Abstract
Background: The aim of the study was to systematically evaluate the biceps femoris long head activation across cross-sectional hamstring strength exercise studies. Methods: A systematic review design was followed. The search strategy conducted in PubMed, Cochrane Library, and Web of Sciences databases found a total of 3643 studies. Once inclusion and exclusion criteria were applied, 29 studies were finally included in this systematic review. A total of 507 participants and 114 different exercises were analyzed. Exercises were evaluated individually and grouped into several categories: Nordics, isokinetic exercises, lunges, squats, deadlifts, good mornings, hip thrusts, bridges, leg curls, swings, hip and back extensions, and others. Results: Results showed the isokinetic and Nordic exercises as the categories with highest biceps femoris activation (>60% of Maximal Voluntary Isometric Contraction). Nordic hamstring exercise ankle dorsiflexion was the exercise that achieved the highest biceps femoris long head activation (128.1% of its Maximal Voluntary Isometric Contraction). Conclusions: The results from this systematic review suggest that isokinetic and Nordic exercises seem to be the best option to activate biceps femoris long head. Future studies evaluating the implementation of these exercises in prevention programs are needed.
1. Introduction
Hamstring strain injury (HSI) is one of the most common injuries in sports involving high-intensity sprinting, acceleration, and decelerations [1]. Injury rates of the hamstring muscles ranges from 6% to 29% of all injuries in track and field, soccer, Australian football, rugby, basketball, or cricket [2].
The biceps femoris long head (BFlh) is the most affected muscle, involving around 80% of all HSIs [3]. Moreover, around 30% of HSIs are recurrent injuries [4]. In fact, previous HSI is a primary risk factor of a re-injury across literature [5,6]. Research into BFlh injuries continues to develop and has led to a better understanding of the problem [7].
Hamstring strength is one of the muscle properties that has received more attention in current research both as preventive and performance-enhancing strategy [8,9,10]. It seems that hamstring strength deficit is a good predictor of HSI [6]. In addition, strength has been also found to be a risk factor for preventing HSI in recent prospective cohort studies [8,11,12]. At the same time, hamstring strength seems to be positively correlated with athletic performance [13,14]. In fact, mostly all sport teams include hamstring strength exercises as part of their performance-enhancing and prevention strategy [15,16,17,18]. Improving athletic performance is a common objective in the sports field. The hamstring muscles are essential in many aspects of sports practice [18]. Hamstring muscle activity is higher than any other muscle group during a sport maneuver as essential to sport as sprinting [18]. For this reason, hamstring training exercises are a crucial component of sports performance.
Interestingly, there are a lot of strength exercises described and used in the current literature, making it difficult to determine the most appropriate when developing specific programs for the training of these muscles.
Several studies had compared BFlh muscle activation by using the surface electromyography (sEMG) activity level between hamstring strength exercises [19,20,21]. sEMG has been shown to be a good instrument to determine muscle activation levels during strength exercises [22]. sEMG has been used to categorize exercise intensity, and therefore, assisting sport coaches and physiotherapists when selecting the most appropriated exercise [21,23]. Previous studies have systematically reviewed muscle activation during commonly used strength exercises in the gluteus maximus (GMax) [24,25], which is another important hip extensor. However, no systematic review has previously investigated the differences in biceps femoris muscle activation across strength exercises. Therefore, the purpose of the current systematically review was to evaluate biceps femoris sEMG during the most common strengthening exercises in a healthy population.
2. Materials and Methods
2.1. Registration
The systematic review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement checklist [26]. The systematic review protocol was registered in the PROSPERO database with ID: CRD42020183079.
2.2. Information Sources and Search
The search strategy was developed following the PICO (Population, Intervention, Comparison, Outcomes) strategy.
Population: healthy adults without lower extremity injury;
Intervention: biceps femoris activation during hamstring strength exercises;
Comparison: no comparison due to specific cross-sectional study designs;
Outcome: biceps femoris muscle activity as assessed with sEMG was primary outcome. The “last 10 years” filter was used in all three databases. Keywords used to develop the search strategy are shown in Table 1.

Table 1.
Keywords used for the search strategy.
Databases used in the current systematic review were PubMed, Cochrane Library, and Web of Science. Furthermore, the lists of references from the studies included were checked to find other studies meeting inclusion criteria. The final search was performed on 1 May 2020. A complete PubMed database search strategy example is shown in Table 2.

Table 2.
Example of search strategy in PubMed database.
2.3. Eligibility Criteria and Study Selection
The inclusion criteria for studies included in this systematic review were as follows: (1) cross-sectional design; (2) healthy individuals; (3) evaluation of hamstring strength exercises; (4) providing data about sEMG of hamstring muscles; (5) providing data normalized by MVIC; (6) specific data about BFlh or “lateral hamstring musculature”; (7) English or Spanish language; and (8) published during the last 10 years. Studies were excluded if they included: (1) elderly people; (2) did not provide percentage activation data; or (3) did not specify the normalization method. Moreover, if studies provided data via bar charts, the corresponding author of the article was contacted, and the means and standard deviations of each exercise were requested.
Titles and abstracts were screened by two independent authors (SRS and LLL). In case of discrepancy, a third author (APB) was consulted. The Cohen’s Kappa index was used in order to assess the inter-rater agreement. Landis et al. [27] categorized the Kappa Statistic as <0.00 as poor inter-rater agreement, 0.00–0.20 as slight, 0.21–0.40 as fair, 0.41–0.60 as moderate, 0.61–0.80 as substantial, and 0.81–1.00 as almost perfect inter-rater agreement.
2.4. Data Collection Process
The following data were extracted for studies included in this systematic review: (1) Author’s last name and year of publication; (2) sample size; (3) exercises performed; (4) normalization method; (5) electrode placement; and (6) testing load.
2.5. Outcomes
As primary outcome, the average sEMG root mean square (RMS) expressed as a percentage of MVIC for BFlh /lateral hamstring musculature was chosen.
This review categorized hamstring exercises according to muscle activation of the hamstring muscles following Macadam and Feser [28]: low activation (0 to 20% Maximal Voluntary Isometric Contraction, MVIC), moderate activation (21 to 40% MVIC), high activation (41 to 60% MVIC), or very high activation (61% or greater MVIC).
2.6. Risk of Bias of Individual Studies
The National Institutes of Health Quality Assessment Tool for Observational Cohort and Cross-sectional Studies was used to assess the methodology quality of the included studies [29]. This tool contains 14 quality questions assessing internal validity (population, sample size, statistical analysis, and outcome measures). Questions must be answered as “Yes”, “No”, “cannot determine (CD)”, “not applicable (NA)”, or “not reported (NR)”. Cross-sectional studies automatically scored “not applicable” on criteria 6, 7 and 10 (Supplementary Table S1). One point was obtained only if the question was answered as “Yes”. All questions were equally weighted in overall quality assessment results.
3. Results
3.1. Study Selection
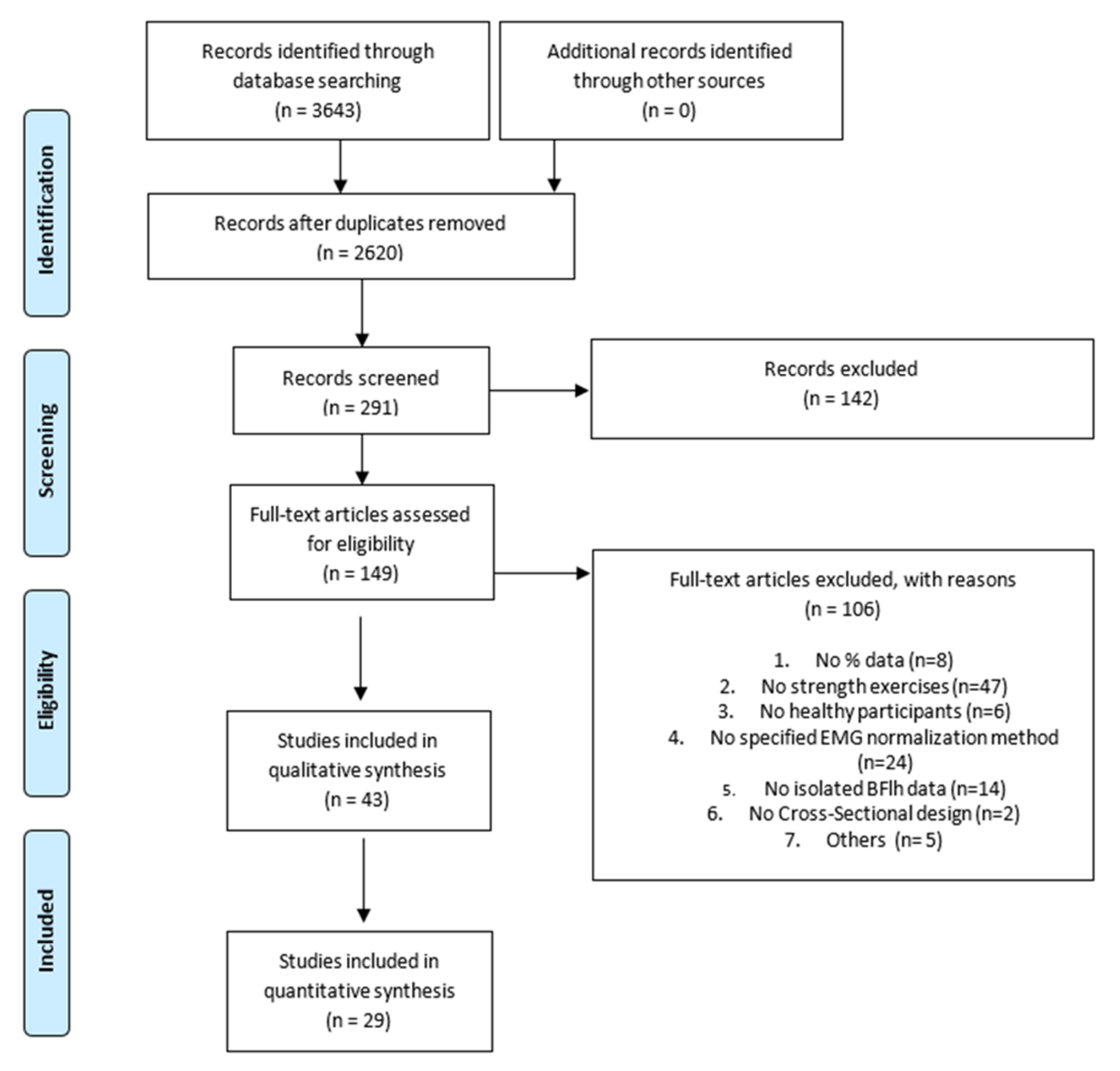
The search strategy found a total of 3643 studies (PubMed: 987; ScienceDirect: 2083; Cochrane Library: 573). Two thousand six hundred and twenty studies were initially included after checking for duplicates. After title screening, 291 studies were considered for full abstract screening. One hundred and forty-two studies were excluded after reading the abstract, so 143 full-text articles were assessed for eligibility. Full-text screening was carried out, and 43 studies finally met the inclusion criteria. The reasons for the exclusion of 106 studies were as follows: did not provide data as %MVIC (n = 8), did not assess hamstring strength exercises (n = 47), did not include healthy participants (n = 6), did not specify sEMG normalization method (n = 24), did not provide isolated BFlh/lateral hamstring data (n = 14), no cross-sectional design (n = 2), others (n = 5). Finally, 43 studies were included in the qualitative analysis. From these 43, twenty did not provide numerical data other than bar charts. Thus, the corresponding authors from these papers were contacted. Twenty-nine studies were finally included in the quantitative analysis. The Cohen’s Kappa index showed an “almost perfect” agreement (k = 0.87). The detailed study selection and reasons for excluded articles can be found in the PRISMA flow chart (Figure 1).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) flow diagram.
3.2. Study Characteristics
Studies involved a total of 507 participants with an age ranging from 19 to 30 years. The exercises mostly commonly assessed in the studies were swings, dead lifts, Nordic hamstring exercises (NHE), squats, leg curls, lunges, good mornings, hip thrusts, and hip extensions. The majority of the studies normalized hamstring EMG data by using MVC in prone position with the knee flexed at 45° and the sEMG electrodes placed following the Surface Electromyography for the Non-Invasive Assessment of Muscles (SENIAM) guideline [30].
The testing load differed among studies, but bodyweight was the more commonly used load. Table 3 summarizes the characteristics of the included studies.

Table 3.
Characteristics of included exercises.
3.3. Quality Assessment
The studies included in this systematic review showed a mean score of 5.75 from a total of 11 points (from 4 to 8 points) in the National Institutes of Health Quality Assessment Tool for Observational Cohort and Cross-sectional Studies [29].
3.4. Muscle Activation
A total of 114 exercises were assessed across articles included in this review. Two different evaluations were performed across exercises. Firstly, we assessed them and ordered them from lower to higher biceps femoris activation (based on %MVIC). Secondly, as many studies performed similar exercises, we grouped them into the following categories: Nordics, deadlifts, hip thrust, swing, squats, good mornings, bridges, hip extensions, isokinetic exercises, and lunges (Figure 2). Data regarding the 114 exercises are available in Supplementary Table S2.
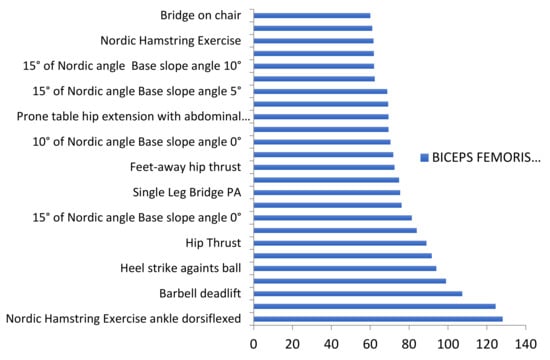
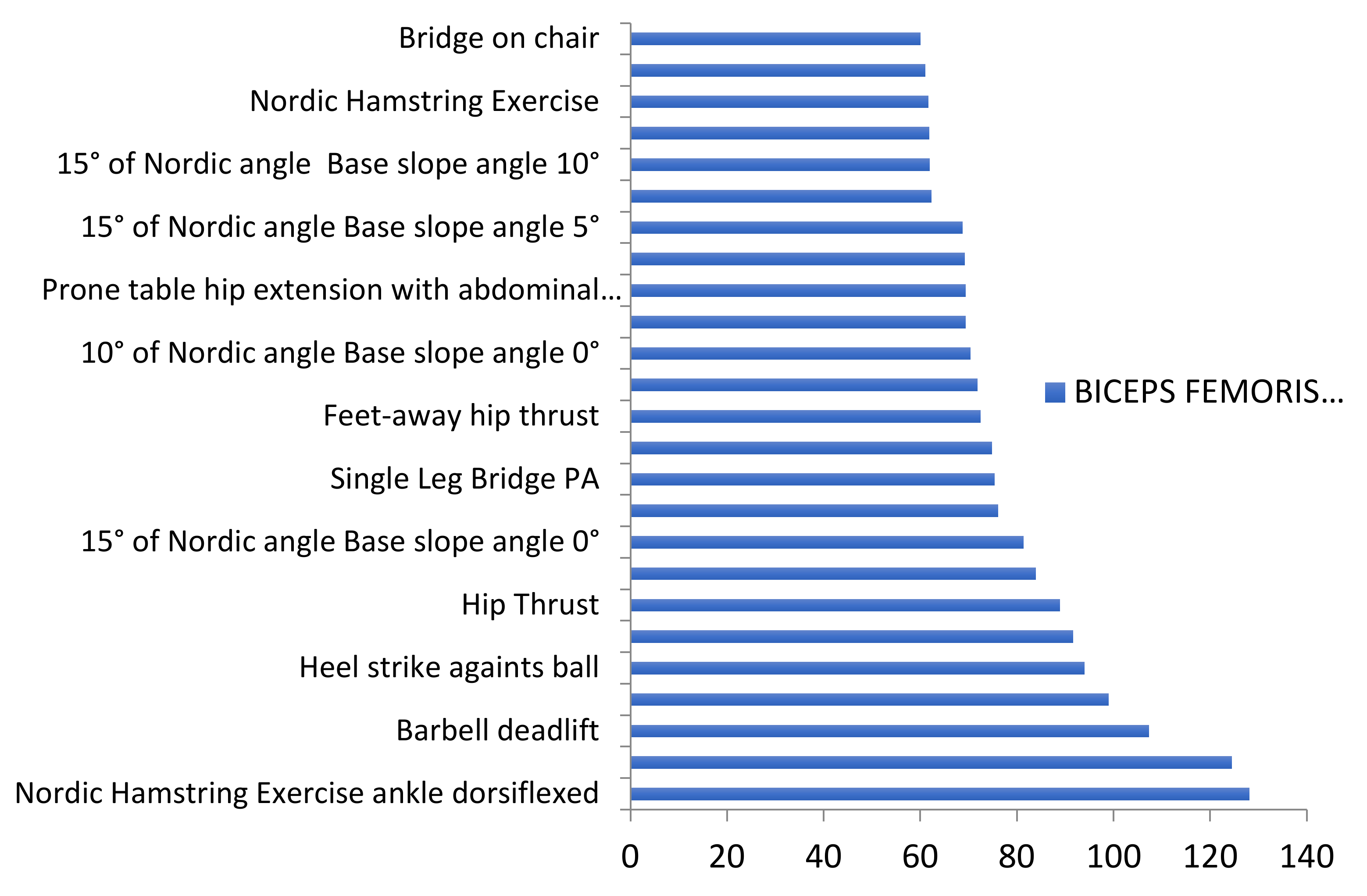
Figure 2.
Exercises with very high BF activation levels.
This figure highlights both NHEs from Comfort et al. [52] and barbell deadlifts from Andersen et al. [59] with biceps femoris activation higher than 100% MVIC. Moreover, the slip leg exercise and the heel strike against ball exercise from Arias-Poblete et al. [39] achieved 99% and 94% of BFlh activation, respectively.
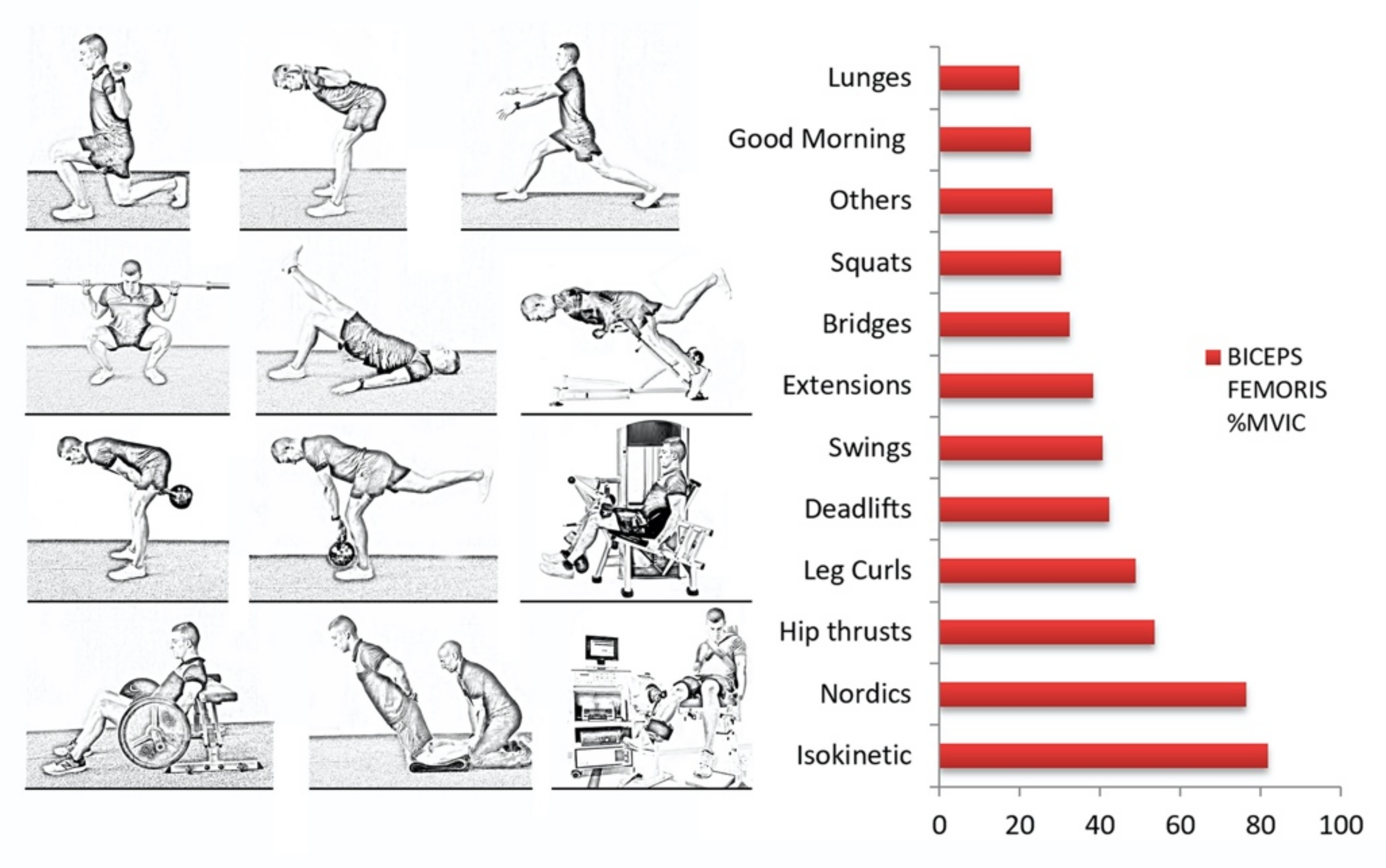
The assessment of categories instead of exercises gives more global information about the exercise typology. Moreover, it minimizes a possible bias in one study which could notably alter the results. Figure 3 shows the results of BFlh activation levels by categories.
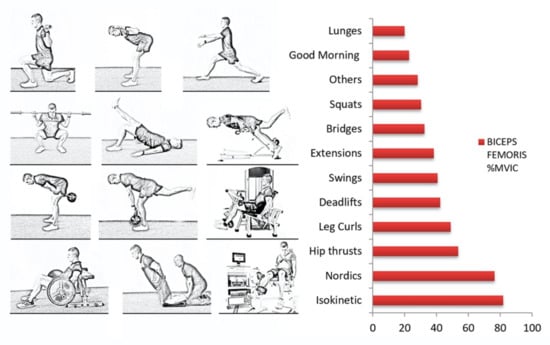
Figure 3.
Categories ordered by BF mean activation levels.
Very high activation (>60%MVIC).
Isokinetic exercises represented the highest biceps femoris activation with a mean of 81.7%MVIC. However, only two exercises were able to be included in this category. Furthermore, NHE also achieved a very high mean activation of 76.5%MVIC. In this second case, eleven NHEs were evaluated. All of them achieved a mean activation higher than 60%MVIC. In fact, the NHE with ankle dorsiflexion achieved the higher BFlh activation in this systematic review with 128%MVIC.
High activation (from 41% to 60%MVIC).
Three exercise categories showed a mean activation between 41% and 60% of the MVIC: hip thrust (53.50%), leg curl (48.78%), and deadlifts (42.17%).
Moderate activation (from 21% to 40%MVIC).
Swing exercises (40.52%), hip or back extensions (38.19%), glute bridges (32.34%), squats (30.24%), other exercises (28.09%), and good mornings (22.79%) were the six categories that produced a moderate activation of the BFlh muscle.
Low activation (<20%MVIC).
Only the lunge exercise category achieved a mean activation lower than 20%. This category showed a mean BFlh activation level of 19.82% of MVIC.
4. Discussion
This systematic review aimed to evaluate the biceps femoris activation among different strength hamstring exercises. The results have shown that the Nordic hamstring exercise with ankle dorsiflexion is the exercise achieving the highest BFlh muscle activation. Moreover, the Nordic hamstring category (all variations) is the second-best exercise for BG activation category. These results may assist coaches, practitioners, or physiotherapists in selecting exercises based on intensity purposes.
The Nordic hamstring exercise has been widely used in the literature. Its first use in research was 2004 when Mjølsnes et al. [60] evaluated its effectiveness in hamstring eccentric strength. The use of NHE to improve hamstring eccentric strength is undoubtable. Several publications [61,62,63] and a recent systematic review and meta-analysis [64] support this idea. Furthermore, the meta-analyses from van Dyk et al. [65] and Al Attar et al. [66] concluded that including the NHE as an injury prevention exercise reduces the rate of HSI. Although some authors have questioned its use [67], current and previous data support the NHE as being associated with the highest levels of muscle BFlh activation.
The isokinetic exercise category was the highest in BFlh activation of all the categories. Isokinetic exercises have been commonly used for testing, for predicting injury risk, and as criteria for return to play after both hamstring and anterior cruciate ligament injury [6,68,69]. However, results from this study also support its use as a potential form of hamstring strengthening due to its very high activation of the biceps femoris muscle.
The results from the two exercises included in the “others” category also need attention. The “slip leg” and “heel strike against ball” exercises are quite different from deadlifts, swings, thrusts, curls, etc. However, they have shown activation levels of 94% and 99% of MVIC, placing them at the top fourth and fifth position in the ranking. Thus, these results would recommend these exercises as part of high-intensity hamstring training.
On the other hand, lunges were the lowest BFlh activation category. These results are due to the fact that lunge exercises are commonly used for improving gluteus muscle but not hamstring strength. In fact, a systematic review evaluating gluteus maximus activation during common strength exercises found lunges variations as high activity (>60% of MVIC) exercises [24]. Thus, this kind of exercise should not be performed when hamstring activation and strength is the objective of the program.
This review focuses on muscle activation during different exercises commonly used to improve sport performance. However, other parameters such as strength, timing, or position may play an important role when choosing exercises [6,70,71]. Malliaropoulus et al. [6] supported the idea that hamstring strength exercises should also be oriented to specific sport demands. The highest activation of the biceps femoris occurs during the late swing phase and early stance phase of high speed running [71]. Thus, both open and closed kinetic chain exercises should be supported to reproduce the high demands of sprinting during sport maneuvers. Furthermore, hamstrings present a dual role in both hip and knee joints at the same time while running [72]. For this reason, both hip and knee dominant exercises should be supported to “simulate” their function during sprinting [6,73].
Although muscle activation gains are usually understood to be a prediction of strength gains, this relationship has not been scientifically proven [70]. This difference between muscle activation and strength must be taken into account when interpreting current results. Nevertheless, it should be also considered how this muscle is integrated in relation to other synergistic muscles involved in the particular or specific movement pattern [70].
4.1. Limitations
We should recognize some limitations from this systematic review. First, some studies evaluating the impact of exercise selection on muscle activity had to be excluded because they did not normalize their sEMG data by MVIC test. Second, in this systematic review, we did not consider exercise loads due to the high heterogeneity and the fact that it could alter the results. The high variability in the normalization methods makes difficult to compare directly several studies. Finally, current data are based only on healthy people; we do not currently know if muscle activation of injured sports players would exhibit a similar tendency. Furthermore, this review did not specify whether the participants were professional athletes or amateurs, nor did it specify the type of sport practiced. Therefore, it cannot be assured that these results can be extrapolated to a specific sport or to a specific level of sport expertise.
4.2. Sports and Clinical Applications
The strength training BFlh programs must be effective and specific to the necessity of sports athletes. The effective BFlh training programs are mandatory to enhance athletic performance. Exercise selection plays an important role to achieve this. This systematic review provides evidence regarding which exercises activate more the biceps femoris, which is one of the main muscles in sports. The results have shown that Nordic hamstring exercises and isokinetic exercises were more efficient to activate the BFlh more.
5. Conclusions
The results from this systematic review allow coaches, athletic trainers, and physical therapists to classify different exercises from low to high muscle activation of the BFlh. These data could implement a progressive training strategy to improve hamstrings strength and therefore athletic performance. However, although this review involves data from more than five hundred participants, individual anatomy variations could modify muscle activations during exercises. Thus, an anamnesis and physical examination of each participant is always recommended in order to individualize exercise selection.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijerph18168733/s1, Table S1: Risk of Bias of Individual Studies and Table S2: Muscle Activation.
Author Contributions
Conceptualization, A.P.-B. and L.L.-A.; methodology, N.L.-L., S.R.-S. and J.R.-S.; formal analysis, L.L.-A., C.F.-d.-l.-P. and C.L.-d.-C.; writing—original draft preparation, A.P.-B., C.F.-d.-l.-P. and L.L.-A.; writing—review and editing, N.L.-L., R.A.-A., C.L.-d.-C., S.R.-S. and J.R.-S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Erickson, L.N.; Sherry, M.A. Rehabilitation and return to sport after hamstring strain injury. J. Sport Health Sci. 2017, 6, 262–270. [Google Scholar] [CrossRef]
- Mendiguchia, J.; Alentorn-Geli, E.; Brughelli, M. Hamstring strain injuries: Are we heading in the right direction? Br. J. Sports Med. 2012, 46, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Bourne, M.N.; Opar, D.A.; Williams, M.D.; Al Najjar, A.; Shield, A.J. Muscle activation patterns in the Nordic hamstring exercise: Impact of prior strain injury. Scand. J. Med. Sci. Sports 2016, 26, 666–674. [Google Scholar] [CrossRef]
- Dalton, S.L.; Kerr, Z.Y.; Dompier, T.P. Epidemiology of Hamstring Strains in 25 NCAA Sports in the 2009–2010 to 2013–2014 Academic Years. Am. J. Sports Med. 2015, 43, 2671–2679. [Google Scholar] [CrossRef] [PubMed]
- Freckleton, G.; Pizzari, T. Risk factors for hamstring muscle strain injury in sport: A systematic review and meta-analysis. Br. J. Sports Med. 2013, 47, 351–358. [Google Scholar] [CrossRef]
- Lee, J.W.Y.; Mok, K.-M.; Chan, H.C.K.; Yung, P.S.H.; Chan, K.-M. Eccentric hamstring strength deficit and poor hamstring-to-quadriceps ratio are risk factors for hamstring strain injury in football: A prospective study of 146 professional players. J. Sci. Med. Sport 2018, 21, 789–793. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Bellmunt, A.; Miguel-Pérez, M.; Brugué, M.B.; Cabús, J.B.; Casals, M.; Martinoli, C.; Kuisma, R. An anatomical and histological study of the structures surrounding the proximal attachment of the hamstring muscles. Man. Ther. 2015, 20, 445–450. [Google Scholar] [CrossRef]
- Maniar, N.; Shield, A.J.; Williams, M.D.; Timmins, R.G.; Opar, D.A. Hamstring strength and flexibility after hamstring strain injury: A systematic review and meta-analysis. Br. J. Sports Med. 2016, 50, 909–920. [Google Scholar] [CrossRef]
- Opar, D.A.; Williams, M.D.; Shield, A.J. Hamstring strain injuries: Factors that lead to injury and re-injury. Sports Med. 2012, 42, 209–226. [Google Scholar] [CrossRef]
- Opar, D.A.; Williams, M.D.; Timmins, R.G.; Hickey, J.; Duhig, S.J.; Shield, A.J. Eccentric Hamstring Strength and Hamstring Injury Risk in Australian Footballers. Med. Sci. Sports Exerc. 2015, 47, 857–865. [Google Scholar] [CrossRef]
- Opar, D.A.; Williams, M.D.; Timmins, R.G.; Dear, N.M.; Shield, A.J. Knee flexor strength and bicep femoris electromyographical activity is lower in previously strained hamstrings. J. Electromyogr. Kinesiol. Off. J. Int. Soc. Electrophysiol. Kinesiol. 2013, 23, 696–703. [Google Scholar] [CrossRef]
- Timmins, R.G.; Bourne, M.N.; Shield, A.J.; Williams, M.D.; Lorenzen, C.; Opar, D.A. Short biceps femoris fascicles and eccentric knee flexor weakness increase the risk of hamstring injury in elite football (soccer): A prospective cohort study. Br. J. Sports Med. 2016, 50, 1524–1535. [Google Scholar] [CrossRef]
- Markovic, G.; Sarabon, N.; Boban, F.; Zoric, I.; Jelcic, M.; Sos, K.; Scappaticci, M. Nordic Hamstring Strength of Highly Trained Youth Football Players and Its Relation to Sprint Performance. J. Strength Cond. Res. 2020, 34, 800–807. [Google Scholar] [CrossRef]
- Ishøi, L.; Aagaard, P.; Nielsen, M.F.; Thornton, K.B.; Krommes, K.K.; Hölmich, P.; Thorborg, K. The Influence of Hamstring Muscle Peak Torque and Rate of Torque Development for Sprinting Performance in Football Players: A Cross-Sectional Study. Int. J. Sports Physiol. Perform. 2019, 14, 665–673. [Google Scholar] [CrossRef]
- O’Brien, J.; Finch, C.F. Injury prevention exercise programmes in professional youth soccer: Understanding the perceptions of programme deliverers. BMJ Open Sport Exerc. Med. 2016, 2, e000075. [Google Scholar] [CrossRef] [PubMed]
- Read, P.J.; Jimenez, P.; Oliver, J.L.; Lloyd, R.S. Injury prevention in male youth soccer: Current practices and perceptions of practitioners working at elite English academies. J. Sports Sci. 2018, 36, 1423–1431. [Google Scholar] [CrossRef] [PubMed]
- Emery, C.A.; Roy, T.-O.; Whittaker, J.L.; Nettel-Aguirre, A.; van Mechelen, W. Neuromuscular training injury prevention strategies in youth sport: A systematic review and meta-analysis. Br. J. Sports Med. 2015, 49, 865–870. [Google Scholar] [CrossRef] [PubMed]
- Morin, J.-B.; Gimenez, P.; Edouard, P.; Arnal, P.; Jimenez-Reyes, P.; Samozino, P.; Brughelli, M.; Mendiguchia, J. Sprint Acceleration Mechanics: The Major Role of Hamstrings in Horizontal Force Production. Front. Physiol. 2015, 6, 404. [Google Scholar] [CrossRef] [PubMed]
- Hegyi, A.; Csala, D.; Péter, A.; Finni, T.; Cronin, N.J. High-density electromyography activity in various hamstring exercises. Scand. J. Med. Sci. Sports 2019, 29, 34–43. [Google Scholar] [CrossRef] [PubMed]
- McCurdy, K.; Walker, J.; Yuen, D. Gluteus Maximus and Hamstring Activation During Selected Weight-Bearing Resistance Exercises. J. Strength Cond. Res. 2018, 32, 594–601. [Google Scholar] [CrossRef]
- Bourne, M.N.; Williams, M.D.; Opar, D.A.; Al Najjar, A.; Kerr, G.K.; Shield, A.J. Impact of exercise selection on hamstring muscle activation. Br. J. Sports Med. 2017, 51, 1021–1028. [Google Scholar] [CrossRef]
- Enoka, R.M.; Duchateau, J. Inappropriate interpretation of surface EMG signals and muscle fiber characteristics impedes understanding of the control of neuromuscular function. J. Appl. Physiol. 2015, 119, 1516–1518. [Google Scholar] [CrossRef]
- Bourne, M.N.; Timmins, R.G.; Opar, D.A.; Pizzari, T.; Ruddy, J.D.; Sims, C.; Williams, M.D.; Shield, A.J. An Evidence-Based Framework for Strengthening Exercises to Prevent Hamstring Injury. Sports Med. 2018, 48, 251–267. [Google Scholar] [CrossRef]
- Neto, W.K.; Soares, E.G.; Vieira, T.L.; Aguiar, R.; Chola, T.A.; Sampaio, V.; de Lima Sampaio, V.; Gama, E.F. Gluteus Maximus Activation during Common Strength and Hypertrophy Exercises: A Systematic Review. J. Sports Sci. Med. 2020, 19, 195–203. [Google Scholar]
- Reiman, M.P.; Bolgla, L.A.; Loudon, J.K. A literature review of studies evaluating gluteus maximus and gluteus medius activation during rehabilitation exercises. Physiother. Theory Pract. 2012, 28, 257–268. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Altman, D.; Antes, G.; Atkins, D.; Barbour, V.; Barrowman, N.; Berlin, J.A.; et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The Measurement of Observer Agreement for Categorical Data. Biometrics 1977, 33, 159. [Google Scholar] [CrossRef] [PubMed]
- Macadam, P.; Feser, E.H. Examination of Gluteus Maximus Electromyographyic Excitation Associated with Dynamic Hip Extension during Body Weight Exercise: A Systematic Review. Int. J. Sports Phys. Ther. 2019, 14, 14–31. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.-L.; Wang, Y.-Y.; Yang, Z.-H.; Huang, D.; Weng, H.; Zeng, X.-T. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: What are they and which is better? Mil. Med. Res. 2020, 7, 7. [Google Scholar] [CrossRef] [PubMed]
- Hermens, H.J.; Freriks, B.; Disselhorst-Klug, C.; Rau, G. Development of recommendations for SEMG sensors and sensor placement procedures. J. Electromyogr. Kinesiol. 2000, 10, 361–374. [Google Scholar] [CrossRef]
- Jeon, I.; Hwang, U.; Jung, S.; Kwon, O. Comparison of gluteus maximus and hamstring electromyographic activity and lumbopelvic motion during three different prone hip extension exercises in healthy volunteers. Phys. Ther. Sport 2016, 22, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Kendall, F.P.; McCreary, E.K.; Provance, P.G. Muscle Testing and Function, 5th ed.; Williams & Wilkins: Baltimore, MD, USA, 2005. [Google Scholar]
- Del Monte, M.J.; Opar, D.A.; Timmins, R.G.; Ross, J.A.; Keogh, J.W.; Lorenzen, C. Hamstring Myoelectrical Activity During Three Different Kettlebell Swing Exercises. J. Strength Cond. Res. 2020, 34, 1953–1958. [Google Scholar] [CrossRef] [PubMed]
- Lyons, B.C.; Mayo, J.J.; Tucker, W.S.; Wax, B.; Hendrix, R.C. Electromyographical Comparison of Muscle Activation Patterns Across Three Commonly Performed Kettlebell Exercises. J. Strength Cond. Res. 2017, 31, 2363–2370. [Google Scholar] [CrossRef] [PubMed]
- Monajati, A.; Larumbe-Zabala, E.; Goss-Sampson, M.; Naclerio, F. Analysis of the Hamstring Muscle Activation During two Injury Prevention Exercises. J. Hum. Kinet. 2017, 60, 29–37. [Google Scholar] [CrossRef]
- Lehecka, B.J.; Edwards, M.; Haverkamp, R.; Martin, L.; Porter, K.; Thach, K.; Sack, R.J.; Hakansson, N.A. Building a Better Gluteal Bridge: Electromyographyic Analysis of Hip Muscle Activity during Modified Single-leg Bridges. Int. J. Sports Phys. Ther. 2017, 12, 543–549. [Google Scholar]
- Marshall, P.W.M.; Desai, I. Electromyographic analysis of upper body, lower body, and abdominal muscles during advanced Swiss ball exercises. J. Strength Cond. Res. 2010, 24, 1537–1545. [Google Scholar] [CrossRef]
- Khaiyat, O.A.; Norris, J. Electromyographic activity of selected trunk, core, and thigh muscles in commonly used exercises for ACL rehabilitation. J. Phys. Ther. Sci. 2018, 30, 642–648. [Google Scholar] [CrossRef]
- Arias-Poblete, L.; Álvarez-Zúñiga, M.; Contreras-Diaz, G.; Jerez-Mayorga, D.; Antúnez, V.J.; Monteverde Sánchez, A. Classification of strengthening exercises of the lower member posterior chain, based on the amplitude of muscular activation in amateur soccer players between 18–25 years. J. Sport Health Res. 2019, 11, 155–163. [Google Scholar]
- Collazo García, C.L.; Rueda, J.; Suárez Luginick, B.; Navarro, E. Differences in the Electromyographic Activity of Lower-Body Muscles in Hip Thrust Variations. J. Strength Cond. Res. 2020, 34, 2449–2455. [Google Scholar] [CrossRef]
- Contreras, B.; Vigotsky, A.D.; Schoenfeld, B.J.; Beardsley, C.; Cronin, J. A Comparison of Gluteus Maximus, Biceps Femoris, and Vastus Lateralis Electromyography Amplitude for the Barbell, Band, and American Hip Thrust Variations. J. Appl. Biomech. 2016, 32, 254–260. [Google Scholar] [CrossRef]
- Severini, G.; Holland, D.; Drumgoole, A.; Delahunt, E.; Ditroilo, M. Kinematic and electromyographic analysis of the Askling L-Protocol for hamstring training. Scand. J. Med. Sci. Sports 2018, 28, 2536–2546. [Google Scholar] [CrossRef]
- Mausehund, L.; Skard, A.E.; Krosshaug, T. Muscle Activation in Unilateral Barbell Exercises: Implications for Strength Training and Rehabilitation. J. Strength Cond. Res. 2019, 33, S85–S94. [Google Scholar] [CrossRef] [PubMed]
- Vigotsky, A.D.; Harper, E.N.; Ryan, D.R.; Contreras, B. Effects of load on good morning kinematics and EMG activity. PeerJ 2015, 3, e708. [Google Scholar] [CrossRef]
- Lawrence, M.A.; Chin, A.; Swanson, B.T. Biomechanical Comparison of the Reverse Hyperextension Machine and the Hyperextension Exercise. J. Strength Cond. Res. 2019, 33, 2053–2056. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-W.; Han, J.-Y.; Kang, M.-H.; Ha, S.-M.; Oh, J.-S. Comparison of Posterior Oblique Sling Activity during Hip Extension in the Prone Position on the Floor and on a Round Foam Roll. J. Phys. Ther. Sci. 2013, 25, 977–979. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jeon, I.; Kwon, O.; Weon, J.-H.; Hwang, U.; Jung, S.-H. Comparison of Hip- and Back-Muscle Activity and Pelvic Compensation in Healthy Subjects During 3 Different Prone Table Hip-Extension Exercises. J. Sport Rehabil. 2017, 26, 216–222. [Google Scholar] [CrossRef]
- Kawama, R.; Takahashi, K.; Wakahara, T. Effect of Hip Joint Position on Electromyographic Activity of the Individual Hamstring Muscles During Stiff-Leg Deadlift. J. Strength Cond. Res. 2021, 35, S38–S43. [Google Scholar] [CrossRef] [PubMed]
- Ryu, Y.; Roh, H. Cervical, Trunk, and Lower Extremity Muscle Activities during Bridging Exercise on Stable vs. Unstable Bases of Support. J. Phys. Ther. Sci. 2012, 24, 585–588. [Google Scholar] [CrossRef][Green Version]
- Choi, K.; Bak, J.; Cho, M.; Chung, Y. The effects of performing a one-legged bridge with hip abduction and use of a sling on trunk and lower extremity muscle activation in healthy adults. J. Phys. Ther. Sci. 2016, 28, 2625–2628. [Google Scholar] [CrossRef]
- Lee, J.-K.; Hwang, J.-H.; Kim, C.-M.; Lee, J.K.; Park, J.-W. Influence of muscle activation of posterior oblique sling from changes in activation of gluteus maximus from exercise of prone hip extension of normal adult male and female. J. Phys. Ther. Sci. 2019, 31, 166–169. [Google Scholar] [CrossRef]
- Comfort, P.; Regan, A.; Herrington, L.; Thomas, C.; McMahon, J.; Jones, P. Lack of Effect of Ankle Position During the Nordic Curl on Muscle Activity of the Biceps Femoris and Medial Gastrocnemius. J. Sport Rehabil. 2017, 26, 202–207. [Google Scholar] [CrossRef]
- Park, S.-Y.; Kim, S.-H.; Park, D.-J. Effect of slope angle on muscle activity during variations of the Nordic exercise. J. Exerc. Rehabil. 2019, 15, 832–838. [Google Scholar] [CrossRef]
- Muyor, J.M.; Martín-Fuentes, I.; Rodríguez-Ridao, D.; Antequera-Vique, J.A. Electromyographic activity in the gluteus medius, gluteus maximus, biceps femoris, vastus lateralis, vastus medialis and rectus femoris during the Monopodal Squat, Forward Lunge and Lateral Step-Up exercises. PLoS ONE 2020, 15, e0230841. [Google Scholar] [CrossRef] [PubMed]
- Jónasson, G.; Helgason, A.; Ingvarsson, Þ.; Kristjánsson, A.M.; Briem, K. The Effect of Tibial Rotation on the Contribution of Medial and Lateral Hamstrings During Isometric Knee Flexion. Sports Health A Multidiscip. Approach 2016, 8, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Yoo, W. Effects of hand and knee positions on muscular activity during trunk extension exercise with the Roman chair. J. Electromyogr. Kinesiol. 2014, 24, 972–976. [Google Scholar] [CrossRef]
- Contreras, B.; Vigotsky, A.D.; Schoenfeld, B.J.; Beardsley, C.; Cronin, J. A Comparison of Gluteus Maximus, Biceps Femoris, and Vastus Lateralis Electromyography Amplitude in the Parallel, Full, and Front Squat Variations in Resistance-Trained Females. J. Appl. Biomech. 2016, 32, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Narouei, S.; Imai, A.; Akuzawa, H.; Hasebe, K.; Kaneoka, K. Hip and trunk muscles activity during nordic hamstring exercise. J. Exerc. Rehabil. 2018, 14, 231–238. [Google Scholar] [CrossRef]
- Andersen, V.; Fimland, M.S.; Mo, D.-A.; Iversen, V.M.; Vederhus, T.; Rockland Hellebø, L.R.; Nordaune, K.I.; Saeterbakken, A.H. Electromyographic Comparison of Barbell Deadlift, Hex Bar Deadlift, and Hip Thrust Exercises: A Cross-Over Study. J. Strength Cond. Res. 2018, 32, 587–593. [Google Scholar] [CrossRef] [PubMed]
- Mjølsnes, R.; Arnason, A.; Østhagen, T.; Raastad, T.; Bahr, R. A 10-week randomized trial comparing eccentric vs. concentric hamstring strength training in well-trained soccer players. Scand. J. Med. Sci. Sports 2004, 14, 311–317. [Google Scholar] [CrossRef]
- Freeman, B.W.; Young, W.B.; Talpey, S.W.; Smyth, A.M.; Pane, C.L.; Carlon, T.A. The effects of sprint training and the Nordic hamstring exercise on eccentric hamstring strength and sprint performance in adolescent athletes. J. Sports Med. Phys. Fitness 2019, 59, 1119–1125. [Google Scholar] [CrossRef]
- Ribeiro-Alvares, J.B.; Marques, V.B.; Vaz, M.A.; Baroni, B.M. Four Weeks of Nordic Hamstring Exercise Reduce Muscle Injury Risk Factors in Young Adults. J. Strength Cond. Res. 2018, 32, 1254–1262. [Google Scholar] [CrossRef] [PubMed]
- Seymore, K.D.; Domire, Z.J.; DeVita, P.; Rider, P.M.; Kulas, A.S. The effect of Nordic hamstring strength training on muscle architecture, stiffness, and strength. Eur. J. Appl. Physiol. 2017, 117, 943–953. [Google Scholar] [CrossRef]
- Medeiros, D.M.; Marchiori, C.; Baroni, B.M. Effect of Nordic Hamstring Exercise Training on Knee Flexors Eccentric Strength and Fascicle Length: A Systematic Review and Meta-Analysis. J. Sport Rehabil. 2020, 30, 482–491. [Google Scholar] [CrossRef] [PubMed]
- Van Dyk, N.; Behan, F.P.; Whiteley, R. Including the Nordic hamstring exercise in injury prevention programmes halves the rate of hamstring injuries: A systematic review and meta-analysis of 8459 athletes. Br. J. Sports Med. 2019, 53, 1362–1370. [Google Scholar] [CrossRef] [PubMed]
- Al Attar, W.S.A.; Alshehri, M.A. A meta-analysis of meta-analyses of the effectiveness of FIFA injury prevention programs in soccer. Scand. J. Med. Sci. Sports 2019, 29, 1846–1855. [Google Scholar] [CrossRef] [PubMed]
- Tyler, T.F.; Schmitt, B.M.; Nicholas, S.J.; McHugh, M.P. Rehabilitation After Hamstring-Strain Injury Emphasizing Eccentric Strengthening at Long Muscle Lengths: Results of Long-Term Follow-Up. J. Sport Rehabil. 2017, 26, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Van Dyk, N.; Bahr, R.; Whiteley, R.; Tol, J.L.; Kumar, B.D.; Hamilton, B.; Farooq, A.; Witvrouw, E. Hamstring and Quadriceps Isokinetic Strength Deficits Are Weak Risk Factors for Hamstring Strain Injuries. Am. J. Sports Med. 2016, 44, 1789–1795. [Google Scholar] [CrossRef]
- Abdel-aziem, A.A.; Soliman, E.S.; Abdelraouf, O.R. Isokinetic peak torque and flexibility changes of the hamstring muscles after eccentric training: Trained versus untrained subjects. Acta Orthop. Traumatol. Turc. 2018, 52, 308–314. [Google Scholar] [CrossRef]
- Vigotsky, A.D.; Halperin, I.; Lehman, G.J.; Trajano, G.S.; Vieira, T.M. Interpreting Signal Amplitudes in Surface Electromyography Studies in Sport and Rehabilitation Sciences. Front. Physiol. 2018, 8, 985. [Google Scholar] [CrossRef]
- Chumanov, E.S.; Heiderscheit, B.C.; Thelen, D.G. The effect of speed and influence of individual muscles on hamstring mechanics during the swing phase of sprinting. J. Biomech. 2007, 40, 3555–3562. [Google Scholar] [CrossRef]
- Novacheck, T.F. The biomechanics of running. Gait Posture 1998, 7, 77–95. [Google Scholar] [CrossRef]
- Mendiguchia, J.; Conceição, F.; Edouard, P.; Fonseca, M.; Pereira, R.; Lopes, H.; Morin, J.-B.; Jiménez-Reyes, P. Sprint versus isolated eccentric training: Comparative effects on hamstring architecture and performance in soccer players. PLoS ONE 2020, 15, e0228283. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).