Theory-Based Social and Non-Social Engagement Features in Smoking Cessation Mobile Apps: A Content Analysis
Abstract
:1. Introduction
1.1. Smoking Cessation Mobile Apps
1.2. Engagement Features of Health-Related Mobile Apps
1.2.1. Social Engagement Features
1.2.2. Non-Social Engagement Features
- RQ1: What social and non-social engagement features are present in current smoking cessation mobile apps?
- RQ2: What social and non-social engagement features predict the engagement of smoking cessation mobile app users?
2. Methods
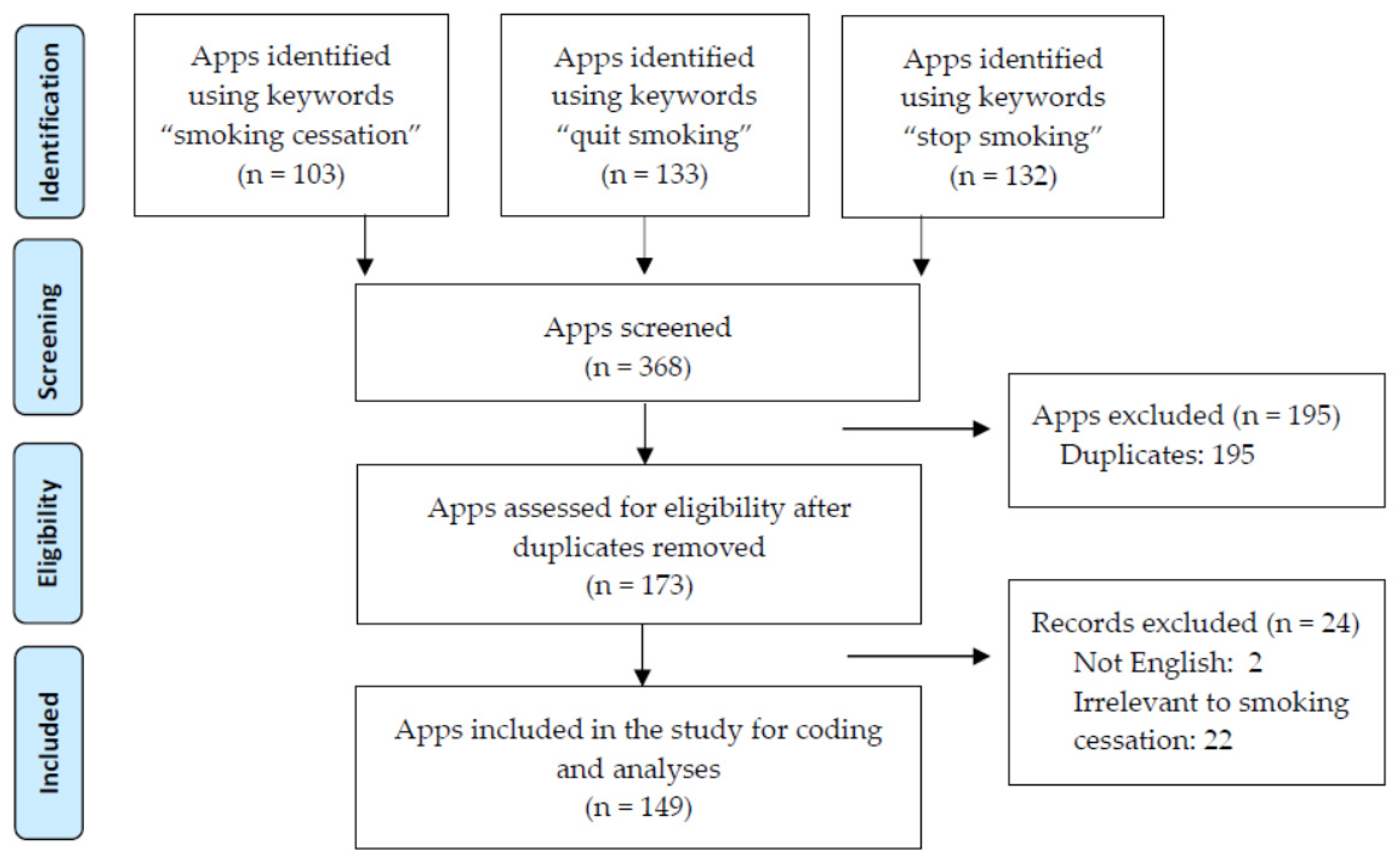
2.1. Sampling
2.2. Coding Scheme
2.3. Coding Procedure
2.4. Data Analysis
3. Results
3.1. Descriptive Statistics
3.2. Inferential Statistics
4. Discussion
4.1. Social Engagement Features
4.2. Non-Social Engagement Features
4.3. Theoretical and Practical Implications
4.4. Limitation and Future Research
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pew Research Center. Mobile Fact Sheet. Available online: http://www.pewinternet.org/fact-sheet/mobile/ (accessed on 7 April 2021).
- Krebs, P.; Duncan, D.T. Health app use among US mobile phone owners: A national survey. JMIR mHealth uHealth 2015, 3, e101. [Google Scholar] [CrossRef] [Green Version]
- Yang, Q.; Van Stee, S.K. The comparative effectiveness of mobile phone interventions in improving health outcomes: Meta-analytic review. JMIR mHealth uHealth 2019, 7, e11244. [Google Scholar] [CrossRef] [PubMed]
- Haskins, B.L.; Lesperance, D.; Gibbons, P.; Boudreaux, E.D. A systematic review of smartphone applications for smoking cessation. Transl. Behav. Med. 2017, 7, 292–299. [Google Scholar] [CrossRef] [PubMed]
- CDC. Smoking and Tobacco Use. Available online: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/fast_facts/index.htm (accessed on 2 June 2021).
- Heminger, C.L.; Schindler-Ruwisch, J.M.; Abroms, L.C. Smoking cessation support for pregnant women: Role of mobile technology. Subst. Abus. Rehabil. 2016, 7, 15–26. [Google Scholar] [CrossRef] [Green Version]
- Schwartz, R.P.; Gryczynski, J.; Mitchell, S.G.; Gonzales, A.; Moseley, A.; Peterson, T.R.; Ondersma, S.J.; O’Grady, K.E. Computerized versus in-person brief intervention for drug misuse: A randomized clinical trial. Addiction 2014, 109, 1091–1098. [Google Scholar] [CrossRef] [Green Version]
- Marcolino, M.S.; Oliveira, J.A.Q.; D’Agostino, M.; Ribeiro, A.L.; Alkmim, M.B.M.; Novillo-Ortiz, D. The Impact of mHealth Interventions: Systematic Review of Systematic Reviews. JMIR mHealth uHealth 2018, 6, e23. [Google Scholar] [CrossRef] [Green Version]
- Ghorai, K.; Akter, S.; Khatun, F.; Ray, P. mHealth for Smoking Cessation Programs: A Systematic Review. J. Pers. Med. 2014, 4, 412–423. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whittaker, R.; McRobbie, H.; Bullen, C.; Borland, R.; Rodgers, A.; Gu, Y. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst. Rev. 2016, 4, CD006611. [Google Scholar] [CrossRef]
- Noorhidawati, A.; Ghalebandi, S.G.; Hajar, R.S. How do young children engage with mobile apps? Cognitive, psychomotor, and affective perspective. Comput. Educ. 2015, 87, 385–395. [Google Scholar] [CrossRef]
- Ramo, D.E.; Thrul, J.; Chavez, K.; Delucchi, K.L.; Prochaska, J.J.; Norman, G.; Sadasivam, R.S.; Mehring, M. Feasibility and Quit Rates of the Tobacco Status Project: A Facebook Smoking Cessation Intervention for Young Adults. J. Med. Internet Res. 2015, 17, e291. [Google Scholar] [CrossRef] [Green Version]
- Yang, Q. Are Social Networking Sites Making Health Behavior Change Interventions More Effective? A Meta-Analytic Review. J. Health Commun. 2017, 22, 223–233. [Google Scholar] [CrossRef]
- Krishnan, A.; Zhou, X. Modeling the effect of health antecedents and social media engagement on healthy eating and quality of life. J. Appl. Commun. Res. 2019, 47, 365–380. [Google Scholar] [CrossRef]
- Richardson, A.; Graham, A.L.; Cobb, N.; Xiao, H.; Mushro, A.; Abrams, D.; Vallone, D. Engagement Promotes Abstinence in a Web-based Cessation Intervention: Cohort Study. J. Med. Internet Res. 2013, 15, e14. [Google Scholar] [CrossRef] [Green Version]
- Thompson, D. Designing Serious Video Games for Health Behavior Change: Current Status and Future Directions. J. Diabetes Sci. Technol. 2012, 6, 807–811. [Google Scholar] [CrossRef] [Green Version]
- Choi, J.; Noh, G.-Y.; Park, D.-J. Smoking Cessation Apps for Smartphones: Content Analysis with the Self-Determination Theory. J. Med. Internet Res. 2014, 16, e44. [Google Scholar] [CrossRef]
- Sama, P.R.; Eapen, Z.J.; Weinfurt, K.P.; Shah, B.R.; Schulman, K.A. An Evaluation of Mobile Health Application Tools. JMIR mHealth uHealth 2014, 2, e19. [Google Scholar] [CrossRef]
- MacMonegle, A.J.; Nonnemaker, J.; Duke, J.C.; Farrelly, M.C.; Zhao, X.; Delahanty, J.C.; Smith, A.A.; Rao, P.; Allen, J.A. Cost-Effectiveness Analysis of The Real Cost Campaign’s Effect on Smoking Prevention. Am. J. Prev. Med. 2018, 55, 319–325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steinhubl, S.R.; Muse, E.D.; Topol, E.J. Can Mobile Health Technologies Transform Health Care? JAMA 2013, 310, 2395–2396. [Google Scholar] [CrossRef] [PubMed]
- Hall, A.K.; Cole-Lewis, H.; Bernhardt, J.M. Mobile Text Messaging for Health: A Systematic Review of Reviews. Annu. Rev. Public Health 2015, 36, 393–415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keoleian, V.; Polcin, D.; Galloway, G.P. Text Messaging for Addiction: A Review. J. Psychoact. Drugs 2015, 47, 158–176. [Google Scholar] [CrossRef] [Green Version]
- Abroms, L.C.; Ahuja, M.; Kodl, Y.; Thaweethai, L.; Sims, J.; Winickoff, J.P.; Windsor, R.A. Text2Quit: Results From a Pilot Test of a Personalized, Interactive Mobile Health Smoking Cessation Program. J. Health Commun. 2012, 17, 44–53. [Google Scholar] [CrossRef] [Green Version]
- Hawkins, R.P.; Han, J.-Y.; Pingree, S.; Shaw, B.R.; Baker, T.B.; Roberts, L.J. Interactivity and presence of three eHealth interventions. Comput. Hum. Behav. 2010, 26, 1081–1088. [Google Scholar] [CrossRef] [Green Version]
- Tate, D.F.; Jackvony, E.H.; Wing, R.R. A Randomized Trial Comparing Human e-Mail Counseling, Computer-Automated Tailored Counseling, and No Counseling in an Internet Weight Loss Program. Arch. Intern. Med. 2006, 166, 1620–1625. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abroms, L.C.; Padmanabhan, N.; Thaweethai, L.; Phillips, T. iPhone Apps for Smoking Cessation: A Content Analysis. Am. J. Prev. Med. 2011, 40, 279–285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abroms, L.C.; Westmaas, J.L.; Bontemps-Jones, J.; Ramani, R.; Mellerson, J. A Content Analysis of Popular Smartphone Apps for Smoking Cessation. Am. J. Prev. Med. 2013, 45, 732–736. [Google Scholar] [CrossRef] [Green Version]
- Hoeppner, B.B.; Hoeppner, S.S.; Seaboyer, L.; Schick, M.R.; Wu, G.W.; Bergman, B.G.; Kelly, J.F. How Smart are Smartphone Apps for Smoking Cessation? A Content Analysis. Nicotine Tob. Res. 2016, 18, 1025–1031. [Google Scholar] [CrossRef] [Green Version]
- The CPG-TTUD 2008 Update Panel, Liaisons, and Staff. A clinical practice guideline for treating tobacco use and dependence: 2008 update: A US public health service report. Am. J. Prev. Med. 2008, 35, 158–176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pechmann, C.; Pan, L.; Delucchi, K.; Lakon, C.M.; Prochaska, J.J. Development of a Twitter-Based Intervention for Smoking Cessation that Encourages High-Quality Social Media Interactions via Automessages. J. Med. Internet Res. 2015, 17, e50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eysenbach, G. The Law of Attrition. J. Med. Internet Res. 2005, 7, e11. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Wills, T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985, 98, 310–357. [Google Scholar] [CrossRef]
- Festinger, L. A Theory of Social Comparison Processes. Hum. Relat. 1954, 7, 117–140. [Google Scholar] [CrossRef]
- Bandura, A. Social cognitive theory of self-regulation. Organ. Behav. Hum. Decis. Process. 1991, 50, 248–287. [Google Scholar] [CrossRef]
- Bandura, A. Social Foundations of Thought and Action: A Social Cognitive Theory; Prentice-Hall: Englewood Cliffs, NJ, USA, 1986. [Google Scholar]
- Ryan, R.M.; Deci, E.L. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am. Psychol. 2000, 55, 68–78. [Google Scholar] [CrossRef]
- Ubhi, H.K.; Michie, S.; Kotz, D.; Van Schayck, O.C.P.; Selladurai, A.; West, R. Characterising smoking cessation smartphone applications in terms of behaviour change techniques, engagement and ease-of-use features. Transl. Behav. Med. 2016, 6, 410–417. [Google Scholar] [CrossRef] [Green Version]
- Baskerville, N.B.; Azagba, S.; Norman, C.; McKeown, K.; Brown, K.S. Effect of a Digital Social Media Campaign on Young Adult Smoking Cessation. Nicotine Tob. Res. 2015, 18, 351–360. [Google Scholar] [CrossRef] [Green Version]
- Struik, L.L.; Baskerville, N.B. The Role of Facebook in Crush the Crave, a Mobile- and Social Media-Based Smoking Cessation Intervention: Qualitative Framework Analysis of Posts. J. Med. Internet Res. 2014, 16, e170. [Google Scholar] [CrossRef] [PubMed]
- Westmaas, J.L.; Bontemps-Jones, J.; E Bauer, J. Social support in smoking cessation: Reconciling theory and evidence. Nicotine Tob. Res. 2010, 12, 695–707. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cavallo, D.N.; Tate, D.F.; Ries, A.V.; Brown, J.D.; DeVellis, R.F.; Ammerman, A.S. A Social Media–Based Physical Activity Intervention: A randomized controlled trial. Am. J. Prev. Med. 2012, 43, 527–532. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Livingston, J.D.; Cianfrone, M.; Korf-Uzan, K.; Coniglio, C. Another time point, a different story: One year effects of a social media intervention on the attitudes of young people towards mental health issues. Soc. Psychiatry Psychiatr. Epidemiol. 2014, 49, 985–990. [Google Scholar] [CrossRef] [PubMed]
- Bull, S.S.; Levine, D.K.; Black, S.R.; Schmiege, S.J.; Santelli, J. Social Media–Delivered Sexual Health Intervention: A cluster randomized controlled trial. Am. J. Prev. Med. 2012, 43, 467–474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsieh, H.-F.; Shannon, S.E. Three Approaches to Qualitative Content Analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef]
- DeviceAtlas. Android v iOS Market Share 2018. Available online: https://deviceatlas.com/blog/android-v-ios-market-share#us (accessed on 9 September 2019).
- Stoyanov, S.R.; Hides, L.; Kavanagh, D.J.; Zelenko, O.; Tjondronegoro, D.; Mani, M. Mobile App Rating Scale: A New Tool for Assessing the Quality of Health Mobile Apps. JMIR mHealth uHealth 2015, 3, e27. [Google Scholar] [CrossRef] [Green Version]
- Krippendorff, K. Content Analysis: An Introduction to Its Methodology, 3rd ed.; SAGE Publications Inc.: Thousand Oaks, CA, USA, 2013. [Google Scholar]
- Bustamante, L.A.; Ménard, C.G.; Julien, S.; Romo, L. Behavior Change Techniques in Popular Mobile Apps for Smoking Cessation in France: Content Analysis. JMIR mHealth uHealth 2021, 9, e26082. [Google Scholar] [CrossRef]
- Foster, D.; Linehan, C.; Kirman, B.; Lawson, S.; James, G. Motivating physical activity at work: Using persuasive social media for competitive step counting. In Proceedings of the 14th International Academic MindTrek Conference on Envisioning Future Media Environments, Tampere, Finland, 6–8 October 2010; pp. 111–116. [Google Scholar]
- Lepper, M.; Master, A.; Yow, W. Intrinsic motivation in education. In Social Psychological Perspectives—Advances in Motivation and Achievement; Maehr, M.L., Karabenick, S.A., Urdan, T.C., Eds.; Emerald: Bingley, UK, 2008; Volume 15, pp. 521–555. [Google Scholar]
- Mummah, S.A.; Mathur, M.; King, A.C.; Gardner, C.D.; Sutton, S. Mobile Technology for Vegetable Consumption: A Randomized Controlled Pilot Study in Overweight Adults. JMIR mHealth uHealth 2016, 4, e51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maher, C.; Ferguson, M.; Vandelanotte, C.; Plotnikoff, R.; De Bourdeaudhuij, I.; Thomas, S.; Nelson-Field, K.; Olds, T. A Web-Based, Social Networking Physical Activity Intervention for Insufficiently Active Adults Delivered via Facebook App: Randomized Controlled Trial. J. Med. Internet Res. 2015, 17, e174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, Q. Understanding Computer-Mediated Support Groups: A Revisit Using a Meta-Analytic Approach. Health Commun. 2020, 35, 209–221. [Google Scholar] [CrossRef] [PubMed]
- Hughes, J.R.; Keely, J.; Naud, S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction 2004, 99, 29–38. [Google Scholar] [CrossRef]
- Du, H.; Venkatakrishnan, A.; Youngblood, G.M.; Ram, A.; Pirolli, P. A Group-Based Mobile Application to Increase Adherence in Exercise and Nutrition Programs: A Factorial Design Feasibility Study. JMIR mHealth uHealth 2016, 4, e4. [Google Scholar] [CrossRef] [Green Version]
- Perski, O.; Blandford, A.; Ubhi, H.K.; West, R.; Michie, S. Smokers’ and drinkers’ choice of smartphone applications and expectations of engagement: A think aloud and interview study. BMC Med. Inform. Decis. Mak. 2017, 17, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Noar, S.M.; Benac, C.N.; Harris, M.S. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol. Bull. 2007, 133, 673–693. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petty, R.E.; Cacioppo, J.T. Attitudes and Persuasion: Classic and Contemporary Approaches; Routledge: New York, NY, USA, 1981. [Google Scholar]
- Regmi, K.; Kassim, N.; Ahmad, N.; Tuah, N.A. Effectiveness of Mobile Apps for Smoking Cessation: A Review. Tob. Prev. Cessat. 2017, 3, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Mierlo, T.; Voci, S.; Lee, S.; Fournier, R.; Selby, P. Superusers in Social Networks for Smoking Cessation: Analysis of Demographic Characteristics and Posting Behavior from the Canadian Cancer Society’s Smokers’ Helpline Online and StopSmokingCenter.net. J. Med. Internet Res. 2012, 14, e66. [Google Scholar] [CrossRef] [PubMed]
- Greene, B.A. Measuring Cognitive Engagement with Self-Report Scales: Reflections from over 20 Years of Research. Educ. Psychol. 2015, 50, 14–30. [Google Scholar] [CrossRef]
- Brusse, C.; Gardner, K.; McAullay, D.; Dowden, M. Social Media and Mobile Apps for Health Promotion in Australian Indigenous Populations: Scoping Review. J. Med. Internet Res. 2014, 16, e280. [Google Scholar] [CrossRef] [PubMed]
| Engagement Features | Operational Definition | n (%) | DV: Engagement | |
|---|---|---|---|---|
| Social | 1. Social support | The app has or creates groups for the users to interact with online or in person for discussing stress, problem solving, encouraging, etc. | 12 (8.1) | β = 0.30 *** |
| 2. Social announcement | The app allows the user to implicit social reinforcement through announcing an achievement, process, or action through an app tool or social media. | 42 (28.2) | β = 0.21 * | |
| 3. Social referencing | The app allows the user to compare their behavior (must be quantifiable such as user score) to other app users, such as through an online or social group that uses the same feature. | 2 (1.3) | β = 0.18 * | |
| Non-social | 1. Personal environmental changes | The environment in the app changes in response to user’s action to promote smoking cessation through the use of soothing sounds, images for meditations, white noise, or other changes. | 59 (39.6) | β = 0.38 *** |
| 2. Goal setting | The app promotes goal setting, such as setting the number of cigarettes that will be decreased day. | 34 (22.8) | β = 0.14 | |
| 3. Progress tracking | The app allows users to identify a goal and then creates tasks based on these goals and tracks the user’s progress. | 31 (20.8) | β = 0.18 * | |
| 4. Reinforcement tracking | A third party assigns reinforcements based on information collected about the user’s health or behaviors. | 0 (0.0) | - | |
| 5. Self-monitoring | The app allows the user to track their behavior (e.g., number of cigarettes smoked per day) with no reference to a specific goal. | 73 (49.0) | β = −0.01 | |
| 6. Personalized recommendations | The app provides tailored verbal/textual detailed feedback and responses based on relevant questions. Examples include tips and messages based on the user’s needs. Does not include tracking. | 14 (9.4) | β = 0.37 *** | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, Q. Theory-Based Social and Non-Social Engagement Features in Smoking Cessation Mobile Apps: A Content Analysis. Int. J. Environ. Res. Public Health 2021, 18, 9106. https://doi.org/10.3390/ijerph18179106
Yang Q. Theory-Based Social and Non-Social Engagement Features in Smoking Cessation Mobile Apps: A Content Analysis. International Journal of Environmental Research and Public Health. 2021; 18(17):9106. https://doi.org/10.3390/ijerph18179106
Chicago/Turabian StyleYang, Qinghua. 2021. "Theory-Based Social and Non-Social Engagement Features in Smoking Cessation Mobile Apps: A Content Analysis" International Journal of Environmental Research and Public Health 18, no. 17: 9106. https://doi.org/10.3390/ijerph18179106






