Effects of Intended Scapular Posterior Tilt Motion on Trapezius Muscle Electromyography Activity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. EMG
2.3. Scapular Posterior Tilt Recording
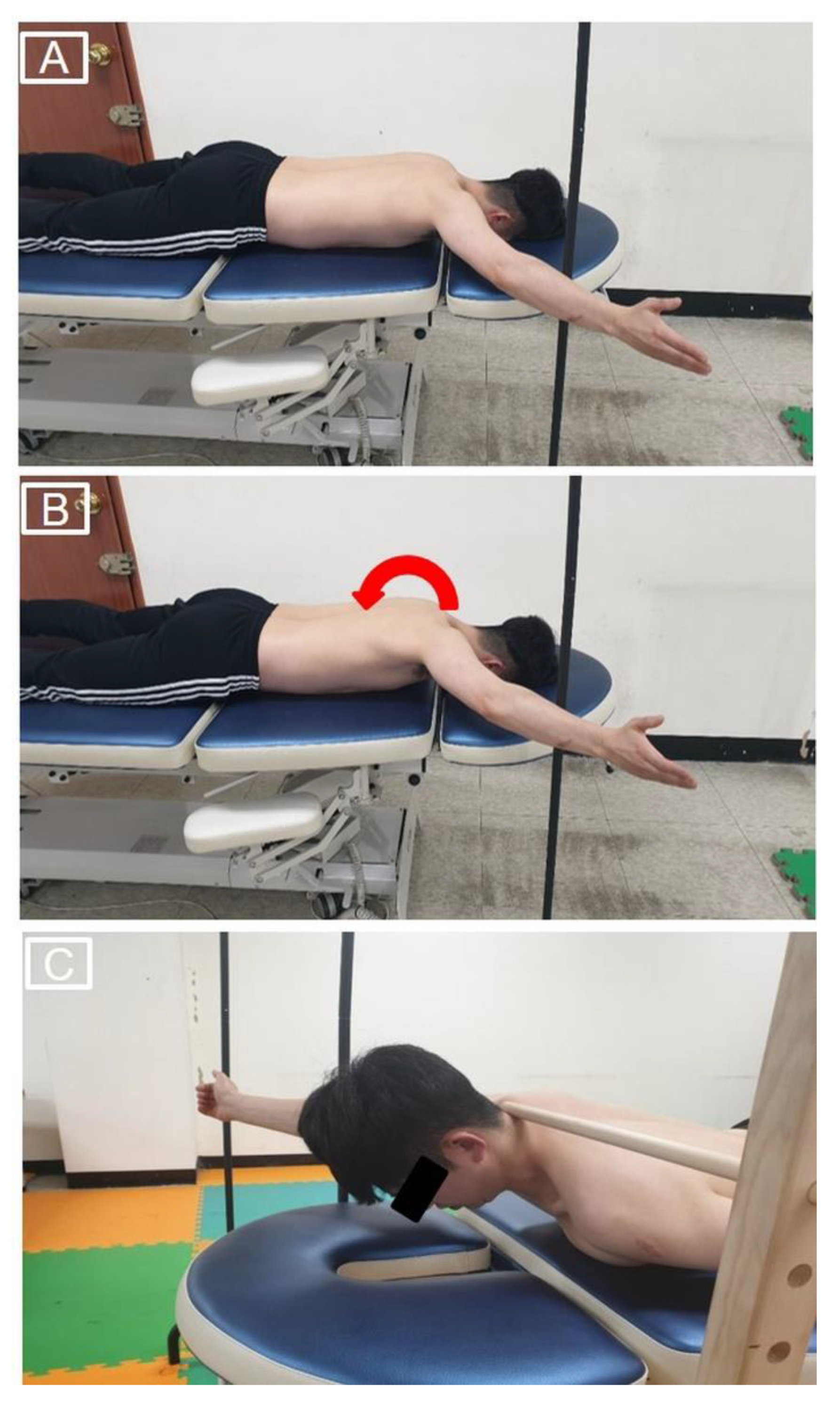
2.4. The Intended Scapular Posterior Tilt Training
2.5. Prone Shoulder Horizontal Abduction Exercises
2.6. Experimental Procedures
2.7. Data and Statistical Analyses
3. Results
3.1. EMG
3.2. Scapular Posterior Tilt
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cools, A.M.; Struyf, F.; De Mey, K.; Maenhout, A.; Castelein, B.; Cagnie, B. Rehabilitation of scapular dyskinesis: From the office worker to the elite overhead athlete. Br. J. Sports Med. 2014, 48, 692–697. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, T.S.; Ou, H.L.; Huang, C.Y.; Lin, J.J. Specific kinematics and associated muscle activation in individuals with scapular dyskinesis. J. Shoulder Elbow Surg. 2015, 24, 1227–1234. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.S.; Du, W.Y.; Wang, T.G.; Tsai, Y.S.; Yang, J.L.; Huang, C.Y.; Lin, J.J. Progressive conscious control of scapular orientation with video feedback has improvement in muscle balance ratio in patients with scapular dyskinesis: A randomized controlled trial. J. Shoulder Elbow Surg. 2018, 27, 1407–1414. [Google Scholar] [CrossRef] [PubMed]
- Kibler, W.B.; Sciascia, A.; Wilkes, T. Scapular dyskinesis and its relation to shoulder injury. J. Am. Acad. Orthop. Surg. 2012, 20, 364–372. [Google Scholar] [CrossRef] [PubMed]
- Cools, A.M.; Witvrouw, E.E.; Declercq, G.A.; Danneels, L.A.; Cambier, D.C. Scapular muscle recruitment patterns: Trapezius muscle latency with and without impingement symptoms. Am. J. Sports Med. 2003, 31, 542–549. [Google Scholar] [CrossRef]
- Ludewig, P.M.; Braman, J.P. Shoulder impingement: Biomechanical considerations in rehabilitation. Man Ther. 2011, 16, 33–39. [Google Scholar] [CrossRef] [Green Version]
- Cools, A.M.; Declercq, G.A.; Cambier, D.C.; Mahieu, N.N.; Witvrouw, E.E. Trapezius activity and intramuscular balance during isokinetic exercise in overhead athletes with impingement symptoms. Scand. J. Med. Sci. Sports 2007, 17, 25–33. [Google Scholar] [CrossRef]
- Smith, M.; Sparkes, V.; Busse, M.; Enright, S. Upper and lower trapezius muscle activity in subjects with subacromial impingement symptoms: Is there imbalance and can taping change it? Phys. Ther. Sport 2009, 10, 45–50. [Google Scholar] [CrossRef]
- Johnson, G.; Bogduk, N.; Nowitzke, A.; House, D. Anatomy and actions of the trapezius muscle. Clin. Biomech. 1994, 9, 44–50. [Google Scholar] [CrossRef]
- Kim, S.Y.; Weon, J.H.; Jung, D.Y.; Oh, J.S. Effect of the scapula-setting exercise on acromio-humeral distance and scapula muscle activity in patients with subacromial impingement syndrome. Phys. Ther. Sport 2019, 37, 99–104. [Google Scholar] [CrossRef]
- Neumann, D.A. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation, 3rd ed.; Elsevier: St. Louis, MI, USA, 2017. [Google Scholar]
- Michener, L.A.; McClure, P.W.; Karduna, A.R. Anatomical and biomechanical mechanisms of subacromial impingement syndrome. Clin. Biomech. 2003, 18, 369–379. [Google Scholar] [CrossRef]
- Struyf, F.; Cagnie, B.; Cools, A.; Baert, I.; Brempt, J.V.; Struyf, P.; Meeus, M. Scapulothoracic muscle activity and recruitment timing in patients with shoulder impingement symptoms and glenohumeral instability. J. Electromyogr. Kinesiol. 2014, 24, 277–284. [Google Scholar] [CrossRef]
- Jones, S.A.; Pamukoff, D.N.; Mauntel, T.C.; Blackburn, J.T.; Myers, J.B. The influence of verbal and tactile feedback on electromyographic amplitude of the shoulder musculature during common therapeutic exercises. J. Sport Rehabil. 2018, 27, 424–430. [Google Scholar] [CrossRef] [PubMed]
- Kinney, E.; Wusthoff, J.; Zyck, A.; Hatzel, B.; Vaughn, D.; Strickler, T.; Glass, S. Activation of the trapezius muscle during varied forms of Kendall exercises. Phys. Ther. Sport 2008, 9, 3–8. [Google Scholar] [CrossRef]
- Ekstrom, R.A.; Donatelli, R.A.; Soderberg, G.L. Surface electromyographic analysis of exercises for the trapezius and serratus anterior muscles. J. Orthop. Sports Phys. Ther. 2003, 33, 247–258. [Google Scholar] [CrossRef] [PubMed]
- Ekstrom, R.A.; Soderberg, G.L.; Donatelli, R.A. Normalization procedures using maximum voluntary isometric contractions for the serratus anterior and trapezius muscles during surface EMG analysis. J. Electromyogr. Kinesiol. 2005, 15, 418–428. [Google Scholar] [CrossRef] [PubMed]
- Arlotta, M.; Lovasco, G.; McLean, L. Selective recruitment of the lower fibers of the trapezius muscle. J. Electromyogr. Kinesiol. 2011, 21, 403–410. [Google Scholar] [CrossRef]
- Chopp-Hurley, J.N.; Prophet, C.; Thistle, B.; Pollice, J.; Maly, M.R. Scapular muscle activity during static yoga postures. J. Orthop. Sports Phys. Ther. 2018, 48, 504–509. [Google Scholar] [CrossRef] [PubMed]
- McGalliard, M.K.; Dedrick, G.S.; Brismée, J.M.; Cook, C.E.; Apte, G.G.; Sizer, P.S., Jr. Changes in transversus abdominis thickness with use of the abdominal drawing-in maneuver during a functional task. PM R 2010, 2, 187–194. [Google Scholar] [CrossRef]
- Mew, R. Comparison of changes in abdominal muscle thickness between standing and crook lying during active abdominal hollowing using ultrasound imaging. Man Ther. 2009, 14, 690–695. [Google Scholar] [CrossRef]
- Ludewig, P.M.; Cook, T.M.; Nawoczenski, D.A. Three-dimensional scapular orientation and muscle activity at selected positions of humeral elevation. J. Orthop. Sports Phys. Ther. 1996, 24, 57–65. [Google Scholar] [CrossRef] [Green Version]
- Worsley, P.; Warner, M.; Mottram, S.; Gadola, S.; Veeger, H.E.; Hermens, H.; Morrissey, D.; Little, P.; Cooper, C.; Carr, A.; et al. Motor control retraining exercises for shoulder impingement: Effects on function, muscle activation, and biomechanics in young adults. J. Shoulder Elbow Surg. 2013, 22, e11–e19. [Google Scholar] [CrossRef] [Green Version]
- De Mey, K.; Danneels, L.A.; Cagnie, B.; Huyghe, L.; Seyns, E.; Cools, A.M. Conscious correction of scapular orientation in overhead athletes performing selected shoulder rehabilitation exercises: The effect on trapezius muscle activation measured by surface electromyography. J. Orthop. Sports Phys. Ther. 2013, 43, 3–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hislop, H.J.; Avers, D.; Brown, M. Daniels and Worthingham’s Muscle Testing: Techniques of Manual Examination and Performance Testing, 9th ed.; Elsevier: St. Louis, MO, USA, 2013. [Google Scholar]
- Kendall, F.P.; McCreary, E.K.; Provance, P.G.; Rodgers, M.M.; Romani, W.A. Muscles: Testing and Function with Posture and Pain, 5th ed.; Williams & Wilkins: Baltimore, MD, USA, 2005. [Google Scholar]
- Scibek, J.S.; Carcia, C.R. Validation of a new method for assessing scapular anterior-posterior tilt. Int. J. Sports Phys. Ther. 2014, 9, 644–656. [Google Scholar] [PubMed]
- Ou, H.L.; Huang, T.S.; Chen, Y.T.; Chen, W.Y.; Chang, Y.L.; Lu, T.W.; Chen, T.H.; Lin, J.J. Alterations of scapular kinematics and associated muscle activation specific to symptomatic dyskinesis type after conscious control. Man Ther. 2016, 26, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Ludewig, P.M.; Cook, T.M. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys. Ther. 2000, 80, 276–291. [Google Scholar] [CrossRef] [PubMed]




| Muscles | Placements of Electrodes | MVIC Methods |
|---|---|---|
| UT | Midway between 7th cervical vertebrae and acromion along the line of muscle fiber | Participant performed shoulder elevation, ipsilateral cervical side-flexion, and contralateral cervical rotation against resistance applied to the shoulder and head by an examiner in the opposite direction of movements of participant in the sitting |
| MT | Midway between 3rd thoracic vertebrae and root of scapular spine along the line of muscle fiber | Participant performed shoulder horizontal abduction in prone with 90° of shoulder abduction and 90° of elbow flexion against resistance applied to the distal humerus by an examiner |
| LT | Midway between 7th thoracic vertebrae and intersection of the spine and medial boarder of the scapula along the line of muscle fiber | Participant performed PSHA with shoulder external rotation and elbow extension while diagonally placing arm overhead in line with LT muscle fiber against resistance applied to the forearm by an examiner |
| Measure | Preferred PSHA | PSHA with The Intended Scapular Posterior Tilt | PSHA with The Intended Scapular Posterior Tilt and Trunk Extension | p |
|---|---|---|---|---|
| UT (%MVIC) | 28.82 ± 12.82 3 | 28.61 ± 14.07 3 | 36.55 ± 16.87 2 | 0.001 1 |
| MT (%MVIC) | 55.20 ± 15.17 | 54.16 ± 16.53 | 56.68 ± 20.96 | 0.710 |
| LT (%MVIC) | 65.67 ± 11.18 3 | 76.23 ± 10.13 2 | 74.98 ± 12.89 2 | <0.001 1 |
| UT/MT activity (ratio) | 0.54 ± 0.26 3 | 0.55 ± 0.27 3 | 0.72 ± 0.42 2 | 0.021 1 |
| UT/LT activity (ratio) | 0.45 ± 0.20 | 0.38 ± 0.17 2,3 | 0.49 ± 0.19 | <0.001 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.-Y.; Yu, I.-Y.; Oh, J.-S.; Kang, M.-H. Effects of Intended Scapular Posterior Tilt Motion on Trapezius Muscle Electromyography Activity. Int. J. Environ. Res. Public Health 2021, 18, 9147. https://doi.org/10.3390/ijerph18179147
Kim S-Y, Yu I-Y, Oh J-S, Kang M-H. Effects of Intended Scapular Posterior Tilt Motion on Trapezius Muscle Electromyography Activity. International Journal of Environmental Research and Public Health. 2021; 18(17):9147. https://doi.org/10.3390/ijerph18179147
Chicago/Turabian StyleKim, Soo-Yong, Il-Young Yu, Jae-Seop Oh, and Min-Hyeok Kang. 2021. "Effects of Intended Scapular Posterior Tilt Motion on Trapezius Muscle Electromyography Activity" International Journal of Environmental Research and Public Health 18, no. 17: 9147. https://doi.org/10.3390/ijerph18179147







