Evaluating the Prevalence and Incidence of Bronchiectasis and Nontuberculous Mycobacteria in South Korea Using the Nationwide Population Data
Abstract
:1. Introduction
2. Materials and Methods
2.1. Procedure
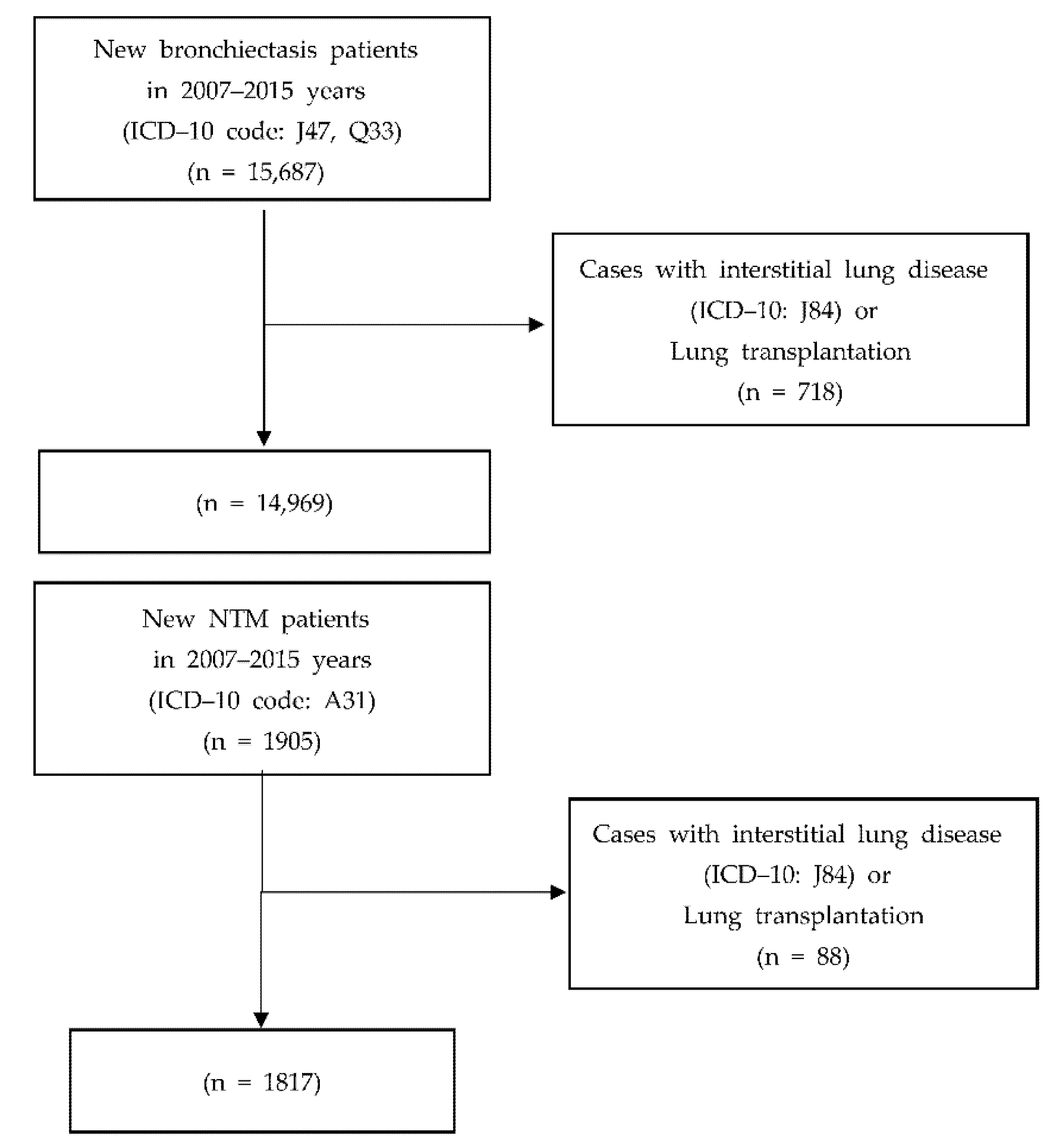
2.1.1. Research Subject Selection
2.1.2. Criteria for Exclusion of Study Subjects
2.2. Samples
Epidemiological Characteristics Investigation Methods
2.3. Ethical Considerations
2.4. Statistical Analysis
3. Results
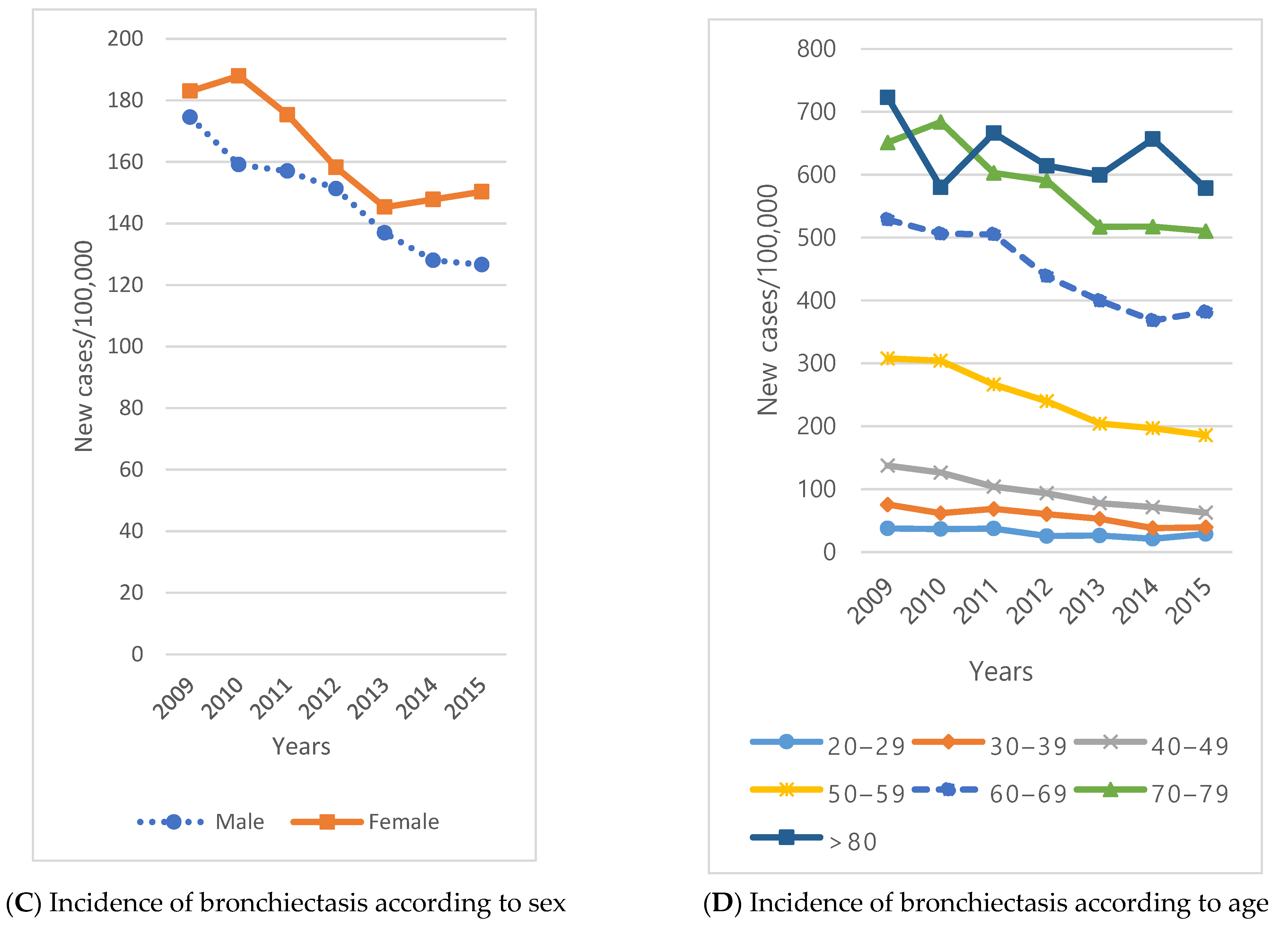
3.1. Bronchiectasis Prevalence/Incidence
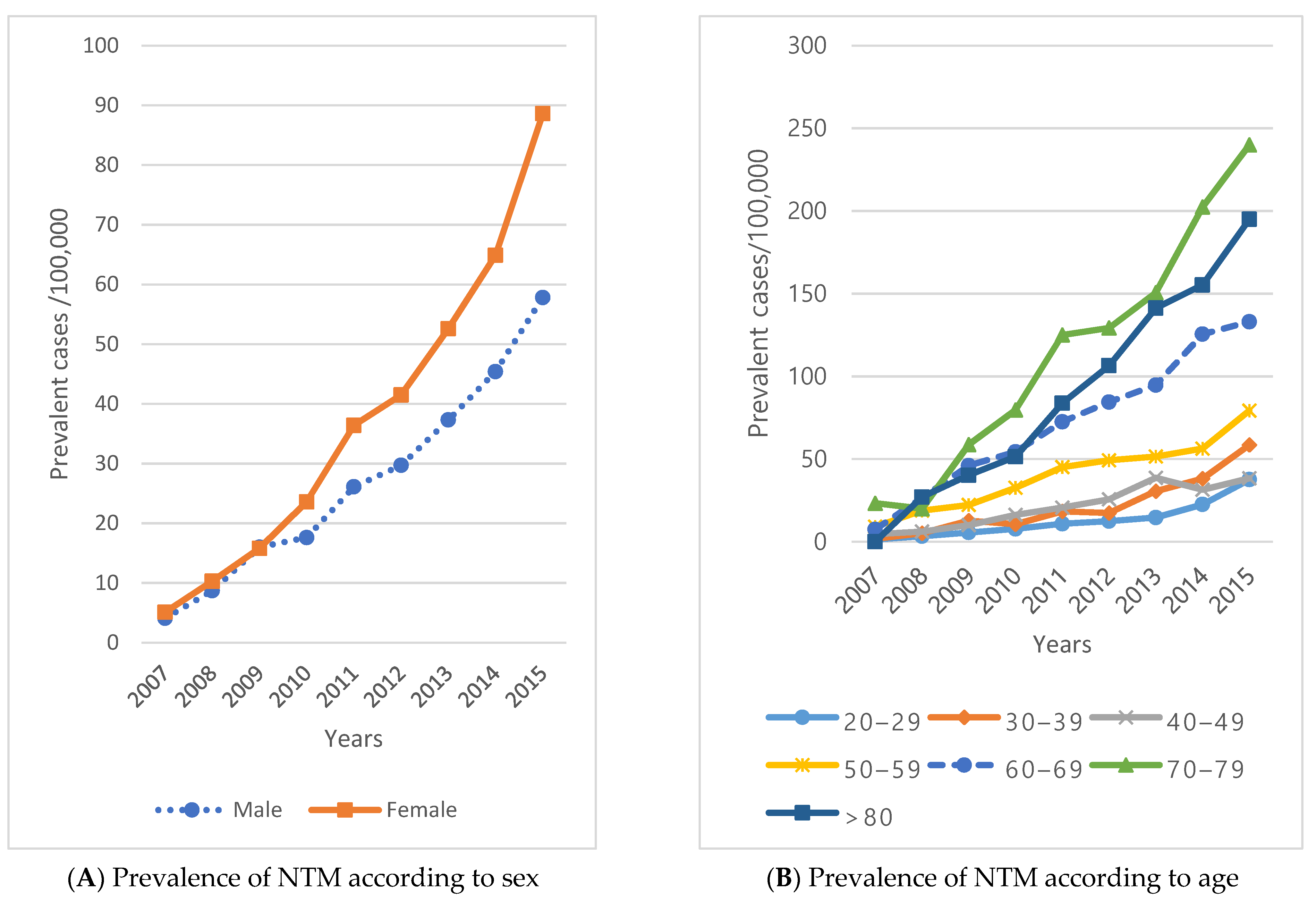
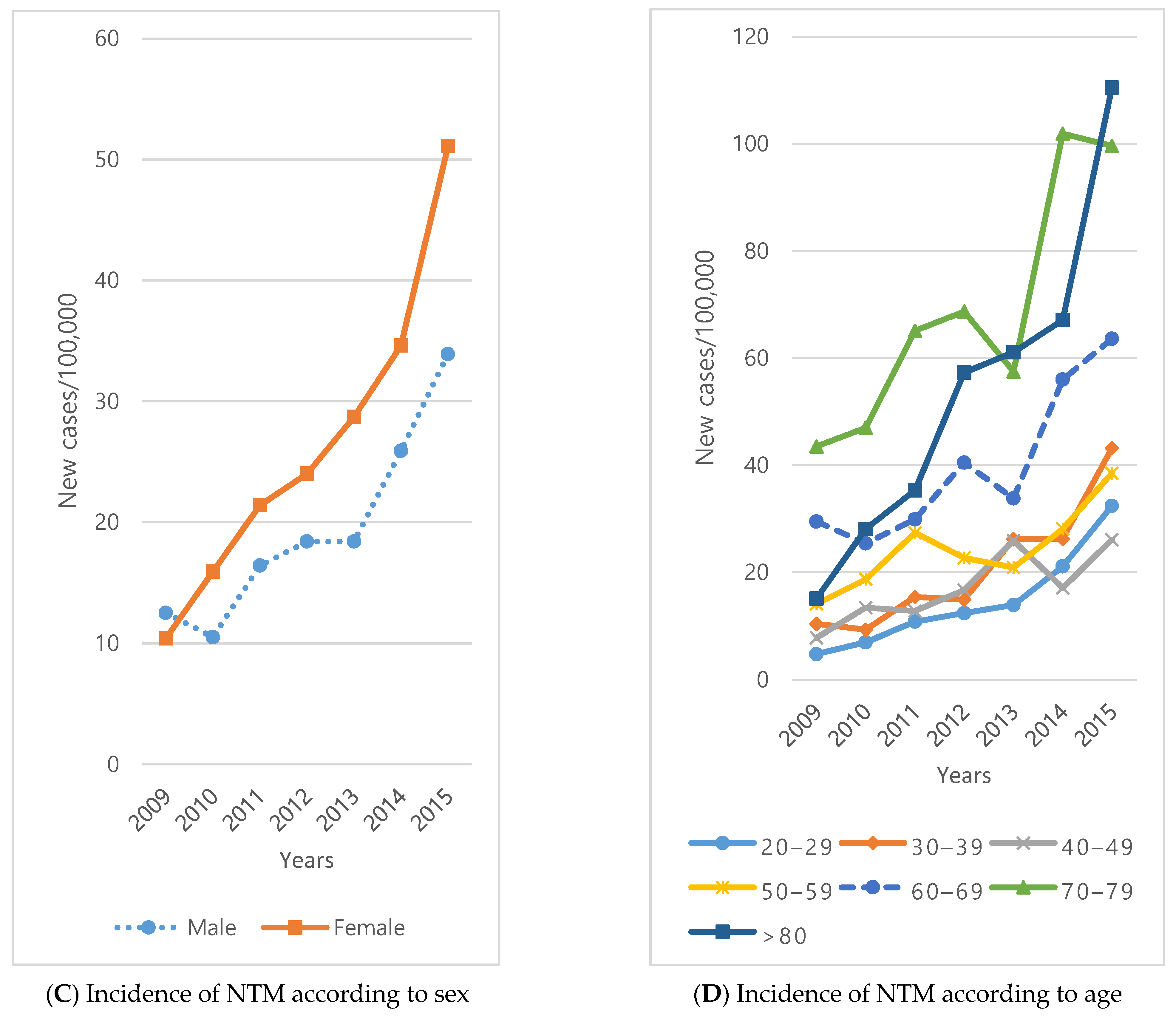
3.2. NTM Prevalence/Incidence
3.3. Relative Risk of Bronchiectasis
3.4. Relative Risk of NTM
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Quint, J.K.; Millett, E.; Joshi, M.; Navaratnam, V.; Thomas, S.L.; Hurst, J.R.; Smeeth, L.; Brown, J.S. Changes in the incidence, prevalence and mortality of bronchiectasis in the UK from 2004 to 2013: A population-based cohort study. Eur. Respir. J. 2016, 47, 186–193. [Google Scholar] [CrossRef]
- Visser, S.K.; Bye, P.; Morgan, L. Management of bronchiectasis in adults. Med. J. Aust. 2018, 209, 177–183. [Google Scholar] [CrossRef]
- Nicotra, M.B.; Rivera, M.; Dale, A.M.; Shepherd, R.; Carter, R. Clinical, Pathophysiologic, and Microbiologic Characterization of Bronchiectasis in an Aging Cohort. Chest 1995, 108, 955–961. [Google Scholar] [CrossRef]
- Jeon, D. Infection Source and Epidemiology of Nontuberculous Mycobacterial Lung Disease. Tuberc. Respir. Dis. 2019, 82, 94–101. [Google Scholar] [CrossRef]
- Griffith, D.E.; Aksamit, T.; Brown-Elliott, B.A.; Catanzaro, A.; Daley, C.; Gordin, F.; Holland, S.M.; Horsburgh, R.; Huitt, G.; Iademarco, M.F.; et al. An official ATS/IDSA statement: Diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am. J. Respir. Crit. Care Med. 2007, 175, 367–416. [Google Scholar] [CrossRef]
- Song, Y.; Jeong, H.; Lee, B.; Huh, H.; Koh, W.; Kim, J.; Ahn, K.; Kyung, Y. Nontuberculous mycobacterial pulmonary disease in a 16-year-old female patient with bronchiectasis. Allergy Asthma Respir. Dis. 2020, 8, 231–236. [Google Scholar] [CrossRef]
- Chan, E.D.; Iseman, M.D. Slender, Older Women Appear to Be More Susceptible to Nontuberculous Mycobacterial Lung Disease. Gend. Med. 2010, 7, 5–18. [Google Scholar] [CrossRef]
- Polverino, E.; Goeminne, P.C.; McDonnell, M.J.; Aliberti, S.; Marshall, S.E.; Loebinger, M.R.; Murris, M.; Cantón, R.; Torres, A.; Dimakou, K.; et al. European Respiratory Society guidelines for the management of adult bronchiectasis. Eur. Respir. J. 2017, 50, 1700629. [Google Scholar] [CrossRef]
- Seitz, A.E.; Olivier, K.N.; Adjemian, J.; Holland, S.M.; Prevots, D.R. Trends in Bronchiectasis Among Medicare Beneficiaries in the United States, 2000 to 2007. Chest 2012, 142, 432–439. [Google Scholar] [CrossRef] [Green Version]
- Chandrasekaran, R.; Mac Aogáin, M.; Chalmers, J.D.; Elborn, S.J.; Chotirmall, S.H. Geographic variation in the aetiology, epidemiology and microbiology of bronchiectasis. BMC Pulm. Med. 2018, 18, 83. [Google Scholar] [CrossRef]
- Metersky, M.; Chalmers, J. Bronchiectasis insanity: Doing the same thing over and over again and expecting different results? F1000Research 2019, 8, 293. [Google Scholar] [CrossRef] [Green Version]
- Chalmers, J.D.; Crichton, M.; Goeminne, P.C.; Loebinger, M.R.; Haworth, C.; Almagro, M.; Vendrell, M.; De Soyza, A.; Dhar, R.; Morgan, L.; et al. The European Multicentre Bronchiectasis Audit and Research Collaboration (EMBARC): Experiences from a successful ERS Clinical Research Collaboration. Breathe 2017, 13, 180–192. [Google Scholar] [CrossRef] [Green Version]
- Huang, H.-Y.; Chung, F.-T.; Lo, C.-Y.; Lin, H.-C.; Huang, Y.-T.; Yeh, C.-H.; Lin, C.-W.; Wang, C.-H. Etiology and characteristics of patients with bronchiectasis in Taiwan: A cohort study from 2002 to 2016. BMC Pulm. Med. 2020, 20, 45. [Google Scholar] [CrossRef] [Green Version]
- Young, S.L.; Puan, Y.; Chew, S.Y.; Haja Mohideen, S.M.; Tiew, P.Y.; Tan, G.L.; Koh, M.S.; Lee, K.C.H. Heterogeneity of non-cystic fibrosis bronchiectasis in multiethnic Singapore: A prospective cohort study at a tertiary pulmonary centre. Ann. Acad. Med. Singap. 2021, 50, 556–565. [Google Scholar] [CrossRef]
- Kwak, H.J.; Moon, J.-Y.; Choi, Y.W.; Kim, T.H.; Sohn, J.W.; Yoon, H.J.; Shin, D.H.; Park, S.S.; Kim, S.-H. High Prevalence of Bronchiectasis in Adults: Analysis of CT Findings in a Health Screening Program. Tohoku J. Exp. Med. 2010, 222, 237–242. [Google Scholar] [CrossRef] [Green Version]
- Nam, J.S.; Jeong, S.W.; Han, S.J.; Chang, J.H.; Choi, H.S. Idiopathic Sudden Sensorineural Hearing Loss Is Correlated with an Increased Risk of Stroke: An 11-Year Nationwide Population-Based Study. Korean J. Otorhinolaryngol. Neck Surg. 2016, 59, 353. [Google Scholar] [CrossRef]
- Lee, J.; Lee, J.S.; Park, S.H.; Shin, S.A.; Kim, K. Cohort profile: The National Health Insurance Service-national sample cohort (NHIS-NSC), South Korea. Int. J. Epidemiol. 2017, 46, e15. [Google Scholar] [CrossRef]
- Korean Standard Classification of Causes of Disease (KCD). Certain Infectious and Parasitic Diseases, A00~B99, 8th. 2020. Available online: https://www.koicd.kr/kcd/kcd.do?degree=08 (accessed on 11 May 2021).
- Lee, J.E.; Choi, J.-K.; Lim, H.S.; Kim, J.H.; Cho, J.H.; Kim, G.S.; Lee, P.H.; Sohn, Y.H.; Lee, J.H. The Prevalence and Incidence of Parkinson′s Disease in South Korea: A 10-Year Nationwide Population–Based Study. J. Korean Neurol. Assoc. 2017, 35, 191–198. [Google Scholar] [CrossRef]
- Vidaillac, C.; Yong, V.F.L.; Jaggi, T.K.; Soh, M.M.; Chotirmall, S.H. Gender differences in bronchiectasis: A real issue? Breathe 2018, 14, 108–121. [Google Scholar] [CrossRef]
- Raghavan, D.; Jain, R. Increasing awareness of sex differences in airway diseases. Respirology 2015, 21, 449–459. [Google Scholar] [CrossRef]
- Tan, Y.; Deng, Y.; Yan, X.; Liu, F.; Tan, Y.; Wang, Q.; Bao, X.; Pan, J.; Luo, X.; Yu, Y.; et al. Nontuberculous mycobacterial pulmonary disease and associated risk factors in China: A prospective surveillance study. J. Infect. 2021, 83, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Girón, R.M.; de Gracia Roldán, J.; Olveira, C.; Vendrell, M.; Martínez-García, M.Á.; de la Rosa, D.; Máiz, L.; Ancochea, J.; Vázquez, L.; Borderías, L.; et al. Sex bias in diagnostic delay in bronchiectasis: An analysis of the Spanish Historical Registry of Bronchiectasis. Chron. Respir. Dis. 2017, 14, 360–369. [Google Scholar] [CrossRef] [Green Version]
- Máiz, L.; Girón, R.; Olveira, C.; Vendrell, M.; Nieto, R.; Martínez-García, M.A. Prevalence and factors associated with nontuberculous mycobacteria in non-cystic fibrosis bronchiectasis: A multicenter observational study. BMC Infect. Dis. 2016, 16, 437. [Google Scholar] [CrossRef] [Green Version]
- Snell, N.; Gibson, J.; Jarrold, I.; Quint, J.K. Epidemiology of bronchiectasis in the UK: Findings from the British Lung Foundation’s “Respiratory health of the nation” project. Respir. Med. 2019, 158, 21–23. [Google Scholar] [CrossRef]
- Guan, W.-J.; Han, X.-R.; De La Rosa-Carrillo, D.; Martinez-Garcia, M.A. The significant global economic burden of bronchiectasis: A pending matter. Eur. Respir. J. 2019, 53, 1802392. [Google Scholar] [CrossRef]
- Goeminne, P.C.; Hernandez, F.; Diel, R.; Filonenko, A.; Hughes, R.; Juelich, F.; Solomon, G.M.; Upton, A.; Wichmann, K.; Xu, W.; et al. The economic burden of bronchiectasis—Known and unknown: A systematic review. BMC Pulm. Med. 2019, 19, 54. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Prevalence Rate | Incidence Rate | |||||||
|---|---|---|---|---|---|---|---|---|
| RR | 95% CI | p-Value | RR | 95% CI | p-Value | |||
| Lower Limit | Upper Limit | Lower Limit | Upper Limit | |||||
| Female | 0.99 | 0.97 | 1.00 | 0.116 | 0.95 | 0.92 | 0.98 | 0.004 |
| Male (ref) | 1.00 | 1 | ||||||
| Age group | ||||||||
| 0–9 | 0.12 | 0.11 | 0.13 | <0.001 | 0.13 | 0.11 | 0.15 | <0.001 |
| 10–19 | 0.17 | 0.16 | 0.18 | <0.001 | 0.16 | 0.14 | 0.18 | <0.001 |
| 20–29 | 0.26 | 0.25 | 0.27 | <0.001 | 0.28 | 0.25 | 0.31 | <0.001 |
| 30–39 | 0.55 | 0.53 | 0.57 | <0.001 | 0.54 | 0.5 | 0.59 | <0.001 |
| 50–59 | 2.66 | 2.59 | 2.72 | <0.001 | 2.56 | 2.41 | 2.72 | <0.001 |
| 60–69 | 4.66 | 4.53 | 4.81 | <0.001 | 4.55 | 4.29 | 4.82 | <0.001 |
| 70–79 | 6.78 | 6.62 | 6.96 | <0.001 | 6.2 | 5.83 | 6.59 | <0.001 |
| >80 | 8.10 | 7.85 | 8.41 | <0.001 | 7.23 | 6.7 | 7.8 | <0.001 |
| 40–49 (ref) | 1 | 1 | ||||||
| Residence | ||||||||
| (1) | 2.05 | 1.97 | 2.12 | <0.001 | 2.04 | 1.88 | 2.20 | <0.001 |
| (2) | 1.20 | 1.16 | 1.23 | <0.001 | 1.21 | 1.13 | 1.30 | <0.001 |
| (3) | 1.15 | 1.12 | 1.19 | <0.001 | 1.16 | 1.09 | 1.24 | <0.001 |
| (4) | 1.07 | 1.04 | 1.09 | <0.001 | 1.15 | 1.09 | 1.22 | <0.001 |
| (5) | 1.02 | 0.99 | 1.04 | 0.203 | 1.01 | 0.96 | 1.06 | 0.770 |
| (6) | 1.25 | 1.21 | 1.30 | <0.001 | 1.28 | 1.17 | 1.39 | <0.001 |
| (7) | 1.14 | 1.06 | 1.22 | 0.001 | 1.21 | 1.03 | 1.41 | 0.018 |
| (8) | 1.07 | 1.03 | 1.11 | <0.001 | 1.1 | 1.02 | 1.19 | 0.010 |
| (9) | 1.27 | 1.22 | 1.32 | <0.001 | 1.33 | 1.21 | 1.46 | <0.001 |
| (10) (ref) | 1 | 1 | ||||||
| Income, decile | ||||||||
| 2nd | 1.02 | 0.98 | 1.06 | 0.324 | 0.99 | 0.90 | 1.08 | 0.776 |
| 3rd | 0.99 | 0.95 | 1.03 | 0.677 | 1.03 | 0.94 | 1.12 | 0.564 |
| 4th | 0.97 | 0.93 | 1.01 | 0.147 | 0.95 | 0.87 | 1.03 | 0.233 |
| 5th | 1.01 | 0.97 | 1.05 | 0.627 | 1 | 0.92 | 1.09 | 0.979 |
| 6th | 0.99 | 0.96 | 1.03 | 0.694 | 1.04 | 0.96 | 1.13 | 0.350 |
| 7th | 1.04 | 1.01 | 1.08 | 0.021 | 1.04 | 0.96 | 1.13 | 0.309 |
| 8th | 1.10 | 1.06 | 1.14 | <0.001 | 1.12 | 1.04 | 1.21 | 0.002 |
| 9th | 1.04 | 1.01 | 1.07 | 0.013 | 1.06 | 0.98 | 1.13 | 0.147 |
| 10th | 1.14 | 1.11 | 1.19 | <0.001 | 1.1 | 1.02 | 1.18 | 0.011 |
| 1st (ref) | 1 | 1 | ||||||
| Types of insurance | ||||||||
| (A) | 1.24 | 1.22 | 1.26 | <0.001 | 1.17 | 1.13 | 1.21 | <0.001 |
| (B) (ref) | 1 | 1 | ||||||
| Prevalence Rate | Incidence Rate | |||||||
|---|---|---|---|---|---|---|---|---|
| RR | 95% CI | p-Value | RR | 95% CI | p-Value | |||
| Lower Limit | Upper Limit | Lower Limit | Upper Limit | |||||
| Female | 1.24 | 1.19 | 1.31 | <0.001 | 1.26 | 1.15 | 1.39 | <0.001 |
| Male (ref) | 1 | 1 | ||||||
| Age group | ||||||||
| 0–9 | 0.77 | 0.68 | 0.88 | <0.001 | 0.82 | 0.66 | 1.03 | 0.087 |
| 10–19 | 0.33 | 0.28 | 0.38 | <0.001 | 0.33 | 0.25 | 0.44 | <0.001 |
| 20–29 | 0.61 | 0.54 | 0.69 | <0.001 | 0.77 | 0.62 | 0.95 | 0.013 |
| 30–39 | 1.08 | 0.98 | 1.2 | 0.120 | 1.05 | 0.88 | 1.26 | 0.575 |
| 50–59 | 1.95 | 1.77 | 2.14 | <0.001 | 1.7 | 1.43 | 2.03 | <0.001 |
| 60–69 | 2.85 | 2.59 | 3.16 | <0.001 | 2.54 | 2.13 | 3.03 | <0.001 |
| 70–79 | 4.97 | 4.53 | 5.47 | <0.001 | 4.61 | 3.87 | 5.5 | <0.001 |
| >80 | 4.54 | 3.97 | 5.16 | <0.001 | 4.23 | 3.32 | 5.37 | <0.001 |
| 40–49 (ref) | 1 | 1 | ||||||
| Residence | ||||||||
| (1) | 0.48 | 0.39 | 0.58 | <0.001 | 0.56 | 0.4 | 0.78 | <0.001 |
| (2) | 0.66 | 0.59 | 0.74 | <0.001 | 0.62 | 0.49 | 0.77 | <0.001 |
| (3) | 0.85 | 0.77 | 0.92 | <0.001 | 1.04 | 0.89 | 1.21 | 0.647 |
| (4) | 0.34 | 0.3 | 0.38 | <0.001 | 0.36 | 0.3 | 0.44 | <0.001 |
| (5) | 1.05 | 0.98 | 1.13 | 0.158 | 0.97 | 0.85 | 1.1 | 0.618 |
| (6) | 0.61 | 0.53 | 0.72 | <0.001 | 0.62 | 0.47 | 0.83 | 0.001 |
| (7) | 0.55 | 0.41 | 0.75 | <0.001 | 0.62 | 0.37 | 1.04 | 0.070 |
| (8) | 0.67 | 0.59 | 0.75 | <0.001 | 0.83 | 0.68 | 1.01 | 0.062 |
| (9) | 0.6 | 0.5 | 0.71 | <0.001 | 0.51 | 0.36 | 0.72 | 0.001 |
| (10) (ref) | 1 | 1 | ||||||
| Income, decile | ||||||||
| 2nd | 1.1 | 0.95 | 1.27 | 0.195 | 1.27 | 1 | 1.63 | 0.054 |
| 3rd | 1.13 | 0.98 | 1.3 | 0.094 | 1.04 | 0.8 | 1.35 | 0.797 |
| 4th | 0.92 | 0.79 | 1.06 | 0.262 | 0.87 | 0.66 | 1.13 | 0.298 |
| 5th | 1.18 | 1.03 | 1.35 | 0.016 | 1.11 | 0.87 | 1.42 | 0.391 |
| 6th | 1.12 | 0.98 | 1.27 | 0.104 | 1.13 | 0.89 | 1.43 | 0.316 |
| 7th | 1.11 | 0.97 | 1.26 | 0.123 | 1.08 | 0.85 | 1.36 | 0.526 |
| 8th | 1.22 | 1.07 | 1.38 | 0.002 | 1.28 | 1.03 | 1.6 | 0.027 |
| 9th | 1.34 | 1.19 | 1.51 | <0.001 | 1.34 | 1.09 | 1.67 | 0.007 |
| 10th | 1.47 | 1.31 | 1.65 | <0.001 | 1.25 | 1.01 | 1.55 | 0.038 |
| 1st (ref) | 1 | 1 | ||||||
| Types of insurance | ||||||||
| (A) | 1.59 | 1.49 | 1.68 | <0.001 | 1.54 | 1.39 | 1.71 | <0.001 |
| (B) (ref) | 1 | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, D.-I.; Kang, S.; Choi, S. Evaluating the Prevalence and Incidence of Bronchiectasis and Nontuberculous Mycobacteria in South Korea Using the Nationwide Population Data. Int. J. Environ. Res. Public Health 2021, 18, 9029. https://doi.org/10.3390/ijerph18179029
Park D-I, Kang S, Choi S. Evaluating the Prevalence and Incidence of Bronchiectasis and Nontuberculous Mycobacteria in South Korea Using the Nationwide Population Data. International Journal of Environmental Research and Public Health. 2021; 18(17):9029. https://doi.org/10.3390/ijerph18179029
Chicago/Turabian StylePark, Da-In, Sungchan Kang, and Seunghye Choi. 2021. "Evaluating the Prevalence and Incidence of Bronchiectasis and Nontuberculous Mycobacteria in South Korea Using the Nationwide Population Data" International Journal of Environmental Research and Public Health 18, no. 17: 9029. https://doi.org/10.3390/ijerph18179029
APA StylePark, D.-I., Kang, S., & Choi, S. (2021). Evaluating the Prevalence and Incidence of Bronchiectasis and Nontuberculous Mycobacteria in South Korea Using the Nationwide Population Data. International Journal of Environmental Research and Public Health, 18(17), 9029. https://doi.org/10.3390/ijerph18179029






