Living with the Late Effects of Childhood Cancer Treatment: A Descriptive Qualitative Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Aims
2.2. Design
2.3. Sample/Participants
2.4. Data Collection
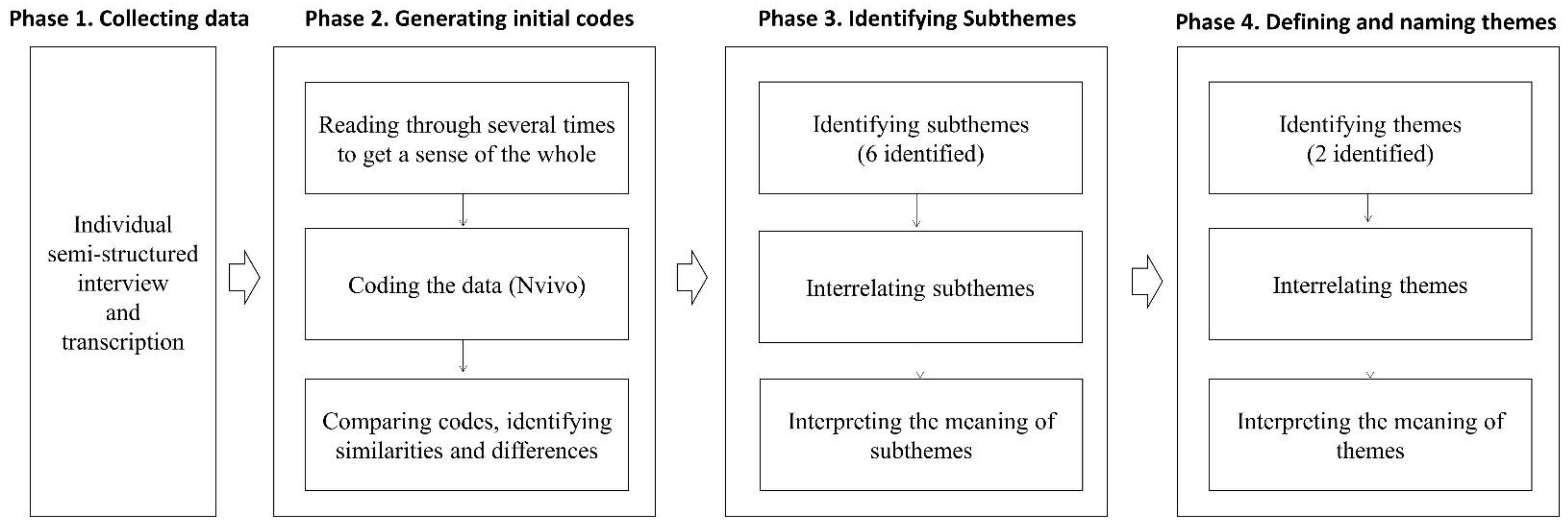
2.5. Data Analysis
2.6. Rigor/Trustworthiness
3. Results
3.1. Theme 1: Things I Encountered While Crossing a Bridge
3.1.1. Do Not Know Where to Get It
I just didn’t know what to do when I got sick. I wouldn’t know where to go. I searched on the internet a lot, but … there are only advertisements and not what I am looking for.… I felt somewhat frustrated about that.(Participant 10)
3.1.2. Not Helpful at All
When I get late effects, I can’t go to a general clinic because I am not a general patient … those doctors in general clinics are not specialized in pediatric cancer, so … there are a lot of limitations because they treat me like one of the general patients.(Participant 7)
3.1.3. Worsening My Situation
I initially tried to store sperm before hematopoietic stem cells transplantation. But they told me there was no sperm. (Interviewer: Before the transplant?) Yes, because I had chemotherapy before…. The health care providers did not tell me this before using chemotherapy … there was no explanation at all … they don’t tell you. Because these people [health care providers] think that the faster the treatment begins, the better, and do not consider … they just want to start treatment right away.(Participant 3)
My mother was extremely overprotective… She only focused on the fact that I was sick, and she tried to lock me in. So, there was often a conflict of opinions between me and her, and she kept on saying, “you need to be careful because you were sick when you were a child, you cannot drink,” always giving me more rules, and I always wanted to be just another college student like everyone else and wondered why I could not be one. So, I understand that I got treatment when I was younger, but why does she keep saying no? … There were some conflicts then … I never told my mother, but I hated how she overprotected me as a childhood cancer patient, and I think it took me a while to get out of it myself.(Participant 10)
3.1.4. People Were There When I Needed Them
3.2. Theme 2: Living as a Survivor
3.2.1. Enduring and Accepting
When I visit the obstetric clinic, I always hear the same thing, you know: you can’t have babies. So, emotionally it gets to me even though I know that fact … in my case, I love children so much … my mother and father try to encourage me. They think I can have babies because future technology may allow this … but I am a more pragmatic person and … tend not to think about far into the future. I don’t expect much.(Participant 8)
3.2.2. Found My Own Coping Strategies
I am a perfectionist, and I keep working on something until it is of the level that I find satisfactory. I cannot sit for long because I don’t have any muscles in my buttocks because of Estradiol injection. So, I divide time to finish my assignment. I assign time … from what time to what time, I finish this assignment and then have a 30-minute rest and then come back to do the assignment. I ensure that I go to bed by a certain time to have strength for the next day.(Participant 8)
3.2.3. My Life Is Special
By chance, I started volunteering at the Korean Association for Children with Leukemia and Cancer…. While volunteering, I met a good mentor, and the mentor told me that I was brave after hearing my history of sickness. People always told me, “you are different [from all these healthy people],” and then I met someone who changed my perspective by saying, “it’s so great that you overcame this”.… Since then, I came to accept the fact that I was sick [positively]…. The reason I chose social welfare studies was because I wanted to work for people with childhood cancer. I was once a person who received support and wanted to give back to society, so I graduated with a degree in social welfare and worked with the Social Work Team at the Seoul St. Mary’s Hospital last year.(Participant 10)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Cancer Society. Cancer Facts & Figures 2020; American Cancer Society: Atlanta, GA, USA, 2020. [Google Scholar]
- Gatta, G.; Botta, L.; Rossi, S.; Aareleid, T.; Bielska-Lasota, M.; Clavel, J.; Dimitrova, N.; Jakab, Z.; Kaatsch, P.; Lacour, B.; et al. Childhood cancer survival in Europe 1999–2007: Results of EUROCARE-5—A population-based study. Lancet Oncol. 2014, 15, 35–47. [Google Scholar] [CrossRef]
- Korea Central Cancer Registry; National Cancer Center. Annual Report of Cancer Statistics in Korea in 2017; Ministry of Health and Welfare: Sejong, Korea, 2019. Available online: https://ncc.re.kr/cancerStatsView.ncc?bbsnum=518&searchKey=total&searchValue=&pageNum=12020 (accessed on 6 August 2021).
- Park, H.J.; Moon, E.K.; Yoon, J.Y.; Oh, C.M.; Jung, K.W.; Park, B.K.; Shin, H.Y.; Won, Y.J. Incidence and survival of childhood cancer in Korea. Cancer Res. Treat. 2016, 48, 869–882. [Google Scholar] [CrossRef]
- Kim, Y.; Lee, K.S.; Koh, K.N. Difficulties faced by long-term childhood cancer survivors: A qualitative study. Eur. J. Oncol. Nurs. 2018, 36, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Cheung, Y.T.; Brinkman, T.M.; Li, C.; Mzayek, Y.; Srivastava, D.; Ness, K.K.; Patel, S.K.; Howell, R.M.; Oeffinger, K.C.; Robison, L.L.; et al. Chronic health conditions and neurocognitive function in aging survivors of childhood cancer: A report from the childhood cancer survivor study. J. Natl. Cancer Inst. 2018, 110, 411–419. [Google Scholar] [CrossRef]
- National Cancer Institute. Late Effects of Treatment for Childhood Cancer-Patient Version. Available online: https://www.cancer.gov/types/childhood-cancers/late-effects-pdq (accessed on 8 June 2021).
- Huang, I.C.; Brinkman, T.M.; Kenzik, K.; Gurney, J.G.; Ness, K.K.; Lanctot, J.; Shenkman, E.; Robison, L.L.; Hudson, M.M.; Krull, K.R. Association between the prevalence of symptoms and health-related quality of life in adult survivors of childhood cancer: A report from the St Jude Lifetime Cohort study. J. Clin. Oncol. 2013, 31, 4242–4251. [Google Scholar] [CrossRef]
- Krull, K.R.; Hardy, K.K.; Kahalley, L.S.; Schuitema, I.; Kesler, S.R. Neurocognitive outcomes and interventions in long-term survivors of childhood cancer. J. Clin. Oncol. 2018, 36, 2181–2189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Foster, R.H.; Brouwer, A.M.; Dillon, R.; Bitsko, M.J.; Godder, K.; Stern, M. “Cancer was a speed bump in my path to enlightenment:” A qualitative analysis of situational coping experiences among young adult survivors of childhood cancer. J. Psychosoc. Oncol. 2017, 35, 377–392. [Google Scholar] [CrossRef]
- Kadan-Lottick, N.S.; Robison, L.L.; Gurney, J.G.; Neglia, J.P.; Yasui, Y.; Hayashi, R.; Hudson, M.; Greenberg, M.; Mertens, A.C. Childhood cancer survivors’ knowledge about their past diagnosis and treatment: Childhood Cancer Survivor Study. JAMA 2002, 287, 1832–1839. [Google Scholar] [CrossRef] [Green Version]
- Yi, J.; Kim, M.A.; Sang, J. Worries of childhood cancer survivors in young adulthood. Eur. J. Oncol. Nurs. 2016, 21, 113–119. [Google Scholar] [CrossRef]
- Duffey-Lind, E.C.; O’Holleran, E.; Healey, M.; Vettese, M.; Diller, L.; Park, E.R. Transitioning to survivorship: A pilot study. J. Pediatr. Oncol. Nurs. 2006, 23, 335–343. [Google Scholar] [CrossRef]
- Howard, A.F.; Kazanjian, A.; Pritchard, S.; Olson, R.; Hasan, H.; Newton, K.; Goddard, K. Healthcare system barriers to long-term follow-up for adult survivors of childhood cancer in British Columbia, Canada: A qualitative study. J. Cancer Surviv. 2018, 12, 277–290. [Google Scholar] [CrossRef] [Green Version]
- Hendriks, M.J.; Harju, E.; Michel, G. The unmet needs of childhood cancer survivors in long-term follow-up care: A qualitative study. Psycho-Oncology 2021, 30, 485–492. [Google Scholar] [CrossRef] [PubMed]
- Gurney, J.G.; Krull, K.R.; Kadan-Lottick, N.; Nicholson, H.S.; Nathan, P.C.; Zebrack, B.; Tersak, J.M.; Ness, K.K. Social outcomes in the Childhood Cancer Survivor Study cohort. J. Clin. Oncol. 2009, 27, 2390–2395. [Google Scholar] [CrossRef] [PubMed]
- Kirchhoff, A.C.; Krull, K.R.; Ness, K.K.; Park, E.R.; Oeffinger, K.C.; Hudson, M.M.; Stovall, M.; Robison, L.L.; Wickizer, T.; Leisenring, W. Occupational outcomes of adult childhood cancer survivors: A report from the childhood cancer survivor study. Cancer 2011, 117, 3033–3044. [Google Scholar] [CrossRef]
- Pivetta, E.; Maule, M.M.; Pisani, P.; Zugna, D.; Haupt, R.; Jankovic, M.; Aricò, M.; Casale, F.; Clerico, A.; Cordero di Montezemolo, L.; et al. Marriage and parenthood among childhood cancer survivors: A report from the Italian AIEOP Off-Therapy Registry. Haematologica 2011, 96, 744–751. [Google Scholar] [CrossRef] [Green Version]
- Evan, E.E.; Kaufman, M.; Cook, A.B.; Zeltzer, L.K. Sexual health and self-esteem in adolescents and young adults with cancer. Cancer 2006, 107, 1672–1679. [Google Scholar] [CrossRef] [PubMed]
- Robert, R.S.; Ottaviani, G.; Huh, W.W.; Palla, S.; Jaffe, N. Psychosocial and functional outcomes in long-term survivors of osteosarcoma: A comparison of limb-salvage surgery and amputation. Pediatr. Blood Cancer 2010, 54, 990–999. [Google Scholar] [CrossRef] [Green Version]
- Ida, H.; Alicia, G.K.; Anna, F.; Irene, L.; Anna, N.; Helena, M.; Maria, E.; Emir, H.; Hannah, N. Quality of life among female childhood cancer survivors with and without premature ovarian insufficiency. J. Cancer Surviv. 2021. e-pub ahead of print. [Google Scholar] [CrossRef]
- Duran, B. Posttraumatic growth as experienced by childhood cancer survivors and their families: A narrative synthesis of qualitative and quantitative research. J. Pediatr. Oncol. Nurs. 2013, 30, 179–197. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y. Exploration of life experiences of positive growth in long-term childhood cancer survivors. Eur. J. Oncol. Nurs. 2017, 30, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Parry, C.; Chesler, M.A. Thematic evidence of psychosocial thriving in childhood cancer survivors. Qual. Health Res. 2005, 15, 1055–1073. [Google Scholar] [CrossRef]
- Hong, H.C.; Kim, Y.M.; Min, A. Symptom clusters in childhood cancer survivors in Korea: A latent class analysis. Eur. J. Cancer Care 2020, 29, e13322. [Google Scholar] [CrossRef]
- Brown, M.C.; Pearce, M.S.; Bailey, S.; Skinner, R. The long-term psychosocial impact of cancer: The views of young adult survivors of childhood cancer. Eur. J. Cancer Care 2016, 25, 428–439. [Google Scholar] [CrossRef]
- Sandelowski, M. Whatever happened to qualitative description? Res. Nurs. Health 2000, 23, 334–340. [Google Scholar] [CrossRef]
- Sandelowski, M. What’s in a name? Qualitative description revisited. Res. Nurs. Health 2010, 33, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Sefcik, J.S.; Bradway, C. Characteristics of Qualitative Descriptive Studies: A Systematic Review. Res. Nurs. Health 2017, 40, 23–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsieh, H.F.; Shannon, S.E. Three approaches to qualitative content analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef]
- Denzin, N.K. The Research Act: A Theoretical Introduction to Sociological Methods, 2nd ed.; McGraw-Hill: New York, NY, USA, 1978. [Google Scholar]
- Guba, E.G.; Lincoln, Y.S. Fourth Generation Evaluation, 1st ed.; Sage Publications: Newbury Park, CA, USA, 1989. [Google Scholar]
- Hauken, M.A.; Grue, M.; Dyregrov, A. “It’s been a life-changing experience!” A qualitative study of young adult cancer survivors’ experiences of the coexistence of negative and positive outcomes after cancer treatment. Scand. J. Psychol. 2019, 60, 577–584. [Google Scholar] [CrossRef]
- Tinga, S.N.; Maree, J.N. Living with the late effects of cervical cancer treatment: A descriptive qualitative study at an academic hospital in Gauteng. S. Afr. J. Gynaecol. Oncol. 2015, 7, 21–26. [Google Scholar] [CrossRef] [Green Version]
- Barton, S.E.; Najita, J.S.; Ginsburg, E.S.; Leisenring, W.M.; Stovall, M.; Weathers, R.E.; Sklar, C.A.; Robison, L.L.; Diller, L. Infertility, infertility treatment, and achievement of pregnancy in female survivors of childhood cancer: A report from the Childhood Cancer Survivor Study cohort. Lancet Oncol. 2013, 14, 873–881. [Google Scholar] [CrossRef] [Green Version]
- Loren, A.W.; Mangu, P.B.; Beck, L.N.; Brennan, L.; Magdalinski, A.J.; Partridge, A.H.; Quinn, G.; Wallace, W.H.; Oktay, K. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J. Clin. Oncol. 2013, 31, 2500–2510. [Google Scholar] [CrossRef]
- Balthazar, U.; Fritz, M.A.; Mersereau, J.E. Fertility preservation: A pilot study to assess previsit patient knowledge quantitatively. Fertil. Steril. 2011, 95, 1913–1916. [Google Scholar] [CrossRef]
- Letourneau, J.M.; Ebbel, E.E.; Katz, P.P.; Katz, A.; Ai, W.Z.; Chien, A.J.; Melisko, M.E.; Cedars, M.I.; Rosen, M.P. Pretreatment fertility counseling and fertility preservation improve quality of life in reproductive age women with cancer. Cancer 2012, 118, 1710–1717. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boyce, W.T. The vulnerable child: New evidence, new approaches. Adv. Pediatr. 1992, 39, 1–33. [Google Scholar] [PubMed]
- Tillery, R.; Long, A.; Phipps, S. Child perceptions of parental care and overprotection in children with cancer and healthy children. J. Clin. Psychol. Med. Settings 2014, 21, 165–172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bruce, M. A systematic and conceptual review of posttraumatic stress in childhood cancer survivors and their parents. Clin. Psychol. Rev. 2006, 26, 233–256. [Google Scholar] [CrossRef] [PubMed]
- Jantien Vrijmoet-Wiersma, C.M.; van Klink, J.M.; Kolk, A.M.; Koopman, H.M.; Ball, L.M.; Maarten Egeler, R. Assessment of parental psychological stress in pediatric cancer: A review. J. Pediatr. Psychol. 2008, 33, 694–706. [Google Scholar] [CrossRef] [Green Version]
- Wakefield, C.E.; McLoone, J.K.; Butow, P.; Lenthen, K.; Cohn, R.J. Parental adjustment to the completion of their child’s cancer treatment. Pediatr. Blood Cancer 2011, 56, 524–531. [Google Scholar] [CrossRef]
- Nir, Y. Post-traumatic stress disorder in children with cancer. In Posttraumatic Stress Disorder in Children, 1st ed.; Eth, I.S., Pynoos, R.S., Eds.; American Psychiatric Press: Washington, DC, USA, 1985; pp. 123–132. [Google Scholar]
- Huang, I.C.; Brinkman, T.M.; Mullins, L.; Pui, C.H.; Robison, L.L.; Hudson, M.M.; Krull, K.R. Child symptoms, parent behaviors, and family strain in long-term survivors of childhood acute lymphoblastic leukemia. Psycho-Oncology 2018, 27, 2031–2038. [Google Scholar] [CrossRef]
- Katz, L.F.; Leary, A.; Breiger, D.; Friedman, D. Pediatric cancer and the quality of children’s dyadic peer interactions. J. Pediatr. Psychol. 2011, 36, 237–247. [Google Scholar] [CrossRef]
- Kim, M.A.; Yi, J. Life after cancer: How does public stigma increase psychological distress of childhood cancer survivors? Int. J. Nurs. Stud. 2014, 51, 1605–1614. [Google Scholar] [CrossRef] [PubMed]
- Bonanno, A.; Esmaeli, B. Cancer and facial disfigurement: Reducing survivors’ stigma in social interaction. Clin. J. Oncol. Nurs. 2012, 16, 153–159. [Google Scholar] [CrossRef] [Green Version]
- Chow, E.J.; Ness, K.K.; Armstrong, G.T.; Bhakta, N.; Yeh, J.M.; Bhatia, S.; Landier, W.; Constine, L.S.; Hudson, M.M.; Nathan, P.C. Current and coming challenges in the management of the survivorship population. Semin. Oncol. 2020, 47, 23–39. [Google Scholar] [CrossRef]
- Robison, L.L.; Hudson, M.M. Survivors of childhood and adolescent cancer: Life-long risks and responsibilities. Nat. Rev. Cancer 2014, 14, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Winick, N. Neurocognitive outcome in survivors of pediatric cancer. Curr. Opin. Pediatr. 2011, 23, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, B.D.; Jacobsen, P.B. Depression in lung cancer patients: The role of perceived stigma. Psycho-Oncology 2021, 21, 239–246. [Google Scholar] [CrossRef] [Green Version]
- Lebel, S.; Castonguay, M.; Mackness, G.; Irish, J.; Bezjak, A.; Devins, G.M. The psychosocial impact of stigma in people with head and neck or lung cancer. Psycho-Oncology 2013, 22, 140–152. [Google Scholar] [CrossRef]
- Phelan, S.M.; Griffin, J.M.; Jackson, G.L.; Zafar, S.Y.; Hellerstedt, W.; Stahre, M.; Nelson, D.; Zullig, L.L.; Burgess, D.J.; van Ryn, M. Stigma, perceived blame, self-blame, and depressive symptoms in men with colorectal cancer. Psycho-Oncology 2013, 22, 65–73. [Google Scholar] [CrossRef]
- Reiter-Purtill, J.; Vannatta, K.; Gerhardt, C.A.; Correll, J.; Noll, R.B. A controlled longitudinal study of the social functioning of children who completed treatment of cancer. J. Pediatr. Hematol./Oncol. 2003, 25, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Schultz, K.A.; Ness, K.K.; Whitton, J.; Recklitis, C.; Zebrack, B.; Robison, L.L.; Zeltzer, L.; Mertens, A.C. Behavioral and social outcomes in adolescent survivors of childhood cancer: A report from the childhood cancer survivor study. J. Clin. Oncol. 2007, 25, 3649–3656. [Google Scholar] [CrossRef]
- Aldridge, A.A.; Roesch, S.C. Coping and adjustment in children with cancer: A meta-analytic study. J. Behav. Med. 2007, 30, 115–129. [Google Scholar] [CrossRef] [PubMed]
- Williamson, H.; Harcourt, D.; Halliwell, E.; Frith, H.; Wallace, M. Adolescents’ and parents’ experiences of managing the psychosocial impact of appearance change during cancer treatment. J. Pediatr. Oncol. Nurs. 2010, 27, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.; Choi, E.K.; Kim, S.Y.; Shin, D.W.; Cho, B.L.; Kim, C.H.; Koh, D.H.; Guallar, E.; Bardwell, W.A.; Park, J.H. Association between cancer stigma and depression among cancer survivors: A nationwide survey in Korea. Psycho-Oncology 2013, 22, 2372–2378. [Google Scholar] [CrossRef] [PubMed]
- Calhoun, L.G.; Tedeschi, R.G. The foundations of posttraumatic growth: An expanded framework. In Handbook of Posttraumatic Growth: Research and Practice, 1st ed.; Calhoun, L.G., Tedeschi, R.G., Eds.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 2006; pp. 3–23. [Google Scholar]
- Lepore, S.J.; Revenson, T.A. Resilience and posttraumatic growth: Recovery, resistance, and reconfiguration. In Handbook of Posttraumatic Growth: Research and Practice, 1st ed.; Calhoun, L.G., Tedeschi, R.G., Eds.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 2006; pp. 24–46. [Google Scholar]
- Hong, H.C.; Kim, Y.M.; Min, A. Factors influencing quality of life among childhood cancer survivors in Korea: A quantile regression approach. Res. Nurs. Health 2021. [Google Scholar] [CrossRef]
| Gender | Diagnosed Age (years) | Treatment end Age (years) | Current Age (years) | Diagnosis | Recurrence | Type of Treatment | Religion | Education Level | Current Job | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chemotherapy | Radiation Therapy | Hematopoietic Stem Cell Transplantation | ||||||||||
| 1 | Male | 2 | 7 | 25 | Leukemia | No | Yes | No | No | Christian | Baccalaureate | None (seeking a new job) |
| 2 | Female | 12 | 14 | 20 | Leukemia | Yes | Yes | Yes | Yes | None | High school | Undergraduate student |
| 3 | Male | 18 | 20 | 25 | Malignant lymphoma | No | Yes | No | Yes | None | High school | Part time job |
| 4 | Female | 14 | 15 | 25 | Malignant lymphoma | No | Yes | No | No | None | High school | Undergraduate student, Part time job |
| 5 | Male | 12 | 18 | 25 | Leukemia | No | Yes | No | No | None | Baccalaureate | Coffee shop manager |
| 6 | Female | 16 | 16 | 26 | Malignant lymphoma | No | Yes | No | No | None | Baccalaureate | Graduate student |
| 7 | Female | 14 | 17 | 20 | Osteosarcoma | Yes (2 times) | Yes | No | Yes | Catholic | High school | Undergraduate student |
| 8 | Female | 13 | 13 | 20 | Leukemia | No | Yes | Yes | Yes | Christian | High school | Undergraduate student |
| 9 | Male | 15 | 16 | 23 | Osteosarcoma | No | Yes | No | No | Catholic | High school | Undergraduate student |
| 10 | Female | 5 | 8 | 25 | Leukemia | No | Yes | No | No | None | Baccalaureate | Social worker |
| 11 | Male | 18 | 19 | 22 | Leukemia | No | Yes | No | No | None | High school | Undergraduate student |
| 12 | Female | 13 | 13 | 19 | Leukemia | No | Yes | No | Yes | None | High school | Undergraduate student |
| 13 | Male | 14 | 20 | 23 | Leukemia | No | Yes | Yes | Yes | Christian | High school | Undergraduate student |
| 14 | Female | 13 | 18 | 25 | Leukemia | Yes | Yes | Yes | Yes | Catholic | High school | Undergraduate student |
| 15 | Female | 13 | 15 | 19 | Malignant lymphoma | No | Yes | Yes | Yes | None | High school | Undergraduate student |
| Themes | Subthemes |
|---|---|
| Things I encountered while crossing a bridge | Do not know where to get it |
| Not helpful at all | |
| Worsening my situation | |
| People were there when I needed them | |
| Living as a survivor | Enduring and accepting |
| Found my own coping strategies | |
| My life is special |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hong, H.C.; Min, A.; Choi, S. Living with the Late Effects of Childhood Cancer Treatment: A Descriptive Qualitative Study. Int. J. Environ. Res. Public Health 2021, 18, 8392. https://doi.org/10.3390/ijerph18168392
Hong HC, Min A, Choi S. Living with the Late Effects of Childhood Cancer Treatment: A Descriptive Qualitative Study. International Journal of Environmental Research and Public Health. 2021; 18(16):8392. https://doi.org/10.3390/ijerph18168392
Chicago/Turabian StyleHong, Hye Chong, Ari Min, and Sungkyoung Choi. 2021. "Living with the Late Effects of Childhood Cancer Treatment: A Descriptive Qualitative Study" International Journal of Environmental Research and Public Health 18, no. 16: 8392. https://doi.org/10.3390/ijerph18168392
APA StyleHong, H. C., Min, A., & Choi, S. (2021). Living with the Late Effects of Childhood Cancer Treatment: A Descriptive Qualitative Study. International Journal of Environmental Research and Public Health, 18(16), 8392. https://doi.org/10.3390/ijerph18168392






