Big Data for Biomedical Education with a Focus on the COVID-19 Era: An Integrative Review of the Literature
Abstract
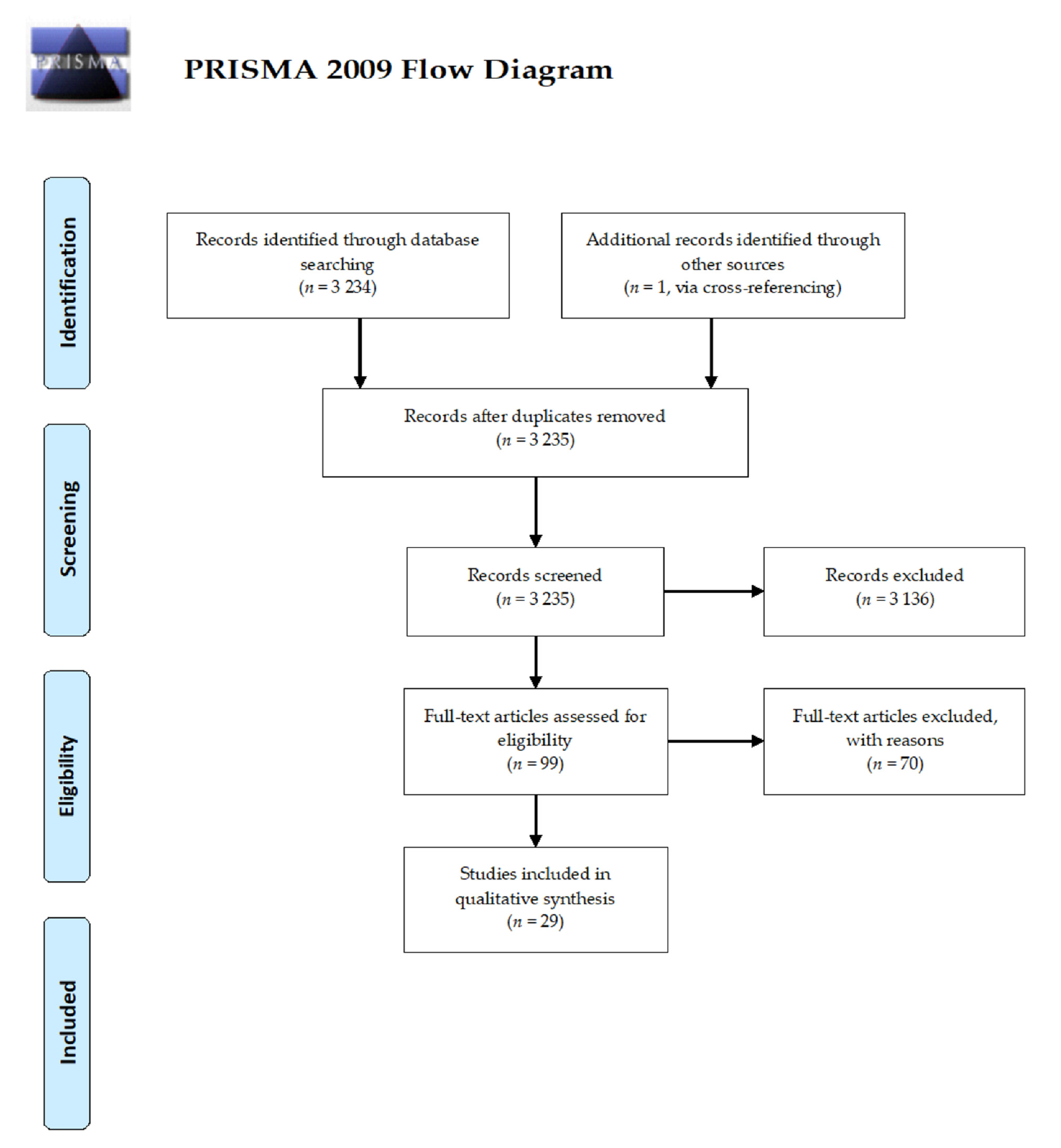
:1. Medical Education: An Overview of Its History and Evolution
2. Material and Methods
3. Results
3.1. Knowledge and Awareness of Big Data among Medical Students
3.2. Integrating and Implementing Big Data Teaching into the Medical Syllabus: Difficulties and Challenges
3.3. Exploiting Big Data to Review, Improve, and Enhance Medical School Curriculum
3.4. Exploiting Big Data to Monitor the Effectiveness of Web-Based Learning Environments among Medical Students
3.5. Exploiting Big Data to Capture the Determinants and Signatures of Successful Academic Performance and Counteract/Prevent Drop-Out
3.6. Exploiting Big Data to Promote Equity, Inclusion, and Diversity
3.7. Exploiting Big Data to Enhance Integrity and Ethics, Avoiding Plagiarism and Duplication Rate
3.8. Empowering Medical Students, Improving and Enhancing Medical Practice
3.9. Exploiting Big Data in Continuous Medical Education and Learning
4. Discussion
5. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Scheele, F. The art of medical education. Facts Views Vis. Obgyn. 2012, 4, 266–269. [Google Scholar]
- Sheikh, A.Y.; Fann, J.I. Artificial Intelligence: Can Information be Transformed into Intelligence in Surgical Education? Thorac. Surg. Clin. 2019, 29, 339–350. [Google Scholar] [CrossRef]
- Ramkumar, P.N.; Kunze, K.N.; Haeberle, H.S.; Karnuta, J.M.; Luu, B.C.; Nwachukwu, B.U.; Williams, R.J. Clinical and Research Medical Applications of Artificial Intelligence. Arthroscopy 2021, 37, 1694–1697. [Google Scholar] [CrossRef]
- Chan, K.S.; Zary, N. Applications and Challenges of Implementing Artificial Intelligence in Medical Education: Integrative Review. JMIR Med. Educ. 2019, 5, e13930. [Google Scholar] [CrossRef] [Green Version]
- Wolff, J.; Pauling, J.; Keck, A.; Baumbach, J. The Economic Impact of Artificial Intelligence in Health Care: Systematic Review. J. Med. Internet Res. 2020, 22, e16866. [Google Scholar] [CrossRef] [PubMed]
- Holmes, W.; Porayska-Pomsta, K.; Holstein, K.; Sutherland, E.; Baker, T.; Buckingham Shum, S.; Santos, O.C.; Rodrigo, M.T.; Cukurova, M.; Bittencourt, I.I.; et al. Ethics of AI in education: Towards a community-wide framework. Int. J. Artif. Intell. Educ. 2021, 1–23. [Google Scholar] [CrossRef]
- Keegan, D. Foundations of Distance Education, 3rd ed.; Routledge: London, UK, 1996; Volume 224. [Google Scholar]
- Schneider, S.P.; Germann, C.G. Technical Communication on the Web: A Profile of Learners and Learning Environments. J. Tech. Writ. Commun. 1999, 8, 37–48. [Google Scholar] [CrossRef]
- Kapp, K.M. The Gamification of Learning and Instruction: Game-Based Methods and Strategies for Training and Education; John Wiley & Sons: Hoboken, NJ, USA, 2012; p. 336. [Google Scholar]
- Lodge, J.M.; Kennedy, G.; Lockyer, L. Digital learning environments, the science of learning and the relationship between the teacher and the learner. In Learning Under the Lens; Routledge: London, UK, 2020; Volume 15. [Google Scholar]
- Dini, G.; Bragazzi, N.L.; Montecucco, A.; Toletone, A.; Debarbieri, N.; Durando, P. Big data in occupational medicine: The convergence of -omics sciences, participatory research and e-health. Med. Lav. 2019, 110, 102–114. [Google Scholar] [CrossRef] [PubMed]
- Khamisy-Farah, R.; Furstenau, L.B.; Kong, J.D.; Wu, J.; Bragazzi, N.L. Gynecology Meets Big data in the Disruptive Innovation Medical Era: State-of-Art and Future Prospects. Int. J. Environ. Res. Public Health 2021, 18, 5058. [Google Scholar] [CrossRef]
- Costa, F.F. Big data in biomedicine. Drug Discov. Today 2014, 19, 433–440. [Google Scholar] [CrossRef]
- López-Belmonte, J.; Pozo-Sánchez, S.; Fuentes-Cabrera, A.; Trujillo-Torres, J.M. Analytical competences of teachers in Big data in the era of digitalized learning. Educ. Sci. 2019, 9, 177. [Google Scholar] [CrossRef] [Green Version]
- Macfadyen, L.P.; Dawson, S.; Pardo, A.; Gaševic, D. Embracing big data in complex educational systems: The learning analytics imperative and the policy challenge. Res. Pract. Assess. 2014, 9, 17–28. [Google Scholar]
- Ferrel, M.N.; Ryan, J.J. The Impact of COVID-19 on Medical Education. Cureus 2020, 12, e7492. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stage, H.B.; Shingleton, J.; Ghosh, S.; Scarabel, F.; Pellis, L.; Finnie, T. Shut and re-open: The role of schools in the spread of COVID-19 in Europe. Philos. Trans. R Soc. Lond. B Biol. Sci. 2021, 376, 20200277. [Google Scholar] [CrossRef]
- Samnani, S.S.; Vaska, M.; Ahmed, S.; Turin, T.C. Review Typology: The Basic Types of Reviews for Synthesizing Evidence for the Purpose of Knowledge Translation. J. Coll. Physicians Surg. Pak. 2017, 27, 635–641. [Google Scholar]
- Russell, C.L. An overview of the integrative research review. Prog. Transplant. 2005, 15, 8–13. [Google Scholar] [CrossRef]
- Sandelowski, M. Qualitative analysis: What it is and how to begin. Res. Nurs. Health 1995, 18, 371–375. [Google Scholar] [CrossRef]
- Casà, C.; Marotta, C.; Di Pumpo, M.; Cozzolino, A.; D’Aviero, A.; Frisicale, E.M.; Silenzi, A.; Gabbrielli, F.; Bertinato, L.; Brusaferro, S. COVID-19 and digital competencies among young physicians: Are we (really) ready for the new era? A national survey of the Italian Young Medical Doctors Association. Ann. Ist. Super Sanita. 2021, 57, 1–6. [Google Scholar] [CrossRef]
- Chow-White, P.; Ha, D.; Laskin, J. Knowledge, attitudes, and values among physicians working with clinical genomics: A survey of medical oncologists. Hum. Resour. Health 2017, 15, 42. [Google Scholar] [CrossRef]
- Hoy, R.R. Quantitative skills in undergraduate neuroscience education in the age of big data. Neurosci. Lett. 2021, 17, 136074. [Google Scholar] [CrossRef]
- Capdarest-Arest, N.; Navarro, C.E. Promoting Health Data Fluency Skills by Expanding Data and Informatics Work in Libraries: The Role of a Health Library Informaticist. Med. Ref. Serv. Q. 2021, 40, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Robeva, R.S.; Jungck, J.R.; Gross, L.J. Changing the Nature of Quantitative Biology Education: Data Science as a Driver. Bull Math Biol. 2020, 82, 127. [Google Scholar] [CrossRef]
- Zanca, F.; Hernandez-Giron, I.; Avanzo, M.; Guidi, G.; Crijns, W.; Diaz, O.; Kagadis, G.C.; Rampado, O.; Lønne, P.I.; Ken, S.; et al. Expanding the medical physicist curricular and professional programme to include Artificial Intelligence. Phys. Med. 2021, 83, 174–183. [Google Scholar] [CrossRef] [PubMed]
- Hameed, B.M.Z.; SDhavileswarapu, A.V.L.; Naik, N.; Karimi, H.; Hegde, P.; Rai, B.P.; Somani, B.K. Big data Analytics in urology: The story so far and the road ahead. Adv. Urol. 2021, 13, 1756287221998134. [Google Scholar] [CrossRef]
- Chen, P.H.; Loehfelm, T.W.; Kamer, A.P.; Lemmon, A.B.; Cook, T.S.; Kohli, M.D. Toward Data-Driven Radiology Education-Early Experience Building Multi-Institutional Academic Trainee Interpretation Log Database (MATILDA). J. Digit. Imaging 2016, 29, 638–644. [Google Scholar] [CrossRef] [Green Version]
- de la Vega, J.S.F. Anatomical pathology (human structural biopathology) in the era of “Big data”, digitalization, 5G and artificial intelligence: Evolution or Revolution? Rev. Esp. Patol. 2020, 53, 226–231. [Google Scholar] [CrossRef]
- Vaitsis, C.; Nilsson, G.; Zary, N. Visual analytics in healthcare education: Exploring novel ways to analyze and represent big data in undergraduate medical education. PeerJ 2014, 2, e683. [Google Scholar] [CrossRef] [Green Version]
- Vaitsis, C.; Nilsson, G.; Zary, N. Big data in medical informatics: Improving education through visual analytics. Stud. Health Technol. Inform. 2014, 205, 1163–1167. [Google Scholar] [PubMed]
- Fritze, O.; Lammerding-Koeppel, M.; Boeker, M.; Narciss, E.; Wosnik, A.; Zipfel, S.; Griewatz, J. Boosting competence-orientation in undergraduate medical education - A web-based tool linking curricular mapping and visual analytics. Med. Teach. 2019, 41, 422–432. [Google Scholar] [CrossRef]
- Menon, A.; Gaglani, S.; Haynes, M.R.; Tackett, S. Using “big data” to guide implementation of a web and mobile adaptive learning platform for medical students. Med. Teach. 2017, 39, 975–980. [Google Scholar] [CrossRef]
- Luo, H.; Wu, C.; He, Q.; Wang, S.Y.; Ma, X.Q.; Wang, R.; Li, B.; He, J. Research on cultivating medical students’ self-learning ability using teaching system integrated with learning analysis technology. Int. J. Clin. Exp. Med. 2015, 8, 14542–14552. [Google Scholar]
- Baron, T.; Grossman, R.I.; Abramson, S.B.; Pusic, M.V.; Rivera, R.; Triola, M.M.; Yanai, I. Signatures of medical student applicants and academic success. PLoS ONE 2020, 15, e0227108. [Google Scholar] [CrossRef]
- Bientzle, M.; Hircin, E.; Kimmerle, J.; Knipfer, C.; Smeets, R.; Gaudin, R.; Holtz, P. Association of Online Learning Behavior and Learning Outcomes for Medical Students: Large-Scale Usage Data Analysis. JMIR. Med. Educ. 2019, 5, e13529. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Argueza, B.R.; Saenz, S.R.; McBride, D. From Diversity and Inclusion to Antiracism in Medical Training Institutions. Acad. Med. 2021, 96, 798–801. [Google Scholar] [CrossRef]
- Levin, J.M.; Oprea, T.I.; Davidovich, S.; Clozel, T.; Overington, J.P.; Vanhaelen, Q.; Cantor, C.R.; Bischof, E.; Zhavoronkov, A. Artificial intelligence, drug repurposing and peer review. Nat. Biotechnol. 2020, 38, 1127–1131. [Google Scholar] [CrossRef]
- Madhavanprabhakaran, G.; Francis, F.; John, S.E.; Al Rawajfah, O. COVID-19 pandemic and remote teaching: Transition and transformation in nursing education. Int. J. Nurs. Educ. Scholarsh. 2021, 18, 18. [Google Scholar] [CrossRef] [PubMed]
- Zikos, D.; Ragina, N.; Strong, O. Enhancing Medical Education with Data-Driven Software: The TrainCoMorb App. Stud. Health Technol. Inform. 2020, 272, 83–86. [Google Scholar] [CrossRef] [PubMed]
- Sanges, S.; Farhat, M.M.; Assaraf, M.; Galland, J.; Rivière, E.; Roubille, C.; Lambert, M.; Yelnik, C.; Maillard, H.; Sobanski, V.; et al. Raising rare disease awareness using red flags, role play simulation and patient educators: Results of a novel educational workshop on Raynaud phenomenon and systemic sclerosis. Orphanet. J. Rare. Dis. 2020, 15, 159. [Google Scholar] [CrossRef] [PubMed]
- Tsopra, R.; Courtine, M.; Sedki, K.; Eap, D.; Cabal, M.; Cohen, S.; Bouchaud, O.; Mechaï, F.; Lamy, J.B. AntibioGame®: A serious game for teaching medical students about antibiotic use. Int. J. Med. Inform. 2020, 136, 104074. [Google Scholar] [CrossRef]
- Kang, S.K.; Rawson, J.V.; Recht, M.P. Supporting Imagers’ VOICE: A National Training Program in Comparative Effectiveness Research and Big data Analytics. J. Am. Coll. Radiol. 2018, 15, 1451–1454. [Google Scholar] [CrossRef]
- Triola, M.M.; Pusic, M.V. The education data warehouse: A transformative tool for health education research. J. Grad. Med. Educ. 2012, 4, 113–115. [Google Scholar] [CrossRef] [Green Version]
- Cobb, A.N.; Eguia, E.; Janjua, H.; Kuo, P.C. Put Me in the Game Coach! Resident Participation in High-risk Surgery in the Era of Big data. J. Surg. Res. 2018, 232, 308–317. [Google Scholar] [CrossRef]
- Rajkomar, A.; Ranji, S.R.; Sharpe, B. Using the Electronic Health Record to Identify Educational Gaps for Internal Medicine Interns. J. Grad. Med. Educ. 2017, 9, 109–112. [Google Scholar] [CrossRef] [Green Version]
- Chahine, S.; Kulasegaram, K.M.; Wright, S.; Monteiro, S.; Grierson, L.E.M.; Barber, C.; Sebok-Syer, S.S.; McConnell, M.; Yen, W.; De Champlain, A.; et al. A Call to Investigate the Relationship Between Education and Health Outcomes Using Big data. Acad. Med. 2018, 93, 829–832. [Google Scholar] [CrossRef] [PubMed]
- Feldman, K.; Chawla, N.V. Does Medical School Training Relate to Practice? Evidence from Big data. Big Data 2015, 3, 103–113. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Au-Yong-Oliveira, M.; Pesqueira, A.; Sousa, M.J.; Dal Mas, F.; Soliman, M. The Potential of Big data Research in HealthCare for Medical Doctors’ Learning. J. Med. Syst. 2021, 45, 13. [Google Scholar] [CrossRef] [PubMed]
- Gorman, D.; Kashner, T.M. Medical Graduates, Truthful and Useful Analytics With Big data, and the Art of Persuasion. Acad. Med. 2018, 93, 1113–1116. [Google Scholar] [CrossRef] [PubMed]
- Arora, V.M. Harnessing the Power of Big data to Improve Graduate Medical Education: Big Idea or Bust? Acad. Med. 2018, 93, 833–834. [Google Scholar] [CrossRef]
- Huynh, T.L.D. Does culture matter social distancing under the COVID-19 pandemic? Saf. Sci. 2020, 130, 104872. [Google Scholar] [CrossRef]
- Xie, K.; Liang, B.; Dulebenets, M.A.; Mei, Y. The Impact of Risk Perception on Social Distancing during the COVID-19 Pandemic in China. Int. J. Environ. Res. Public Health 2020, 17, 6256. [Google Scholar] [CrossRef]
- Jaja, I.F.; Anyanwu, M.U.; Iwu Jaja, C.-J. Social distancing: How religion, culture and burial ceremony undermine the effort to curb COVID-19 in South Africa. Emerg. Microbes. Infect. 2020, 9, 1077–1079. [Google Scholar] [CrossRef] [PubMed]
- Khorram-Manesh, A.; Dulebenets, M.A.; Goniewicz, K. Implementing Public Health Strategies—The Need for Educational Initiatives: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 5888. [Google Scholar] [CrossRef] [PubMed]
- Marchiori, M. COVID-19 and the social distancing paradox: Dangers and solutions. arXiv 2020, arXiv:2005.12446v1. [Google Scholar]
- Wartman, S.A.; Combs, C.D. Reimagining Medical Education in the Age of AI. AMA J. Ethics. 2019, 21, E146–E152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scott, P.; Dunscombe, R.; Evans, D.; Mukherjee, M.; Wyatt, J. Learning health systems need to bridge the ‘two cultures’ of clinical informatics and data science. J. Innov. Health Inform. 2018, 25, 126–131. [Google Scholar] [CrossRef] [Green Version]
- Mylopoulos, M.; Steenhof, N.; Kaushal, A.; Woods, N.N. Twelve tips for designing curricula that support the development of adaptive expertise. Med. Teach. 2018, 40, 850–854. [Google Scholar] [CrossRef] [PubMed]
- Payne, P.R.O.; Bernstam, E.V.; Starren, J.B. Biomedical informatics meets data science: Current state and future directions for interaction. JAMIA Open 2018, 1, 136–141. [Google Scholar] [CrossRef] [PubMed]
- Altman, R.B. Challenges for Training Translational Researchers in the Era of Ubiquitous Data. Clin. Pharmacol. Ther. 2018, 103, 171–173. [Google Scholar] [CrossRef]
- Caliebe, A.; Leverkus, F.; Antes, G.; Krawczak, M. Does big data require a methodological change in medical research? BMC Med. Res. Methodol. 2019, 19, 125. [Google Scholar] [CrossRef]
- Car, J.; Sheikh, A.; Wicks, P.; Williams, M.S. Beyond the hype of big data and artificial intelligence: Building foundations for knowledge and wisdom. BMC Med. 2019, 17, 143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tekian, A.; Watling, C.J.; Roberts, T.E.; Steinert, Y.; Norcini, J. Qualitative and quantitative feedback in the context of competency-based education. Med. Teach. 2017, 39, 1245–1249. [Google Scholar] [CrossRef] [PubMed]
- Saqr, M.; Tedre, M. Should we teach computational thinking and big data principles to medical students? Int. J. Health Sci. 2019, 13, 1–2. [Google Scholar]
| Reference | Year | Study Design | Country | Main Findings | Main Topic | Sub-Topic |
|---|---|---|---|---|---|---|
| Casà et al. [21] | 2021 | Web-delivered, questionnaire-based study, with 362 subjects (young medical doctors) | Italy | Only 6–22% out of 362 participants had knowledge of big data. Replies to the survey enabled to profile three types of medical doctor: namely, high-tech, low-tech, and no-tech | Big data and medical curricula | Knowledge and awareness of big data among medical students |
| Chow-White et al. [22] | 2017 | Survey-based study, with 31 participants (medical oncologists, 52.5% response rate) | British Columbia, Canada | Knowledge was moderate. Participants perceived and anticipated that big data are likely to have a great impact on medical education and practice in the future | ||
| Hoy [23] | 2021 | Commentary | Not applicable | Advanced statistical courses (data analysis/data science) should be offered, as well as homegrown bootcamps and workshops, taking advantage of open-source and freely available online materials (such as YouTube tutorials) | Integrating and implementing big data teaching into the medical syllabus: difficulties and challenges | |
| Capdarest-Arest and Navarro [24] | 2021 | Case study | Blaisdell Medical Library, University of California, Davis/Sacramento, California, USA | There is a need for data-related training in biomedical education. Health science libraries can help develop and implement integrated syllabuses | ||
| Robeva et al. [25] | 2021 | Commentary/theoretical article/perspective article | Not applicable | Open curricula and syllabuses integrating modeling methods, experimental, and computational approaches through engaging, problem-oriented, and hands-on projects, fully exploiting the pedagogy of “experiential teaching” and “experiential learning”. Utilizing big data in medical education implies a major paradigm shift | ||
| Zanca et al. [26] | 2021 | Case study | Several European countries (Belgium, the Netherlands, Italy, Spain, France, Ireland, Greece, Switzerland, Germany, Finland, Norway) | Authors devised an ad hoc curriculum for medical physicists (medical imaging and radiation therapy) incorporating big data and artificial intelligence components and utilizing a knowledge, skills, and competences (KSC) approach | ||
| Hameed et al. [27] | 2021 | Literature review | Not applicable | Big data can enrich and enhance curricula of residents in urology and related sub-specialties (urologic oncology, renal transplant, urolithiasis, reproductive urology, pediatric urology, and endourology) | ||
| Chen et al. [28] | 2016 | Case study | USA | MATILDA is an important example of a big data-based initiative among radiology residents from three American diagnostic radiology residency programs (one in the South, one in the Midwest, and a third in the Northeast of the USA) | ||
| Sánchez Fernández de la Vega [29] | 2020 | Conceptual paper | Not applicable | A proposal of an updated system of the Organization of Scientific Biomedical Knowledge | ||
| Vaitsis et al. [30,31] | 2014 | Visual analytics-based study | Not applicable | Authors identified three approaches of educational data visualization and representation and five competencies at undergraduate medical program level addressed in courses | Exploiting big data to review, improve and enhance medical school curriculum | |
| Fritze et al. [32] | 2019 | Design-based, multicenter study | Germany | Authors devised and implemented a web-based interactive platform for medical curriculum mapping, diagnostics, and development (MERlin database) | ||
| Menon et al. [33] | 2017 | Educational data mining-based study, with a sample of 6787 medical students | USA | Authors used a big data-based approach to investigate the determinants of the use of an adaptive learning platform called Osmosis | Big data and medical academic performance | Exploiting big data to monitor the effectiveness of web-based learning environments among medical students |
| Luo et al. [34] | 2015 | Technical paper (software/platform development and effectiveness case-control study, recruiting a sample of 116 medical students) | The Second Military Medical University Shanghai, Shanghai, China | Authors found that big data can provide strategic information and facilitate decision-making in improving medical students’ self-learning skills | ||
| Baron et al. [35] | 2020 | Database-based study, with a sample of 1088 medical students | New York University Grossman School of Medicine, New York, NY, USA | Authors utilized “academic big data” (standardized tests and undergraduate grade point average or uGPA) to identify various paths to academic success, via an optimized logistic regression model. Authors identified four different paths/trajectories to success | Exploiting big data to capture the determinants and signatures of successful academic performance and counteract/prevent drop-out | |
| Bientzle et al. [36] | 2019 | Database-based study, with a sample of 23,633 students | Germany | Authors exploited big data to link between use of an online platform (Amboss) providing learning materials for preparation for medical exams and performance outcomes | ||
| Argueza et al. [37] | 2021 | Commentary/theoretical article/perspective article | Not applicable | Authors provided recommendations, including use of big data, to make contemporary society more inclusive and less racist | Big data and societal/bioethical issues in biomedical education | Exploiting big data to promote equity, inclusion, and diversity |
| Levin et al. [38] | 2020 | Commentary | Not applicable | Authors showed how to exploit big data to counteract ethical breaches, avoid plagiarism and preserve research integrity in the field of medical education and research | Exploiting big data to enhance integrity and ethics, avoiding plagiarism and duplication rate | |
| Madhavanprabhakaran et al. [39] | 2021 | Commentary | Not applicable | Authors showed the difficulties and barriers to the implementation of remote teaching in the field of nursing education and how COVID-19 acted as a catalyst for innovation | ||
| Zikos et al. [40] | 2020 | Technical paper (software development) | Not applicable | Authors described the development of TrainCoMorb, an online, data-driven (claims database-based) application specifically devised for medical students and residents. The application can help students recognize comorbidities and understand their prognostic outcome by means of a dynamic Bayesian algorithm | Big data and medical career | Empowering medical students, improving and enhancing medical practice |
| Sange et al. [41] | 2020 | Case-study | France | Authors showed how big data can be utilized to raise awareness of rare symptoms/diseases, via two simulated consultations Participants felt very satisfied with the training and more comfortable about diagnosing and managing rare symptoms/diseases. Big data, role-playing, simulations, “immersive learning” and involvement of patient educators, together with other innovative, emerging educational tools, can play a significant role in medical education | ||
| Tsopra et al. [42] | 2020 | Questionnaire-based study, administered to 57 medical students | France | AntibioGame® is a case-based serious game, which enables medical students to simulate various real-life primary care scenarios. It was deemed good and quite satisfactory in terms of usability and playability | ||
| Kang et al. [43] | 2018 | Case-study | USA | Authors described the development of the Value of Imaging Through Comparative Effectiveness (VOICE) Research Program, which provides medical residents from radiology and cardiology with practical, hands-on training in five areas, including big data principles, and applications of big data analytics, and exploits blended teaching | ||
| Triola and Pusic [44] | 2012 | Literature review and case-study | USA | Authors described the development of the Education Data Warehouse, an initiative aimed at utilizing big data to link between medical educational curricula and patient healthcare outcomes | ||
| Cobb et al. [45] | 2018 | Database-based study, with a sample of 25,363 patients | USA | Authors exploited big data to monitor the safety of surgical operations performed by medical residents | ||
| Rajkomar et al. [46] | 2017 | Retrospective, database-based study | University of California, San Francisco, USA | Authors analyzed 53,066 clinical notes from 10,022 hospitalizations with 1436 different diagnoses spanning 217 diagnostic categories, written by postgraduate year 1, 2, and 3 internal medicine residents. Educational gaps could be identified | ||
| Chahine et al. [47] | 2018 | Literature review and case-study | Ontario, Canada | Authors presented a grassroots initiative, showing that big data can be used to dissect the relationship between various pedagogical/educational approaches to medical training and patient healthcare outcomes | ||
| Feldman and Chawla [48] | 2015 | Database-based analysis (geographic distribution analysis, and school similarity analysis) | USA | Authors utilized a large database to link between medical doctor’s training and performance/clinical outcomes. Big data can be exploited to shed light on knowledge transfer and educational experiences | ||
| Au-Yong-Oliveira et al. [49] | 2021 | Systematic literature review and bibliometric review of two major scholarly databases (PubMed/MEDLINE and Google Scholar), carried out by means of VOSviewer software | Not applicable | 215 studies were included, with a total of 757 (co-)authors. Fifteen authors resulted particularly inter-connected. Similarly, 379 out of 569 keywords were highly inter-connected. Based on the review, authors formulated a 4-dimension model: (I) data transformation (health information services; new health applications; medical images; artificial intelligence systems related to health procedures); (II) health intelligence (epidemic outbreak forecasting/nowcasting; drug discovery; big data analytics applied to diseases prediction; genome data); (III) data leveraging (patient information; health records; operational data; public health data); and, (IV) decision-making (disease diagnosis; real-time monitoring and tracking of patients; improving and enhancing of medical treatments; offering and delivering of patient-centered care provisions) | Exploiting big data in continuous medical education and learning |
| Potential Use/Application (Example) |
|---|
| Empowering medical students and enhancing classical education |
| Counteracting drop-out |
| Digitalizing education |
| Personalizing education |
| Promoting equity, inclusion, diversity |
| Enhancing integrity and ethics, avoiding plagiarism and duplication rate |
| Enhancing medical practice and continuous medical education and learning |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khamisy-Farah, R.; Gilbey, P.; Furstenau, L.B.; Sott, M.K.; Farah, R.; Viviani, M.; Bisogni, M.; Kong, J.D.; Ciliberti, R.; Bragazzi, N.L. Big Data for Biomedical Education with a Focus on the COVID-19 Era: An Integrative Review of the Literature. Int. J. Environ. Res. Public Health 2021, 18, 8989. https://doi.org/10.3390/ijerph18178989
Khamisy-Farah R, Gilbey P, Furstenau LB, Sott MK, Farah R, Viviani M, Bisogni M, Kong JD, Ciliberti R, Bragazzi NL. Big Data for Biomedical Education with a Focus on the COVID-19 Era: An Integrative Review of the Literature. International Journal of Environmental Research and Public Health. 2021; 18(17):8989. https://doi.org/10.3390/ijerph18178989
Chicago/Turabian StyleKhamisy-Farah, Rola, Peter Gilbey, Leonardo B. Furstenau, Michele Kremer Sott, Raymond Farah, Maurizio Viviani, Maurizio Bisogni, Jude Dzevela Kong, Rosagemma Ciliberti, and Nicola Luigi Bragazzi. 2021. "Big Data for Biomedical Education with a Focus on the COVID-19 Era: An Integrative Review of the Literature" International Journal of Environmental Research and Public Health 18, no. 17: 8989. https://doi.org/10.3390/ijerph18178989
APA StyleKhamisy-Farah, R., Gilbey, P., Furstenau, L. B., Sott, M. K., Farah, R., Viviani, M., Bisogni, M., Kong, J. D., Ciliberti, R., & Bragazzi, N. L. (2021). Big Data for Biomedical Education with a Focus on the COVID-19 Era: An Integrative Review of the Literature. International Journal of Environmental Research and Public Health, 18(17), 8989. https://doi.org/10.3390/ijerph18178989







