outcomes: Protocol of a prospective observational cohort study. BMC Pregnancy Childbirth 2020, 20, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, C. ACOG practice bulletin no. 92: Use of psychiatric medications during pregnancy and lactation. Obstet. Gynecol. 2008, 111, 1001–1020. [Google Scholar] [CrossRef]
- Lockwood, L.E.; Youssef, N.A. Systematic review of epigenetic effects of pharmacological agents for bipolar disorders. Brain Sci. 2017, 7, 154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hanson, C.; Schumacher, M.V.; Lyden, E.; Su, D.; Furtado, J.; Cammack, R. Fat-soluble vitamins A and E and health disparities in a cohort of pregnant women at delivery. J. Nutr. Sci. 2018, 7, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Radhika, M.S.; Bhaskaram, P.; Balakrishna, N.; Ramalakshmi, B.A.; Devi, S.; Kumar, B.S. Effects of vitamin A deficiency during pregnancy on maternal and child health. BJOG Obstet. Gynecol. Int. J. 2002, 109, 689–693. [Google Scholar] [CrossRef] [PubMed]
- McCauley, M.E.; Van Den Broek, N.; Dou, L.; Othman, M. Vitamin A supplementation during pregnancy for maternal and newborn outcomes. Cochrane Database Syst. Rev. 2015, 10, CD008666. [Google Scholar] [CrossRef]
- Hoekzema, E.; Tamnes, C.K.; Berns, P.; Barba-Müller, E.; Pozzobon, C.; Picado, M. Becoming a mother entails anatomical changes in the ventral striatum of the human brain that facilitate its responsiveness to offspring cues. Psychoneuroendocrinology 2020, 112, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Anderson, M.V.; Rutherford, M.D. Cognitive reorganization during pregnancy and the postpartum period: An evolutionary perspective. Evol. Psychol. 2012, 10, 659–687. [Google Scholar] [CrossRef] [PubMed]
- Pearson, R.M.; Lightman, S.L.; Evans, J. Emotional sensitivity for motherhood: Late pregnancy is associated with enhanced accuracy to encode emotional faces. Horm. Beh. 2009, 56, 557–563. [Google Scholar] [CrossRef]
- Meins, E.; Fernyhough, C.; Fradley, E.; Tuckey, M. Rethinking maternal sensitivity: Mothers’ comments on infants’ mental processes predict security of attachment at 12 months. J. Child Psycol. Psychiatry 2001, 42, 637–648. [Google Scholar] [CrossRef]
- Szyf, M.; Tang, Y.-Y.; Hill, K.G.; Musci, R. The dynamic epigenome and its implications for behavioral interventions: A role for epigenetics to inform disorder prevention and health promotion. Transl. Behav. Med. 2016, 6, 55–62. [Google Scholar] [CrossRef]
- De Socio, J.E. Epigenetics, maternal prenatal psychosocial stress, and infant mental health. Arch. Psychiatry Nurs. 2018, 32, 901–906. [Google Scholar] [CrossRef]
- Bale, T.L. Lifetime stress experience: Transgenerational epigenetics and germ cell programming. Epigenetics 2014, 16, 297–305. [Google Scholar] [CrossRef]
- Buss, C.; Entringer, S.; Swanson, J.M.; Wadwa, P.D. The Role of Stress in Brain Development: The Gestational Environment’s Long-Term Effects on the Brain. Cerebrum 2012, 4, 1–16. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3574809/ (accessed on 15 July 2021).
- Lewis, A.J.; Galbally, M.; Gannon, T.; Symeonides, C. Early life programming as a target for prevention of child and adolescent mental disorders. BMC Med. 2014, 12, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Mersky, J.P.; Plummer Lee, C.T. Adverse childhood experiences and poor birth outcomes in a diverse, low-income sample. BMC Pregnancy Childbirth 2019, 19, 1–7. [Google Scholar] [CrossRef]
- Racine, N.; Devereaux, C.; Cooke, J.E.; Eirich, R.; Zhu, J.; Madigan, S. Adverse childhood experiences and maternal anxiety and depression: A meta-analysis. BMC Psychiatry 2021, 21, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Olsen, J.M. Integrative review of pregnancy health risks and outcomes associated with adverse childhood experiences. J. Obstet Gynecol. Neonatal. Nurs. 2018, 47, 783–794. [Google Scholar] [CrossRef] [PubMed]
- Bjelica, A.; Kapor-Stanulovic, P. Pregnancy as a psychological event. Med. Rev. 2004, 57, 144–148. [Google Scholar] [CrossRef] [PubMed]
- Jou, J.; Kozhimannil, K.B.; Johnson, P.J.; Sakala, C. Patient-perceived pressure from clinicians for labor induction and cesarean delivery: A population-based survey of U.S. women. Health Serv. Res. 2014, 50, 961–981. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Renbarger, K.M.; Shieh, C.; Moorman, M.; Latham-Mintus, K.; Draucker, C. Health care encounters of pregnant and postpartum women with substance use disorders. West. J. Nurs. Res. 2019, 42, 612–628. [Google Scholar] [CrossRef]
- Nicholls, J.; David, A.L.; Iskaros, J.; Lanceley, A. Consent in pregnancy: A qualitative study of the views and experiences of women and their healthcare professionals. Eur. J. Obstet. Gynecol. Reprod. Biol. X 2019, 238, 132–137. [Google Scholar] [CrossRef]
- Bauman, B.L.; Ko, J.Y.; Cox, S.; D’Angelo, D.V.; Warner, L.; Folger, S. Vital signs: Postpartum depressive symptoms and provider discussions about perinatal depression—United States, 2018. MMWR 2020, 69, 575–581. [Google Scholar] [CrossRef]
- Beck, C.T. Predictors of postpartum depression. Nurs. Res. 2001, 50, 275–285. [Google Scholar] [CrossRef] [Green Version]
- Ely, D.M.; Driscoll, A.K. Infant Mortality in the United States: Data from the Period Linked Birth/Infant Death File. Natl. Vital. Stat. Rep. 2019, 68, 1–20. Available online: https://www.cdc.gov/nchs/data/nvsr/nvsr68/nvsr68_10-508.pdf (accessed on 12 July 2021).
- Lorch, S.A.; Enlow, E. The role of social determinants in explaining racial/ethnic disparities in perinatal outcomes. Res. Pediatr. 2015, 79, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Coussons-Read, M.E. Effects of prenatal stress on pregnancy and human development: Mechanisms and pathways. Obstet. Med. 2013, 6, 52–57. [Google Scholar] [CrossRef] [Green Version]
- Holzman, C.; Eyster, J.; Kleyn, M.; Messer, L.C.; Kaufman, J.S.; Laraia, B.A. Maternal weathering and risk of preterm delivery. Am. J. Public Health 2009, 99, 1864–1871. [Google Scholar] [CrossRef]
- Rubin, L.P. Maternal and pediatric health and disease: Integrating biopsychosocial models and epigenetics. Pediatr. Res. 2015, 79, 127–135. [Google Scholar] [CrossRef] [Green Version]
- Halfon, N. Racial and ethnic disparities in birth outcomes: A life-course perspective. J. Mother Child 2003, 7, 13–30. [Google Scholar] [CrossRef]
- Kramer, M.R.; Williamson, R. Multivariate bayesian spatial model of preterm birth and cardiovascular disease among Georgia women: Evidence for life course social determinants of health. Spat. Spatiotemporal. Epidemiol. 2013, 6, 25–35. [Google Scholar] [CrossRef] [PubMed]
- Youssef, N.; Lockwood, L.; Su, S.; Hao, G.; Rutten, B. The effects of trauma, with or without PTSD, on the transgenerational DNA methylation alterations in human offsprings. Brain Sci. 2018, 8, 83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giurgescu, C.; Norr, K.F.; Dancy, B.L.; Twigg, N.; McFarlin, B.L.; Engeland, C.G. Stressors, resources, and stress responses in pregnant African American women. J. Perinat. Neonatal. Nurs. 2013, 27, 81–96. [Google Scholar] [CrossRef] [Green Version]
- Prather, C.; Fuller, T.R.; Jeffries, W.L.; Marshall, K.J.; Howell, A.V.; Belyue-Umole, A. Racism, African American Women, and Their Sexual and Reproductive Health: A Review of Historical and Contemporary Evidence and Implications for Health Equity. Health Equity 2018, 2, 249–259. Available online: https://soilorg/10/1089/heq.2017.0045 (accessed on 12 July 2021). [CrossRef]
- Ronsmans, C.; Graham, W.J. Maternal mortality: Who, when, where, and why. Lancet 2006, 368, 1189–1200. [Google Scholar] [CrossRef]
- Black, R.E.; Allen, L.H.; Bhutta, Z.A.; Caulfield, L.E.; de Onis, M.; Ezzati, M. Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet 2008, 371, 243–260. [Google Scholar] [CrossRef]
- Agaku, I.T.; King, B.A.; Dube, S.R. Current Cigarette Smoking among Adults-United States, 2005–2012. MMWR 2014, 63, 29–34. Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6302a2.htm (accessed on 15 July 2021).
- Cerdá, M.; Johnson-Lawrence, V.D.; Galea, S. Lifetime income patterns and alcohol consumption: Investigating the association between long- and short-term income trajectories and drinking. Soc. Sci. Med. 2011, 73, 1178–1185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strutz, K.L.; Hogan, V.K.; Siega-Riz, A.M.; Suchindran, C.M.; Halpern, C.T.; Hussey, J.M. Preconception stress, birth weight, and birth weight disparities among US women. Am. J. Public Health 2014, 104, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Najman, J.M.; Hayatbakhsh, M.R.; Heron, M.A.; Bor, W.; O’Callaghan, M.J.; Williams, G.M. The impact of episodic and chronic poverty on child cognitive development. J. Pediatr. 2009, 154, 284–289. [Google Scholar] [CrossRef] [PubMed]
- Hamad, R.; Rehkopf, D.H. Poverty, pregnancy, and birth outcomes: A study of the earned income tax credit. Paediatr. Pernat. Epidemiol. 2015, 29, 444–452. [Google Scholar] [CrossRef] [Green Version]
- Kaufman, J.S.; Dole, N.; Savitz, D.A.; Herring, A.H. Modeling community-level effects on preterm birth. Ann. Epidemiol. 2003, 13, 377–384. [Google Scholar] [CrossRef]
- Cubbin, C.; Kim, Y.; Vohra-Gupta, S.; Margerison, C. Longitudinal measures of neighborhood poverty and income inequality are associated with adverse birth outcomes in Texas. Soc. Sci. Med. 2020, 245. [Google Scholar] [CrossRef]
- Bird, S.T.; Bogart, L.M. Perceived Race-Based and Socioeconomic Status (SES)-Based Discrimination in Interactions with Health Care Providers. Ethn. Dis. 2001, 11, 554–563. Available online: https://pubmed.ncbi.nlm.nih.gov/11572421/ (accessed on 12 July 2021).
- Lillie-Blanton, M.; Brodie, M.; Rowland, D.; Altman, D.; McIntosh, M. Race, ethnicity, and the health care system: Public perceptions and experiences. Med. Care Res. Rev. 2000, 57, 218–235. [Google Scholar] [CrossRef]
- De Marco, M.; Thorburn, S.; Zhao, W. Perceived discrimination during prenatal care, labor, and delivery: An examination of data from the Oregon pregnancy risk assessment monitoring system, 1998–1999, 2000, and 2001. Am. J. Public Health 2008, 98, 1818–1822. [Google Scholar] [CrossRef] [PubMed]
- Pamuk, E.; Makjuc, D.; Heck, K.; Reuben, C.; Lochner, K. Socioeconomic Status and Health Chartbook (Report No. 76-641496); U.S. Department of Health and Human Services: Hyattsville, MD, USA, 1998. Available online: https://www.cdc.gov/nchs/data/hus/hus98cht.pdf (accessed on 15 July 2021).
- Dominguez, T.P. Adverse birth outcomes in African American women: The social context of persistent reproductive disadvantage. Soc. Work. Public Health 2011, 26, 3–16. [Google Scholar] [CrossRef] [PubMed]
- Petersen, E.E.; Davis, N.L.; Goodman, D.; Cox, S.; Syverson, C.; Seed, K. Racial/ethnic disparities in pregnancy-related deaths—United States, 2007–2016. MMWR 2019, 68, 762–765. [Google Scholar] [CrossRef] [Green Version]
- Chalhoub, T.; Rimar, K. The Health Care System and Racial Disparities in Maternal Mortality. Cent. Am. Prog. 2018, 1–7. Available online: https://cdn.americanprogress.org/content/uploads/2018/05/09121820/HealthSystemDisparitiesInMaternalMortality-Brief.pdf?_ga=2.71795347.1206125014.1623721127-1221635400.1623721127 (accessed on 15 July 2021).
- Vedam, S.; Stoll, K.; Taiwo, T.K.; Rubashkin, N.; Cheyney, M.; Strauss, N. The giving voice to mothers study: Inequity and mistreatment during pregnancy and childbirth in the United States. Reprod. Health 2019, 16, 1–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McLemore, M.R.; Altman, M.R.; Cooper, N.; Williams, S.; Rand, L.; Franck, L. Health care experiences of pregnant, birthing and postnatal women of color at risk for preterm birth. Soc. Sci. Med. 2018, 201, 127–135. [Google Scholar] [CrossRef] [Green Version]
- Stapleton, L.R.; Schetter, C.D.; Westling, E.; Rini, C.; Glynn, L.M.; Hobel, C.J. Perceived partner support in pregnancy predicts lower maternal and infant distress. J. Fam. Pschol. 2012, 26, 453–463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whisman, M.A.; Davila, J.; Goodman, S.H. Relationship adjustment, depression, and anxiety during pregnancy and the postpartum period. J. Fam. Psychol. 2011, 25, 375–383. [Google Scholar] [CrossRef] [Green Version]
- Alhusen, J.L.; Ray, E.; Sharps, P.; Bullock, L. Intimate partner violence during pregnancy: Maternal and neonatal outcomes. J. Women’s Health 2015, 24, 100–106. [Google Scholar] [CrossRef] [Green Version]
- Tjaden, P.; Thoennes, N. Full Report of the Prevalence, Incidence, and Consequences of Violence against Women: Findings from the National Violence against Women Survey. Natl. Inst. Justice Cent. Dis. Control Prev. 2000, 1–59. Available online: https://www.ojp.gov/pdffiles1/nij/183781.pdf (accessed on 12 July 2021).
- Vest, J.R.; Caitlin, T.K.; Brownson, R.C. Multistate analysis of factors associated with intimate partner violence. Am. J. Prev. Med. 2002, 22, 156–164. [Google Scholar] [CrossRef]
- Bhatt, C.B.; Beck-Sagué, C.M. Medicaid expansion and infant mortality in the United States. Am. J. Public Health 2018, 108, 565–567. [Google Scholar] [CrossRef] [PubMed]
- Guttmacher Institute. Benefits of Contraceptive Use in the United States (Video Transcript). Available online: https://www.guttmacher.org/benefits-contraceptive-use-united-states-video-transcript (accessed on 12 July 2021).
- Thomas, M.P.; Ammann, G.; Brazier, E.; Noyes, P.; Maybank, A. Doula services within a healthy start program: Increasing access for an underserved population. J. Mother Child 2017, 21, 59–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Granello, D.; Young, M.E. Counseling Today: Foundations of Professional Identity, 2nd ed.; Pearson: Upper Saddle River, NJ, USA, 2019. [Google Scholar]
- Myers, J.E.; Luecht, R.M.; Sweeney, T.J. The factor structure of wellness: Reexamining theoretical and empirical models underlying the wellness evaluation of lifestyle (WEL) and the five-factor wei. Meas. Eval. Couns. Dev. 2004, 36, 194–208. [Google Scholar] [CrossRef]
- Ratts, M.J.; Singh, A.A.; Nassar-McMillan, S.; Butler, S.K.; McCullough, J.R. Multicultural and social justice counseling competencies: Guidelines for the counseling profession. J. Multicult. Couns. Dev. 2016, 44, 28–48. [Google Scholar] [CrossRef]
| Tenets | Risk Factors | Components |
|---|---|---|
| Biological | ||
| Physical | Body changes, hormonal changes, medication concerns, epigenetic changes | |
| Nutritional | Poor nutrition, vitamin deficiencies, lack of access to quality food | |
| Neurobiological | Neurological changes (e.g., brain structure changes), genetic predisposition to illness/health | |
| Adverse Childhood Events (ACEs) | Negative/traumatic experiences of childhood | |
| Psychological | ||
| Peri-Partum | Anxiety, fatigue/exhaustion, baby blues, mood changes (in last month of gestation or first few months after delivery) | |
| Post-Partum | Baby blues, post-partum depression (PPD), depression, self-esteem issues, anxiety, stress, lack of support (in post-gestation) | |
| Stressors | Caused by biological components (e.g., physical changes, nutritional demands, neurobiological changes, traumatic events), mental wellness concerns, anxiety, lack of support, weathering phenomenon | |
| Transgenerational Trauma | Past traumatic experiences influencing offspring | |
| Sociological | ||
| Income/Poverty | Lower SES associated with negative maternal and neonatal outcomes | |
| Discrimination | Unjust treatment, negative impacts on maternal and neonatal outcomes | |
| Race | Racial disparities in birth outcomes, most common form is verbal-based discrimination, WOC experience worse maternal and neonatal pregnancy lifecycle outcomes | |
| Relational Aspects | Love, friendship, social support, intimate partner violence (IPV) | |
| Access to Insurance/Quality Healthcare | Insurance plans, family planning access/reproductive care |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blount, A.J.; Adams, C.R.; Anderson-Berry, A.L.; Hanson, C.; Schneider, K.; Pendyala, G. Biopsychosocial Factors during the Perinatal Period: Risks, Preventative Factors, and Implications for Healthcare Professionals. Int. J. Environ. Res. Public Health 2021, 18, 8206. https://doi.org/10.3390/ijerph18158206
Blount AJ, Adams CR, Anderson-Berry AL, Hanson C, Schneider K, Pendyala G. Biopsychosocial Factors during the Perinatal Period: Risks, Preventative Factors, and Implications for Healthcare Professionals. International Journal of Environmental Research and Public Health. 2021; 18(15):8206. https://doi.org/10.3390/ijerph18158206
Chicago/Turabian StyleBlount, Ashley J., Charmayne R. Adams, Ann L. Anderson-Berry, Corrine Hanson, Kara Schneider, and Gurudutt Pendyala. 2021. "Biopsychosocial Factors during the Perinatal Period: Risks, Preventative Factors, and Implications for Healthcare Professionals" International Journal of Environmental Research and Public Health 18, no. 15: 8206. https://doi.org/10.3390/ijerph18158206
APA StyleBlount, A. J., Adams, C. R., Anderson-Berry, A. L., Hanson, C., Schneider, K., & Pendyala, G. (2021). Biopsychosocial Factors during the Perinatal Period: Risks, Preventative Factors, and Implications for Healthcare Professionals. International Journal of Environmental Research and Public Health, 18(15), 8206. https://doi.org/10.3390/ijerph18158206







