The Health Behaviour of German Outpatient Caregivers in Relation to the COVID-19 Pandemic: A Mixed-Methods Study
Abstract
:1. Introduction
1.1. Background
1.2. Current State of Research
1.2.1. Eating and Drinking Behaviour
1.2.2. Physical Activity
1.2.3. Smoking Behaviour
1.2.4. Regeneration Behaviour
1.3. Study Aims and Research Questions
- How do outpatient caregivers perceive their health behaviour during the COVID-19 pandemic?
- Did outpatient caregivers perceive any change in their health behaviour due to the COVID-19 pandemic?
2. Materials and Methods
2.1. Study Design
2.2. Qualitative Approach
2.2.1. Design, Participants and Recruitment
2.2.2. Interview Guideline
2.2.3. Data Analysis
2.3. Quantitative Approach
2.3.1. Design, Participants and Recruitment
2.3.2. Variables, Measures and Processes
2.3.3. Statistical Analysis
3. Results
3.1. Qualitative Approach
3.1.1. Sample Characteristics
3.1.2. Health Behaviour of Outpatient Caregivers
“Usually I used fresh ingredients, now I have more frozen food because the joy of cooking has decreased due to this stress. I won’t stand in the kitchen for two hours, I’m glad if it’s only one.” (Outpatient Caregiver #3, 31–40 years, <1 year outpatient care experience)
“No, it stayed the same, well I drink a lot of water and coffee and so on.” (Outpatient Caregiver #6, ≥41 years, 1–5 years outpatient care experience)
“Well at home I used to drink a lot more soft drinks such as Coke or Fanta but that’s reduced currently, significantly less” (Outpatient Caregiver #7, 20–30 years, 1–5 years outpatient care experience)
“Well, I used to go to the gym and that’s simply not possible anymore. You have to be creative at home but there are just not the same possibilities (…).” (Outpatient Caregiver #7, 20–30 years, 1–5 years outpatient care experience)
“I am that person who likes to smoke while talking on the phone and that became more. Whereby actually, while I’m working I’m smoking less because I hate it when my mask is smelling like smoke.” (Outpatient Caregiver #11, ≥41 years, >5 years outpatient care experience)
“Well, usually we liked to have breakfast together. But now this is over.” (Outpatient Caregiver #1, 31–40 years, <1 year outpatient care experience)
“Well, I can’t recover at all. Because of screaming children in the background when I want to relax.” (Outpatient Caregiver #8, 31–40 years, >5 years outpatient care experience)
“Yes, we must protect ourselves with masks and gloves.” (Outpatient Caregiver #3, 31–40 years, <1 year outpatient care experience)
”Yes, one is washing hands more often suddenly. That’s truly the case. You wash your hands all the time (…)” (Outpatient Caregiver #2, 31–40 years, <1 year outpatient care experience)
“There is also an arrangement with the car that you clean the steering wheel, the gear stick, the door handle from the inside before you park the car again and the next person goes in there.” (Outpatient Caregiver #12, ≥41 years, >5 years outpatient care experience)
“I always try to be careful and do not become careless about respecting the distance rules (…).” (Outpatient Caregiver #14, ≥41 years, >5 years outpatient care experience)
“I have to say that it was even more extreme in March, but now it’s not like you’re standing there all the time, then I’d be lying, because I don’t have the time to clean everything every two hours.” (Outpatient Caregiver #1, 31–40 years, <1 year outpatient care experience)
“Privately, I always wear mouth-nose protection.” (Outpatient Caregiver #5, 20–30 years, 1–5 years outpatient care experience)
“Yes, we wash our hands much more often. Much more often and also [our children’s hands] much more often. It is very much in our consciousness.” (Outpatient Caregiver #8, 31–40 years, >5 years outpatient care experience)
“In private? I have reduced my contacts, I do not go out privately.” (Outpatient Caregiver #10, 31–40 years, 1–5 years outpatient care experience)
“I try to take my child with me as little as possible.” (Outpatient Caregiver #3, 31–40 years, <1 year outpatient care experience)
“Yeah. That’s good. I think everything digital is great. (...). I just read a report that it works so well in China, so that would be something.” (Outpatient Caregiver #8, 31–40 years, >5 years outpatient care experience)
“No, neither. I have already made sure to have plenty of fresh air beforehand, to go for walks and, yes, to do sports and all that. So I didn’t have the feeling that I had to do anything else during the pandemic (…) It didn’t affect my activity or anything else.” (Outpatient Caregiver #14, ≥41 years, >5 years outpatient care experience)
3.2. Quantitative Approach
3.2.1. Participants
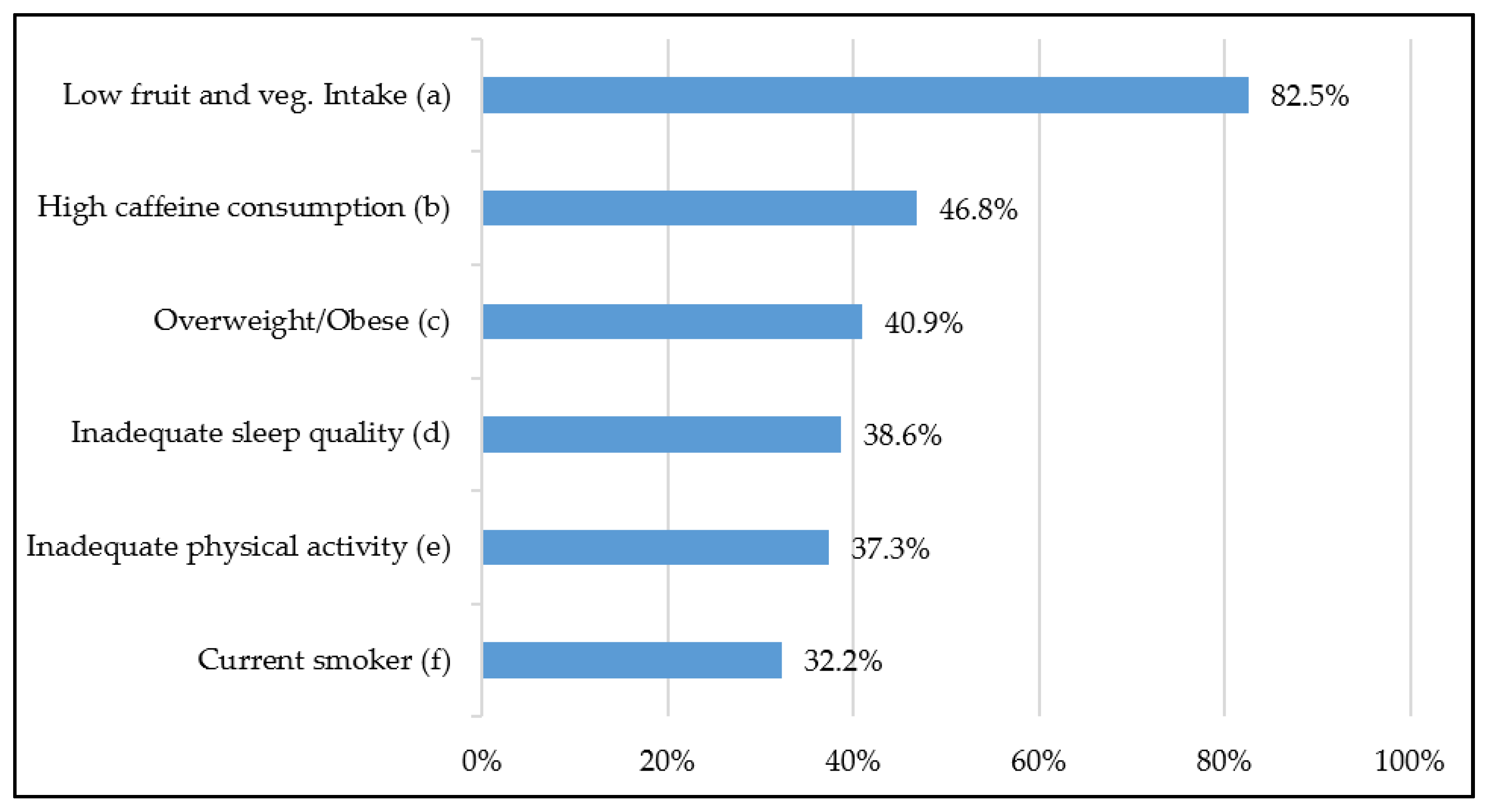
3.2.2. Health Behaviour of Participants
3.2.3. Differences in Health Behaviour in Times of the COVID-19 Pandemic
3.2.4. Subgroup Analyses
4. Discussion
4.1. Discussion of the Interview and Survey Results
4.1.1. Eating Behaviour
4.1.2. Drinking Behaviour
4.1.3. Physical Activity
4.1.4. Smoking Behaviour
4.1.5. Regeneration at Work: Break Behaviour
4.1.6. Regeneration after Work: Sleep Behaviour
4.1.7. Stress Perception
4.1.8. Personal Health-Promoting Behaviour
4.2. Strengths and Limitations
4.3. Practical Implications for Further Research and Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Statistisches Bundesamt. Pflegestatistik—Pflege im Rahmen der Pflegeversicherung: Deutschlandergebnisse. 2018. Available online: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Pflege/Publikationen/Downloads-Pflege/pflege-deutschlandergebnisse-5224001179004.pdf?__blob=publicationFile (accessed on 26 July 2021).
- Büscher, A.; Krebs, M. Qualität in der ambulanten Pflege. In Pflege-Report 2018. Qualität in der Pflege; Jacobs, K., Kuhlmey, A., Greß, S., Klauber, J., Schwinger, A., Eds.; Springer: Berlin, Germany, 2018; pp. 127–134. [Google Scholar]
- Bundesministerium für Gesundheit. Pflegedienst und Pflegesachleistungen. Available online: https://www.bundesgesundheitsministerium.de/pflegedienst-und-pflegesachleistungen.html (accessed on 16 July 2021).
- Schulz, E. Pflegemarkt: Drohendem Arbeitskräftemangel kann entgegengewirkt werden. DIW Wochenber. 2012, 79, 3–18. [Google Scholar]
- Techniker Krankenkasse. Gesundheitsreport. Pflegefall Pflegebranche? So geht’s Deutschlands Pflegekräften; Techniker Krankenkasse: Hamburg, Germany, 2019. [Google Scholar]
- Poulsen, K.; Cleal, B.; Clausen, T.; Andersen, L.L. Work, Diabetes and Obesity: A Seven Year Follow-Up Study among Danish Health Care Workers. PLoS ONE 2014, 9, e103425. [Google Scholar] [CrossRef] [Green Version]
- Steel, J.L.; Cheng, H.; Pathak, R.; Wang, Y.; Miceli, J.; Hecht, C.L.; Haggerty, D.; Peddada, S.; Geller, D.A.; Marsh, W.; et al. Psychosocial and behavioral pathways of metabolic syndrome in cancer caregivers. Psycho-Oncol. 2019, 28, 1735–1742. [Google Scholar] [CrossRef] [PubMed]
- Wirth, T.; Kozak, A.; Schedlbauer, G.; Nienhaus, A. Health behaviour, health status and occupational prospects of apprentice nurses and kindergarten teachers in Germany: A cross-sectional study. J. Occup. Med. Toxicol. 2016, 11, 26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kramer, A.; Son, J. Who Cares about the Health of Health Care Professionals? An 18-Year Longitudinal Study of Working Time, Health, and Occupational Turnover. ILR Rev. 2016, 69, 939–960. [Google Scholar] [CrossRef]
- Eckel, N.; Li, Y.; Kuxhaus, O.; Stefan, N.; Hu, F.B.; Schulze, M.B. Transition from metabolic healthy to unhealthy phenotypes and association with cardiovascular disease risk across BMI categories in 90 257 women (the Nurses′ Health Study): 30 year follow-up from a prospective cohort study. Lancet Diabetes Endocrinol. 2018, 6, 714–724. [Google Scholar] [CrossRef]
- Félix, N.D.C.; Nóbrega, M. Metabolic Syndrome: Conceptual analysis in the nursing context. Rev. Lat. Am. Enferm. 2019, 27, e3154. [Google Scholar] [CrossRef] [PubMed]
- Hruby, A.; Manson, J.E.; Qi, L.; Malik, V.S.; Rimm, E.B.; Sun, Q.; Willett, W.C.; Hu, F.B. Determinants and Consequences of Obesity. Am. J. Public Health 2016, 106, 1656–1662. [Google Scholar] [CrossRef]
- Martinez-Ferran, M.; de la Guía-Galipienso, F.; Sanchis-Gomar, F.; Pareja-Galeano, H. Metabolic Impacts of Confinement during the COVID-19 Pandemic Due to Modified Diet and Physical Activity Habits. Nutrients 2020, 12, 1549. [Google Scholar] [CrossRef]
- Bergh, M.F.Q.K.-V.D.; Buiting, A.G.M.; Pas, S.D.; Bentvelsen, R.; Bijllaardt, W.V.D.; Van Oudheusden, A.J.G.; Van Rijen, M.M.L.; Verweij, J.J.; Koopmans, M.P.G.; Kluytmans, J.A.J.W. Prevalence and Clinical Presentation of Health Care Workers With Symptoms of Coronavirus Disease 2019 in 2 Dutch Hospitals During an Early Phase of the Pandemic. JAMA Netw. Open 2020, 3, e209673. [Google Scholar] [CrossRef]
- Lai, X.; Wang, M.; Qin, C.; Tan, L.; Ran, L.; Chen, D.; Zhang, H.; Shang, K.; Xia, C.; Wang, S.; et al. Coronavirus Disease 2019 (COVID-2019) Infection Among Health Care Workers and Implications for Prevention Measures in a Tertiary Hospital in Wuhan, China. JAMA Netw. Open 2020, 3, e209666. [Google Scholar] [CrossRef]
- Lietz, J.; Westermann, C.; Nienhaus, A.; Schablon, A. The Occupational Risk of Influenza A (H1N1) Infection among Healthcare Personnel during the 2009 Pandemic: A Systematic Review and Meta-Analysis of Observational Studies. PLoS ONE 2016, 11, e0162061. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.P.; Yeung, W.-S. Staff Mental Health Self-Assessment During the COVID-19 Outbreak. East. Asian Arch. Psychiatry 2020, 30, 34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dal’Bosco, E.B.; Floriano, L.S.M.; Skupien, S.V.; Arcaro, G.; Martins, A.R.; Anselmo, A.C.C. Mental health of nursing in coping with COVID-19 at a regional university hospital. Rev. Bras. Enferm. 2020, 73, e20200434. [Google Scholar] [CrossRef]
- Huang, J.Z.; Han, M.F.; Luo, T.D.; Ren, A.K.; Zhou, X.P. Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2020, 38, 192–1951. [Google Scholar]
- Kang, L.; Ma, S.; Chen, M.; Yang, J.; Wang, Y.; Li, R.; Yao, L.; Bai, H.; Cai, Z.; Yang, B.X.; et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav. Immun. 2020, 87, 11–17. [Google Scholar] [CrossRef]
- Kim, H.; Park, K.J.; Shin, Y.W.; Lee, J.S.; Chung, S.; Lee, T.; Kim, M.J.; Jung, J.; Lee, J.; Yum, M.S.; et al. Psychological Impact of Quarantine on Caregivers at a Children’s Hospital for Contact with Case of COVID-19. J. Korean Med. Sci. 2020, 35, e255. [Google Scholar] [CrossRef]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Network Open 2020, 3, e203976. [Google Scholar] [CrossRef]
- Li, Z.; Ge, J.; Yang, M.; Feng, J.; Qiao, M.; Jiang, R.; Bi, J.; Zhan, G.; Xu, X.; Wang, L.; et al. Vicarious traumatization in the general public, members, and non-membersof medical teams aiding in COVID-19 control. Brain. Behav. Immun. 2020. [Google Scholar] [CrossRef]
- Liang, Y.; Chen, M.; Zheng, X.; Liu, J. Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. J. Psychosom. Res. 2020, 133, 110102. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Luo, D.; Haase, J.E.; Guo, Q.; Wang, X.Q.; Liu, S.; Xia, L.; Liu, Z.; Yang, J.; Yang, B.X. The experiences of health-care providers during the COVID-19 crisis in China: A qualitative study. Lancet Glob. Health 2020, 8, e790–e798. [Google Scholar] [CrossRef]
- Liu, Z.; Wu, J.; Shi, X.; Ma, Y.; Ma, X.; Teng, Z.; You, X.; Zhang, Y.; Zhang, W.; Feng, Z.; et al. Mental Health Status of Healthcare Workers in China for COVID-19 Epidemic. Ann. Glob. Health 2020, 86, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Lu, W.; Wang, H.; Lin, Y.; Li, L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res. 2020, 288, 112936. [Google Scholar] [CrossRef] [PubMed]
- Mo, Y.; Deng, L.; Zhang, L.; Lang, Q.; Liao, C.; Wang, N.; Qin, M.; Huang, H. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J. Nurs. Manag. 2020, 28, 1002–1009. [Google Scholar] [CrossRef] [Green Version]
- Paffenholz, P.; Peine, A.; Hellmich, M.; Paffenholz, S.V.; Martin, L.; Luedde, M.; Haverkamp, M.; Roderburg, C.; Marx, G.; Heidenreich, A.; et al. Perception of the 2020 SARS-CoV-2 pandemic among medical professionals in Germany: Results from a nationwide online survey. Emerg. Microbes Infect. 2020, 9, 1590–1599. [Google Scholar] [CrossRef]
- Shen, X.; Zou, X.; Zhong, X.; Yan, J.; Li, L. Psychological stress of ICU nurses in the time of COVID-19. Crit. Care 2020, 24, 1–3. [Google Scholar] [CrossRef]
- Sun, N.; Wei, L.; Shi, S.; Jiao, D.; Song, R.; Ma, L.; Wang, H.; Wang, C.; Wang, Z.; You, Y.; et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am. J. Infect. Control. 2020, 48, 592–598. [Google Scholar] [CrossRef]
- Xiao, H.; Zhang, Y.; Kong, D.; Li, S.; Yang, N. The Effects of Social Support on Sleep Quality of Medical Staff Treating Patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. 2020, 26, e923549. [Google Scholar] [CrossRef]
- Zerbini, G.; Ebigbo, A.; Reicherts, P.; Kunz, M.; Messman, H. Psychosocial burden of healthcare professionals in times of COVID-19—A survey conducted at the University Hospital Augsburg. Ger. Med. Sci. 2020, 18, Doc05. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wei, L.; Li, H.; Pan, Y.; Wang, J.; Li, Q.; Wu, Q.; Wei, H. The Psychological Change Process of Frontline Nurses Caring for Patients with COVID-19 during Its Outbreak. Issues Ment. Health Nurs. 2020, 41, 525–530. [Google Scholar] [CrossRef]
- Wolf-Ostermann, K.; Schmidt, A.; Preuß, B.; Heinze, F.; Seibert, K.; Friedrich, A.-C.; Domhoff, D.; Stolle, C.; Rothgang, H. Pflege in Zeiten von Corona: Ergebnisse einer deutschlandweiten Querschnittbefragung von ambulanten Pflegediensten und teilstationären Einrichtungen. Pflege 2020, 33, 277–288. [Google Scholar] [CrossRef] [PubMed]
- Mojtahedzadeh, N.; Rohwer, E.; Neumann, F.A.; Nienhaus, A.; Augustin, M.; Zyriax, B.-C.; Harth, V.; Mache, S. The Health Behaviour of German Outpatient Caregivers in Relation to Their Working Conditions: A Qualitative Study. Int. J. Environ. Res. Public Health 2021, 18, 5942. [Google Scholar] [CrossRef]
- Blättner, B.; Waller, H. Gesundheitswissenschaft. Eine Einführung in Grundlagen, Theorie und Anwendung, 6th ed.; Kohlhammer: Stuttgart, Germany, 2018. [Google Scholar]
- Anderson, R. Gesundheitsförderung: Ein Überblick. Europäische Monographien zur Forschung. Gesundheitserziehung 1984, 6, 1–140. [Google Scholar]
- Lindeman, K.; Kugler, J.; Klewer, J. Ernährungsgewohnheiten, BMI und Diätversuche von Auszubildenden in Gesundheitsfachberufen. HeilberufeScience 2011, 2, 67–70. [Google Scholar] [CrossRef]
- Perry, L.; Gallagher, R.; Duffield, C. The health and health behaviours of Australian metropolitan nurses: An exploratory study. BMC Nurs. 2015, 14, 45. [Google Scholar] [CrossRef] [Green Version]
- Schneider, A.; Bak, M.; Mahoney, C.; Hoyle, L.; Kelly, M.; Atherton, I.M.; Kyle, R.G. Health-related behaviours of nurses and other healthcare professionals: A cross-sectional study using the Scottish Health Survey. J. Adv. Nurs. 2019, 75, 1239–1251. [Google Scholar] [CrossRef] [PubMed]
- Gupta, C.C.; Coates, A.M.; Dorrian, J.; Banks, S. The factors influencing the eating behaviour of shiftworkers: What, when, where and why. Ind. Health 2019, 57, 419–453. [Google Scholar] [CrossRef] [Green Version]
- Buchvold, H.V.; Pallesen, S.; Øyane, N.M.F.; Bjorvatn, B. Associations between night work and BMI, alcohol, smoking, caffeine and exercise - a cross-sectional study. BMC Public Health 2015, 15, 1112. [Google Scholar] [CrossRef] [Green Version]
- Damerow, S.; Rommel, A.; Prütz, F.; Beyer, A.-K.; Hapke, U.; Schienkiewitz, A.; Starker, A.; Richter, A.; Baumert, J.; Fuchs, J.; et al. Die gesundheitliche Lage in Deutschland in der Anfangsphase der COVID-19-Pandemie. Zeitliche Entwicklung ausgewählter Indikatoren der Studie GEDA-EHIS 2019. J. Health Monit. 2020, 3–22. [Google Scholar] [CrossRef]
- Zupo, R.; Castellana, F.; Sardone, R.; Sila, A.; Giagulli, V.A.; Triggiani, V.; Cincione, R.I.; Giannelli, G.; De Pergola, G. Preliminary Trajectories in Dietary Behaviors during the COVID-19 Pandemic: A Public Health Call to Action to Face Obesity. Int. J. Environ. Res. Public Health 2020, 17, 7073. [Google Scholar] [CrossRef]
- Duong, T.V.; Pham, K.M.; Do, B.N.; Kim, G.B.; Dam, H.T.B.; Le, V.-T.T.; Nguyen, T.T.P.; Nguyen, H.T.; Nguyen, T.T.; Le, T.T.; et al. Digital Healthy Diet Literacy and Self-Perceived Eating Behavior Change during COVID-19 Pandemic among Undergraduate Nursing and Medical Students: A Rapid Online Survey. Int. J. Environ. Res. Public Health 2020, 17, 7185. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Han, K.; Trinkoff, A.M.; Storr, C.L.; Geiger-Brown, J.; Johnson, K.L.; Park, S. Comparison of Job Stress and Obesity in Nurses With Favorable and Unfavorable Work Schedules. J. Occup. Environ. Med. 2012, 54, 928–932. [Google Scholar] [CrossRef]
- Lehmann, F.; von Lindeman, K.; Klewer, J.; Kugler, J. BMI, physical inactivity, cigarette and alcohol consumption in female nursing students: A 5-year comparison. BMC Med. Educ. 2014, 14, 82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mc Carthy, V.J.C.; Wills, T.; Crowley, S. Nurses, age, job demands and physical activity at work and at leisure: A cross-sectional study. Appl. Nurs. Res. 2018, 40, 116–121. [Google Scholar] [CrossRef]
- Zaworski, K.; Kubińska, Z.; Dziewulska, A.; Walasek, O. Physical Activity of Poles in the Care for Their Health Potential Before and During the COVID-19 Pandemic. Disaster Med. Public Health Prep. 2020, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Özden, G.; Parlar Kiliç, S. The Effect of Social Isolation during COVID-19 Pandemic on Nutrition and Exercise Behaviors of Nursing Students. Ecol. Food Nutr. 2021, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Nilan, K.; McKeever, T.M.; McNeill, A.; Raw, M.; Murray, R.L. Prevalence of tobacco use in healthcare workers: A systematic review and meta-analysis. PLoS ONE 2019, 14, 1–26. [Google Scholar] [CrossRef]
- Tran, T.V.; Nguyen, H.C.; Pham, L.V.; Nguyen, M.H.; Nguyen, H.C.; Ha, T.H.; Phan, D.T.; Dao, H.K.; Nguyen, P.B.; Trinh, M.V.; et al. Impacts and interactions of COVID-19 response involvement, health-related behaviours, health literacy on anxiety, depression and health-related quality of life among healthcare workers: A cross-sectional study. BMJ Open 2020, 10, e041394. [Google Scholar] [CrossRef]
- Wendsche, J.; Hacker, W.; Wegge, J. Understaffing and registered nurses’ turnover: The moderating role of regular rest breaks. Ger. J. Hum. Resour. Manag. 2017, 31, 238–259. [Google Scholar] [CrossRef]
- Glaser, J.; Höge, T. Probleme und Lösungen in der Pflege aus Sicht der Arbeits-und Gesundheitswissenschaften; Bundesanstalt für Arbeitsschutz und Arbeitsmedizin: Dortmund, Germany, 2005. [Google Scholar]
- Heath, G.; Dorrian, J.; Coates, A. Associations between shift type, sleep, mood, and diet in a group of shift working nurses. Scand. J. Work. Environ. Health 2019, 45, 402–412. [Google Scholar] [CrossRef]
- Simonetti, V.; Durante, A.; Ambrosca, R.; Arcadi, P.; Graziano, G.; Pucciarelli, G.; Simeone, S.; Vellone, E.; Alvaro, R.; Cicolini, G. Anxiety, sleep disorders and self-efficacy among nurses during COVID-19 pandemic: A large cross-sectional study. J. Clin. Nurs. 2021, 30, 1360–1371. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.Q.; Zhang, R.; Lu, Y.; Liu, H.; Kong, S.; Baker, J.S.; Zhang, H. Occupational stressors, mental health, and sleep difficulty among nurses during the COVID-19 pandemic: The mediating roles of cognitive fusion and cognitive reappraisal. J. Contextual Behav. Sci. 2021, 19, 64–71. [Google Scholar] [CrossRef]
- Zheng, Y.; Wang, L.; Feng, L.; Ye, L.; Zhang, A.; Fan, R. Sleep quality and mental health of medical workers during the coronavirus disease 2019 pandemic. Sleep Biol. Rhythm. 2021, 1–8. [Google Scholar] [CrossRef]
- Al Maqbali, M.; Al Sinani, M.; Al-Lenjawi, B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: A systematic review and meta-analysis. J. Psychosom. Res. 2021, 141, 110343. [Google Scholar] [CrossRef]
- Puci, M.V.; Nosari, G.; Loi, F.; Puci, G.V.; Montomoli, C.; Ferraro, O.E. Risk Perception and Worries among Health Care Workers in the COVID-19 Pandemic: Findings from an Italian Survey. Healthcare 2020, 8, 535. [Google Scholar] [CrossRef]
- Teddlie, C.; Yu, F. Mixed methods sampling: A typology with examples. J. Mix. Methods Res. 2007, 1, 77–100. [Google Scholar] [CrossRef]
- Witzel, A. Verfahren der qualitativen Sozialforschung. Überblick und Alternativen; Campus: Frankfurt, Germany; New York, NY, USA, 1982. [Google Scholar]
- Witzel, A.; Reiter, H. The Problem-Centred Interview; SAGE: London, UK, 2012. [Google Scholar]
- Misoch, S. Qualitative Interviews; De Gruyter: Oldenburg, Germany, 2015. [Google Scholar]
- Hetzmann, M.S.; Mojtahedzadeh, N.; Nienhaus, A.; Harth, V.; Mache, S. Occupational Health and Safety Measures in German Outpatient Care Services during the COVID-19 Pandemic: A Qualitative Study. Int. J. Environ. Res. Public Health 2021, 18, 2987. [Google Scholar] [CrossRef] [PubMed]
- Mojtahedzadeh, N.; Wirth, T.; Nienhaus, A.; Harth, V.; Mache, S. Job Demands, Resources and Strains of Outpatient Caregivers during the COVID-19 Pandemic in Germany: A Qualitative Study. Int. J. Environ. Res. Public Health 2021, 18, 3684. [Google Scholar] [CrossRef]
- VERBI Software MAXQDA 2020 [Computer Software]; VERBI Software: Berlin, Germany, 2019.
- Mayring, P. Qualitative Inhaltsanalyse [Qualitative content analysis]. Forum Qual. Soc. Res. 2000, 1. [Google Scholar] [CrossRef]
- World Health Organization. Body mass inde-BMI. Available online: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (accessed on 3 May 2021).
- Bruno, E.; Manoukian, S.; Venturelli, E.; Oliverio, A.; Rovera, F.; Iula, G.; Morelli, D.; Peissel, B.; Azzolini, J.; Roveda, E.; et al. Adherence to Mediterranean Diet and Metabolic Syndrome in BRCA Mutation Carriers. Integr. Cancer Ther. 2018, 17, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Hebestreit, K.; Yahiaoui-Doktor, M.; Engel, C.; Vetter, W.; Siniatchkin, M.; Erickson, N.; Halle, M.; Kiechle, M.; Bischoff, S.C. Validation of the German version of the Mediterranean Diet Adherence Screener (MEDAS) questionnaire. BMC Cancer 2017, 17, 341. [Google Scholar] [CrossRef] [PubMed]
- Kiechle, M.; Dukatz, R.; Yahiaoui-Doktor, M.; Berling, A.; Basrai, M.; Staiger, V.; Niederberger, U.; Marter, N.; Lammert, J.; Grill, S.; et al. Feasibility of structured endurance training and Mediterranean diet in BRCA1 and BRCA2 mutation carriers—An interventional randomized controlled multicenter trial (LIBRE-1). BMC Cancer 2017, 17, 752. [Google Scholar] [CrossRef] [PubMed]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef] [PubMed]
- Schröder, H.; Fitó, M.; Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Lamuela-Raventós, R.; Ros, E.; Salaverría, I.; Fiol, M.; et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deutsche Gesellschaft für Ernährung e.V. Presseinformation der Deutschen Gesellschaft für Ernährung e.V. Available online: https://www.dge.de/uploads/media/DGE-Pressemeldung-intern-09-2017-10R-aktualisiert.pdf (accessed on 20 May 2021).
- Bull, S.; Brown, T.; Burnett, K.; Ashdown, L.; Rushton, L. Extensive literature search as preparatory work for the safety assessment for caffeine. EFSA Supporting Publ. 2015, 12, 561E. [Google Scholar] [CrossRef]
- Wanner, M.; Hartmann, C.; Pestoni, G.; Martin, B.W.; Siegrist, M.; Martin-Diener, E. Validation of the Global Physical Activity Questionnaire for self-administration in a European context. BMJ Open Sport Amp Exerc. Med. 2017, 3, e000206. [Google Scholar] [CrossRef] [Green Version]
- Bull, F.C.; Maslin, T.S.; Armstrong, T. Global physical activity questionnaire (GPAQ): Nine country reliability and validity study. J. Phys. Act. Health 2009, 6, 790–804. [Google Scholar] [CrossRef] [Green Version]
- Aguilar-Farias, N.; Leppe Zamora, J. Is a single question of the Global Physical Activity Questionnaire (GPAQ) valid for measuring sedentary behaviour in the Chilean population? J. Sports Sci. 2017, 35, 1652–1657. [Google Scholar] [CrossRef] [PubMed]
- Mumu, S.J.; Ali, L.; Barnett, A.; Merom, D. Validity of the global physical activity questionnaire (GPAQ) in Bangladesh. BMC Public Health 2017, 17, 650. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Courten, M.d. Developing a Simple Global Physical Activity Questionnaire for Population Studies. Australas. Epidemiol. 2002, 9, 6–9. [Google Scholar]
- Surveillance and Population-Based Prevention; Prevention of Noncommunicable Diseases Department; World Health Organization. Global Physical Activity Questionnaire (GPAQ). Analysis Guide. Available online: https://www.who.int/ncds/surveillance/steps/resources/GPAQ_Analysis_Guide.pdf (accessed on 3 May 2021).
- Latza, U.; Hoffmann, W.; Terschüren, C.; Chang-Claude, J.; Kreuzer, M.; Schaffrath Rosario, A.; Kropp, S.; Stang, A.; Ahrens, W.; Lampert, T. Erhebung, Quantifizierung und Analyse der Rauchexposition in Epidemiologischen Studien. 2005. Available online: https://www.rki.de/DE/Content/Gesundheitsmonitoring/Themen/Rauchen/Rauchexposition_epidstudien.pdf%3F__blob%3DpublicationFile (accessed on 26 July 2021).
- Piper, M.E.; Baker, T.B.; Benowitz, N.L.; Smith, S.S.; Jorenby, D.E. E-cigarette Dependence Measures in Dual Users: Reliability and Relations With Dependence Criteria and E-cigarette Cessation. Nicotine Tob. Res. 2019, 22, 756–763. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Rosenthal, R.; DiMatteo, M.R. Meta-analysis: Recent developments in quantitative methods for literature reviews. Annu. Rev. Psychol. 2001, 52, 59–82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bortz, A.E. Basic Statistical Concepts, 4th ed.; Upper Saddle River: Merrill, NJ, USA, 1999. [Google Scholar]
- Bamberg, E.; Keller, M.; Wohlert, C.; Zeh, A. BGW-Stresskonzept: Das arbeitspsychologische Stressmodell; Berufsgenossenschaft für Gesundheitsdienst und Wohlfahrtspflege (BGW): Hamburg, Germany, 2012. [Google Scholar]
- Bleses, P.; Jahns, K. Soziale Innovationen in der ambulanten Pflege. In Zusammen-Arbeit-Gestalten. Soziale Innovationen in Sozialen und Gesundheitsbezogenen Dienstleistungen, 1st ed.; Becke, G., Bleses, P., Freirichs, F., Goldmann, M., Hinding, B., Schweer, M.K.W., Eds.; Springer VS: Wiesbaden, Germany, 2016; pp. 127–144. [Google Scholar]
- Kuckartz, U. Mixed Methods. Methodologie, Forschungsdesigns und Analyseverfahren; Springer VS: Wiesbaden, Germany, 2014. [Google Scholar]
- Kuckartz, U. Datenanalyse in der Mixed-Methods-Forschung. KZfSS Kölner Z. Für Soziologie Und Soz. 2017, 69, 157–183. [Google Scholar] [CrossRef]
- Creswell, J.W.; Plano Clark, V.L. Designing and Conducting Mixed Methods Research; SAGE: Thousand Oaks, CA, USA, 2007. [Google Scholar]
- Gomes, C.M.; Favorito, L.A.; Henriques, J.V.T.; Canalini, A.F.; Anzolch, K.M.J.; Fernandes, R.d.C.; Bellucci, C.H.S.; Silva, C.S.; Wroclawski, M.L.; Pompeo, A.C.L.; et al. Impact of COVID-19 on clinical practice, income, health and lifestyle behavior of Brazilian urologists. Int. Braz J. Urol. 2020, 46, 1042–1071. [Google Scholar] [CrossRef]
- Kochuvilayil, T.; Fernandez, R.S.; Moxham, L.J.; Lord, H.; Alomari, A.; Hunt, L.; Middleton, R.; Halcomb, E.J. COVID-19: Knowledge, anxiety, academic concerns and preventative behaviours among Australian and Indian undergraduate nursing students: A cross-sectional study. J. Clin. Nurs. 2021, 30, 882–891. [Google Scholar] [CrossRef] [PubMed]
- de Pinho, L.G.; Sampaio, F.; Sequeira, C.; Teixeira, L.; Fonseca, C.; Lopes, M.J. Portuguese Nurses’ Stress, Anxiety, and Depression Reduction Strategies during the COVID-19 Outbreak. Int. J. Environ. Res. Public Health 2021, 18, 3490. [Google Scholar] [CrossRef] [PubMed]
- Gifkins, J.; Jophnston, A.; Loudoun, R. The impact of shift work on eating patterns and self-care strategies utilised by experienced and inexperienced nurses. Chronobiol. Int. 2018, 35, 811–820. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Centofanti, S.; Banks, S.; Colella, A.; Dingle, C.; Devine, L.; Galindo, H.; Pantelios, S.; Brkic, G.; Dorrian, J. Coping with shift work-related circadian disruption: A mixed-methods case study on napping and caffeine use in Australian nurses and midwives. Chronobiol. Int. 2018, 35, 853–864. [Google Scholar] [CrossRef]
- Dorrian, J.; Paterson, J.; Dawson, D.; Pincombe, J.; Grech, C.; Rogers, A.E. Sleep, stress and compensatory behaviours in Australian nurses and midwives. Rev. Saude Publica 2017, 45, 922–930. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, A. Effects of caffeine on human behavior. Food Chem. Toxicol. 2002, 40, 1243–1255. [Google Scholar] [CrossRef]
- Bundesministerium für Gesundheit. Gesundheitsförderung für Pflegekräfte: Wer Pflegt die Pflege? Ausgangslage: Die Arbeitssituation in der Pflege, 3rd ed.; Bundesministerium für Gesundheit: Berlin, Germany, 2017. [Google Scholar]
- Lim, S.; Tellez, M.; Ismail, A.I. Chronic Stress and Unhealthy Dietary Behaviors among Low-Income African-American Female Caregivers. Curr. Dev. Nutr. 2020, 4. [Google Scholar] [CrossRef] [PubMed]
- Pierce, H.M.; Perry, L.; Gallagher, R.; Chiarelli, P. Delaying voiding, limiting fluids, urinary symptoms, and work productivity: A survey of female nurses and midwives. J. Adv. Nurs. 2019, 75, 2579–2590. [Google Scholar] [CrossRef] [PubMed]
- Schreck, J.H.; Lashaki, M.J.; Hashemi, J.; Dhanak, M.; Verma, S. Aerosol generation in public restrooms. Phys. Fluids 2021, 33, 033320. [Google Scholar] [CrossRef]
- Mojtahedzadeh, N.; Neumann, F.A.; Augustin, M.; Zyriax, B.-C.; Harth, V.; Mache, S. Das Gesundheitsverhalten von Pflegekräften—Aktueller Forschungsstand, Potenziale und mögliche Herausforderungen. Prävention Und. Gesundh. 2020, 16, 16–20. [Google Scholar] [CrossRef]
- Neill, E.; Meyer, D.; Toh, W.L.; van Rheenen, T.E.; Phillipou, A.; Tan, E.J.; Rossell, S.L. Alcohol use in Australia during the early days of the COVID-19 pandemic: Initial results from the COLLATE project. Psychiatry Clin. Neurosci. 2020, 74, 542–549. [Google Scholar] [CrossRef]
- Škrlec, I.; Talapko, J.; Pustijanac, E.; Meštrović, T. Depression, Anxiety, Stress and Physical Activity in Health-Related University Students during COVID-19. Proceedings 2021, 1–6. [Google Scholar] [CrossRef]
- Que, J.; Shi, L.; Deng, J.; Liu, J.; Zhang, L.; Wu, S.; Gong, Y.; Huang, W.; Yuan, K.; Yan, W.; et al. Psychological impact of the COVID-19 pandemic on healthcare workers: A cross-sectional study in China. Gen. Psychiatr. 2020, 33, e100259. [Google Scholar] [CrossRef]
- Shechter, A.; Diaz, F.; Moise, N.; Anstey, D.E.; Ye, S.; Agarwal, S.; Birk, J.L.; Brodie, D.; Cannone, D.E.; Chang, B.; et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen. Hosp. Psychiatry 2020, 66, 1–8. [Google Scholar] [CrossRef]
- Pinho, L.; Correia, T.; Sampaio, F.; Sequeira, C.; Teixeira, L.; Lopes, M.; Fonseca, C. The use of mental health promotion strategies by nurses to reduce anxiety, stress, and depression during the COVID-19 outbreak: A prospective cohort study. Environ. Res. 2021, 195, 110828. [Google Scholar] [CrossRef]
- Silva-Costa, A.; Harter Griep, R.; Fischer, F.M.; Rotenberg, L. Need for recovery from work and sleep-related complaints among nursing professionals. Work 2012, 41, 3726–3731. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heidke, P.; Madsen, W.L.; Langham, E.M. Registered nurses as role models for healthy lifestyles. Aust. J. Adv. Nurs. 2020, 37, 11–18. [Google Scholar] [CrossRef] [Green Version]
- Edwards, R.; Tu, D.; Stanley, J.; Martin, G.; Gifford, H.; Newcombe, R. Smoking prevalence among doctors and nurses—2013 New Zealand census data. N. Z. Med. Assoc. J. 2018, 131, 48–57. [Google Scholar]
- Pan American Health Organization. Protecting Mental Health during Epidemics. 2009. Available online: https://www.paho.org/en/documents/protecting-mental-health-during-epidemics (accessed on 26 July 2021).
- An, Y.; Yang, Y.; Wang, A.; Li, Y.; Zhang, Q.; Cheung, T.; Ungvari, G.S.; Qin, M.-Z.; An, F.-R.; Xiang, Y.-T. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J. Affect. Disord. 2020, 276, 312–315. [Google Scholar] [CrossRef]
- Bundesanstalt für Arbeitsschutz und Arbeitsmedizin. Arbeit in der Pflege—Arbeit am Limit? Arbeitsbedingungen in der Pflegebranche. BIBB/BAuA-Faktenblatt 10; Bundesanstalt für Arbeitsschutz und Arbeitsmedizin: Dortmund, Germany, 2014; p. 2. [Google Scholar]
- Arbeitszeitgesetz (ArbZG). Arbeitszeitgesetz vom 6. Juni 1994 (BGBl. I S. 1170, 1171), das Zuletzt Durch. Artikel 6 des Gesetzes vom 22. Dezember 2020 (BGBl. I S. 3334) geändert worden ist. 1994. Available online: https://www.gesetze-im-internet.de/arbzg/BJNR117100994.html#BJNR117100994BJNG000100307 (accessed on 26 July 2021).
- Lohmann-Haislah, A.; Wendsche, J.; Schulz, A.; Schöllgen, I.; Escobar Pinzon, L.C. Einflussfaktoren und Folgen des Ausfalls gesetzlicher Ruhepausen bei Pflegekräften in Deutschland. Z. Arb. 2019, 73, 418–438. [Google Scholar] [CrossRef]
- Wendsche, J.; Ghadiri, A.; Bengsch, A.; Wegge, J. Antecedents and outcomes of nurses’ rest break organization: A scoping review. Int. J. Nurs. Stud. 2017, 75, 65–80. [Google Scholar] [CrossRef]
- Sarna, L.; Aguinaga Bialous, S.; Wells, M.J.; Kotlerman, J.; Sivarajan, F.E.; Wewers, M.E. Do You Need to Smoke to Get a Break?: Smoking Status and Missed Work Breaks Among Staff Nurses. Am. J. Prev. Med. 2009, 37, 165–171. [Google Scholar] [CrossRef]
- Sarna, L.; Aguinaga Bialous, S.; Wewers, M.E.; Sivarajan Froehlicher, E.; Danao, L. Nurses, smoking, and the workplace. Res. Nurs. Health 2004, 28, 79–90. [Google Scholar] [CrossRef]
- Romero-Blanco, C.; Rodríguez-Almagro, J.; Onieva-Zafra, M.D.; Parra-Fernández, M.L.; Prado-Laguna, M.d.C.; Hernández-Martínez, A. Sleep Pattern Changes in Nursing Students during the COVID-19 Lockdown. Int. J. Environ. Res. Public Health 2020, 17, 5222. [Google Scholar] [CrossRef]
- Jahrami, H.; BaHammam, A.S.; AlGahtani, H.; Ebrahim, A.; Faris, M.; AlEid, K.; Saif, Z.; Haji, E.; Dhahi, A.; Marzooq, H.; et al. The examination of sleep quality for frontline healthcare workers during the outbreak of COVID-19. Sleep Breath. 2021, 25, 503–511. [Google Scholar] [CrossRef]
- Lin, S.-H.; Liao, W.-C.; Chen, M.-Y.; Fan, J.-Y. The impact of shift work on nurses’ job stress, sleep quality and self-perceived health status. J. Nurs. Manag. 2014, 22, 604–612. [Google Scholar] [CrossRef]
- Zverev, Y.P.; Misiri, H.E. Perceived effects of rotating shift work on nurses\’ sleep quality and duration. Malawi Med. J. 2009, 21, 19–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heath, G.; Roach, G.D.; Dorrian, J.; Ferguson, S.A.; Darwent, D.; Sargent, C. The effect of sleep restriction on snacking behaviour during a week of simulated shiftwork. Accid. Anal. Prev. 2012, 45, 62–67. [Google Scholar] [CrossRef]
- Bundesregierung, P.-u.I.d. Telefonschaltkonferenz der Bundeskanzlerin mit den Regierungschefinnen und Regierungschefs der Länder am 15. April 2020. Available online: https://www.bundesregierung.de/breg-de/suche/telefonschaltkonferenz-der-bundeskanzlerin-mit-den-regierungschefinnen-und-regierungschefs-der-laender-am-15-april-2020-1744228 (accessed on 26 July 2021).
- Rheindorf, J.; Blocker, J.; Himmel, C.; Trost, A. Wie erleben Pflegefachpersonen die Corona-Pandemie? Pflege Z. 2020, 73, 50–53. [Google Scholar] [CrossRef]
- Hennein, R.; Lowe, S. A hybrid inductive-abductive analysis of health workers’ experiences and wellbeing during the COVID-19 pandemic in the United States. PLoS ONE 2020, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Chew, N.W.S.; Lee, G.K.H.; Tan, B.Y.Q.; Jing, M.; Goh, Y.; Ngiam, N.J.H.; Yeo, L.L.L.; Ahmad, A.; Ahmed Khan, F.; Napolean Shanmugam, G.; et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain. Behav. Immun. 2020, 88, 559–565. [Google Scholar] [CrossRef]
- Zhan, Y.; Ma, S.; Jian, X.; Cao, Y.; Zhan, X. The Current Situation and Influencing Factors of Job Stress Among Frontline Nurses Assisting in Wuhan in Fighting COVID-19. Front. Public Health 2020, 8, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Blanco-Donoso, L.M.; Moreno-Jiménez, J.; Amutio, A.; Gallego-Alberto, L.; Moreno-Jiménez, B.; Garrosa, E. Stressors, Job Resources, Fear of Contagion, and Secondary Traumatic Stress Among Nursing Home Workers in Face of the COVID-19: The Case of Spain. J. Appl. Gerontol. 2020, 1–13. [Google Scholar] [CrossRef]
- Martínez-López, J.A.; Lázaro-Pérez, C.; Gómez-Galán, J.; del Mar Fernández-Martinez, M. Psychological Impact of COVID-19 Emergency on Health Professionals: Burnout Incidence at the Most Critical Period in Spain. J. Clin. Med. 2020, 9, 3029. [Google Scholar] [CrossRef]
- Preti, E.; Di Mattei, V.; Perego, G.; Ferrari, F.; Mazzetti, M.; Taranto, P.; Di Pierro, R.; Madeddu, F.; Calati, R. The Psychological Impact of Epidemic and Pandemic Outbreaks on Healthcare Workers: Rapid Review of the Evidence. Curr. Psychiatry Rep. 2020, 22, 43. [Google Scholar] [CrossRef]
- Ramaci, T.; Barattucci, M.; Ledda, C.; Rapisarda, V. Social Stigma during COVID-19 and its Impact on HCWs Outcomes. Sustainability 2020, 12, 3834. [Google Scholar] [CrossRef]
- Burisch, M. Das Burnout-Syndrom. Theorie der inneren Erschöpfung–Zahlreiche Fallbeispiele–Hilfen zur Selbsthilfe, 5th ed.; Springer: Berlin, Germany, 2014. [Google Scholar]
- Wenzel, R.P.; Bearman, G.; Edmond, M.B. Lessons from Severe Acute Respiratory Syndrome (SARS): Implications for Infection Control. Arch. Med. Res. 2005, 36, 610–616. [Google Scholar] [CrossRef]
- Robert Koch-Institut. Hinweise für Ambulante Pflegedienste im Rahmen der COVID-19-Pandemie, Stand: 23.11.2020. Available online: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Altenpflegeheime.html (accessed on 23 December 2020).
- Agarwal, A.; Ranjan, P.; Saraswat, A.; Kasi, K.; Bharadiya, V.; Vikram, N.; Singh, A.; Upadhyay, A.D.; Baitha, U.; Klanidhi, K.B.; et al. Are health care workers following preventive practices in the COVID-19 pandemic properly?—A cross-sectional survey from India. Diabetes Metab. Syndr. Clin. Res. Rev. 2021, 15, 69–75. [Google Scholar] [CrossRef]
- Powell-Jackson, T.; King, J.J.C.; Makungu, C.; Spieker, N.; Woodd, S.; Risha, P.; Goodman, C. Infection prevention and control compliance in Tanzanian outpatient facilities: A cross-sectional study with implications for the control of COVID-19. Lancet Glob. Health 2020, 8, e780–e789. [Google Scholar] [CrossRef]
- Bashirian, S.; Jenabi, E.; Khazaei, S.; Barati, M.; Karimi-Shahanjarini, A.; Zareian, S.; Rezapur-Shahkolai, F.; Moeini, B. Factors associated with preventive behaviours of COVID-19 among hospital staff in Iran in 2020: An application of the Protection Motivation Theory. J. Hosp. Infect. 2020, 105, 430–433. [Google Scholar] [CrossRef] [PubMed]
- Alsoghair, M.; Almazyad, M.; Alburaykan, T.; Alsultan, A.; Alnughaymishi, A.; Almazyad, S.; Alharbi, M.; Alkassas, W.; Almadud, A.; Alsuhaibani, M. Medical Students and COVID-19: Knowledge, Preventive Behaviors, and Risk Perception. Int. J. Environ. Res. Public Health 2021, 18, 842. [Google Scholar] [CrossRef]
- Albaqawi, H.M.; Alquwez, N.; Balay-Odao, E.; Bajet, J.B.; Alabdulaziz, H.; Alsolami, F.; Tumala, R.B.; Alsharari, A.F.; Tork, H.M.M.; Felemban, E.M.; et al. Nursing Students′ Perceptions, Knowledge, and Preventive Behaviors Toward COVID-19: A Multi-University Study. Front. Public Health 2020, 8, 573390. [Google Scholar] [CrossRef] [PubMed]
- Taghrir, M.H.; Borazjani, R.; Shiraly, R. COVID-19 and Iranian Medical Students; A Survey on Their Related-Knowledge, Preventive Behaviors and Risk Perception. Arch. Iran. Med. 2020, 23, 249–254. [Google Scholar] [CrossRef] [Green Version]
- Lai, X.; Wang, X.; Yang, Q.; Xu, X.; Tang, Y.; Liu, C.; Tan, L.; Lai, R.; Wang, H.; Zhang, X.; et al. Will healthcare workers improve infection prevention and control behaviors as COVID-19 risk emerges and increases, in China? Antimicrob. Resist. Infect. Control. 2020, 9, 83. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Advice on the use of masks in the context of COVID-19. Interim Guidance. 5 June 2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/332293/WHO-2019-nCov-IPC_Masks-2020.4-eng.pdf?sequence=1&isAllowed=y (accessed on 6 May 2021).
- Reszke, R.; Matusiak, Ł.; Krajewski, P.K.; Szepietowska, M.; Białynicki-Birula, R.; Szepietowski, J.C. The Utilization of Protective Face Masks among Polish Healthcare Workers during COVID-19 Pandemic: Do We Pass the Exam? Int. J. Environ. Res. Public Health 2021, 18, 841. [Google Scholar] [CrossRef]
- Brown, L. Use of personal protective equipment in nursing practice. Nurs. Stand. 2019, 34, 59–66. [Google Scholar] [CrossRef]
- Abukhelaif, A.E.E. Personal Protective Equipment Knowledge and Practices among Nurses Working at Al-Baha King Fahad Hospital, Saudi Arabia. J. Healthc. Commun. 2019, 4, 2. [Google Scholar] [CrossRef]
- World Health Organization; Patient Safety. WHO Guidelines on Hand Hygiene in Health Care; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Moore, L.D.; Robbins, G.; Quinn, J.; Arbogast, J.W. The impact of COVID-19 pandemic on hand hygiene performance in hospitals. Am. J. Infect. Control. 2021, 49, 30–33. [Google Scholar] [CrossRef] [PubMed]
- Huang, F.; Armando, M.; Dufau, S.; Florea, O.; Brouqui, P.; Boudjema, S. COVID-19 outbreak and healthcare worker behavioural change toward hand hygiene practices. J. Hosp. Infect. 2021, 111, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Die Bundesregierung. Corona. Das sind die Geltenden Regeln und Einschränkungen. Available online: https://www.bundesregierung.de/breg-de/themen/coronavirus/corona-diese-regeln-und-einschraenkung-gelten-1734724 (accessed on 6 May 2021).
- Yıldırım, M.; Güler, A. COVID-19 severity, self-efficacy, knowledge, preventive behaviors, and mental health in Turkey. Death Stud. 2020, 1–8. [Google Scholar] [CrossRef]
- Polit, D.F.; Beck, C.T. Is there still gender bias in nursing research? An update. Res. Nurs. Health 2013, 36, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Polit, D.F.; Beck, C.T. Is there gender bias in nursing research? Res. Nurs. Health 2008, 31, 417–427. [Google Scholar] [CrossRef]
- Polit, D.F.; Beck, C.T. International gender bias in nursing research, 2005–2006: A quantitative content analysis. Int. J. Nurs. Stud. 2009, 46, 1102–1110. [Google Scholar] [CrossRef] [Green Version]
- Bundesministerium für Gesundheit. Pflegekräfte. Beschäftigte in der Pflege. Available online: https://www.bundesgesundheitsministerium.de/themen/pflege/pflegekraefte/beschaeftigte.html (accessed on 14 August 2020).
- Scholl, A. Die Befragung, 3rd ed.; UVK Verlagsgesellschaft: Munich, Germany, 2015. [Google Scholar]
- Opdenakker, R.J.G. Advantages and Disadvantages of Four Interview Techniques in Qualitative Research. Forum Qual. Soz. Forum Qual. Soc. Res. 2006, 7. [Google Scholar] [CrossRef]
- Novick, G. Is there a bias against telephone interviews in qualitative research? Res. Nurs. Health 2008, 31, 391–398. [Google Scholar] [CrossRef] [Green Version]
- Kaiser, R. Qualitative Experteninterviews. Konzeptionelle Grundlagen und Praktische Durchführung; Springer VS: Siegen, Germany, 2014. [Google Scholar]
- Statistisches Bundesamt (Destatis). Pflegestatistik, Pflege im Rahmen der Pflegeversicherung Deutschlandergebnisse, 2019. 2020. Available online: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Pflege/Publikationen/Downloads-Pflege/pflege-deutschlandergebnisse-5224001199004.pdf;jsessionid=3E2FA409AE1ED4307CE9A6FC2386BCFF.live711?__blob=publicationFile (accessed on 26 July 2021).
- Kollamparambil, U.; Oyenubi, A. Behavioural response to the Covid-19 pandemic in South Africa. PLoS ONE 2021, 16, e0250269. [Google Scholar] [CrossRef]
- Ruiz-Fernández, M.D.; Ramos-Pichardo, J.D.; Ibáñez-Masero, O.; Cabrera-Troya, J.; Carmona-Rega, M.I.; Ortega-Galán, Á.M. Compassion fatigue, burnout, compassion satisfaction and perceived stress in healthcare professionals during the COVID-19 health crisis in Spain. J. Clin. Nurs. 2020, 29, 4321–4330. [Google Scholar] [CrossRef]
- Jacobs, D.R., Jr.; Petersen, K.S.; Svendsen, K.; Ros, E.; Sloan, C.B.; Steffen, L.M.; Tapsell, L.C.; Kris-Etherton, P.M. Considerations to facilitate a US study that replicates PREDIMED. Metabolism 2018, 85, 361–367. [Google Scholar] [CrossRef]
- Keating, X.D.; Zhou, K.; Liu, X.; Hodges, M.; Liu, J.; Guan, J.; Phelps, A.; Castro-Piñero, J. Reliability and Concurrent Validity of Global Physical Activity Questionnaire (GPAQ): A Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 4128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brener, N.D.; Billy, J.O.; Grady, W.R. Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: Evidence from the scientific literature. J. Adolesc. Health 2003, 33, 436–457. [Google Scholar] [CrossRef] [Green Version]
- Paul-Ehrlich-Institut. COVID-19 Impfstoffe. Available online: https://www.pei.de/DE/arzneimittel/impfstoffe/covid-19/covid-19-node.html (accessed on 6 May 2021).
- Bundesministerium für Gesundheit. Verordnung zum Anspruch auf Schutzimpfung Gegen das Coronavirus SARS-CoV-2 (Coronavirus-Impfverordnung–CoronaImpfV). Available online: https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/3_Downloads/C/Coronavirus/Verordnungen/CoronaImpfV_BAnz_AT_08.02.2021_V1.pdf (accessed on 6 May 2021).
- Mojtahedzadeh, N.; Neumann, F.A.; Rohwer, E.; Augustin, M.; Zyriax, B.-C.; Harth, V.; Mache, S. Betriebliche Gesundheitsförderung in der Pflege. Prävention Gesundh. 2021, 16, 163–169. [Google Scholar] [CrossRef]
- Brandenburg, U.; Nieder, P. Betriebliches Fehlzeiten-Management. Instrumente und Praxisbeispiele für Erfolgreiches Anwesenheits-und Vertrauensmanagement, 2nd ed.; Gabler: Wiesbaden, Germany, 2009. [Google Scholar]
- Badura, B.; Hehlmann, T. Gesundheit, Verhalten, Organisation. In Betriebliche Gesundheitspolitik. der Weg zur gesunden Organisation; Badura, B., Hehlmann, T., Eds.; Springer: Berlin/Heidelberg, Germany, 2003; pp. 13–58. [Google Scholar]
- Riedel-Heller, S.G.; Luppa, M.; Seidler, A.; Becker, T.; Stengler, K. Psychische Gesundheit und Arbeit. Konzepte, Evidenz und Implikationen für Forschung und Praxis. Nervenarzt 2013, 84, 832–837. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H.; Consortium Health Literacy Project, E. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [Green Version]
- Stefan, N.; Birkenfeld, A.L.; Schulze, M.B.; Ludwig, D.S. Obesity and impaired metabolic health in patients with COVID-19. Nat. Rev. Endocrinol. 2020, 16, 341–342. [Google Scholar] [CrossRef] [Green Version]
- Hu, X.; Pan, X.; Zhou, W.; Gu, X.; Shen, F.; Yang, B.; Hu, Z. Clinical epidemiological analyses of overweight/obesity and abnormal liver function contributing to prolonged hospitalization in patients infected with COVID-19. Int. J. Obes. 2020, 44, 1784–1789. [Google Scholar] [CrossRef]
- Rychter, A.M.; Zawada, A.; Ratajczak, A.E.; Dobrowolska, A.; Krela-Kaźmierczak, I. Should patients with obesity be more afraid of COVID-19? Obes. Rev. 2020, 21, e13083. [Google Scholar] [CrossRef]
- Albashir, A.A.D. The potential impacts of obesity on COVID-19. Clin. Med. 2020, 20, e109–e113. [Google Scholar] [CrossRef]
- World Health Organization. Tobacco. Available online: https://www.who.int/news-room/fact-sheets/detail/tobacco (accessed on 15 April 2021).
- Kamisli, S.; Öz, F. Evalution of a Smoking Cessation Psychoeducational Program for Nurses. J. Addict. Nurs. 2011, 22, 117–123. [Google Scholar] [CrossRef]
- World Health Organization. Global Strategy on Diet., Physical Activity and Health. Physical Activity. 2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/20142/A57_R17bis-en.pdf?sequence=3&isAllowed=y (accessed on 26 July 2021).
- Wendsche, J.; Lohmann-Haislah, A. Psychische Gesundheit in der Arbeitswelt: Pausen; Bundesanstalt für Arbeitsschutz und Arbeitsmedizin (BAuA): Dortmund, Germany; Berlin, Germany; Dresden, Germany, 2016. [Google Scholar]
- Blasche, G.; Pasalic, S.; Bauböck, V.-M.; Haluza, D.; Schoberberger, R. Effects of Rest-Break Intention on Rest-Break Frequency and Work-Related Fatigue. Hum. Factors 2017, 59, 289–298. [Google Scholar] [CrossRef] [PubMed]
- Tucker, P. The impact of rest breaks upon accident risk, fatigue and performance: A review. Work Stress 2003, 17, 123–137. [Google Scholar] [CrossRef]
- McDowall, K.; Murphy, E.; Anderson, K. The impact of shift work on sleep quality among nurses. Occup. Med. 2017, 67, 621–625. [Google Scholar] [CrossRef] [Green Version]
- Deng, X.; Liu, X.; Fang, R. Evaluation of the correlation between job stress and sleep quality in community nurses. Medicine 2020, 99, e18822. [Google Scholar] [CrossRef]
- Lally, P.; van Jaarsveld, C.M.; Potts, H.W.W.; Wardle, J. How are habits formed: Modelling habit formation in the real world. Eur. J. Soc. Psychol. 2010, 40, 998–1009. [Google Scholar] [CrossRef] [Green Version]
- Badura, B.; Walter, U.; Hehlmann, T. Die Vision der gesunden Organisation. In Betriebliche Gesundheitspolitik. Der Weg zur gesunden Organisation, 2nd ed.; Badura, B., Walter, U., Hehlmann, T., Eds.; Springer: Heidelberg, Germany, 2010; pp. 31–40. [Google Scholar]
- Dovey, T.M. Eating Behaviour; McGraw Hill: Berkshire, Germany, 2010. [Google Scholar]
- Robert Koch-Institut. Hinweise zu Reinigung und Desinfektion von Ober flächen außerhalb von Gesundheits Einrichtungen im Zusammen Hang mit der COVID-19-Pandemie. Available online: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Reinigung_Desinfektion.html (accessed on 6 May 2021).
- Torquati, L.; Kolbe-Alexander, T.; Pavey, T.; Persson, C.; Leveritt, M. Diet and physical activity behaviour in nurses: A qualitative study. Int. J. Health Promot. Educ. 2016, 54, 268–282. [Google Scholar] [CrossRef] [Green Version]
- Power, B.T.; Kiezebrink, K.; Allan, J.L.; Campbell, M.K. Understanding perceived determinants of nurses’eating and physical activity behaviour: A theory-informed qualitative interview study. BMC Obes. 2017, 4, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Peplonska, B.; Bukowska, A.; Sobala, W. Rotating night shift work and physical activity of nurses and midwives in the cross-sectional study in Łódź, Poland. Chronobiol. Int. 2014, 31, 1152–1159. [Google Scholar] [CrossRef]
- da Costa Fernandes, J.; Fernandes Portela, L.; Rotenberg, L.; Harter Griep, R. Jornada de trabajo y comportamientos de salud entre enfermeros de hospitales públicos. Rev. Lat. Am. Enferm. 2013, 21. [Google Scholar] [CrossRef] [Green Version]
- Bundesministerium für Gesundheit. Gesundheitsförderung für Pflegekräfte: Wer pflegt die Pflege? Lösungsansatz: Betriebliche Gesundheitsförderung für Pflegekräfte; Bundesministerium für Gesundheit: Berlin, Germany, 2017. [Google Scholar]
- Fang, R.; Li, X. A regular yoga intervention for staff nurse sleep quality and work stress: A randomised controlled trial. J. Clin. Nurs. 2015, 24, 3374–3379. [Google Scholar] [CrossRef] [PubMed]
- Reddy, R.K.; Charles, W.N.; Sklavounos, A.; Dutt, A.; Seed, P.T.; Khajuria, A. The effect of smoking on COVID-19 severity: A systematic review and meta-analysis. J. Med. Virol. 2021, 93, 1045–1056. [Google Scholar] [CrossRef]
- Eisenberg, S.-L.; Eisenberg, M.J. Smoking Cessation During the COVID-19 Epidemic. Nicotine Tob. Res. 2020, 22, 1664–1665. [Google Scholar] [CrossRef] [PubMed]
- Patanavanich, R.; Glantz, S.A. Smoking Is Associated With COVID-19 Progression: A Meta-analysis. Nicotine Tob. Res. 2020, 22, 1653–1656. [Google Scholar] [CrossRef] [PubMed]
- Richter, P.; Wegge, J. Occupational Health Psychology–Gegenstand, Modelle, Aufgaben. In Klinische Psychologie & Psychotherapie – Ein Lehrbuch, 2nd ed.; Wittchen, H.-U., Hoyer, J., Eds.; Springer Verlag: Berlin, Germany, 2011; pp. 337–357. [Google Scholar]
- Badura, B.; Greiner, W.; Rixgens, P.; Ueberle, M.; Behr, M. Sozialkapital–Grundlagen von Gesundheit und Unternehmenserfolg, 2nd ed.; Springer: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Bradtke, E.; Clauss, E.; Ernst, C.; Gregersen, S.; Huxholl, H.; Schwarzmann, K.; Taskan-Karamürsel, E.; Theiler, A. Sachgebiet Psyche und Gesundheit in der Arbeitswelt. Psychische Belastung und Beanspruchung von Beschäftigten im Gesundheitsdienst Während der Coronavirus-Pandemie; Deutsche Gesetzliche Unfallversicherung e.V. (DGUV): Berlin, Germany, 2020. [Google Scholar]
- Said, R.M.; El-Shafei, D.A. Occupational stress, job satisfaction, and intent to leave: Nurses working on front lines during COVID-19 pandemic in Zagazig City, Egypt. Environ. Sci. Pollut. Res. 2021, 28, 8791–8801. [Google Scholar] [CrossRef] [PubMed]
- Bamberg, E.; Ducki, A.; Greiner, B. Betriebliche Gesundheitsförderung: Theorie und Praxis, Anspruch und Realität. In Betriebliche Gesundheitsförderung: Problembezogene Psychologische Interventionen; Steffgen, G., Ed.; Hogrefe Verlag: Göttingen, Germany, 2004; pp. 11–35. [Google Scholar]
| Sample Characteristics | n |
|---|---|
| Gender | |
| Female | 12 |
| Male | 3 |
| Age (years) | |
| 20–30 | 2 |
| 31–40 | 7 |
| ≥41 | 6 |
| Children in household | |
| 0 | 9 |
| ≥1 | 6 |
| Date of Interview | |
| May 2020 | 9 |
| June 2020 | 6 |
| Qualification | |
| Caregiver | 1 |
| Geriatric nurse | 8 |
| Home and family care | 1 |
| Healthcare and nursing staff | 1 |
| Social manager | 1 |
| Geriatric nurse, additional qualification intensive and palliative care | 1 |
| Wound expert | 1 |
| Geriatric nurse and wound expert | 1 |
| Occupation | |
| Outpatient geriatric nurse | 8 |
| Outpatient home and family caregiver | 1 |
| Outpatient caregiver | 2 |
| Outpatient geriatric nurse and office manager in health sector | 1 |
| Care specialist and nutrition manager in the outpatient care | 1 |
| Care specialist and deputy care management in the outpatient care | 1 |
| Outpatient geriatric nurse and wound expert | 1 |
| Work experience (years) | |
| <1 | 2 |
| 1–5 | 5 |
| >5 | 8 |
| Work Schedule | |
| Full-time | 13 |
| Part-time | 2 |
| Sample Characteristics | n (%) |
|---|---|
| Gender | |
| Male | 57 (33.3%) |
| Female | 112 (65.5%) |
| Diverse | 2 (1.2%) |
| Age (years) | |
| 18–29 | 18 (10.5%) |
| 30–39 | 55 (32.2%) |
| 40–49 | 40 (23.4%) |
| 50–59 | 44 (25.7%) |
| ≥60 | 14 (8.2%) |
| Origin | |
| German Parents | 132 (77.2%) |
| Migration Background | 39 (22.8%) |
| Highest Education Level | |
| General Secondary School | 18 (10.5%) |
| Intermediate Secondary School | 87 (50.9%) |
| Specialised Grammer School | 21 (12.3%) |
| Grammar School | 45 (26.3%) |
| BMI | |
| Normal Weight | 101 (59.1 %) |
| Overweight | 40 (23.4 %) |
| Obese | 30 (17.5 %) |
| Health Behaviour | M | SD | Z a | p | r b | 95% CI |
|---|---|---|---|---|---|---|
| Eating Behaviour | −0.19 | 0.85 | −2.89 | 0.004 | 0.22 | [−0.32, −0.06] |
| Physical Activity | −0.37 | 0.87 | −5.51 | <0.001 | 0.42 | [−0.50, −0.24] |
| Smoking | 0.02 | 0.73 | 0.18 | 0.855 | - | [−0.09, 0.13] |
| Perceived Stress | 0.41 | 1.22 | 4.40 | <0.001 | 0.34 | [0.23, 0.59] |
| Sleep Quality | −0.65 | 0.80 | −10.60 | <0.001 | 0.81 | [−0.77, −0.53] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mojtahedzadeh, N.; Neumann, F.A.; Rohwer, E.; Nienhaus, A.; Augustin, M.; Harth, V.; Zyriax, B.-C.; Mache, S. The Health Behaviour of German Outpatient Caregivers in Relation to the COVID-19 Pandemic: A Mixed-Methods Study. Int. J. Environ. Res. Public Health 2021, 18, 8213. https://doi.org/10.3390/ijerph18158213
Mojtahedzadeh N, Neumann FA, Rohwer E, Nienhaus A, Augustin M, Harth V, Zyriax B-C, Mache S. The Health Behaviour of German Outpatient Caregivers in Relation to the COVID-19 Pandemic: A Mixed-Methods Study. International Journal of Environmental Research and Public Health. 2021; 18(15):8213. https://doi.org/10.3390/ijerph18158213
Chicago/Turabian StyleMojtahedzadeh, Natascha, Felix Alexander Neumann, Elisabeth Rohwer, Albert Nienhaus, Matthias Augustin, Volker Harth, Birgit-Christiane Zyriax, and Stefanie Mache. 2021. "The Health Behaviour of German Outpatient Caregivers in Relation to the COVID-19 Pandemic: A Mixed-Methods Study" International Journal of Environmental Research and Public Health 18, no. 15: 8213. https://doi.org/10.3390/ijerph18158213
APA StyleMojtahedzadeh, N., Neumann, F. A., Rohwer, E., Nienhaus, A., Augustin, M., Harth, V., Zyriax, B.-C., & Mache, S. (2021). The Health Behaviour of German Outpatient Caregivers in Relation to the COVID-19 Pandemic: A Mixed-Methods Study. International Journal of Environmental Research and Public Health, 18(15), 8213. https://doi.org/10.3390/ijerph18158213








