Factors Influencing Physician Decision Making to Attempt Advanced Resuscitation in Asystolic Out-of-Hospital Cardiac Arrest
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Prehospital Management of OHCA and Decisions
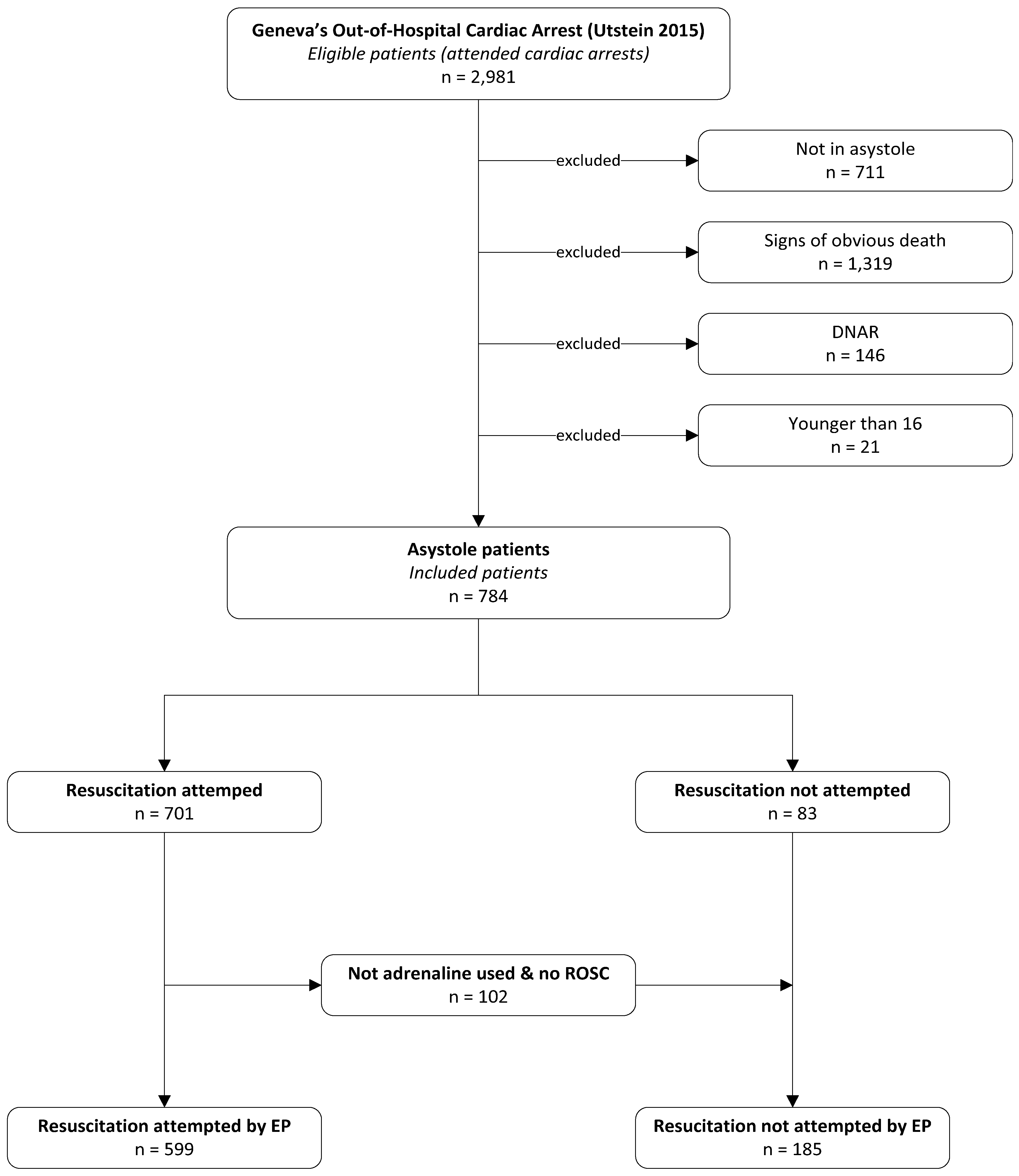
2.3. Study Population
2.4. Variables
2.5. Statistical Analysis
2.6. Patients and Public Involvement
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Anderson, N.E.; Gott, M.; Slark, J. Commence, continue, withhold or terminate?: A systematic review of decision-making in out-of-hospital cardiac arrest. Euro. J. Emer. Med. 2017, 24, 80–86. [Google Scholar] [CrossRef]
- Anderson, N.E.; Slark, J.; Gott, M. Prehospital Resuscitation Decision Making: A model of ambulance personnel experiences, preparation and support. Emerg. Med. Australas. 2021, 33, 697–702. [Google Scholar] [CrossRef]
- Mancini, M.E.; Diekema, D.S.; Hoadley, T.A.; Kadlec, K.D.; Leveille, M.H.; McGowan, J.E.; Munkwitz, M.M.; Panchal, A.R.; Sayre, M.R.; Sinz, E.H. Part 3: Ethical Issues. 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015, 132, S383–S396. [Google Scholar] [CrossRef]
- Bossaert, L.L.; Perkins, G.D.; Askitopoulou, H.; Raffay, V.I.; Greif, R.; Haywood, K.L.; Mentzelopoulos, S.D.; Nolan, J.P.; Van de Voorde, P.; Xanthos, T.T.; et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 11. The ethics of resuscitation and end-of-life decisions. Resuscitation 2015, 95, 302–311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Panchal, A.R.; Bartos, J.A.; Cabañas, J.G.; Donnino, M.W.; Drennan, I.R.; Hirsch, K.G.; Kudenchuk, P.J.; Kurz, M.C.; Lavonas, E.J.; Morley, P.T.; et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S366–S468. [Google Scholar] [CrossRef]
- Soar, J.; Nolan, J.P.; Böttiger, B.W.; Perkins, G.D.; Lott, C.; Carli, P.; Pellis, T.; Sandroni, C.; Skrifvars, M.B.; Smith, G.B.; et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 3. Adult advanced life support. Resuscitation 2015, 95, 100–147. [Google Scholar] [CrossRef] [Green Version]
- Embong, H.; Md, I.S.A.; Harunarashid, H.; Abd Samat, A.H. Factors associated with prolonged cardiopulmonary resuscitation attempts in out-of-hospital cardiac arrest patients presenting to the emergency department. Australas. Emerg. Care 2020, 24, 84–88. [Google Scholar] [CrossRef]
- Patel, F. Recognition of life extinct (ROLE)—Multidiscipline role of healthcare professionals. J. Foren. Legal Med. 2008, 15, 359–362. [Google Scholar] [CrossRef] [PubMed]
- Lockey, A.S. Recognition of death and termination of cardiac resuscitation attempts by UK ambulance personnel. Emerg. Med. J. 2002, 19, 345–347. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, T.; Woollard, M. Paramedic accuracy in using a decision support algorithm when recognising adult death: A prospective cohort study. Emerg. Med. J. 2003, 20, 473–475. [Google Scholar] [CrossRef] [PubMed]
- Rajagopal, S.; Kaye, C.R.; Lall, R.; Deakin, C.D.; Gates, S.; Pocock, H.; Quinn, T.; Rees, N.; Smyth, M.; Perkins, G.D. Characteristics of patients who are not resuscitated in out of hospital cardiac arrests and opportunities to improve community response to cardiac arrest. Resuscitation 2016, 109, 110–115. [Google Scholar] [CrossRef] [Green Version]
- Kämäräinen, A.; Virkkunen, I.; Yli-Hankala, A.; Silfvast, T. Presumed futility in paramedic-treated out-of-hospital cardiac arrest: An Utstein style analysis in Tampere, Finland. Resuscitation 2007, 75, 235–243. [Google Scholar] [CrossRef]
- Kind, C.; Berner, D.; Brauer, S.; Flotron, S.; Gutscher, H.; Hürlimann, D.; Hurst, S.; Kunz, R.; Monteverde, S.; Neuenschwander, H.; et al. Attitude Towards the End-of-Life or Death; Académie Suisse des Sciences Médicales (ASSM): Bern, Switzerland, 2018; pp. 1–36. [Google Scholar]
- Morrison, L.J.; Visentin, L.M.; Kiss, A.; Theriault, R.; Eby, D.; Vermeulen, M.; Sherbino, J.; Verbeek, P.R. Validation of a rule for termination of resuscitation in out-of-hospital cardiac arrest. N. Engl. J. Med. 2006, 355, 478–487. [Google Scholar] [CrossRef]
- Ebell, M.H.; Vellinga, A.; Masterson, S.; Yun, P. Meta-analysis of the accuracy of termination of resuscitation rules for out-of-hospital cardiac arrest. Emerg. Med. J. 2019, 36, 479–484. [Google Scholar] [CrossRef]
- Javaudin, F.; Penverne, Y.; Montassier, E. Organisation of prehospital care: The French experience. Eur. J. Emerg. Med. 2020, 27, 404–405. [Google Scholar] [CrossRef]
- Larribau, R.; Deham, H.; Niquille, M.; Sarasin, F.P. Improvement of out-of-hospital cardiac arrest survival rate after implementation of the 2010 resuscitation guidelines. PLoS ONE 2018, 13, e0204169. [Google Scholar] [CrossRef] [PubMed]
- Chappuis, V.N.; Deham, H.; Cottet, P.; Gartner, B.A.; Sarasin, F.P.; Niquille, M.; Suppan, L.; Larribau, R. Emergency physician’s dispatch by a paramedic-staffed emergency medical communication centre: Sensitivity, specificity and search for a reference standard. Scand. J. Traum. Resusc. Emerg. Med. 2021, 29, 31. [Google Scholar] [CrossRef]
- Von, E.E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [Green Version]
- Suppan, L.; Chan, M.; Gartner, B.; Regard, S.; Campana, M.; Chatellard, G.; Cottet, P.; Larribau, R.; Sarasin, F.P.; Niquille, M. Evaluation of a Prehospital Rotation by Senior Residents: A Web-Based Survey. Healthcare 2020, 9, 24. [Google Scholar] [CrossRef]
- Chan, M.; Fehlmann, C.A.; Pasquier, M.; Suppan, L.; Savoldelli, G.L. Endotracheal Intubation Success Rate in an Urban, Supervised, Resident-Staffed Emergency Mobile System: An 11-Year Retrospective Cohort Study. J. Clin. Med. 2020, 9, 238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perkins, G.D.; Jacobs, I.G.; Nadkarni, V.M.; Berg, R.A.; Bhanji, F.; Biarent, D.; Bossaert, L.L.; Brett, S.J.; Chamberlain, D.; de Caen, A.R.; et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest: A statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation 2015, 132, 1286–1300. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Zajic, P.; Zoidl, P.; Deininger, M.; Heschl, S.; Fellinger, T.; Posch, M.; Metnitz, P.; Prause, G. Factors associated with physician decision making on withholding cardiopulmonary resuscitation in prehospital medicine. Sci. Rep. 2021, 11, 5120. [Google Scholar] [CrossRef] [PubMed]
- Duchateau, F.X.; Burnod, A.; Ricard-Hibon, A.; Mantz, J.; Juvin, P. Withholding advanced cardiac life support in out-of-hospital cardiac arrest: A prospective study. Resuscitation 2008, 76, 134–136. [Google Scholar] [CrossRef]
- Huang, J.B.; Lee, K.H.; Ho, Y.N.; Tsai, M.T.; Wu, W.T.; Cheng, F.J. Association between prehospital prognostic factors on out-of-hospital cardiac arrest in different age groups. BMC Emerg. Med. 2021, 21, 3. [Google Scholar] [CrossRef]
- Andrew, E.; Nehme, Z.; Bernard, S.; Smith, K. The influence of comorbidity on survival and long-term outcomes after out-of-hospital cardiac arrest. Resuscitation 2017, 110, 42–47. [Google Scholar] [CrossRef]
- Ono, Y.; Hayakawa, M.; Iijima, H.; Maekawa, K.; Kodate, A.; Sadamoto, Y.; Mizugaki, A.; Murakami, H.; Katabami, K.; Sawamura, A.; et al. The response time threshold for predicting favourable neurological outcomes in patients with bystander-witnessed out-of-hospital cardiac arrest. Resuscitation 2016, 107, 65–70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Evans, C.C.; Petersen, A.; Meier, E.N.; Buick, J.E.; Schreiber, M.; Kannas, D.; Austin, M.A. Prehospital traumatic cardiac arrest: Management and outcomes from the resuscitation outcomes consortium epistry-trauma and PROPHET registries. J. Traum. Acute Care Surg. 2016, 81, 285–293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferrand, E.; Robert, R.; Ingrand, P.; Lemaire, F. Withholding and withdrawal of life support in intensive-care units in France: A prospective survey. French LATAREA Group. Lancet 2001, 357, 9–14. [Google Scholar] [CrossRef]
- Le, C.P.; Riochet, D.; Batard, E.; Volteau, C.; Giraudeau, B.; Arnaudet, I.; Labastire, L.; Levraut, J.; Thys, F.; Lauque, D.; et al. Death in emergency departments: A multicenter cross-sectional survey with analysis of withholding and withdrawing life support. Intens. Care Med. 2010, 36, 765–772. [Google Scholar] [CrossRef]
- Rockwood, K.; Song, X.; MacKnight, C.; Bergman, H.; Hogan, D.B.; McDowell, I.; Mitnitski, A. A global clinical measure of fitness and frailty in elderly people. Can. Med. Assn. J. 2005, 173, 489–495. [Google Scholar] [CrossRef] [Green Version]
- Guidet, B.; Flaatten, H.; Boumendil, A.; Morandi, A.; Andersen, F.H.; Artigas, A.; Bertolini, G.; Cecconi, M.; Christensen, S.; Faraldi, L.; et al. Withholding or withdrawing of life-sustaining therapy in older adults (≥ 80 years) admitted to the intensive care unit. Intens. Care Med. 2018, 44, 1027–1038. [Google Scholar] [CrossRef] [PubMed]
- Druwé, P.; Monsieurs, K.G.; Gagg, J.; Nakahara, S.; Cocchi, M.N.; Élő, G.; van Schuppen, H.; Alpert, E.A.; Truhlář, A.; Huybrechts, S.A.; et al. Impact of perceived inappropiate cardiopulmonary resuscitation on emergency clinicians’ intention to leave the job: Results from a cross-sectional survey in 288 centres across 24 countries. Resuscitation 2021, 158, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Mincarone, P.; Leo, C.G.; Trujillo-Martín, M.D.M.; Manson, J.; Guarino, R.; Ponzini, G.; Sabina, S. Standardized languages and notations for graphical modelling of patient care processes: A systematic review. Int. J. Qual. Health. Care. 2018, 30, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Clemency, B.M.; Innes, J.C.; Waldrop, M.; White, L.J.; Dievendorf, E.; Orlowski, R.; Wang, K.; Lindstrom, H.A.; Canty, J.M., Jr.; Hostler, D. Changes in Field Termination of Resuscitation and Survival Rates After an Educational Intervention to Promote on Scene Resuscitation for Out-of-Hospital Cardiac Arrest. J. Emerg. Med. 2021, 60, 349–354. [Google Scholar] [CrossRef]
- Ferrand, E.; Marty, J. Prehospital withholding and withdrawal of life-sustaining treatments. The French LATASAMU Survey. Intens. Care Med. 2006, 32, 1498–1505. [Google Scholar] [CrossRef] [PubMed]
- Richardson, P.G.; Greenslade, J.; Isoardi, J.; Davey, M.; Gillett, M.; Tucker, A.; Klim, S.; Kelly, A.M.; Abdelmahmoud, I. End-of-life issues: Withdrawal and withholding of life-sustaining healthcare in the emergency department: A comparison between emergency physicians and emergency registrars: A sub-study. Emerg. Med. Australas. 2016, 28, 684–690. [Google Scholar] [CrossRef]
- Mentzelopoulos, S.D.; Couper, K.; Voorde, P.V.; Druwé, P.; Blom, M.; Perkins, G.D.; Lulic, I.; Djakow, J.; Raffay, V.; Lilja, G.; et al. European Resuscitation Council Guidelines 2021: Ethics of resuscitation and end of life decisions. Resuscitation 2021, 161, 408–432. [Google Scholar] [CrossRef]

| Variables | Total | Resuscitation Attempted by EP | Resuscitation Not Attempted by EP | p-Value 2 |
|---|---|---|---|---|
| n = 784 | n = 599 | n = 185 | ||
| Patient’s sex (male), n (% 1) | 496 (63.3) | 392 (65.4) | 104 (56.2) | 0.023 |
| Patient’s age (years), mean ± SD | 66.9 (±18.1) | 64.6 (±17.6) | 74.4 (±17.8) | <0.001 |
| Charlson comorbidity index, n (% 1) | ||||
| 0 | 427 (54.5) | 341 (56.9) | 86 (46.5) | 0.001 |
| 1–2 | 277 (35.3) | 210 (35.1) | 67 (36.2) | |
| 3–4 | 38 (4.9) | 26 (4.3) | 12 (6.5) | |
| 5+ | 42 (5.4) | 22 (3.7) | 20 (10.8) | |
| Presumed aetiology, n (% 1) | ||||
| Medical (cardiac and noncardiac) | 256 (32.7) | 218 (36.4) | 38 (20.5) | 0.001 |
| Trauma | 51 (6.5) | 20 (3.3) | 31 (16.8) | |
| Asphyxiation (external causes) | 40 (5.1) | 35 (5.8) | 5 (2.7) | |
| Unknown | 437 (55.8) | 326 (54.4) | 111 (60.0) | |
| Witnessed arrest (yes), n (% 1) | 415 (52.9) | 337 (56.3) | 78 (42.2) | 0.001 |
| Bystander CPR (yes), n (% 1) | 187 (23.9) | 169 (28.2) | 18 (9.7) | <0.001 |
| EMS response time (min), mean ± SD | 9.2 (±4.3) | 9.2 (±4.1) | 9.3 (±4.8) | 0.869 |
| EMS response time, n (% 1) | ||||
| 0–2 min | 24 (3.1) | 14 (2.3) | 10 (5.4) | 0.305 |
| 2–6 min | 100 (12.8) | 79 (76.4) | 21 (11.4) | |
| 6–9 min | 274 (35.0) | 212 (35.4) | 62 (33.5) | |
| 9–12 min | 200 (25.5) | 149 (24.9) | 51 (27.6) | |
| 12–25 min | 128 (16.3) | 98 (16.4) | 30 (16.2) | |
| >25 min | 9 (1.2) | 6 (1.0) | 3 (1.6) | |
| Missing | 49 (6.4) | 41 (6.8) | 8 (4.3) | |
| Lead physician’s sex (male), n (% 1) | 488 (62.2) | 373 (62.3) | 115 (62.2) | 0.979 |
| Lead physician’s experience, n (% 1) | ||||
| Junior | 456 (58.2) | 353 (58.9) | 103 (55.7) | 0.282 |
| Intermediate | 220 (28.1) | 160 (26.7) | 60 (32.4) | |
| Senior | 108 (13.8) | 86 (14.4) | 22 (11.9) |
| Variables | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|
| Patient’s sex (male) | 1.47 (1.05–2.06) | 1.15 (0.77–1.72) |
| Patient’s age (years) | ||
| 18–64 | Ref. | Ref. |
| 65–79 | 0.69 (0.44–1.07) | 0.52 (0.32–0.89) |
| ≥80 | 0.24 (0.16–0.36) | 0.14 (0.09–0.24) |
| Charlson comorbidity index | ||
| 0 | Ref. | Ref. |
| 1–2 | 0.79 (0.55–1.14) | 0.57 (0.36–0.89) |
| 3–4 | 0.55 (0.26–1.13) | 0.41 (0.17–0.95) |
| 5+ | 0.28 (0.14–0.53) | 0.12 (0.06–0.27) |
| Presumed aetiology | ||
| Medical (cardiac and noncardiac) | Ref. | Ref. |
| Trauma | 0.11 (0.06–0.22) | 0.04 (0.02–0.08) |
| Asphyxiation (external causes) | 1.22 (0.45–3.31) | 0.75 (0.25–2.26) |
| Unknown | 0.51 (0.34–0.77) | 0.55 (0.35–0.87) |
| Witnessed arrest (yes) | 1.76 (1.26–2.46) | 2.14 (1.43–3.20) |
| Bystander CPR (yes) | 3.65 (2.17–6.12) | 4.10 (2.28–7.39) |
| EMS response time | ||
| 0–2 min | Ref. | Ref. |
| 2–6 min | 2.69 (1.05–6.90) | 2.00 (0.63–6.35) |
| 6–9 min | 2.44 (1.03–5.70) | 1.91 (0.65–5.56) |
| 9–12 min | 2.09 (0.87–4.90) | 1.48 (0.5–4.40) |
| 12–25 min | 2.33 (0.94–5.70) | 1.86 (0.6–5.78) |
| >25 min | 1.43 (0.29–7.10) | 1.14 (0.16–8.03) |
| Missing | 3.66 (1.21–11.10) | 1.95 (0.51–7.51) |
| Lead physician’s sex (male) | 1.00 (0.72–1.41) | 0.99 (0.67–1.47) |
| Lead physician’s experience | ||
| Junior | Ref. | Ref. |
| Intermediate | 0.78 (0.54–1.13) | 0.83 (0.54–1.28) |
| Senior | 1.14 (0.68–1.91) | 1.31 (0.71–2.41) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Payot, C.; Fehlmann, C.A.; Suppan, L.; Niquille, M.; Lardi, C.; Sarasin, F.P.; Larribau, R. Factors Influencing Physician Decision Making to Attempt Advanced Resuscitation in Asystolic Out-of-Hospital Cardiac Arrest. Int. J. Environ. Res. Public Health 2021, 18, 8323. https://doi.org/10.3390/ijerph18168323
Payot C, Fehlmann CA, Suppan L, Niquille M, Lardi C, Sarasin FP, Larribau R. Factors Influencing Physician Decision Making to Attempt Advanced Resuscitation in Asystolic Out-of-Hospital Cardiac Arrest. International Journal of Environmental Research and Public Health. 2021; 18(16):8323. https://doi.org/10.3390/ijerph18168323
Chicago/Turabian StylePayot, Charles, Christophe A. Fehlmann, Laurent Suppan, Marc Niquille, Christelle Lardi, François P. Sarasin, and Robert Larribau. 2021. "Factors Influencing Physician Decision Making to Attempt Advanced Resuscitation in Asystolic Out-of-Hospital Cardiac Arrest" International Journal of Environmental Research and Public Health 18, no. 16: 8323. https://doi.org/10.3390/ijerph18168323
APA StylePayot, C., Fehlmann, C. A., Suppan, L., Niquille, M., Lardi, C., Sarasin, F. P., & Larribau, R. (2021). Factors Influencing Physician Decision Making to Attempt Advanced Resuscitation in Asystolic Out-of-Hospital Cardiac Arrest. International Journal of Environmental Research and Public Health, 18(16), 8323. https://doi.org/10.3390/ijerph18168323







