Primary Care and Physical Literacy: A Non-Randomized Controlled Pilot Study to Combat the High Prevalence of Physically Inactive Adults in Austria
Abstract
:1. Introduction
2. Materials and Methods
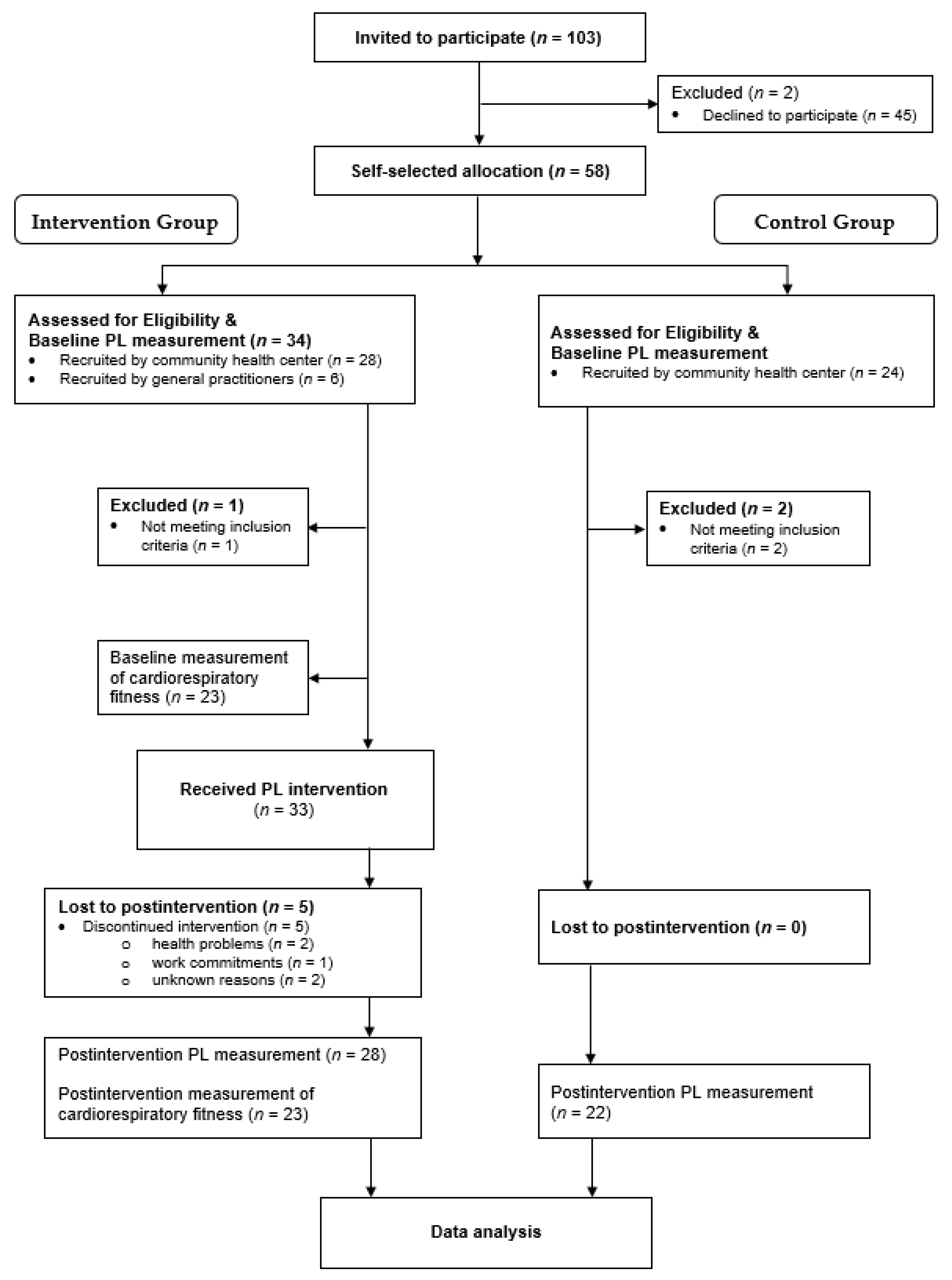
2.1. The Design, Participants, and Procedures
2.2. Physical Literacy
2.2.1. Motivation, Knowledge, and Attitude/Understanding Domains
2.2.2. Self-Efficacy/Confidence Domain
2.2.3. Physical Activity Behavior Domain
2.2.4. Physical Literacy Composite Score and Domain Scores
2.3. Cardiorespiratory Fitness (CRF)
2.4. Sociodemographic and Anthropometric Data
2.5. The Physical Literacy-Based Intervention
2.6. Sample Size
2.7. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Adherence and Intervention Parameters
3.3. Reliability of the Physical Literacy Questionnaire
3.4. Physical Literacy
3.5. Domain Scores of Physical Literacy
3.5.1. Physical Activity Behavior Domain
3.5.2. Attitude/Understanding Domain
3.5.3. Motivation Domain
3.5.4. Knowledge Domain
3.5.5. Self-Efficacy/Confidence Domain
3.6. Factors Influencing Changes in Physical Literacy
3.7. Changes in Cardiorespiratory Fitness (CRF)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Ethics Committee Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Baseline M (SD) | Postintervention M (SD) | Interaction (Group × Time) | Post Hoc Comparison | |||||
|---|---|---|---|---|---|---|---|---|
| F | p Value | ηp2 | t | p Value | d | |||
| Physical Literacy | ||||||||
| Intervention group | 99.0 ± 5.8 | 101.3 ± 6.3 | 19.2 | <0.001 | 0.29 | 2.9 | 0.006 | 0.38 |
| Control group | 101.3 ± 5.1 | 98.4 ± 5.4 | −3.3 | 0.002 | −0.56 | |||
| PA Behavior (min/wk) | ||||||||
| Intervention group | 89.6 ± 96.9 | 178.4 ± 130.8 | 5.6 | 0.02 | 0.11 | 3.4 | 0.005 | 0.77 |
| Control group | 143.6 ± 131.5 | 123.4 ± 144.1 | −0.5 | 0.56 | -0.15 | |||
| Attitude/Understanding | ||||||||
| Intervention group | 3.0 ± 0.8 | 3.5 ± 0.7 | 9.1 | 0.004 | 0.16 | 5.0 | <0.001 | 0.52 |
| Control group | 3.3 ± 0.6 | 3.3 ± 0.5 | −0.2 | 0.87 | −0.04 | |||
| Motivation | ||||||||
| Intervention group | 3.7 ± 0.5 | 3.7 ± 0.6 | 0.6 | 0.44 | 0.01 | n/a | ||
| Control group | 3.8 ± 0.6 | 3.9 ± 0.7 | ||||||
| Knowledge | ||||||||
| Intervention group | 2.8 ± 1.1 | 3.5 ± 1.1 | 5.0 | 0.03 | 0.10 | 2.9 | 0.004 | 0.66 |
| Control group | 2.6 ± 1.3 | 2.5 ± 1.1 | -0.3 | 0.75 | -0.08 | |||
| Self-Efficacy/Confidence | ||||||||
| Intervention group | 3.0 ± 0.6 | 3.5 ± 0.5 | 5.9 | 0.02 | 0.11 | 4.9 | <0.001 | 0.83 |
| Control group | 3.2 ± 0.6 | 3.3 ± 0.6 | 1.2 | 0.25 | 0.19 | |||
References
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef] [Green Version]
- Sattelmair, J.; Pertman, J.; Ding, E.L.; Kohl, H.W.; Haskell, W.; Lee, I.M. Dose response between physical activity and risk of coronary heart disease: A meta-analysis. Circulation 2011, 124, 789–795. [Google Scholar] [CrossRef] [Green Version]
- Dunn, A.L.; Trivedi, M.H.; O’Neal, H.A. Physical activity dose-response effects on outcomes of depression and anxiety. Med. Sci. Sports Exerc. 2001, 33, 587–597. [Google Scholar] [CrossRef]
- Schuch, F.B.; Vancampfort, D.; Firth, J.; Rosenbaum, S.; Ward, P.B.; Silva, E.S.; Hallgren, M.; Ponce De Leon, A.; Dunn, A.L.; Deslandes, A.C.; et al. Physical Activity and Incident Depression: A Meta-Analysis of prospective cohort studies. Am. J. Psychiatry 2018, 175, 631–648. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef] [Green Version]
- Physical activity in leisure Time—Austrian Health Interview Survey. Available online: http://www.statistik.at/web_de/statistiken/menschen_und_gesellschaft/gesundheit/gesundheitsdeterminanten/koerperliche_aktivitaet/index.html (accessed on 13 January 2021).
- Holler, P.; Soffried, J. Physical Inactivity in Austrian Health Care Regions. 2018. Available online: https://www.ifgp.at/cdscontent/load?contentid=10008.727095&version=1574240815 (accessed on 14 January 2021).
- Österreich, F.G. (Ed.) Austrian Physical Activity Recommendations. 2020. Available online: https://fgoe.org/sites/fgoe.org/files/2020-06/WB17_bewegungsempfehlungen_bfrei.pdf (accessed on 14 June 2021).
- Rhodes, R.E.; Nasuti, G. Trends and changes in research on the psychology of physical activity across 20 Years: A quantitative analysis of 10 journals. Prev. Med. 2011, 53, 17–23. [Google Scholar] [CrossRef]
- Stokols, D. Translating social ecological theory into guidelines for community health promotion. Am. J. Health Promot. 1996, 10, 282–298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rhodes, R.E.; Kowalski, K. Building skills to promote physical activity. In ACSM’s Behavioral Aspects of Physical Activity and Exercise; Nigg, C.R., Ed.; Williams & Wilkins: Lippincott, PA, USA, 2014; pp. 71–101. [Google Scholar]
- Cornish, K.; Fox, G.; Fyfe, T.; Koopmans, E.; Pousette, A. Understanding physical literacy in the context of health: A rapid scoping review. BMC Public Health 2020, 20, 1569. [Google Scholar] [CrossRef] [PubMed]
- Edwards, L.C.; Bryant, A.S.; Keegan, R.J.; Morgan, K.; Cooper, S.M.; Jones, A.M. Measuring’ physical literacy and related constructs: A systematic review of empirical findings. Sports Med. 2018, 48, 659–682. [Google Scholar] [CrossRef] [Green Version]
- Corbin, C.B. Implications of physical literacy for research and practice: A Commentary. Res. Q. Exerc. Sport 2016, 87, 14–27. [Google Scholar] [CrossRef]
- Edwards, L.C.; Bryant, A.S.; Keegan, R.J.; Morgan, K.; Jones, A.M. Definitions, foundations and associations of physical literacy: A systematic review. Sports Med. 2017, 47, 113–126. [Google Scholar] [CrossRef] [Green Version]
- Hyndman, B.; Pill, S. What’s in a concept? A leximancer text mining analysis of physical literacy across the international literature. Eur. Phys. Educ. Rev. 2017. [Google Scholar] [CrossRef]
- Whitehead, M. (Ed.) Physical Literacy: Throughout the Lifecourse, 1st ed.; Routledge: New York, NY, USA, 2010. [Google Scholar]
- Francis, C.E.; Longmuir, P.E.; Boyer, C.; Andersen, L.B.; Barnes, J.D.; Boiarskaia, E.; Cairney, J.; Faigenbaum, A.D.; Faulkner, G.; Hands, B.P.; et al. The canadian assessment of physical literacy: Development of a model of children’s capacity for a healthy, active lifestyle through a delphi process. J. Phys. Act. Health 2016, 13, 214–222. [Google Scholar] [CrossRef]
- Deci, E.L.; Ryan, R.M. Intrinsic Motivation and Self-Determination in Human; Plenum Publishing Co.: New York, NY, USA, 1985. [Google Scholar]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef] [PubMed]
- Stevens-Smith, D.A. Physical Literacy: Getting Kids Active for Life. Strategies 2016, 29, 3–9. [Google Scholar] [CrossRef]
- Bremer, E.; Graham, J.D.; Cairney, J. Outcomes and Feasibility of a 12-Week Physical Literacy Intervention for Children in an Afterschool Program. Int. J. Environ. Res. Public Health 2020, 17, 3129. [Google Scholar] [CrossRef] [PubMed]
- Cairney, J.; Dudley, D.; Kwan, M.; Bulten, R.; Kriellaars, D. Physical literacy, physical activity and health: Toward an evidence-informed conceptual model. Sports Med. 2019, 49, 371–383. [Google Scholar] [CrossRef]
- Austria Health Target Number 8: To Promote Healthy, Safe Exercise and Activity in Everyday Life through Appropriate Environment—Working Group Report. Available online: https://gesundheitsziele-oesterreich.at/website2017/wp-content/uploads/2017/05/bericht-arbeitsgruppe-8-gesundheitsziele-oesterreich.pdf (accessed on 14 January 2021).
- Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World. Available online: https://apps.who.int/iris/bitstream/handle/10665/272722/9789241514187-eng.pdf (accessed on 14 January 2021).
- Taplin, L. Physical literacy an introduction to the concept. Phys. Educ. Matters 2011, 6, 28–30. [Google Scholar]
- Liu, Y.; Chen, S. Physical literacy in children and adolescents, definitions, assessments, and interventions. Eur. Phys. Educ. Rev. 2021, 27, 96–112. [Google Scholar] [CrossRef]
- Almond, L. What Is the Relevance of Physical Literacy for Adults? ICSSPE 2013, 65, 215–236. [Google Scholar]
- Whitehead, M. Stages in Physical Literacy Journey. ICSSPE 2013, 65, 52–56. [Google Scholar]
- Whitehead, M. Definition of Physical Literacy and Clarification of Related Issues. ICSSPE 2013, 65, 29–34. [Google Scholar]
- Robinson, D.B.; Randall, L. Marking physical literacy or missing the mark on physical literacy? A conceptual critique of Canada’s physical literacy assessment instruments. Meas. Phys. Educ. Exerc. Sci. 2016, 21, 40–55. [Google Scholar] [CrossRef]
- McAuley, E. Enhancing psychological health through physical activity. In Towards Active Living: Proceedings of the International Conference on Physical Activity, Fitness and Health; Quinney, H.A., Gauvin, L., Wall, A.E.T., Eds.; Human Kinetics: Champaign, IL, USA, 1994; pp. 83–90. [Google Scholar]
- Allender, S.; Cowburn, G.; Foster, C. Understanding participation in sport and physical activity among children and adults: A review of qualitative studies. Health Educ. Res. 2006, 21, 826–835. [Google Scholar] [CrossRef] [Green Version]
- Burke, S.; Carron, A.; Eys, M.; Ntoumanis, M.; Estabrooks, P. Group versus individual approach? a meta-analysis of the effectiveness of interventions to promote physical activity. Int. Rev. Sport Exerc. Psychol. 2005, 2, 19–35. [Google Scholar]
- Patel, M.; Doku, V.; Tennakoon, L. Challenges in recruitment of research participants. Adv. Psychiatr. Treat. 2003, 9, 229–238. [Google Scholar] [CrossRef] [Green Version]
- Carroll, J.K.; Yancey, A.K.; Spring, B.; Figueroa-Moseley, C.; Mohr, D.C.; Mustian, K.M.; Sprod, L.K.; Purnell, J.Q.; Fiscella, K. What are successful recruitment and retention strategies for underserved populations? Examining physical activity interventions in primary care and community settings. Transl. Behav. Med. 2011, 1, 234–251. [Google Scholar] [CrossRef] [PubMed]
- Van Doorslaer, E.; Masseria, C.; Koolman, X. OECD Health Equity Research Group. Inequalities in access to medical care by income in developed countries. CMAJ 2006, 174, 177–183. [Google Scholar] [CrossRef] [Green Version]
- Phillips, E.M.; Kennedy, M.A. The exercise prescription: A tool to improve physical activity. PM R 2012, 4, 818–825. [Google Scholar] [CrossRef] [PubMed]
- Holler, P.; Jaunig, J.; Amort, F.M.; Tuttner, S.; Hofer-Fischanger, K.; Wallner, D.; Simi, H.; Müller, A.; van Poppel, M.N.M.; Moser, O. Holistic physical exercise training improves physical literacy among physically inactive adults: A pilot intervention study. BMC Public Health 2019, 19, 393. [Google Scholar] [CrossRef]
- Kukull, W.A.; Ganguli, M. Generalizability: The trees, the forest, and the low-hanging fruit. Neurology 2012, 78, 1886–1891. [Google Scholar] [CrossRef] [Green Version]
- Markland, D.; Tobin, V. A modification of the behavioural regulation in exercise questionnaire to include an assessment of Amotivation. J. Sport Exerc. Psychol. 2004, 26, 191–196. [Google Scholar] [CrossRef] [Green Version]
- Guay, F.; Vallerand, R.J.; Blanchard, C. On the assessment of situational intrinsic and extrinsic motivation: The situational motivation scale (SIMS). Motiv. Emot. 2000, 23, 175–213. [Google Scholar] [CrossRef]
- Pelletier, L.G.; Fortier, M.S.; Vallerand, R.J.; Tuson, K.M.; Biere, N.M.; Blais, M.R. Toward a new measure of intrinsic motivation, Extrinsic motivation, and amotivation in sport: The sport motivation scale (SMS). J. Sport Exerc. Psychol. 1995, 17, 35–53. [Google Scholar] [CrossRef] [Green Version]
- Fitzgerald, J.T.; Singleton, S.P.; Neale, A.V.; Prasad, A.S.; Hess, J.W. Active level, fitness status, exercise knowledge, and exercise Beliefs among healthy, older African American and white women. J. Aging Health 1994, 6, 296–323. [Google Scholar] [CrossRef]
- IOX Assessement Association. A Handbook to Evaluate Physical Fitness Program; Prepared for the Center for Health Promotion and Education, Centers of Disease Control; In Cooperation with the Office of Diseases Prevention and Health Promotion; DHHS: Cincinnati, OH, USA, 1983; Volume 200, pp. 253–257. [Google Scholar]
- Renner, B.; Schwarzer, R. Risk and Health Behaviors—Documentation of the Scales of the Research Project Risk Appraisal Consequences in Korea (RACK). Available online: http://www.gesundheitsrisiko.de/docs/RACKEnglish.pdf (accessed on 16 February 2021).
- Albani, C.; Blaser, G.; Geyer, M.; Daig, I.; Schmutzer, G.; Bailer, H.; Grulke, N.; Brähler, E. Überprüfung und Normierung des “Fragebogen zum Körperbild“ FKB-20 von Clement und Löwe (1996) an einer repräsentativen deutschen Bevölkerungsstichprobe. Z. Med. Psychol. 2006, 15, 99–109. [Google Scholar]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, M.K.; Lin, F.C.; Ward, S.E.; Fine, J.P. Composite variables: When and how. Nurs. Res. 2013, 62, 45–49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sykes, K. Capacity assessment in the workplace: A new step test. Occup. Health (Lond.) 1995, 47, 20–22. [Google Scholar]
- Sykes, K.; Roberts, A. The Chester step test—A simple yet effective tool for the prediction of aerobic capacity. Physiotherapy 2004, 90, 183–188. [Google Scholar] [CrossRef]
- Bennett, H.; Parfitt, G.; Davison, K.; Eston, R. Validity of Submaximal Step Tests to Estimate Maximal Oxygen Uptake in Healthy Adults. Sports Med. 2016, 46, 737–750. [Google Scholar] [CrossRef] [PubMed]
- Kilpatrick, M.; Herbert, E.P.; Jacobsen, D. Physical Activity Motivation: A Practitioner’s Guide to Self-Determination Theory. J. Phys. Educ. Recreat. Dance 2002, 73, 36–41. [Google Scholar] [CrossRef]
- Frikkel, J.; Götte, M.; Beckmann, M.; Kasper, S.; Hense, J.; Teufel, M.; Schuler, M.; Tewes, M. Fatigue, barriers to physical activity and predictors for motivation to exercise in advanced Cancer patients. BMC Palliat. Care 2020, 19. [Google Scholar] [CrossRef] [PubMed]
- Trost, S.G.; Saunders, R.; Ward, D.S. Determinants of Physical Activity in Middle School Children. Am. J. Health Behav. 2002, 26, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Whitehead, M.; Almond, L. Creating Learning Experiences to Foster physical Literacy. ICSSPE 2013, 65, 73–80. [Google Scholar]
- Maruf, F.A.; Ojukwu, C.C.; Akindele, M.O. Perception, knowledge, and attitude toward physical activity behaviour: Implications for Participation among Individuals with essential hypertension. High Blood Press Cardiovasc. Prev. 2018, 25, 53–60. [Google Scholar] [CrossRef]
- Latimer, A.E.; Brawley, L.R.; Bassett, R.L. A systematic review of three approaches for constructing physical activity messages: What messages work and what improvements are needed? Int. J. Behav. Nutr. Phys. Act. 2010, 7, 36. [Google Scholar] [CrossRef] [Green Version]
- Rhodes, R.E.; Pfaeffli, L.A. Mediators of physical activity behaviour change among adult non-clinical populations: A review update. Int. J. Behav. Nutr. Phys. Act. 2010, 7. [Google Scholar] [CrossRef] [Green Version]
- Löllgen, H. Das Anstrengungsempfinden (RPE, Borg-Skala). Dtsch. Z. Sportmed. 2004, 55, 299–300. [Google Scholar]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.M.; Nieman, D.C.; Swain, D.P.; American College of Sports Medicine. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, H.; Monahan, K.D.; Seals, D.R. Age-predicted maximal heart rate revisited. J. Am. Coll. Cardiol. 2001, 37, 153–156. [Google Scholar] [CrossRef] [Green Version]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Steiner, L.D. Starting at the Beginning: An Introduction to Coefficient Alpha and Internal Consistency. J. Pers. Assess. 2003, 80, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: New York, NY, USA, 1988. [Google Scholar]
- Costa, D.S. Reflective, causal, and composite indicators of quality of life: A conceptual or an empirical distinction? Qual. Life Res. 2015, 24, 2057–2065. [Google Scholar] [CrossRef]
- Kwan, M.Y.W.; Graham, J.D.; Bedard, C.; Bremer, E.; Healey, C.; Cairney, J. Examining the Effectiveness of a Pilot Physical Literacy-Based Intervention Targeting First-Year University Students: The physical literacyUS Program. SAGE Open 2019. [Google Scholar] [CrossRef]
- Warner, M.; Robinson, J.; Heal, B.; Lloyd, J.; Mandigo, J.; Lennox, B.; Larkin, D.H. Increasing physical literacy in youth: A two-week Sport for Development program for children aged 6–10. Prospects 2021, 50, 165–182. [Google Scholar] [CrossRef]
- Courneya, K.S.; Segal, R.J.; Gelmon, K.; Reid, R.D.; Mackey, J.R.; Friedenreich, C.M.; Proulx, C.; Lane, K.; Ladha, A.B.; Vallance, J.K.; et al. Predictors of supervised exercise adherence during breast cancer chemotherapy. Med. Sci. Sports Exerc. 2008, 40, 1180–1187. [Google Scholar] [CrossRef] [PubMed]
- Udoh, A.; Bruno, A.; Bates, I.; Galbraith, K. Transnational comparability of advanced pharmacy practice developmental frameworks: A country-level crossover mapping study. Int. J. Pharm. Pract. 2018, 26, 550–559. [Google Scholar] [CrossRef] [Green Version]
- National Research Council. When I’m 64; The National Academies Press: Washington, DC, USA, 2006. [Google Scholar]
- Gordon-Larsen, P.; Nelson, M.C.; Popkin, B.M. Longitudinal physical activity and sedentary behavior trends: Adolescence to adulthood. Am. J. Prev. Med. 2004, 27, 277–283. [Google Scholar] [CrossRef]
- Lang, J.J.; Chaput, J.; Longmuir, P.E.; Barnes, J.D.; Belanger, K.; Tomkinson, G.R.; Anderson, K.D.; Bruner, B.; Copeland, J.L.; Gregg, M.J.; et al. Cardiorespiratory fitness is associated with physical literacy in a large sample of Canadian children aged 8 to 12 years. BMC Public Health 2018, 18. [Google Scholar] [CrossRef]
- Kwak, L.; Kremers, S.; Walsh, A.; Brug, H. How is your walking group running? Health Educ. 2006, 106, 21–31. [Google Scholar] [CrossRef]
- Tulloch, H.; Sweet, S.N.; Fortier, M.; Capstick, G.; Kenny, G.P.; Sigal, R.J. Exercise facilitators and barriers from adoption to maintenance in the diabetes aerobic and resistance exercise trial. Can. J. Diabetes 2013, 37, 367–374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Action Plan Movement (NAP.b). Available online: https://www.bmkoes.gv.at/sport/breitensport/breiten-gesundheitssport/nap-bewegung.html (accessed on 17 January 2021).
- Donnachie, C.; Hunt, K.; Mutrie, N.; Gill, J.M.R.; Kelly, P. Responsiveness of Device-Based and Self-Report Measures of Physical Activity to Detect Behavior Change in Men Taking Part in the Football Fans in Training (FFIT) Program. J. Meas. Phys. Behav. 2020, 3, 67–77. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | IG | CG | p-Value |
|---|---|---|---|
| Gender (Female) | 25 (89%) | 21 (96%) | 0.43 |
| Age (Years) | 53 ± 10 | 50 ± 11 | 0.20 |
| Anthropometry | |||
| Height (cm) | 166 ± 8 | 167 ± 5 | 0.69 |
| Weight (kg) | 77 ± 16 | 73 ± 11 | 0.35 |
| BMI (kg/m²) | 28 ± 5 | 26 ± 4 | 0.18 |
| Education Level N (%) | |||
| Compulsory school | 0 (0%) | 1 (4%) | 0.46 |
| Apprenticeship/Professional school degree | 19 (68%) | 11 (50%) | |
| School examination (A-Level) | 5 (18%) | 5 (23%) | |
| Grad | 4 (14%) | 5 (23%) | |
| Chronic Diseases N (%) | 10 (36%) | 3 (14%) | 0.08 |
| Physical Literacy | 99.0 ± 5.8 | 101.3 ± 5.1 | 0.14 |
| Physical activity behavior (min/wk) | 89.6 ± 96.9 | 143.6 ± 131.5 | 0.10 |
| Attitude/Understanding a | 3.0 ± 0.8 | 3.3 ± 0.6 | 0.25 |
| Motivation a | 3.7 ± 0.5 | 3.8 ± 0.6 | 0.46 |
| Knowledge a | 2.8 ± 1.1 | 2.6 ± 1.3 | 0.55 |
| Self-efficacy/Confidence | 3.0 ± 0.6 | 3.2 ± 0.6 | 0.26 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Holler, P.; Jaunig, J.; Moser, O.; Tuttner, S.; Simi, H.; Wallner, D.; Amort, F.M.; van Poppel, M. Primary Care and Physical Literacy: A Non-Randomized Controlled Pilot Study to Combat the High Prevalence of Physically Inactive Adults in Austria. Int. J. Environ. Res. Public Health 2021, 18, 8593. https://doi.org/10.3390/ijerph18168593
Holler P, Jaunig J, Moser O, Tuttner S, Simi H, Wallner D, Amort FM, van Poppel M. Primary Care and Physical Literacy: A Non-Randomized Controlled Pilot Study to Combat the High Prevalence of Physically Inactive Adults in Austria. International Journal of Environmental Research and Public Health. 2021; 18(16):8593. https://doi.org/10.3390/ijerph18168593
Chicago/Turabian StyleHoller, Peter, Johannes Jaunig, Othmar Moser, Silvia Tuttner, Helmut Simi, Dietmar Wallner, Frank Michael Amort, and Mireille van Poppel. 2021. "Primary Care and Physical Literacy: A Non-Randomized Controlled Pilot Study to Combat the High Prevalence of Physically Inactive Adults in Austria" International Journal of Environmental Research and Public Health 18, no. 16: 8593. https://doi.org/10.3390/ijerph18168593








