The Effect of Group Music Therapy with Physical Activities to Prevent Frailty in Older People Living in the Community
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
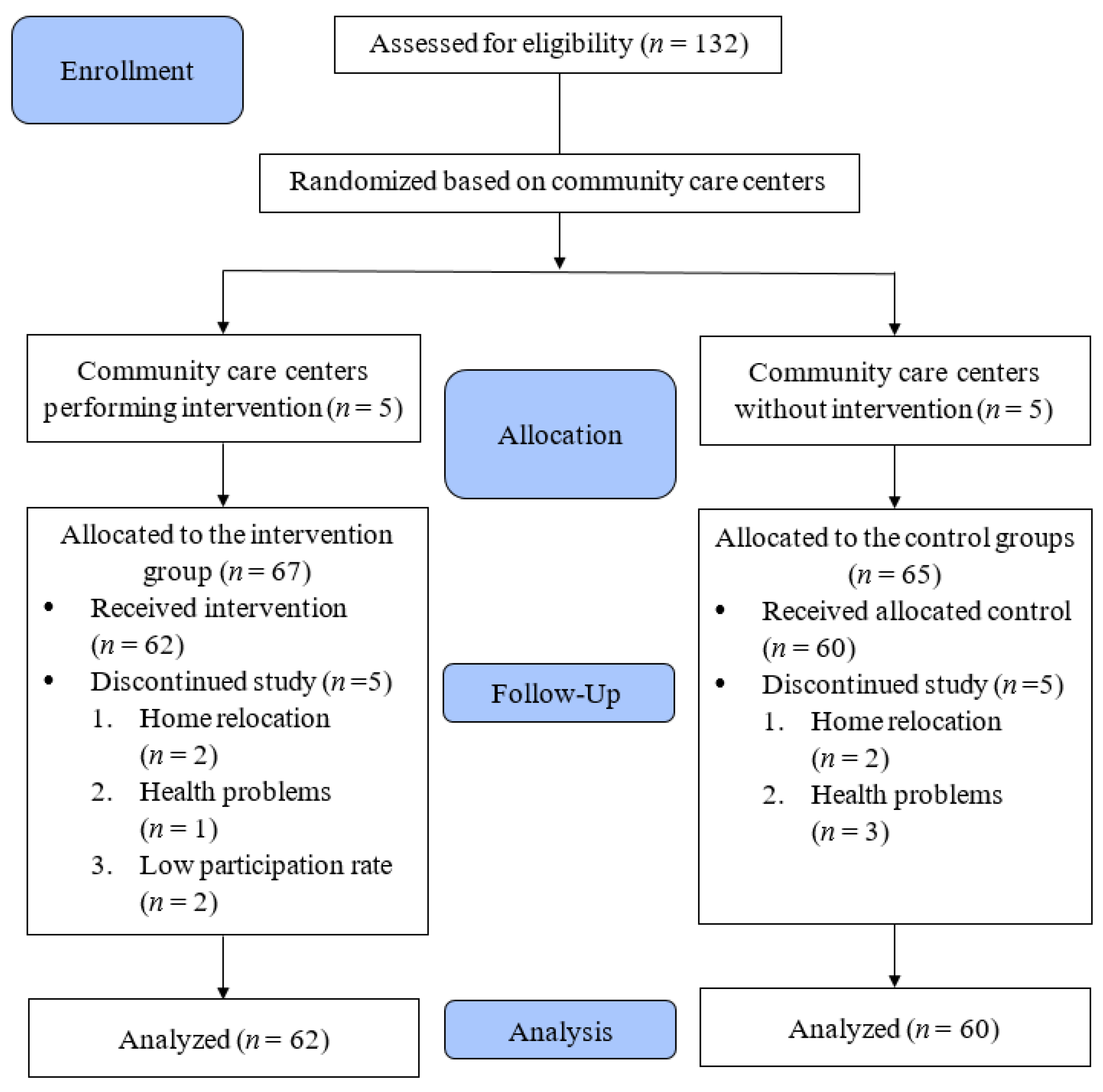
2.2. Sample and Settings
2.3. Intervention
2.4. Data Collection
2.4.1. Kihon Checklist (KCL)
2.4.2. Senior Fitness Test
2.4.3. Mini-Mental Status Examination (MMSE)
2.4.4. Geriatric Depression Scale-Short Form (GDS-SF)
2.5. Data Analysis
3. Results
4. Discussion
4.1. Study Limitations
4.2. Relevance to Clinical Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- He, W.; Goodkind, D.; Kowal, P.R. An Aging World, 2015. 2016. Available online: https://ifa.ngo/wp-content/uploads/2016/04/An-Aging-World-2015-Census-bureau-and-WHO.pdf (accessed on 21 May 2021).
- Ministry of the Interior. Resident Population by Age of 0–14, 15–64, 65+ and by 6-Year Age Group. Available online: https://www.moi.gov.tw/files/site_stuff/321/1/month/month.html (accessed on 21 May 2021).
- National Development Council. Population Projections for the R.O.C. Available online: https://pop-proj.ndc.gov.tw/main_en/dataSearch.aspx?uid=78&pid=78 (accessed on 28 July 2021).
- Ofori-Asenso, R.; Chin, K.L.; Mazidi, M.; Zomer, E.; Ilomaki, J.; Zullo, A.R.; Gasevic, D.; Ademi, Z.; Korhonen, M.J.; LoGiudice, D.; et al. Global Incidence of Frailty and Prefrailty Among Community-Dwelling Older Adults: A Systematic Review and Meta-analysis. JAMA Netw. Open 2019, 2, e198398. [Google Scholar] [CrossRef] [Green Version]
- Cheng, M.-H.; Chang, S.-F. Frailty as a Risk Factor for Falls among Community Dwelling People: Evidence from a Meta-Analysis. J. Nurs. Sch. 2017, 49, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Lally, F.; Crome, P. Understanding frailty. Postgrad. Med. J. 2007, 83, 16–20. [Google Scholar] [CrossRef] [PubMed]
- Han, L.; Clegg, A.; Doran, T.; Fraser, L. The impact of frailty on healthcare resource use: A longitudinal analysis using the Clinical Practice Research Datalink in England. Age Ageing 2019, 48, 665–671. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in Older Adults: Evidence for a Phenotype. J. Gerontol. Ser. A Biol. Sco. Med. Sci. 2001, 56, M146–M157. [Google Scholar] [CrossRef] [PubMed]
- Chu, W.; Chang, S.; Ho, H.; Lin, H. The Relationship Between Depression and Frailty in Community-Dwelling Older People: A Systematic Review and Meta-Analysis of 84,351 Older Adults. J. Nurs. Sch. 2019, 51, 547–559. [Google Scholar] [CrossRef]
- Ensrud, K.E.; Ewing, S.K.; Taylor, B.; Fink, H.A.; Cawthon, P.M.; Stone, K.L.; Hillier, T.A.; Cauley, J.A.; Hochberg, M.C.; Rodondi, N.; et al. Comparison of 2 Frailty Indexes for Prediction of Falls, Disability, Fractures, and Death in Older Women. Arch. Intern. Med. 2008, 168, 382–389. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horibe, Y.; Ueda, T.; Watanabe, Y.; Motokawa, K.; Edahiro, A.; Hirano, H.; Shirobe, M.; Ogami, K.; Kawai, H.; Obuchi, S.; et al. A 2-year longitudinal study of the relationship between masticatory function and progression to frailty or pre-frailty among community-dwelling Japanese aged 65 and older. J. Oral Rehabil. 2018, 45, 864–870. [Google Scholar] [CrossRef] [PubMed]
- Furtado, G.; Patrício, M.; Loureiro, M.; Teixeira, A.M.; Ferreira, J.P. Physical Fitness and Frailty Syndrome in Institutionalized Older Women. Percept. Mot. Ski. 2017, 124, 754–776. [Google Scholar] [CrossRef]
- Haider, S.; Grabovac, I.; Dorner, T.E. Effects of physical activity interventions in frail and prefrail community-dwelling people on frailty status, muscle strength, physical performance and muscle mass—A narrative review. Wien. Klin. Wochenschr. 2019, 131, 244–254. [Google Scholar] [CrossRef] [Green Version]
- Shimizu, N.; Umemura, T.; Hirai, T.; Tamura, T.; Sato, K.; Kusaka, Y. Effects of Movement Music Therapy with the Naruko Clapper on Psychological, Physical and Physiological Indices among Elderly Females: A Randomized Controlled Trial. Gerontology 2013, 59, 355–367. [Google Scholar] [CrossRef]
- Jun, E.-M.; Roh, Y.H.; Kim, M.J. The effect of music-movement therapy on physical and psychological states of stroke patients. J. Clin. Nurs. 2012, 22, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Li, H.-C.; Wang, H.-H.; Lu, C.-Y.; Chen, T.-B.; Lin, Y.-H.; Lee, I. The effect of music therapy on reducing depression in people with dementia: A systematic review and meta-analysis. Geriatr. Nurs. 2019, 40, 510–516. [Google Scholar] [CrossRef]
- Li, H.-C.; Wang, H.-H.; Chou, F.-H.; Chen, K.-M. The Effect of Music Therapy on Cognitive Functioning among Older Adults: A Systematic Review and Meta-Analysis. J. Am. Med Dir. Assoc. 2015, 16, 71–77. [Google Scholar] [CrossRef]
- Ministry of Health Labour and Welfare. Guidelines for the Comprehensive Project on Nursing Care Prevention/Daily Living Support. Available online: https://www.mhlw.go.jp/file/05-Shingikai-12301000-Roukenkyoku-Soumuka/0000052670.pdf (accessed on 20 December 2020).
- Arai, H.; Satake, S. English translation of the Kihon Checklist. Geriatr. Gerontol. Int. 2015, 15, 518–519. [Google Scholar] [CrossRef] [PubMed]
- Satake, S.; Senda, K.; Hong, Y.-J.; Miura, H.; Endo, H.; Sakurai, T.; Kondo, I.; Toba, K. Validity of the Kihon Checklist for assessing frailty status. Geriatr. Gerontol. Int. 2016, 16, 709–715. [Google Scholar] [CrossRef]
- Sentandreu-Mañó, T.; Fernández, I.; Iranzo, M.À.C.I.; Tomás, J.M. Dimensions underlying frailty indicators in the Kihon Checklist. Geriatr. Gerontol. Int. 2019, 19, 982–987. [Google Scholar] [CrossRef]
- Yamada, Y.; Nanri, H.; Watanabe, Y.; Yoshida, T.; Yokoyama, K.; Itoi, A.; Date, H.; Yamaguchi, M.; Miyake, M.; Yamagata, E.; et al. Prevalence of Frailty Assessed by Fried and Kihon Checklist Indexes in a Prospective Cohort Study: Design and Demographics of the Kyoto-Kameoka Longitudinal Study. J. Am. Med. Dir. Assoc. 2017, 18, 733.e7–733.e15. [Google Scholar] [CrossRef]
- Chen, H.-T.; Lin, C.-H.; Yu, L.-H. Normative Physical Fitness Scores for Community-Dwelling Older Adults. J. Nurs. Res. 2009, 17, 30–41. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.-M.; Chen, M.-H.; Hong, S.-M.; Chao, H.-C.; Lin, H.-S.; Li, C.-H. Physical fitness of older adults in senior activity centres after 24-week silver yoga exercises. J. Clin. Nurs. 2008, 17, 2634–2646. [Google Scholar] [CrossRef] [PubMed]
- Hesseberg, K.; Bentzen, H.; Bergland, A. Reliability of the Senior Fitness Test in Community-dwelling Older People with Cognitive Impairment. Physiother. Res. Int. 2014, 20, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Rikli, R.E.; Jones, C.J. Senior Fitness Test Manual; Human Kinetics: Champaign, IL, USA, 2001. [Google Scholar]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Chan, A.C.-M. Clinical Validation of the Geriatric Depression Scale (GDS). J. Aging Health 1996, 8, 238–253. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.-M.; Li, C.-H.; Chang, Y.-H.; Huang, H.-T.; Cheng, Y.-Y. An elastic band exercise program for older adults using wheelchairs in Taiwan nursing homes: A cluster randomized trial. Int. J. Nurs. Stud. 2015, 52, 30–38. [Google Scholar] [CrossRef]
- Hsu, C.-C.; Chen, S.-R.; Lee, P.-H.; Lin, P.-C. The Effect of Music Listening on Pain, Heart Rate Variability, and Range of Motion in Older Adults After Total Knee Replacement. Clin. Nurs. Res. 2019, 28, 529–547. [Google Scholar] [CrossRef]
- Park, Y.S.; Koh, K.; Yang, J.S.; Shim, J.K. Efficacy of rhythmic exercise and walking exercise in older adults’ exercise participation rates and physical function outcomes. Geriatr. Gerontol. Int. 2017, 17, 2311–2318. [Google Scholar] [CrossRef]
- Xu, B.; Sui, Y.; Zhu, C.; Yang, X.; Zhou, J.; Li, L.; Ren, L.; Wang, X. Music intervention on cognitive dysfunction in healthy older adults: A systematic review and meta-analysis. Neurol. Sci. 2017, 38, 983–992. [Google Scholar] [CrossRef]
- Picanço-Diniz, C.W.; De Oliveira, T.C.G.; Soares, F.C.; Macedo, L.D.E.D.D.; Diniz, D.L.W.P.; Bento-Torres, N.V.O. Beneficial effects of multisensory and cognitive stimulation on age-related cognitive decline in long-term-care institutions. Clin. Interv. Aging 2014, 9, 309–320. [Google Scholar] [CrossRef] [Green Version]
- Dev, A.; Smitha, K.; Pillai, R. Music therapy for institutionalised elderly persons with depression. Open J. Psychiatry Allied Sci. 2015, 6, 15–19. [Google Scholar]
- Chu, H.; Yang, C.-Y.; Lin, Y.; Ou, K.-L.; Lee, T.-Y.; O’Brien, A.P.; Chou, K. The Impact of Group Music Therapy on Depression and Cognition in Elderly Persons with Dementia. Biol. Res. Nurs. 2013, 16, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Chan, M.F.; Chan, E.A.; Mok, E. Effects of music on depression and sleep quality in elderly people: A randomised controlled trial. Complement. Ther. Med. 2010, 18, 150–159. [Google Scholar] [CrossRef]
- De Guzman, A.B.; Lagdaan, L.F.M.; Lagoy, M.L.V. The Role of Life-Space, Social Activity, and Depression on the Subjective Memory Complaints of Community-Dwelling Filipino Elderly: A Structural Equation Model. Educ. Gerontol. 2014, 41, 348–360. [Google Scholar] [CrossRef]
- Holtfreter, K.; Reisig, M.D.; Turanovic, J. Depression and infrequent participation in social activities among older adults: The moderating role of high-quality familial ties. Aging Ment. Health 2015, 21, 379–388. [Google Scholar] [CrossRef] [PubMed]
| Variable | Total | Intervention Group (n = 62) | Comparison Group (n = 60) | p Value | ||
|---|---|---|---|---|---|---|
| n | (%) | n | (%) | |||
| Sex | 0.003 | |||||
| Male | 27 | 7 | (11.3) | 20 | (33.3) | |
| Female | 95 | 55 | (88.7) | 40 | (66.7) | |
| Age (years, mean ± SD) | 73.90 ± 6.86 | 74.29 ± 7.53 | 73.50 ± 6.14 | 0.631 | ||
| Education level | 0.168 | |||||
| Illiteracy | 33 | 15 | (24.2) | 8 | (13.3) | |
| Primary school/literate | 49 | 26 | (41.9) | 23 | (38.3) | |
| Junior high school and above | 50 | 21 | (33.9) | 29 | (48.3) | |
| Religious belief | 0.744 | |||||
| Yes | 10 | 6 | (9.7) | 4 | (6.7) | |
| No | 112 | 56 | (90.3) | 56 | (93.3) | |
| Marital relationship | 0.144 | |||||
| Yes | 49 | 29 | (46.8) | 20 | (33.3) | |
| No | 73 | 33 | (53.2) | 40 | (66.7) | |
| Children | 0.356 | |||||
| Yes | 5 | 4 | (6.5) | 1 | (1.7) | |
| No | 117 | 58 | (93.5) | 59 | (98.3) | |
| Living with family and friends | 0.369 | |||||
| Yes | 24 | 14 | (22.6) | 10 | (16.7) | |
| No | 98 | 48 | (77.4) | 50 | (83.3) | |
| Health behavior | 0.234 | |||||
| Yes | 115 | 2 | (3.2) | 5 | (8.2) | |
| No | 7 | 60 | (96.8) | 56 | (91.8) | |
| Number of illnesses (mean ± SD) | 2.87 ± 2.31 | 3.23 ± 2.20 | 2.50 ± 2.52 | 0.092 | ||
| Physical illness | 0.722 | |||||
| Yes | 13 | 6 | (9.7) | 7 | (11.7) | |
| No | 109 | 56 | (90.3) | 53 | (88.3) | |
| Variable | Intervention Group (n = 62) | Comparison Group (n = 60) | t | p Value |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| Kihon Checklist | ||||
| Pre-intervention | 8.08 ± 4.82 | 6.57 ± 3.67 | 1.845 | 0.068 |
| Post-intervention | 5.84 ± 4.15 | 6.65 ± 3.76 | −1.130 | 0.261 |
| Paired t-test (p value) | 8.144 (<0.001) | −1.692 (0.096) | ||
| Total physical fitness score | ||||
| Pre-intervention | 18.37 ± 7.47 | 16.45 ± 4.30 | 1.748 | 0.084 |
| Post-intervention | 21.95 ± 7.26 | 15.93 ± 4.11 | 5.654 | <0.001 |
| Paired t-test (p value) | −7.961 (<0.001) | 4.305 (<0.001) | ||
| BMI | ||||
| Pre-intervention | 23.58 ± 3.51 | 23.82 ± 5.10 | −0.309 | 0.758 |
| Post-intervention | 23.67 ± 3.49 | 23.90 ± 5.09 | −0.291 | 0.772 |
| Paired t-test (p value) | 0.904 (0.369) | 3.113 (0.003) | ||
| MMSE total score | ||||
| Pre-intervention | 26.74 ± 2.45 | 26.88 ± 1.96 | −0.353 | 0.725 |
| Post-intervention | 27.63 ± 2.25 | 26.72 ± 2.07 | 2.331 | 0.021 |
| Paired t-test (p value) | 3.935 (<0.001) | −1.932 (0.058) | ||
| Geriatric depression | ||||
| Pre-intervention | 2.18 ± 2.24 | 2.10 ± 2.30 | 0.188 | 0.851 |
| Post-intervention | 1.55 ± 1.52 | 2.10 ± 2.00 | −1.719 | 0.088 |
| Paired t-test (p value) | −4.608(<0.001) | 0.000 (>0.999) |
| Group (Ref. = Comparison Group) | |||||||
|---|---|---|---|---|---|---|---|
| Pre-Mean | Post-Mean | F | p Value | Effect Size | |||
| Variable | Intervention | Comparison | Intervention | Comparison | |||
| Kihon posttest score | 8.08 | 6.57 | 5.20 | 7.31 | 63.509 | <0.001 | 0.350 |
| Posttest BMI (kg/m2) | 23.58 | 23.82 | 23.78 | 23.78 | 0.000 | 0.997 | <0.001 |
| Posttest total score of physical fitness | 18.37 | 16.45 | 21.21 | 16.70 | 89.260 | <0.001 | 0.431 |
| Physical fitness sub-items | |||||||
| 1 Posttest lower limb muscle endurance (times) | 13.61 | 14.00 | 17.20 | 13.26 | 63.261 | <0.001 | 0.349 |
| 2.Pretest upper limb muscle endurance test (times) | 18.74 | 16.27 | 20.67 | 17.08 | 29.679 | <0.001 | 0.201 |
| 3 Cardiorespiratory endurance (times) | 66.48 | 78.57 | 83.40 | 71.59 | 18.263 | <0.001 | 0.134 |
| 4 Posttest lower limb flexibility-right (cm) | −1.95 | −2.47 | 0.84 | −2.47 | 53.289 | <0.001 | 0.311 |
| 5 Posttest lower limb flexibility-left (cm) | −1.61 | −3.12 | 0.53 | −2.92 | 41.138 | <0.001 | 0.259 |
| 6 Posttest static body balance-right (s) | 11.32 | 16.13 | 18.78 | 13.09 | 16.503 | <0.001 | 0.123 |
| 7. Posttest static body balance-left (s) | 10.36 | 12.41 | 16.32 | 11.53 | 8.148 | 0.005 | 0.065 |
| 8. Posttest upper limb flexibility (cm) | −8.41 | −8.53 | −6.43 | −8.81 | 17.483 | <0.001 | 0.129 |
| 9. Posttest functional mobility (s) | 13.11 | 10.68 | 10.44 | 12.52 | 63.878 | <0.001 | 0.351 |
| MMSE posttest score | 26.74 | 26.88 | 27.72 | 26.63 | 21.029 | <0.001 | 0.151 |
| Geriatric depression posttest score | 2.18 | 1.55 | 1.52 | 2.13 | 23.484 | <0.001 | 0.166 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, F.-C.; Li, H.-C.; Wang, H.-H. The Effect of Group Music Therapy with Physical Activities to Prevent Frailty in Older People Living in the Community. Int. J. Environ. Res. Public Health 2021, 18, 8791. https://doi.org/10.3390/ijerph18168791
Sun F-C, Li H-C, Wang H-H. The Effect of Group Music Therapy with Physical Activities to Prevent Frailty in Older People Living in the Community. International Journal of Environmental Research and Public Health. 2021; 18(16):8791. https://doi.org/10.3390/ijerph18168791
Chicago/Turabian StyleSun, Feng-Ching, Hui-Chi Li, and Hsiu-Hung Wang. 2021. "The Effect of Group Music Therapy with Physical Activities to Prevent Frailty in Older People Living in the Community" International Journal of Environmental Research and Public Health 18, no. 16: 8791. https://doi.org/10.3390/ijerph18168791






