Analysis of Patient Safety Incidents in Primary Care Reported in an Electronic Registry Application
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting
2.3. Reporting System
- -
- Notification: a structured record is generated. There are different forms, which correspond to the type of incident reported.
- -
- Management: encourages proactive incident analysis to detect flaws and improve processes. Tools such as the risk matrix, cause-effect, process and root cause analyses are available for professionals responsible for incident management [29]. For instance, the risk matrix evaluates the risk of an incident based on the probability of occurring and the impact on the patient. These two criteria are represented in a table where each box colour is related to risk severity (green colour indicates low risk, yellow moderate risk, and red high risk). For the cause-effect analysis, we design a fishbone diagram (Ishikawa diagram) describing the problem and the main underlying causes. The root-cause-analysis is a systematic process to determine the underlying factors that have contributed to the occurrence of the incident, particularly the analysis of latent conditions (systems and processes). The end goal is to sensibly respond to the following questions: What happened?; Why did it happen?; Can we prevent it from happening again?
- -
- Analysis and reports: the platform analyses incidents to systematically identify risks and prevent errors.
- -
- Improvement actions: allows planning and monitoring of improvement actions, preventative measures or changes in the organisation.
2.4. Incident Notification Procedure of General Practices and Data Collectors
2.5. Taxonomy and Definitions
2.6. Notification Evaluation Procedure
2.7. Statistical Analysis
3. Results
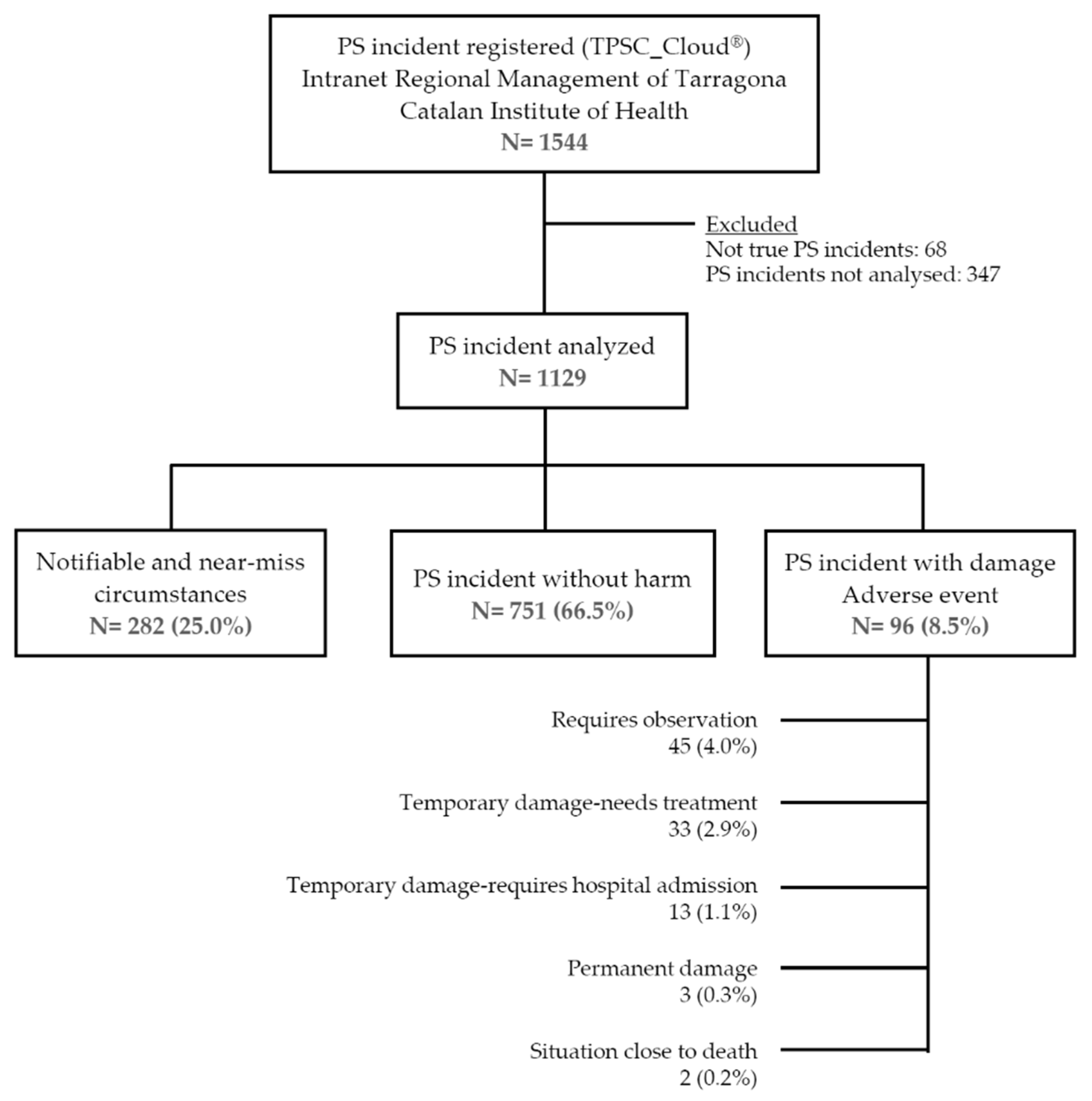
3.1. Report Classification
3.2. Causal and Contributing Factors
3.3. Resolution Level and Proposed Actions
- Creation of multidisciplinary improvement teams to standardise clinical practice. For example, the adequacy of diagnostic tests or pharmacological treatments (such as oral anticoagulant therapy), the implementation of checklists that allow a structured and daily briefing to be carried out in the health centre and each reference laboratory, or the standardization of various administrative processes.
- Continuing professional development yearly. 95% of the professionals in primary care centres have received PS training. This training takes place yearly and consists of a 6-h workshop accredited by the Institut Català de la Salut. Furthermore, all professionals of the Central Patient Safety Functional Unit have been trained in the management of adverse events and in relation to second and third victims. These concepts acknowledge that “harm from PS incidents does not always stop with patients and their families” (considered the first victims of the error), since often it is “the healthcare workers involved in an incident, who can also experience significant harm” (second victims) and, even “those with indirect exposure to an adverse event can become victims (third) of an adverse event” [33]. A webpage is available in Spain with information regarding second victims (http://www.segundasvictimas.es/index.php, accessed on 12 August 2021), and the Department of Health of the Generalitat de Catalunya provides online training accessible by all health organisations (http://seguretatdelspacients.gencat.cat/ca/professionals/formacio/gestio_de_riscos/segones-victimes/, accessed on 12 August 2021).
- Creation of transversal PS units to analyse incidents related to communication between different healthcare services.
- Root-cause analysis of severe adverse events related to diagnostic delay in cancer patients, lack of coordination between different levels of care and control of narcotics in health centres.
- Publication of patient safety bulletins with general and specific content on adverse events, in relation to communication, laboratory and safe use of medication. In reports on health warnings, such as the case of necrotizing fasciitis due to simultaneous intramuscular administration of metamizole and diclofenac.
4. Discussion
4.1. Summary of Main Findings
4.2. Comparison with Existing Literature
4.3. Major Strengths and Limitations of This Study
4.4. Implications for Clinical Practice and Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sheikh, A.; Panesar, S.S.; Larizgoitia, I.; Bates, D.W.; Donaldson, L.J. Safer primary care for all: A global imperative. Lancet Glob. Health 2013, 1, e182–e183. [Google Scholar] [CrossRef] [Green Version]
- World Health Organisation. World Alliance for Patient Safety; The Launch of the World Alliance for Patient Safety: Washington, DC, USA, 27 October 2004; Available online: https://www.who.int/patientsafety/worldalliance/en/ (accessed on 1 July 2021).
- Iglesia, M.; Margetidis, G.; Montante, S.; Azzolini, E.; Ricciardi, W. Moving a step forward to promote patient safety and quality of care in Europe. Epidemiol. Biostat. Public Health 2014, 11, e11034. [Google Scholar] [CrossRef]
- Terol, E.; Agra, Y.; Fernández-Maíllo, M.M.; Casal, J.; Sierra, E.; Bandrés, B.; García, M.J.; del Peso, P. Resultados de la estrategia en seguridad del paciente del Sistema Nacional de Salud español, período 2005–2007. Med. Clin. 2008, 131 (Suppl. 3), 4–11. [Google Scholar] [CrossRef]
- Astier-Peña, M.P.; Torijano-Casalengua, M.L.; Olivera-Cañadas, G.; Patient Safety Group of the Spanish Society of Family and Community Medicine (SEMFYC). Prioridades en seguridad del paciente en Atención Primaria. Atención Primaria 2016, 48, 3–7. [Google Scholar] [CrossRef] [Green Version]
- Pronovost, P.J.; Colantuoni, E. Measuring preventable harm: Helping science keep pace with policy. JAMA 2009, 301, 1273–1275. [Google Scholar] [CrossRef] [PubMed]
- Cooper, J.; Williams, H.; Hibbert, P.; Edwards, A.; Butt, A.; Wood, F.; Parry, G.; Smith, P.; Sheikh, A.; Donaldson, L.; et al. Classification of patient-safety incidents in primary care. Bull. World Health Organ. 2018, 96, 498–505. [Google Scholar] [CrossRef] [PubMed]
- Leape, L.; Berwick, D.; Clancy, C.; Conway, J.; Gluck, P.; Guest, J.; Lawrence, D.; Morath, J.; O’Leary, D.; O’Neill, P.; et al. Transforming healthcare: A safety imperative. Qual. Saf. Health Care 2009, 18, 424–428. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Committee on Quality of Healthcare in America. To Err Is Human: Building a Safer Health System; Kohn, L.T., Corrigan, J.M., Donaldson, M.S., Eds.; National Academies Press: Washington, DC, USA, 2000. [Google Scholar]
- Weaver, S.J.; Lubomksi, L.H.; Wilson, R.F.; Pfoh, E.R.; Martinez, K.A.; Dy, S.M. Promoting a culture of safety as a patient safety strategy: A systematic review. Ann. Intern. Med. 2013, 158, 369–374. [Google Scholar] [CrossRef]
- Vincent, C. Incident reporting and patient safety. BMJ 2007, 334, 51. [Google Scholar] [CrossRef] [Green Version]
- Wilson, T.; Pringle, M.; Sheikh, A. Promoting patient safety in primary care. BMJ 2001, 323, 583–584. [Google Scholar] [CrossRef]
- Madden, C.; Lydon, S.; Curran, C.; Murphy, A.W.; O’Connor, P. Potential value of patient record review to assess and improve patient safety in general practice: A systematic review. Eur. J. Gen. Pract. 2018, 24, 192–201. [Google Scholar] [CrossRef] [Green Version]
- Panagioti, M.; Khan, K.; Keers, R.N.; Abuzour, A.; Phipps, D.; Kontopantelis, E.; Bower, P.; Campbell, S.; Haneef, R.; Avery, A.J.; et al. Prevalence, severity, and nature of preventable patient harm across medical care settings: Systematic review and meta-analysis. BMJ 2019, 366, l4185. [Google Scholar] [CrossRef] [Green Version]
- Verbakel, N.J.; Langelaan, M.; Verheij, T.J.; Wagner, C.; Zwart, D.L. Improving Patient Safety Culture in Primary Care: A Systematic Review. J. Patient Saf. 2016, 12, 152–158. [Google Scholar] [CrossRef] [Green Version]
- World Health Organisation. The Safer Primary Care Expert Working Group. Safer Primary Care: A Global Challenge; World Health Organisation: Geneva, Switzerland, 2012; Available online: http://www.who.int/patientsafety/summary_report_of_primary_care_consultation.pdf (accessed on 1 July 2021).
- Klemp, K.; Dovey, S.; Valderas, J.M.; Rohe, J.; Godycki-Cwirko, M.; Elliott, P.; Beyer, M.; Gerlach, F.M.; Hoffmann, B. Developing a patient safety incident classification system for primary care. A literature review and Delphi-survey by the LINNEAUS collaboration on patient safety in primary care. Eur. J. Gen. Pract. 2015, 21 (Suppl. 1), 35–38. [Google Scholar] [CrossRef] [Green Version]
- Panesar, S.S.; de Silva, D.; Carson-Stevens, A.; Cresswell, K.M.; Salvilla, S.A.; Slight, S.P.; Javad, S.; Netuveli, G.; Larizgoitia, I.; Donaldson, L.J.; et al. How safe is primary care? A systematic review. BMJ Qual. Saf. 2016, 25, 544–553. [Google Scholar] [CrossRef] [Green Version]
- APEAS Study. Patient Safety in Primary Healthcare; Ministry of Health and Consumer Affairs: Madrid, Spain, 2008. Available online: https://www.mscbs.gob.es/organisacion/sns/planCalidadSNS/docs/estudio_apeas.pdf (accessed on 1 July 2021).
- Aranaz-Andrés, J.M.; Aibar, C.; Limón, R.; Mira, J.J.; Vitaller, J.; Agra, Y.; Terol, E. A study of the prevalence of adverse events in primary healthcare in Spain. Eur. J. Public Health 2012, 22, 921–925. [Google Scholar] [CrossRef] [PubMed]
- Lawati, M.H.A.; Dennis, S.; Short, S.D.; Abdulhadi, N.N. Patient safety and safety culture in primary healthcare: A systematic review. BMC Fam. Pract. 2018, 19, 104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ministry of Health Government of Spain. Statistical Portal: Primary Care Information System (SIAP). Available online: https://pestadistico.inteligenciadegestion.mscbs.es/publicoSNS/S/sistema-de-informacion-de-atencion-primaria-siap (accessed on 1 July 2021).
- Catalán, A.; Borrell, F.; Pons, A.; Amado, E.; Baena, J.M.; Morales, V. Seguridad del paciente en atención primaria: Proyecto PREFASEG (PREscripción FArmacológica SEGura). Med. Clin. 2014, 143 (Suppl. 1), 32–35. [Google Scholar] [CrossRef]
- Departament de Salut. Generalitat de Catalunya. Pla de Salut 2016–2020. Available online: https://salutweb.gencat.cat/ca/el_departament/Pla_salut/pla-de-salut-2016-2020/ (accessed on 1 July 2021).
- Davins, J.; Gens, M.; Pareja, C.; Guzmán, R.; Marquet, R.; Vallès, R. El modelo de acreditación de atención primaria de Catalunya: Un modelo válido. Med. Clin. 2014, 143 (Suppl. 1), 74–80. [Google Scholar] [CrossRef] [PubMed]
- Departament de Salut. Generalitat de Catalunya. DECRET 151/2017, de 17 d’Octubre. Diari Oficial de la Generalitat de Catalunya. Núm. 7477—19.10.2017. Available online: https://portaldogc.gencat.cat/utilsEADOP/PDF/7477/1639926.pdf (accessed on 1 July 2021).
- Massanés, M.; Álava, F.; Oliva, G.; Navarro, L.; Jiménez, M.; Esquerra, M.; Davins, J.; Rams, N. Notificació i gestió d’incidents relacionats amb la seguretat dels pacients com a eina per a la millora contínua. Ann. Med. 2017, 100, 18–22. [Google Scholar]
- Departament de Salut. Generalitat de Catalunya. Seguretat dels Pacients. Available online: http://seguretatdelspacients.gencat.cat/ca/detalls/noticia/Actualitat-00350 (accessed on 1 July 2021).
- National Patient Safety Agency. Seven Steps to Patient Safety. NHS. 2004. Available online: https://www.publichealth.hscni.net/sites/default/files/directorates/files/Seven%20steps%20to%20safety.pdf (accessed on 12 August 2021).
- World Health Organisation. World Alliance for Patient Safety. Conceptual Framework for the International Classification of Patient Safety; Final Technical Report; World Health Organisation: Geneva, Switzerland, 2009; Available online: http://www.who.int/patientsafety/taxonomy/icps_full_report.pdf (accessed on 1 July 2021).
- Departament de Salut. Generalitat de Catalunya. Acreditació d’Equips d‘Atenció Primària a Catalunya. Manual d’Estàndards. Available online: https://salutweb.gencat.cat/web/.content/_serveis/Acreditacio-de-centres-sanitaris/Equips-datencio-primaria/estandards_acred_eap.pdf (accessed on 1 July 2021).
- Davins, J.; Gens, M.; García, A.; Álava, F.; Oliva, G.; Lushchenkova, O.; Navarro, L.; Esquerra, M.; Fabré, P.; Constante, C. Desenvolupament de les unitats funcionals de seguretat dels pacients en l’atenció primària de Catalunya. Ann. Med. 2012, 95, 111–114. Available online: https://www.academia.cat/files/499-165-FITXER/roda01.pdf (accessed on 1 July 2021).
- Holden, J.; Card, A.J. Patient safety professionals as the third victims of adverse events. J. Patient Saf. Risk Manag. 2019, 24, 166–175. [Google Scholar] [CrossRef]
- Pham, J.C.; Girard, T.; Pronovost, P.J. What to do with healthcare incident reporting systems. J. Public Health Res. 2013, 2, e27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cresswell, K.M.; Panesar, S.S.; Salvilla, S.A.; Carson-Stevens, A.; Larizgoitia, I.; Donaldson, L.J.; Bates, D.; Sheikh, A.; World Health Organisation’s (WHO) Safer Primary Care Expert Working Group. Global research priorities to better understand the burden of iatrogenic harm in primary care: An international Delphi exercise. PLoS Med. 2013, 10, e1001554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lay-Flurrie, S.; Mathieu, E.; Bankhead, C.; Nicholson, B.D.; Perera-Salazar, R.; Holt, T.; Hobbs, F.D.R.; Salisbury, C.; NIHR School for Primary Care Research, Nuffield Department of Primary Care Health Sciences, University of Oxford. Patient consultation rate and clinical and NHS outcomes: A cross-sectional analysis of English primary care data from 2.7 million patients in 238 practices. BMC Health Serv. Res. 2019, 19, 219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woods, D.M.; Thomas, E.J.; Holl, J.L.; Weiss, K.B.; Brennan, T.A. Ambulatory care adverse events and preventable adverse events leading to a hospital admission. Qual. Saf. Healthc. 2007, 16, 127–131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Astier-Peña, M.P.; Torijano-Casalengua, M.L.; Olivera-Cañadas, G.; Silvestre-Busto, C.; Agra-Varela, Y.; Maderuelo-Fernández, J.Á. Are Spanish primary care professionals aware of patient safety? Eur. J. Public Health 2015, 25, 781–787. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Howell, A.M.; Burns, E.M.; Bouras, G.; Donaldson, L.J.; Athanasiou, T.; Darzi, A. Can Patient Safety Incident Reports Be Used to Compare Hospital Safety? Results from a Quantitative Analysis of the English National Reporting and Learning System Data. PLoS ONE 2015, 10, e0144107. [Google Scholar] [CrossRef]
- Boaz, A.; Hanney, S.; Jones, T.; Soper, B. Does the engagement of clinicians and organisations in research improve healthcare performance: A three-stage review. BMJ Open 2015, 5, e009415. [Google Scholar] [CrossRef] [PubMed]
- O’Beirne, M.; Sterling, P.D.; Zwicker, K.; Hebert, P.; Norton, P.G. Safety incidents in family medicine. BMJ Qual. Saf. 2011, 20, 1005–1010. [Google Scholar] [CrossRef] [PubMed]
- Guerra-García, M.M.; Campos-Rivas, B.; Sanmarful-Schwarz, A.; Vírseda-Sacristán, A.; Dorrego-López, M.A.; Charle-Crespo, Á. Descripción de factores contribuyentes en sucesos adversos relacionados con la seguridad del paciente y su evitabilidad. Atención Primaria 2018, 50, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Pham, J.C.; Gianci, S.; Battles, J.; Beard, P.; Clarke, J.R.; Coates, H.; Donaldson, L.; Eldridge, N.; Fletcher, M.; Goeschel, C.A.; et al. Establishing a global learning community for incident-reporting systems. Qual. Saf. Healthc. 2010, 19, 446–451. [Google Scholar] [CrossRef] [PubMed]
- Chaneliere, M.; Koehler, D.; Morlan, T.; Berra, J.; Colin, C.; Dupie, I.; Michel, P. Factors contributing to patient safety incidents in primary care: A descriptive analysis of patient safety incidents in a French study using CADYA (categorization of errors in primary care). BMC Fam. Pract. 2018, 19, 121. [Google Scholar] [CrossRef] [PubMed]
- Michel, P.; Brami, J.; Chanelière, M.; Kret, M.; Mosnier, A.; Dupie, I.; Haeringer-Cholet, A.; Keriel-Gascou, M.; Maradan, C.; Villebrun, F.; et al. Patient safety incidents are common in primary care: A national prospective active incident reporting survey. PLoS ONE 2017, 12, e0165455. [Google Scholar] [CrossRef] [Green Version]
- Müller, M.; Jürgens, J.; Redaèlli, M.; Klingberg, K.; Hautz, W.E.; Stock, S. Impact of the communication and patient hand-off tool SBAR on patient safety: A systematic review. BMJ Open 2018, 8, e022202. [Google Scholar] [CrossRef] [Green Version]
- Morris, R.L.; Stocks, S.J.; Alam, R.; Taylor, S.; Rolfe, C.; Glover, S.W.; Whitcombe, J.; Campbell, S.M. Identifying primary care patient safety research priorities in the UK: A James Lind Alliance Priority Setting Partnership. BMJ Open 2018, 8, e020870. [Google Scholar] [CrossRef] [Green Version]
- Edwards, L.; Monro, M.; Butterfield, Y.; Johl, R.; Loftsgard, K.C.; Pelletier, H.; McGavin, C.; Lavergne, M.R. What matters most to patients about primary healthcare: Mixed-methods patient priority setting exercises within the PREFeR (PRioritiEs For Research) project. BMJ Open 2019, 9, e025954. [Google Scholar] [CrossRef] [Green Version]
- Kaushal, R.; Kern, L.M.; Barrón, Y.; Quaresimo, J.; Abramson, E.L. Electronic prescribing improves medication safety in community-based office practices. J. Gen. Intern. Med. 2010, 25, 530–536. [Google Scholar] [CrossRef] [Green Version]
- Ammenwerth, E.; Schnell-Inderst, P.; Machan, C.; Siebert, U. The effect of electronic prescribing on medication errors and adverse drug events: A systematic review. J. Am. Med. Inform. Assoc. 2008, 15, 585–600. [Google Scholar] [CrossRef] [Green Version]
- Nanji, K.C.; Rothschild, J.M.; Salzberg, C.; Keohane, C.A.; Zigmont, K.; Devita, J.; Gandhi, T.K.; Dalal, A.K.; Bates, D.W.; Poon, E.G. Errors associated with outpatient computerized prescribing systems. J. Am. Med. Inform. Assoc. 2011, 18, 767–773. [Google Scholar] [CrossRef] [Green Version]
- Doran, D.M.; Baker, G.R.; Szabo, C.; McShane, J.; Carryer, J. Identification of serious and reportable events in home care: A Delphi survey to develop consensus. Int. J. Qual. Healthc. 2014, 26, 136–143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Makeham, M.; Dovey, S.; Runciman, W.; Larizgoitia, I. Methods and Measures Used in Primary Care Patient Safety Research; Results of a Literature Review; World Health Organisation: Geneva, Switzerland, 2008; Available online: https://www.who.int/patientsafety/research/methods_measures/makeham_dovey_full.pdf (accessed on 1 July 2021).
- Lydon, S.; Cupples, M.E.; Murphy, A.W.; Hart, N.; O’Connor, P. A Systematic Review of Measurement Tools for the Proactive Assessment of Patient Safety in General Practice. J. Patient Saf. 2021, 17, e406–e412. [Google Scholar] [CrossRef] [PubMed]
- Ramírez, E.; Martín, A.; Villán, Y.; Lorente, M.; Ojeda, J.; Moro, M.; Vara, C.; Avenza, M.; Domingo, M.J.; Alonso, P.; et al. Effectiveness and limitations of an incident-reporting system analyzed by local clinical safety leaders in a tertiary hospital: Prospective evaluation through real-time observations of patient safety incidents. Medicine 2018, 97, e12509. [Google Scholar] [CrossRef]
- Ferorelli, D.; Solarino, B.; Trotta, S.; Mandarelli, G.; Tattoli, L.; Stefanizzi, P.; Bianchi, F.P.; Tafuri, S.; Zotti, F.; Dell’Erba, A. Incident Reporting System in an Italian University Hospital: A New Tool for Improving Patient Safety. Int. J. Environ. Res. Public Health 2020, 17, 6267. [Google Scholar] [CrossRef] [PubMed]
- Sujan, M.A.; Huang, H.; Braithwaite, J. Learning from incidents in health care: Critique from a Safety-II perspective. Saf. Sci. 2017, 99, 115–121. [Google Scholar] [CrossRef] [Green Version]
- Khalil, H.; Bell, B.; Chambers, H.; Sheikh, A.; Avery, A.J. Professional, estructural and organisational interventions in primary care for reducing medication errors. Cochrane Datebase Syst. Rev. 2017, 10, CD003942. [Google Scholar] [CrossRef] [Green Version]
- Rees, P.; Edwards, A.; Powell, C.; Hibbert, P.; Williams, H.; Makeham, M.; Carter, B.; Luff, D.; Parry, G.; Avery, A.; et al. Patient Safety Incidents Involving Sick Children in Primary Care in England and Wales: A Mixed Methods Analysis. PLoS Med. 2017, 14, e1002217. [Google Scholar] [CrossRef] [PubMed]
- Giles, S.J.; Parveen, S.; Hernan, A.L. Validation of the Primary Care Patient Measure of Safety (PC PMOS) questionnaire. BMJ Qual. Saf. 2019, 28, 389–396. [Google Scholar] [CrossRef]
- Palabindala, V.; Pamarthy, A.; Jonnalagadda, N.R. Adoption of electronic health records and barriers. J. Community Hosp. Intern. Med. Perspect. 2016, 6, 32643. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gaal, S.; Verstappen, W.; Wensing, M. What do primary care physicians and researchers consider the most important patient safety improvement strategies? BMC Health Serv. Res. 2011, 11, 102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kirkman, M.A.; Sevdalis, N.; Arora, S.; Baker, P.; Vincent, C.; Ahmed, M. The outcomes of recent patient safety education interventions for trainee physicians and medical students: A systematic review. BMJ Open 2015, 5, e007705. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarkar, U. Tip of the iceberg: Patient safety incidents in primary care. BMJ Qual. Saf. 2016, 25, 477–479. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsang, C.; Bottle, A.; Majeed, A.; Aylin, P. Adverse events recorded in English primary care: Observational study using the General Practice Research Database. Br. J. Gen. Pract. 2013, 63, e534–e542. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Total PS Incidents | PS Incident Not Reach the Patient | PS Incident without Harm | Adverse Event | |
|---|---|---|---|---|
| Incidents notified | 1129 (100.0) | 282 (25.0) | 751 (66.5) | 96 (8.5) |
| Severity of incident and clinical repercussions * | ||||
| Circumstance that might cause error | 103 (9.1) | 95 (33.7) | 8 (7.8) | |
| Error has occurred but has been detected before reaching the patient | 193 (17.1) | 177 (62.8) | 16 (8.3) | |
| Error has occurred without causing harm | 733 (64.9) | 7 (2.5) | 726 (99.0) | |
| Observation required; no harm caused | 49 (4.3) | 3 (1.1) | 1 (2.0) | 45 (46.9) |
| Treatment required and/or temporary harm | 33 (2.9) | 33 (34.4) | ||
| Temporary damage has been caused that has required or lengthened hospitalization | 13 (1.2) | 13 (13.5) | ||
| Permanent damage has occurred | 3 (0.3) | 3 (3.1) | ||
| A near-death situation has occurred | 2 (0.2) | 2 (2.1) | ||
| PROBABILITY | ||||||
|---|---|---|---|---|---|---|
| Very Rare | Uncommon | Possible | Probable | Frequent | ||
| IMPACT/SEVERITY | Does not reach patient: notifiable circumstances | 6 (0.5) | 11 (1) | 24 (2.1) | 20 (1.8) | 41 (3.6) |
| Does not reach patient: near-miss circumstances | 17 (1.5) | 24 (2.1) | 44 (3.9) | 47 (4.2) | 59 (5.2) | |
| Minimal | 33 (2.9) | 79 (7) | 140 (12.4) | 170 (15.1) | 297 (26.3) | |
| Minor | 3 (0.3) | 3 (0.3) | 16 (1.4) | 7 (0.6) | 19 (1.7) | |
| Moderate 1 | 2 (0.2) | 4 (0.4) | 9 (0.8) | 11 (1) | 4 (0.4) | |
| Moderate 2 | 2 (0.2) | 2 (0.2) | 4 (0.4) | 4 (0.4) | 1 (0.1) | |
| Critical 1 | 2 (0.2) | 1 (0.1) | ||||
| Critical 2 | 1 (0.1) | 1 (0.1) | ||||
| Total PS Incidents | PS Incident Not Reach the Patient | PS Incident without Harm | Adverse Event | |
|---|---|---|---|---|
| Incidents notified | 1129 (100.0) | 282 (25.0) | 751 (66.5) | 96 (8.5) |
| Type of incident notified (related to) categorised according to the Department of Health model * | ||||
| Administrative processes | 259 (22.9) | 48 (17.0) | 201 (26.8) | 10 (10.4) |
| Lab | 244 (21.6) | 53 (18.8) | 183 (24.4) | 8 (8.3) |
| Safe use of medicines | 184 (16.3) | 62 (22.0) | 104 (13.8) | 18 (18.8) |
| Continuity of care | 77 (6.8) | 9 (3.2) | 55 (7.3) | 13 (13.5) |
| General services | 69 (6.1) | 27 (9.6) | 41(5.5) | 1 (1.0) |
| Diagnostic imaging | 60 (5.3) | 6 (2.1) | 38 (5.1) | 16 (16.7) |
| Healthcare process | 60 (5.3) | 13 (4.6) | 40 (5.3) | 7 (7.3) |
| Emergency care | 50 (4.4) | 7 (2.5) | 18 (2.4) | |
| Vaccines | 46 (4.1) | 24 (8.5) | 22 (2.9) | |
| Management of clinical material | 22 (1.9) | 14 (5.0) | 8 (1.1) | |
| Ethics and rights of citizens | 17 (1.5) | 2 (0.7) | 14 (1.9) | 1 (1.0) |
| Infection surveillance, prevention and control | 3 (0.3) | 1 (0.1) | 2 (2.1) | |
| Waste management | 2 (0.2) | 2 (0.3) | ||
| Health education | 1 (0.1) | 1 (0.1) | ||
| Total PS Incidents | PS Incident Not Reach the Patient | PS Incident without Harm | Adverse Event | |
|---|---|---|---|---|
| Incidents notified | 1129 (100.0) | 282 (25.0) | 751 (66.5) | 96 (8.5) |
| Resolution level * | ||||
| Health Centre | 528 (46.8) | 166 (58.9) | 320 (42.6) | 42 (43.8) |
| Patient Safety Functional Unit | 211 (18.7) | 20 (7.1) | 156 (20.8) | 35 (36.5) |
| Primary Care Management | 312 (27.6) | 62 (22.0) | 236 (31.4) | 14 (14.6) |
| Other (ICS, CatSalut.…) | 78 (6.9) | 34 (12.1) | 39 (5.2) | 5 (5.2) |
| Total PS Incidents | PS Incident Not Reach the Patient | PS Incident without Harm | Adverse Event | |
|---|---|---|---|---|
| Incidents notified | 1129 (100.0) | 282 (25.0) | 751 (66.5) | 96 (8.5) |
| Improvement actions in the same health centre * (n = 604; 53.5%) | ||||
| Committee/management | 218 (19.3) | 49 (17.4) | 142 (18.9) | 27 (28.1) |
| Training | 204 (18.1) | 58 (20.6) | 197 (26.2) | 36 (37.5) |
| Report review | 166 (12.6) | 63 (22.3) | 127 (16.9) | 14 (14.6) |
| Improvement team | 16 (1.4) | 2 (0.7) | 14 (1.9) | |
| Improvement actions in the Patient Safety Functional Unit * (n = 525; 46.5%) | ||||
| Committee/management | 93 (8.2) | 21 (7.4) | 48 (6.4) | 24 (25.0) |
| Improvement team | 21 (1.9) | 16 (2.1) | 15 (15.6) | |
| Report review | 6 (0.5) | 6 (0.8) | ||
| Warning | 1 (0.1) | 1 (1.0) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gens-Barberà, M.; Hernández-Vidal, N.; Vidal-Esteve, E.; Mengíbar-García, Y.; Hospital-Guardiola, I.; Oya-Girona, E.M.; Bejarano-Romero, F.; Castro-Muniain, C.; Satué-Gracia, E.M.; Rey-Reñones, C.; et al. Analysis of Patient Safety Incidents in Primary Care Reported in an Electronic Registry Application. Int. J. Environ. Res. Public Health 2021, 18, 8941. https://doi.org/10.3390/ijerph18178941
Gens-Barberà M, Hernández-Vidal N, Vidal-Esteve E, Mengíbar-García Y, Hospital-Guardiola I, Oya-Girona EM, Bejarano-Romero F, Castro-Muniain C, Satué-Gracia EM, Rey-Reñones C, et al. Analysis of Patient Safety Incidents in Primary Care Reported in an Electronic Registry Application. International Journal of Environmental Research and Public Health. 2021; 18(17):8941. https://doi.org/10.3390/ijerph18178941
Chicago/Turabian StyleGens-Barberà, Montserrat, Núria Hernández-Vidal, Elisa Vidal-Esteve, Yolanda Mengíbar-García, Immaculada Hospital-Guardiola, Eva M. Oya-Girona, Ferran Bejarano-Romero, Carles Castro-Muniain, Eva M. Satué-Gracia, Cristina Rey-Reñones, and et al. 2021. "Analysis of Patient Safety Incidents in Primary Care Reported in an Electronic Registry Application" International Journal of Environmental Research and Public Health 18, no. 17: 8941. https://doi.org/10.3390/ijerph18178941
APA StyleGens-Barberà, M., Hernández-Vidal, N., Vidal-Esteve, E., Mengíbar-García, Y., Hospital-Guardiola, I., Oya-Girona, E. M., Bejarano-Romero, F., Castro-Muniain, C., Satué-Gracia, E. M., Rey-Reñones, C., & Martín-Luján, F. M. (2021). Analysis of Patient Safety Incidents in Primary Care Reported in an Electronic Registry Application. International Journal of Environmental Research and Public Health, 18(17), 8941. https://doi.org/10.3390/ijerph18178941






