Association between Statin Use and Meniere’s Disease: Results from a National Health Screening Cohort
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics
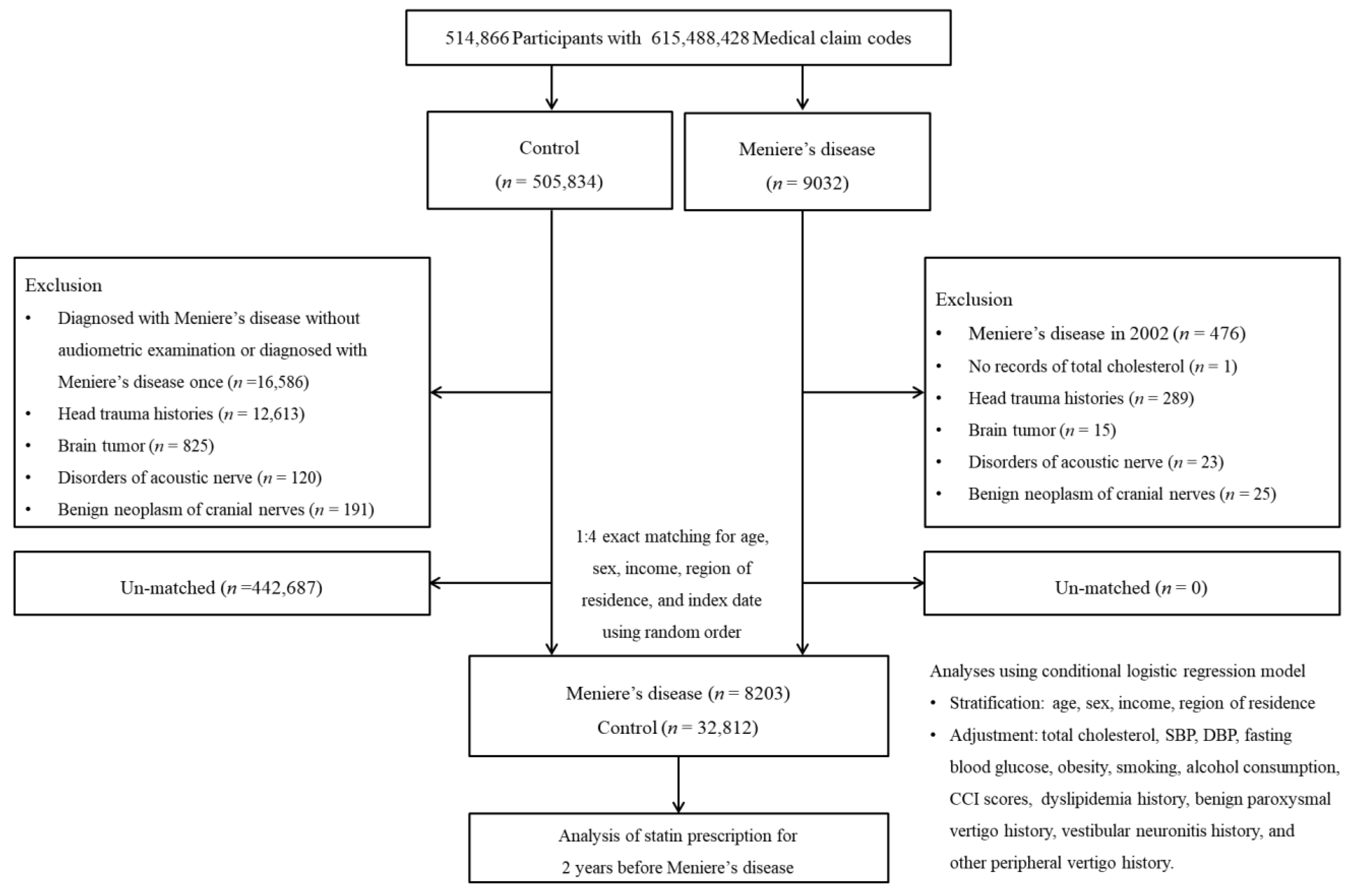
2.2. Study Population and Participant Selection
2.3. Independent Variable
2.4. Dependent Variable
2.5. Covariates
2.6. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Istvan, E.S.; Deisenhofer, J. Structural mechanism for statin inhibition of HMG-CoA reductase. Science 2001, 292, 1160–1164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chou, R.; Dana, T.; Blazina, I.; Daeges, M.; Jeanne, T.L. Statins for Prevention of Cardiovascular Disease in Adults: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2016, 316, 2008–2024. [Google Scholar] [CrossRef]
- Thomson, N.C. Clinical Studies of Statins in Asthma and COPD. Curr. Mol. Pharmacol. 2017, 10, 60–71. [Google Scholar] [CrossRef] [PubMed]
- Cortese, F.; Gesualdo, M.; Cortese, A.; Carbonara, S.; Devito, F.; Zito, A.; Ricci, G.; Scicchitano, P.; Ciccone, M.M. Rosuvastatin: Beyond the cholesterol-lowering effect. Pharmacol. Res. 2016, 107, 1–18. [Google Scholar] [CrossRef]
- Chung, S.D.; Chen, C.H.; Hung, S.H.; Lin, H.C.; Wang, L.H. A population-based study on the association between statin use and sudden sensorineural hearing loss. Otolaryngol. Head Neck Surg. 2015, 152, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, T.A.; Cheeley, M.K.; Jones, P.H.; La Forge, R.; Maki, K.C.; Lopez, J.A.G.; Xiang, P.; Bushnell, D.M.; Martin, M.L.; Cohen, J.D. The STatin Adverse Treatment Experience Survey: Experience of patients reporting side effects of statin therapy. J. Clin. Lipidol. 2019, 13, 415–424. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Hui, L.; Zhang, B.; Ren, L.; Zhu, J.; Wang, F.; Li, S. The Correlation Between Endolymphatic Hydrops and Clinical Features of Meniere Disease. Laryngoscope 2021, 131, E144–E150. [Google Scholar] [CrossRef]
- Hallpike, C.S.; Cairns, H. Observations on the Pathology of Meniere’s Syndrome: (Section of Otology). Proc. R. Soc. Med. 1938, 31, 1317–1336. [Google Scholar]
- Yamakawa, K. The pathology of a labyrinth with Meniere’s disease. Jpn. J. Otol. 1938, 44, 2310–2312. [Google Scholar]
- Gurkov, R.; Pyyko, I.; Zou, J.; Kentala, E. What is Meniere’s disease? A contemporary re-evaluation of endolymphatic hydrops. J. Neurol. 2016, 263 (Suppl. 1), S71–S81. [Google Scholar] [CrossRef] [Green Version]
- Menière, P. Sur une forme de sourdité grave dépendant d’une lésion de l’oreille interne. Gaz Med. Paris 1861, 16, 55–57. [Google Scholar]
- Watanabe, Y.; Mizukoshi, K.; Shojaku, H.; Watanabe, I.; Hinoki, M.; Kitahara, M. Epidemiological and clinical characteristics of Meniere’s disease in Japan. Acta Otolaryngol. Suppl. 1995, 519, 206–210. [Google Scholar] [CrossRef] [PubMed]
- Semaan, M.T.; Megerian, C.A. Contemporary perspectives on the pathophysiology of Meniere’s disease: Implications for treatment. Curr. Opin. Otolaryngol. Head Neck Surg. 2010, 18, 392–398. [Google Scholar] [CrossRef] [PubMed]
- Merchant, S.N.; Adams, J.C.; Nadol, J.B., Jr. Pathophysiology of Meniere’s syndrome: Are symptoms caused by endolymphatic hydrops? Otol. Neurotol. 2005, 26, 74–81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.Y.; Lee, C.H.; Min, C.; Park, I.S.; Choi, H.G. Bidirectional analysis of the association between Meniere’s disease and depression: Two longitudinal follow-up studies using a national sample cohort. Clin. Otolaryngol. 2020, 45, 687–694. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Song, Y.S.; Wee, J.H.; Min, C.; Yoo, D.M.; Choi, H.G. Association between Meniere’s disease and thyroid diseases: A nested case-control study. Sci. Rep. 2020, 10, 18224. [Google Scholar] [CrossRef] [PubMed]
- Portmann, G. Vasomotor Affections of the Internal Ear. Proc. R. Soc. Med. 1928, 21, 1917–1923. [Google Scholar]
- Inoue, H.; Uemura, T. Sluggishness of pupillary light contraction in patients with Meniere’s disease. Acta Otolaryngol. 1988, 105, 582–586. [Google Scholar] [CrossRef]
- Franz, B.; Altidis, P.; Altidis, B.; Collis-Brown, G. The cervicogenic otoocular syndrome: A suspected forerunner of Meniere’s disease. Int. Tinnitus J. 1999, 5, 125–130. [Google Scholar]
- Atkinson, M. Evidence for a Vascular Mechanism in Meniere’s Syndrome. Proc. R. Soc. Med. 1946, 39, 807–809. [Google Scholar]
- Filipo, R.; Ciciarello, F.; Attanasio, G.; Mancini, P.; Covelli, E.; Agati, L.; Fedele, F.; Viccaro, M. Chronic cerebrospinal venous insufficiency in patients with Meniere’s disease. Eur. Arch. Otorhinolaryngol. 2015, 272, 77–82. [Google Scholar] [CrossRef]
- Li, S.Y.; Chen, H.H.; Lin, C.L.; Yeh, S.Y.; Kao, C.H. The Different Cardiovascular Outcomes Between Long-Term Efficacy of Hydrophilic and Lipophilic Statin Therapy in Both Asian Diabetic Sexes. Dose Response 2019, 17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.Y.; Min, C.; Oh, D.J.; Choi, H.G. Tobacco Smoking and Alcohol Consumption Are Related to Benign Parotid Tumor: A Nested Case-Control Study Using a National Health Screening Cohort. Clin. Exp. Otorhinolaryngol. 2019, 12, 412–419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.Y.; Wee, J.H.; Min, C.; Yoo, D.M.; Choi, H.G. Relationship between Bell’s Palsy and Previous Statin Use: A Case/Non-Case Study. Int. J. Environ. Res. Public Health 2020, 17, 8408. [Google Scholar] [CrossRef]
- Quan, H.; Li, B.; Couris, C.M.; Fushimi, K.; Graham, P.; Hider, P.; Januel, J.M.; Sundararajan, V. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am. J. Epidemiol. 2011, 173, 676–682. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernandez, K.A.; Allen, P.; Campbell, M.; Page, B.; Townes, T.; Li, C.M.; Cheng, H.; Garrett, J.; Mulquin, M.; Clements, A.; et al. Atorvastatin is associated with reduced cisplatin-induced hearing loss. J. Clin. Investig. 2021, 131, e142616. [Google Scholar] [CrossRef]
- Lee, Y.Y.; Choo, O.S.; Kim, Y.J.; Gil, E.S.; Jang, J.H.; Kang, Y.; Choung, Y.H. Atorvastatin prevents hearing impairment in the presence of hyperlipidemia. Biochim. Biophys. Acta Mol. Cell Res. 2020, 1867, 118850. [Google Scholar] [CrossRef] [PubMed]
- Flook, M.; Frejo, L.; Gallego-Martinez, A.; Martin-Sanz, E.; Rossi-Izquierdo, M.; Amor-Dorado, J.C.; Soto-Varela, A.; Santos-Perez, S.; Batuecas-Caletrio, A.; Espinosa-Sanchez, J.M.; et al. Differential Proinflammatory Signature in Vestibular Migraine and Meniere Disease. Front. Immunol. 2019, 10, 1229. [Google Scholar] [CrossRef] [PubMed]
- Park, J.S.; Kim, S.W.; Park, K.; Choung, Y.H.; Jou, I.; Park, S.M. Pravastatin attenuates noise-induced cochlear injury in mice. Neuroscience 2012, 208, 123–132. [Google Scholar] [CrossRef]
- Godlowski, Z. Pathogenesis and management of Meniere’s syndrome in terms of microcirculation. Pharmacologic decompression of the endolymphatic hydrops. Angiology 1965, 16, 644–650. [Google Scholar] [CrossRef]
- Attanasio, G.; Califano, L.; Bruno, A.; Giugliano, V.; Ralli, M.; Martellucci, S.; Milella, C.; de Vincentiis, M.; Russo, F.Y.; Greco, A. Chronic cerebrospinal venous insufficiency and meniere’s disease: Interventional versus medical therapy. Laryngoscope 2020, 130, 2040–2046. [Google Scholar] [CrossRef] [PubMed]
- Schachter, M. Chemical, pharmacokinetic and pharmacodynamic properties of statins: An update. Fundam Clin. Pharmacol. 2005, 19, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Bytyci, I.; Bajraktari, G.; Bhatt, D.L.; Morgan, C.J.; Ahmed, A.; Aronow, W.S.; Banach, M.; Lipid and Blood Pressure Meta-analysis Collaboration. Hydrophilic vs lipophilic statins in coronary artery disease: A meta-analysis of randomized controlled trials. J. Clin. Lipidol. 2017, 11, 624–637. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total Participants | |||
|---|---|---|---|---|
| Meniere’ Disease | Comparison | p-Value | ||
| Total number (n, %) | 7734 (100.0) | 30,936 (100.0) | ||
| Age (years old) (n, %) | 40–44 | 72 (0.9) | 288 (0.9) | 1.000 |
| 45–49 | 470 (6.1) | 1880 (6.1) | ||
| 50–54 | 1130 (14.6) | 4520 (14.6) | ||
| 55–59 | 1336 (17.3) | 5344 (17.3) | ||
| 60–64 | 1257 (16.3) | 5028 (16.3) | ||
| 65–69 | 1231 (15.9) | 4924 (15.9) | ||
| 70–74 | 1115 (14.4) | 4460 (14.4) | ||
| 75–79 | 726 (9.4) | 2904 (9.4) | ||
| 80–84 | 318 (4.1) | 1272 (4.1) | ||
| 85+ | 79 (1.0) | 316 (1.0) | ||
| Sex (n, %) | Male | 2752 (35.6) | 11,008 (35.6) | 1.000 |
| Female | 4982 (64.4) | 19,928 (64.4) | ||
| Income (n, %) | 1 (lowest) | 1343 (17.4) | 5372 (17.4) | 1.000 |
| 2 | 967 (12.5) | 3868 (12.5) | ||
| 3 | 1193 (15.4) | 4772 (15.4) | ||
| 4 | 1605 (20.8) | 6420 (20.8) | ||
| 5 (highest) | 2626 (40.0) | 10,504 (40.0) | ||
| Region of residence (n, %) | Urban | 3267 (42.2) | 13,068 (42.2) | 1.000 |
| Rural | 4467 (57.8) | 17,868 (57.8) | ||
| Obesity (n, %) † | Underweight | 152 (2.0) | 809 (2.6) | <0.001 * |
| Normal | 2638 (34.1) | 11,006 (35.6) | ||
| Overweight | 2168 (28.0) | 8337 (27.0) | ||
| Obese I | 2541 (32.9) | 9709 (31.4) | ||
| Obese II | 235 (3.0) | 1075 (3.5) | ||
| Smoking status (n, %) | Nonsmoker | 6249 (80.8) | 24,360 (78.7) | <0.001 * |
| Past smoker | 812 (10.5) | 3011 (9.7) | ||
| Current smoker | 673 (8.7) | 3565 (11.5) | ||
| Alcohol consumption (n, %) | <1 time a week | 5804 (75.0) | 22,323 (72.2) | <0.001 * |
| ≥1 time a week | 1930 (25.0) | 8613 (27.8) | ||
| Systolic blood pressure (n, %) | <120 mmHg | 2387 (30.9) | 9315 (30.1) | 0.006 * |
| 120–139 mmHg | 3806 (49.2) | 14,948 (48.3) | ||
| ≥140 mmHg | 1541 (19.9) | 6673 (21.6) | ||
| Diastolic blood pressure (n, %) | <80 mmHg | 3828 (49.5) | 14,836 (48.0) | 0.002 * |
| 80–89 mmHg | 2749 (35.5) | 40,998 (35.5) | ||
| ≥90 mmHg | 1157 (15.0) | 5102 (16.5) | ||
| Fasting blood glucose (n, %) | <100 mg/dL | 4897 (63.3) | 19,414 (62.8) | 0.010 * |
| 100–125 mg/dL | 2211 (28.6) | 8678 (28.0) | ||
| ≥126 mg/dL | 626 (8.1) | 2844 (9.2) | ||
| Total cholesterol (n, %) | <200 mg/dL | 3989 (51.6) | 15,984 (51.7) | 0.989 |
| 200–239 mg/dL | 2609 (33.7) | 10,420 (33.7) | ||
| ≥240 mg/dL | 1136 (14.7) | 4532 (14.6) | ||
| CCI score (n, %) | 0 | 4876 (63.0) | 21,066 (68.1) | <0.001 * |
| 1 | 1412 (18.3) | 4495 (14.5) | ||
| ≥2 | 1446 (18.7) | 5375 (17.4) | ||
| Dyslipidemia history (n, %) | 2949 (38.1) | 9337 (30.2) | <0.001 * | |
| Benign paroxysmal vertigo history (n, %) | 1777 (23.0) | 1161 (3.7) | <0.001 * | |
| Vestibular neuronitis history (n, %) | 506 (6.5) | 288 (0.9) | <0.001 * | |
| Other peripheral vertigo history (n, %) | 1180 (15.3) | 878 (2.8) | <0.001 * | |
| The dates of statin prescription (days, mean, SD) | 50.77 (112.8) | 43.18 (107.0) | <0.001 * | |
| The dates of hydrophilic statin prescription (days, mean, SD) | 9.11 (51.38) | 7.38 (46.73) | <0.001 * | |
| The dates of lipophilic statin prescription (days, mean, SD) | 41.66 (102.4) | 35.78 (97.60) | <0.001 * | |
| Characteristics | Odds Ratios for Meniere’ Disease | p Value for Interaction | |||||
|---|---|---|---|---|---|---|---|
| Crude† | p-Value | Model 1 †‡ | p-Value | Model 2 †§ | p-Value | ||
| Total participants (n = 38,670) | |||||||
| Statin prescription (1 year) | 1.26 (1.17–1.37) | <0.001 * | 0.96 (0.88–1.06) | 0.433 | 0.92 (0.83–1.02) | 0.110 | |
| Age < 65 years old (n = 21,325) | 0.668 | ||||||
| Statin prescription (1 year) | 1.31 (1.15–1.49) | <0.001 * | 0.90 (0.77–1.04) | 0.167 | 0.85 (0.72–1.00) | 0.051 | |
| Age ≥ 65 years old (n = 17,345) | |||||||
| Statin prescription (1 year) | 1.24 (1.11–1.37) | <0.001 * | 1.02 (0.90–1.15) | 0.740 | 0.98 (0.86–1.13) | 0.84 | |
| Men (n = 13,760) | 0.675 | ||||||
| Statin prescription (1 year) | 1.26 (1.09–1.45) | 0.002 * | 0.92 (0.79–1.09) | 0.347 | 0.88 (0.74–1.05) | 0.158 | |
| Women (n = 24,910) | |||||||
| Statin prescription (1 year) | 1.27 (1.15–1.40) | <0.001 * | 0.98 (0.88–1.11) | 0.803 | 0.94 (0.83–1.07) | 0.343 | |
| Low income (n = 17,515) | 0.821 | ||||||
| Statin prescription (1 year) | 1.30 (1.15–1.47) | <0.001 * | 0.93 (0.80–1.07) | 0.319 | 0.88 (0.75–1.03) | 0.117 | |
| High income (n = 22,335) | |||||||
| Statin prescription (1 year) | 1.24 (1.11–1.38) | <0.001 * | 0.99 (0.87–1.12) | 0.876 | 0.95 (0.83–1.09) | 0.462 | |
| Urban residents (n = 16,335) | 0.425 | ||||||
| Statin prescription (1 year) | 1.20 (1.06–1.36) | 0.004 * | 0.91 (0.79–1.05) | 0.215 | 0.87 (0.74–1.02) | 0.094 | |
| Rural residents (n = 22,335) | |||||||
| Statin prescription (1 year) | 1.31 (1.18–1.46) | <0.001 * | 1.00 (0.88–1.14) | 0.965 | 0.95 (0.83–1.09) | 0.496 | |
| Characteristics | Odds Ratios for Meniere’ Disease | p for Interaction | |||||
|---|---|---|---|---|---|---|---|
| Crude† | p-Value | Model 1 †‡ | p-Value | Model 2 †§ | p-Value | ||
| Total participants (n = 38,670) | |||||||
| Lipophilic statin prescription (1 year) | 1.24 (1.14–1.36) | <0.001 * | 0.95 (0.86–1.05) | 0.308 | 0.90 (0.81–1.00) | 0.058 | |
| Age < 65 years old (n = 21,325) | 0.941 | ||||||
| Lipophilic statin prescription (1 year) | 1.26 (1.09–1.45) | 0.002 * | 0.87 (0.74–1.02) | 0.084 | 0.81 (0.68–0.97) | 0.023 * | |
| Age ≥ 65 years old (n = 17,345) | |||||||
| Lipophilic statin prescription (1 year) | 1.23 (1.10–1.38) | <0.001 * | 1.01 (0.89–1.16) | 0.775 | 0.98 (0.85–1.12) | 0.741 | |
| Men (n = 13,760) | 0.625 | ||||||
| Lipophilic statin prescription (1 year) | 1.24 (1.06–1.45) | 0.007 * | 0.93 (0.78–1.10) | 0.406 | 0.87 (0.72–1.06) | 0.161 | |
| Women (n = 24,910) | |||||||
| Lipophilic statin prescription (1 year) | 1.24 (1.11–1.39) | <0.001 * | 0.96 (0.85–1.09) | 0.555 | 0.92 (0.80–1.05) | 0.208 | |
| Low income (n = 17,515) | 0.760 | ||||||
| Lipophilic statin prescription (1 year) | 1.29 (1.12–1.47) | <0.001 * | 0.92 (0.79–1.07) | 0.297 | 0.87 (0.74–1.03) | 0.106 | |
| High income (n = 22,335) | |||||||
| Lipophilic statin prescription (1 year) | 1.21 (1.07–1.36) | 0.002 * | 0.97 (0.85–1.11) | 0.647 | 0.92 (0.80–1.07) | 0.274 | |
| Urban residents (n = 16,335) | 0.476 | ||||||
| Lipophilic statin prescription (1 year) | 1.17 (1.02–1.35) | 0.022 * | 0.90 (0.77–1.05) | 0.177 | 0.85 (0.72–1.01) | 0.070 | |
| Rural residents (n = 22,335) | |||||||
| Lipophilic statin prescription (1 year) | 1.30 (1.15–1.46) | <0.001 * | 0.98 (0.86–1.13) | 0.864 | 0.93 (0.81–1.08) | 0.336 | |
| Characteristics | Odds Ratios for Meniere’ Disease | p for Interaction | |||||
|---|---|---|---|---|---|---|---|
| Crude † | p-Value | Model 1 †‡ | p-Value | Model 2 †§ | p-Value | ||
| Total participants (n = 38,670) | |||||||
| Hydrophilic statin prescription (1 year) | 1.30 (1.08–1.55) | 0.004 * | 1.04 (0.86–1.25) | 0.696 | 1.06 (0.77–1.47) | 0.704 | |
| Age < 65 years old (n = 21,325) | 0.451 | ||||||
| Hydrophilic statin prescription (1 year) | 1.48 (1.11–1.96) | 0.007 * | 1.07 (0.80–1.44) | 0.627 | 1.34 (0.80–1.33) | 0.801 | |
| Age ≥ 65 years old (n = 17,345) | |||||||
| Hydrophilic statin prescription (1 year) | 1.19 (0.94–1.51) | 0.137 | 1.02 (0.80–1.29) | 0.878 | 1.04 (0.80–1.34) | 0.785 | |
| Men (n = 13,760) | 0.867 | ||||||
| Hydrophilic statin prescription (1 year) | 1.26 (0.94–1.70) | 0.122 | 0.95 (0.70–1.29) | 0.751 | 0.97 (0.69–1.36) | 0.844 | |
| Women (n = 24,910) | |||||||
| Hydrophilic statin prescription (1 year) | 1.38 (1.05–1.65) | 0.016 * | 1.11 (0.86–1.36) | 0.498 | 1.17 (0.83–1.38) | 0.590 | |
| Low income (n = 17,515) | 0.935 | ||||||
| Hydrophilic statin prescription (1 year) | 1.29 (1.98–1.71) | 0.071 | 1.00 (0.75–1.33) | 0.993 | 0.99 (0.72–1.36) | 0.956 | |
| High income (n = 22,335) | |||||||
| Hydrophilic statin prescription (1 year) | 1.30 (1.03–1.64) | 0.027 * | 1.07 (0.84–1.36) | 0.574 | 1.08 (0.83–1.40) | 0.550 | |
| Urban residents (n = 16,335) | 0.716 | ||||||
| Hydrophilic statin prescription (1 year) | 1.27 (0.97–1.66) | 0.083 | 1.01 (0.77–1.33) | 0.939 | 1.01 (0.74–1.37) | 0.939 | |
| Rural residents (n = 22,335) | |||||||
| Hydrophilic statin prescription (1 year) | 1.32 (1.04–1.68) | 0.022 * | 1.06 (0.83–1.36) | 0.646 | 1.07 (0.82–1.40) | 0.624 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.Y.; Yoo, D.M.; Min, C.; Choi, H.G. Association between Statin Use and Meniere’s Disease: Results from a National Health Screening Cohort. Int. J. Environ. Res. Public Health 2021, 18, 8692. https://doi.org/10.3390/ijerph18168692
Kim SY, Yoo DM, Min C, Choi HG. Association between Statin Use and Meniere’s Disease: Results from a National Health Screening Cohort. International Journal of Environmental Research and Public Health. 2021; 18(16):8692. https://doi.org/10.3390/ijerph18168692
Chicago/Turabian StyleKim, So Young, Dae Myoung Yoo, Chanyang Min, and Hyo Geun Choi. 2021. "Association between Statin Use and Meniere’s Disease: Results from a National Health Screening Cohort" International Journal of Environmental Research and Public Health 18, no. 16: 8692. https://doi.org/10.3390/ijerph18168692
APA StyleKim, S. Y., Yoo, D. M., Min, C., & Choi, H. G. (2021). Association between Statin Use and Meniere’s Disease: Results from a National Health Screening Cohort. International Journal of Environmental Research and Public Health, 18(16), 8692. https://doi.org/10.3390/ijerph18168692






