Effect of Distraction Intervention for Needle-Related Pain and Distress in Children: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. The Review
2.1. Aims
2.2. Design
2.3. Search Methods
2.4. Search Outcomes
2.5. Quality Appraisal
2.6. Data Abstraction
2.7. Synthesis
3. Results
3.1. Study Characteristics
3.2. Methodological Quality
3.3. Effect of Distraction Intervention on Needle-Related Pain in Children
3.4. Effect of Distraction Intervention on Needle-Related Distress in Children
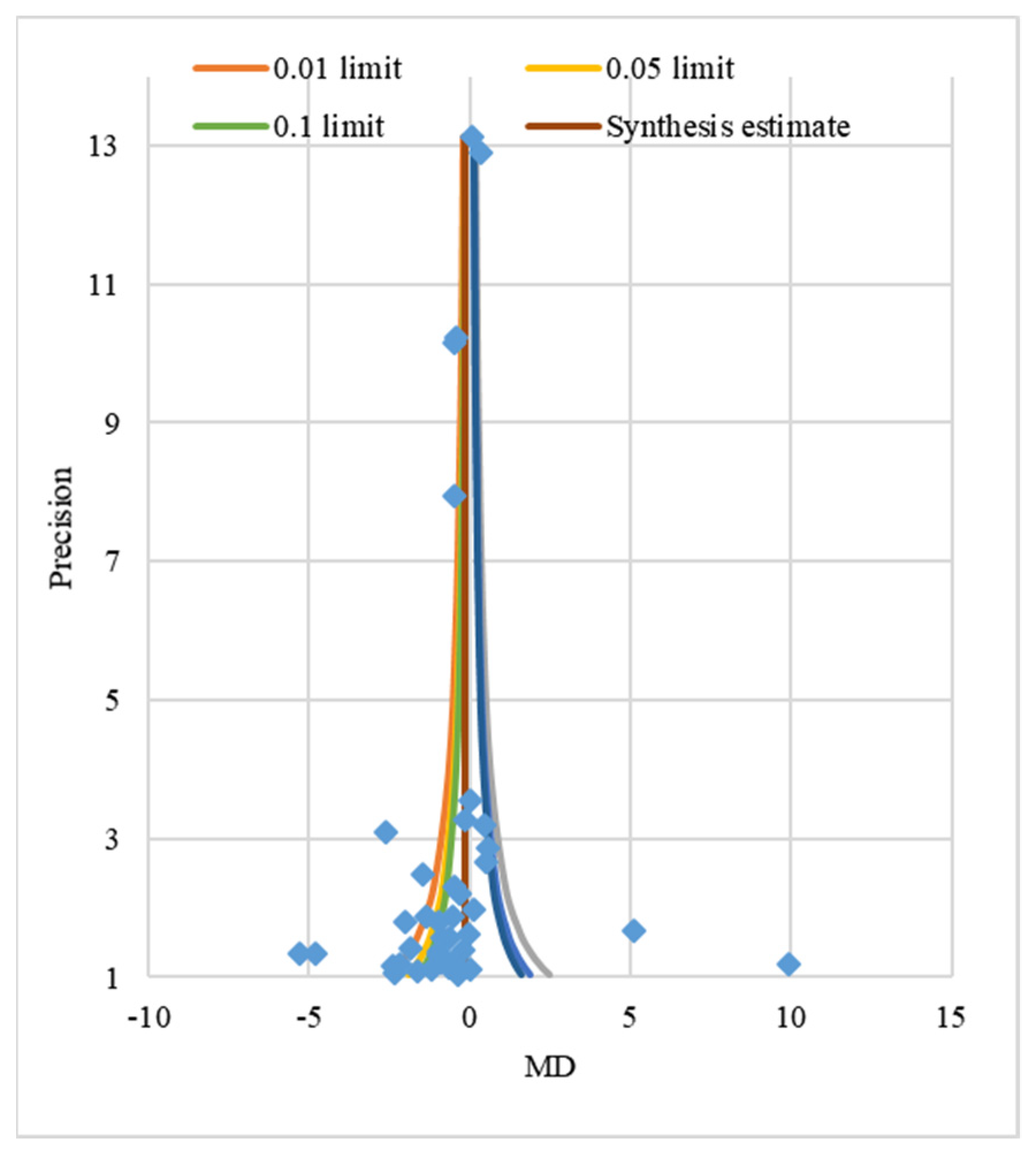
3.5. Publication Bias Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Curtis, S.; Wingert, A.; Ali, S. The Cochrane Library and Procedural Pain in Children: An Overview of Reviews. Evid. Based Child Health A Cochrane Rev. J. 2012, 7, 1363–1399. [Google Scholar] [CrossRef]
- Petovello, K. Pediatric Procedural Pain Management: A Review of the Literature. Int. J. Child Youth Fam. Stud. 2012, 3, 569–589. [Google Scholar] [CrossRef]
- Czarnecki, M.L.; Turner, H.N.; Collins, P.M.; Doellman, D.; Wrona, S.; Reynolds, J. Procedural Pain Management: A Position Statement with Clinical Practice Recommendations. Pain Manag. Nurs. 2011, 12, 95–111. [Google Scholar] [CrossRef] [PubMed]
- Taddio, A.; Ipp, M.; Thivakaran, S.; Jamal, A.; Parikh, C.; Smart, S.; Sovran, J.; Stephens, D.; Katz, J. Survey of the Prevalence of Immunization Non-Compliance due to Needle Fears in Children and Adults. Vaccine 2012, 30, 4807–4812. [Google Scholar] [CrossRef] [Green Version]
- Koller, D.; Goldman, R.D. Distraction Techniques for Children Undergoing Procedures: A Critical Review of Pediatric Research. J. Pediatr. Nurs. 2012, 27, 652–681. [Google Scholar] [CrossRef]
- Blount, R.L.; Piira, T.; Cohen, L.L.; Cheng, P.S. Pediatric Procedural Pain. Behav. Modif. 2006, 30, 24–49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Birnie, K.A.; Noel, M.; Parker, J.A.; Chambers, C.T.; Uman, L.S.; Kisely, S.R.; McGrath, P.J. Systematic Review and Meta-Analysis of Distraction and Hypnosis for Needle-Related Pain and Distress in Children and Adolescents. J. Pediatr. Psychol. 2014, 39, 783–808. [Google Scholar] [CrossRef] [Green Version]
- Buscemi, N.; Vandermeer, B.; Curtis, S. The Cochrane Library and Procedural Pain in Children: An Overview of Reviews. Evid.-Based Child Health A Cochrane Rev. J. 2008, 3, 260–279. [Google Scholar] [CrossRef]
- Birnie, K.A.; Noel, M.; Chambers, C.T.; Uman, L.S.; Parker, J.A. Psychological Interventions for Needle-related Procedural Pain and Distress in Children and Adolescents. Cochrane Database Syst. Rev. 2018. [Google Scholar] [CrossRef]
- Noel, M.; McMurtry, C.M.; Chambers, C.T.; McGrath, P.J. Children’s Memory for Painful Procedures: The Relationship of Pain Intensity, Anxiety, and Adult Behaviors to Subsequent Recall. J. Pediatr. Psychol. 2009, 35, 626–636. [Google Scholar] [CrossRef] [Green Version]
- Cummings, E.A.; Reid, G.J.; Finley, G.A.; McGrath, P.J.; Ritchie, J.A. Prevalence and Source of Pain in Pediatric Inpatients. Pain 1996, 68, 25–31. [Google Scholar] [CrossRef]
- Kazak, A.E. Comprehensive Care for Children with Cancer and their Families: A Social Ecological Framework Guiding Research, Practice, and Policy. Child. Serv. Soc. Policy Res. Pract. 2001, 4, 217–233. [Google Scholar] [CrossRef]
- Cramton, R.E.; Gruchala, N.E. Managing Procedural Pain in Pediatric Patients. Curr. Opin. Pediatr. 2012, 24, 530–538. [Google Scholar] [CrossRef]
- Casey, G. Pain-the Fifth Vital Sign. Kai Tiaki Nurs. N. Z. 2011, 17, 24. [Google Scholar]
- Erdoğan, Ç.; Turan, T.; Pınar, B. The Effect of Maternal Voice for Procedural Pain in Paediatric Intensive Care Unit: A Randomised Controlled Trial. Intensive Crit. Care Nurs. 2020, 56, 102767. [Google Scholar] [CrossRef] [PubMed]
- Stinson, J.; Yamada, J.; Dickson, A.; Lamba, J.; Stevens, B. Review of Systematic Reviews on Acute Procedural Pain in Children in the Hospital Setting. Pain Res. Manag. 2008, 13, 465891. [Google Scholar] [CrossRef]
- Uman, L.S.; Chambers, C.T.; McGrath, P.J.; Kisely, S. A Systematic Review of Randomized Controlled Trials Examining Psychological Interventions for Needle-Related Procedural Pain and Distress in Children and Adolescents: An Abbreviated Cochrane Review. J. Pediatr. Psychol. 2008, 33, 842–854. [Google Scholar] [CrossRef] [PubMed]
- Kleiber, C.; McCarthy, A.M. Evaluating Instruments for a Study on Children’s Responses to a Painful Procedure when Parents are Distraction Coaches. J. Pediatr. Nurs. 2006, 21, 99–107. [Google Scholar] [CrossRef]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [Green Version]
- Littell, J.H.; Corcoran, J.; Pillai, V. Systematic Reviews and Meta-Analysis; Oxford University Press: Oxford, UK, 2008. [Google Scholar]
- JBI. Checklist for Case Control Studies. Available online: https://jbi.global/critical-appraisal-tools (accessed on 21 November 2020).
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.; Rothstein, H.R. Introduction to Meta-Analysis; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2011. [Google Scholar]
- Mavridis, D.; Salanti, G. How to assess publication bias: Funnel plot, trim-and-fill method and selection models. Evid. Based Ment. Health 2014, 17, 30. [Google Scholar] [CrossRef]
- Lakens, D. Calculating and Reporting Effect Sizes to Facilitate Cumulative Science: A Practical Primer for T-Tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef] [Green Version]
- Bell, A.; Fairbrother, M.; Jones, K. Fixed and Random Effects Models: Making an Informed Choice. Qual. Quant. 2019, 53, 1051–1074. [Google Scholar] [CrossRef] [Green Version]
- Im, E.S.; Kim, J.S. Distraction Techniques for Children Undergoing Procedures: A Critical Review of Korean Intervention Research. Child Health Nurs. Res. 2014, 20, 340–349. [Google Scholar] [CrossRef]
- Beran, T.N.; Ramirez-Serrano, A.; Vanderkooi, O.G.; Kuhn, S. Reducing Children’s Pain and Distress Towards Flu Vaccinations: A Novel and Effective Application of Humanoid Robotics. Vaccine 2013, 31, 2772–2777. [Google Scholar] [CrossRef] [PubMed]
- PLOS Medicine Editors. Observational Studies: Getting Clear about Transparency. PLoS Med. 2014, 11, e1001711. [Google Scholar] [CrossRef] [Green Version]
- Oermann, M.H.; Turner, K.; Carman, M. Preparing Quality Improvement, Research, and Evidence-Based Practice Manuscripts. Nurs. Econ. 2014, 32, 57. [Google Scholar]
- Moadad, N.; Kozman, K.; Shahine, R.; Ohanian, S.; Badr, L.K. Distraction using the BUZZY for Children during an IV Insertion. J. Pediatr. Nurs. 2016, 31, 64–72. [Google Scholar] [CrossRef]



| Study ID | Author (Year) | Country | Center | Procedure (Sample Size) | Age (Year) | IRB | Fund | Design | Type of Intervention (Characteristics) | Control | Outcome | Quality Assessment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Canbulat et al. (2014) | Turkey | 1 hospital | Phlebotomy (n = 126), E: 63, C: 63 | 7–11 (8.8 ± 1.5) | Yes | Yes | RCT | Visual distraction (distraction cards) | No intervention | Pain: WB-FACES, Anxiety: CFS | 9 |
| 2 | Canbulat et al. (2014) | Turkey | 1 hospital | Phlebotomy (n= 125), E: 62, C: 63 | 7–11 (8.8 ± 1.5) | Yes | Yes | RCT | Visual distraction (Kaleidoscope) | No intervention | Pain: WB-FACES (0–10), Anxiety: CFS (0–4) | 9 |
| 3 | Hsieh et al. (2017) | Taiwan | 1 hospital | IV (n = 68), E: 35, C: 33 | 6–12 (E:8.3 ± 1.6, C:7.8 ± 1.5) | Yes | No | Quasi | Cognitive-behavioral program (pre: Educational photo book 10–15 min, during: Favorite music video 5–10 min (40–60 dB)) | Routine care | Pain: NRS (0–10) | 9 |
| 4 | Rimon et al. (2016) | Israel | 1 hospital | IV (n = 53), E: 29, C: 24 | 2–15 (E:5.6 ± 2.8, C:6.9 ± 3.4) | No | Yes | RCT | Medical clown (pre: Distraction via humor, during: Distraction via humor 15 min) | Parent regular distraction and comfort | Pain: VAS, FPS-R, S-cortisol | 7 |
| 5 | Kuo et al. (2016) | Taiwan | 1 medical center | IV (n = 184), E: 92, C: 92 | 3–7 (E:4.5, C: 4.51) | Yes | No | RCT | Visual distraction (story book reading) | Oral instruction | OSBD-R (1–4) | 8 |
| 6 | Kuo et al. (2016) | Taiwan | 1 medical center | IV (n = 184), E: 92, C: 92 | 3–7 (E:4.5, C:4.51) | Yes | No | RCT | Visual distraction (cartoon viewing (iPad)) | Oral instruction | OSBD-R (1–4) | 8 |
| 7 | Sahiner and Bal (2016) | Turkey | 1 hospital | Phlebotomy (n = 60), E: 30, C: 30 | 6–12 (9.1 ± 1.6) | Yes | No | RCT | Visual distraction (distraction cards) | Routine care | Pain: WB-FACES, Anxiety: CFS | 11 |
| 8 | Sahiner and Bal (2016) | Turkey | 1 hospital | 60 children for Phlebotomy (n = 60), E: 30, C: 30 | 6–12 (9.1 ± 1.6) | Yes | No | RCT | Audial distraction (music playback) | Routine care | Pain: WB-FACES, Anxiety: CFS | 11 |
| 9 | Sahiner and Bal (2016) | Turkey | 1 hospital | Phlebotomy (n = 60), E: 30, C: 30 | 6–12 (9.1 ± 1.6) | Yes | No | RCT | Touch distraction (balloon inflation) | Routine care | Pain: WB-FACES, Anxiety: CFS | 11 |
| 10 | Miller et al. (2016) | Australia | 1 hospital | IV (n = 40), E: 20, C: 20 | 3–12 (E:8.1 ± 3.0, C:7.0 ± 2.3) | Yes | No | RCT | Visual distraction (PSP: Sony handheld PSP, age- appropriate games) | Standard distraction | Pain: WB-FACES, VAS (0–10), FLACC (0–10) | 11 |
| 11 | Miller et al. (2016) | Australia | 1 hospital | IV (n = 40), E: 20, C: 20 | 3–12 (E:8.1 ± 3.0, C:6.4 ± 2.9) | Yes | No | RCT | Multisensory stimuli (animated visual content, sound) and vibration; Ditto-D: PSP + interactive games) | Standard distraction | Pain: WB-FACES, VAS (0–10), FLACC (0–10) | 11 |
| 12 | Miller et al. (2016) | Australia | 1 hospital | IV (n = 39), E: 19, C: 20 | 3–12 (E: 8.1 ± 3.0, C: 6.2 ± 2.8) | Yes | No | RCT | Multisensory stimuli (animated visual content, sound) and vibration; Ditto-PP: interactive procedural preparation story) | Standard distraction | Pain: WB-FACES, VAS (0–10), FLACC (0–10) | 11 |
| 13 | Miller et al. (2016) | Australia | 1 hospital | IV (n = 39), E: 19, C: 20 | 3–12 (E:8.1 ± 3.0, C:6.0 ± 2.3) | Yes | No | RCT | Multisensory stimuli (animated visual content, sound) and vibration; Ditto-C: story + interactive stories and games) | Standard distraction | Pain: WB-FACES, VAS (0–10), FLACC (0–10) | 11 |
| 14 | Sadeghi et al. (2018) | Iran | 1 hospital | IV (n = 60), E: 30, C: 30 | 4-6 | No | Yes | Quasi | Touch distraction (press a soft ball with the opposite hand | No intervention | Pain: WB-FACES | 7 |
| 15 | Aydin et al. (2016) | Turkey | 1 hospital | Phlebotomy (n = 60), E: 30, C: 30 | 7–12 (E:9.3 ± 1.8, C:9.9 ± 2.0) | Yes | No | RCT | Visual distraction (distraction cards) | Routine care | Pain: WB-FACES, Anxiety: CFS | 9 |
| 16 | Aydin et al. (2016) | Turkey | 1 hospital | Phlebotomy (n = 60), E: 30, C: 30 | 7–12 (E:9.7 ± 2.2, C:9.9 ± 2.0) | Yes | No | RCT | Touch distraction (soft ball) | Routine care | Pain: WB-FACES, Anxiety: CFS | 9 |
| 17 | Aydin et al. (2016) | Turkey | 1 hospital | Phlebotomy (n = 60), E: 30, C: 30 | 7–12 (E:9.7 ± 2.4, C:9.9 ± 2.0) | Yes | No | RCT | Touch distraction (balloon inflation) | Routine care | Pain: WB-FACES, Anxiety: CFS | 9 |
| 18 | Pour et al. (2017) | Iran | 2 hospital | Phlebotomy (n = 80), E: 40, C: 40 | 6–12 (8.0 ± 1.8) | Yes | No | RCT | Local anesthesia (2g EMLA cream, 45 min) | Routine care | Pain: FLACC (0–10) | 8 |
| 19 | Pour et al. (2017) | Iran | 2 hospital | Phlebotomy (n = 80), E: 40, C: 40 | 6–12 (8.0 ± 1.8) | Yes | No | RCT | Acupressure (Yintang (extra 1) and Laogong (P-8)) | Routine care | Pain: FLACC (0–11) | 8 |
| 20 | McCarthy et al. (2014) | USA | 3 hospitals | IV (n = 232), E: 116, C: 116 | 4–10 (7.3 ± 1.9) | Yes | Yes | RCT | Visual distraction (enhanced: RA distraction coaching) | Patent directed distraction | Pain: Oucher (0–10), PRCD (1–7), OSBD-R (1–4), Salivary cortisol | 8 |
| 21 | McCarthy et al. (2014) | USA | 3 hospitals | IV (n = 240), E: 124, C: 116 | 4–10 (7.3 ± 1.9) | Yes | Yes | RCT | Visual distraction (professional: RA distraction support) | Patent directed distraction | Pain: 23 Oucher 24 (0–10), PRCD25 (1–7), OSBD-26R (1–4), Salivary cortisol | 8 |
| 22 | Hillgrove-Stuart et al. (2013) | Canada | 1 clinic | IV (n = 66), E: 32, C: 34 | 1–2 (1.3 ± 0.2) | Yes | Yes | RCT | Touch distraction (parent directed distraction) | Routine care | Pain: M29BPS (0–10), 30MAISD | 11 |
| 23 | Hillgrove-Stuart et al. (2013) | Canada | 1 clinic | IV (n = 67), E: 33, C: 34 | 1–2 (1.3 ± 0.2) | Yes | Yes | RCT | Touch distraction (RA directed distraction) | Routine care | Pain: MBPS (0–10), MAISD | 11 |
| 24 | Cohen et al. (2015) | USA | 1 hospital | Immunization (n = 60), E: 30, C: 30 | 4–6.5 (4.8 ± 0.8) | Yes | Yes | RCT | Visual distraction (age- appropriate movie+ parent teaching program) | Routine care | Pain: CAPS, parent knowledge, parent behavior, children behavior | 11 |
| 25 | Cohen et al. (2015) | USA | 1 hospital | Immunization (n = 60), E: 30, C: 30 | 4–6.5 (4.8 ± 0.8) | Yes | Yes | RCT | Visual distraction+ education (age-appropriate movie) | Routine care | Pain: CAPS, parent knowledge, parent behavior, children behavior | 11 |
| 26 | Inal and Kelleci (2012) | Turkey | 1 hospital | IV (n = 123), E: 61, C: 62 | 6–12 (E:9.4 ± 2.1, C:9.3 ± 1.8) | Yes | No | RCT | Visual distraction (distraction cards) | Routine care | Pain: CAPS (0–5), FPS (0–10), anxiety | 12 |
| 27 | Jibb et al. (2018) | Canada | 1 hospital | SCP needle insertion for chemo (EMLA 60 min) (n = 39), E: 18, C: 21 | 4–9 (E:6.3 ± 1.4, C:6.1 ± 1.5) | Yes | Yes | RCT | Web-based service cognitive-behavioral program (MEDiPORT humanoid robot) | Active distraction robot with dancing and singing | Pain: FPS, NRS (0–10), fear: CFS (0–10), distress: BAADS (1–5) | 9 |
| 28 | Kristja and Kristja (2011) | Canada | 1 school | Immunization (n = 77), E: 38, C: 39 | 13–15 (14 ± 0.18) | Yes | No | RCT | Audial distraction (musical distraction: With headphone) | Standard care | Pain: VAS (0–10), anxiety, fear (0–10) | 7 |
| 29 | Kristja and Kristja (2011) | Canada | 1 school | Immunization (n = 80), E: 41, C: 39 | 13–15 (14 ± 0.18) | Yes | No | RCT | Audial distraction (musical distraction: without headphone) | Standard care | Pain: VAS (0–10), anxiety, fear (0–10) | 7 |
| 30 | Nilsson et al. (2015) | Sweden | 3 school | HPV vaccination (n = 37), E: 37, C: 37 | 11–12 | Yes | Yes | Crossover RCT | Visual distraction (relaxation and guided imagery) | Standard care | Pain: CAS (0–10), FAS (0.04–0.97), salivary cortisol | 10 |
| 31 | Oliveira et al. (2016) | Brazil | 1 hospital | IV (n = 40), E: 22, C: 18 | 6–12 (E:8.3 ± 2.1, C:8.7 ± 1.8) | Yes | No | Crossover RCT | Audiovisual distraction (Disney movie) | Routine care | Pain: VAS (0–10), FPS (0–10), PCS-C (13 item, 1–5), CSS (35 item, 0–4) | 8 |
| 32 | Hartling et al. (2013) | Canada | 1 hospital | IV (n = 42), E: 21, C: 21 | 3–11 | Yes | Yes | RCT | Audial distraction (musical distraction: with headphone) | Standard care | Pain: FPS-R (0–10), OSBD-R, anxiety | 10 |
| 33 | Redfern et al. (2018) | USA | 1 hospital | Vaccination (n = 50), E: 25, C: 25 | 3–18 (E:10.7 ± 4.7, C:10.5 ± 4.7) | Yes | No | RCT | Visual distraction (distraction cards) | No intervention | Pain: WB-FACES, parent satisfaction (0–10) | 12 |
| 34 | Risaw et al. (2017) | India | 1 hospital | Phlebotomy (n = 210), E: 105, C: 105 | 4–6 (4.8 ± 0.8) | Yes | No | RCT | Visual distraction (distraction cards) | Standard care | Pain: FLACC (0–10) | 10 |
| 35 | Bergomi et al. (2018) | Italy | 1 hospital | IV (n = 75), E: 36, C: 39 | 5–12 (E:8.3 ± 2.2, C:9.4 ± 2.3) | Yes | No | RCT | Touch distraction (BUZZY device) | Standard care | Pain: WB-FPS, CEMS, parent anxiety: NRS (0–10) | 7 |
| 36 | Bergomi et al. (2018) | Italy | 1 hospital | IV (n = 76), E: 37, C: 39 | 5–12 (E:9.4 ± 2.0, C:9.4 ± 2.3) | Yes | No | RCT | Visual distraction (cartoon) | Standard care | Pain: WB-FPS, CEMS, parent anxiety: NRS (0–10) | 7 |
| 37 | Bergomi et al. (2018) | Italy | 1 hospital | IV (n = 77), E: 38, C: 39 | 5–12 (E:8.6 ± 2.1, C:9.4 ± 2.3) | Yes | No | RCT | Touch distraction (BUZZY device + cartoon) | Standard care | Pain: WB-FPS, CEMS, parent anxiety: NRS (0–10) | 7 |
| 38 | Meiri et al. (2016) | Israel | 1 hospital | IV (n = 66), E: 33, C: 33 | 2–10 (E:5.4 ± 2.6, C:5.5 ± 2.6) | Yes | Yes | RCT | Medical clown (medical clown) | Standard care | Pain: VAS (0–10), anxiety (0–10), crying time | 7 |
| 39 | Meiri et al. (2016) | Israel | 1 hospital | IV (n = 67), E: 34, C: 33 | 2–10 (E:5.0 ± 2.4, C:5.5 ± 2.6) | Yes | Yes | RCT | Local anesthesia (EMLA cream, 50min) | Standard care | Pain: VAS (0–10), anxiety (0–10), crying time | 7 |
| 40 | Karakaya and Duygu G€ozen (2016) | Turkey | 1 hospital | IV (n = 144), E: 72, C: 72 | 7–12 | Yes | No | RCT | Visual distraction (kaleidoscope) | No intervention | Pain: FPS (0–10), pulse oximeter, thermometer | 7 |
| 41 | Cerne et al. (2014) | Italy | 1hospital | Immunization (n = 35), E: 18, C: 17 | 6 | Yes | No | RCT | Audiovisual distraction (cartoon movie) | Standard care | Pain: WB-FACES Distress: OSBD-A | 8 |
| 42 | Vagnoli et al. (2015) | Italy | 1hospital | Phlebotomy (n = 50), E: 25, C: 25 | 4–11 (E:7.1 ± 1.8, C:7.38 ± 2.5) | Yes | No | RCT | Visual distraction (dog presence) | Standard care | Pain: WB-FACES Distress: OSBD-A | 10 |
| 43 | Singh (2012) | India | 1hospital | Immunization (n = 60), E: 30, C: 30 | 1.5–2 | No | No | Quasi | Touch distraction (toy) | Standard care | Pain: FLACC (0–10) | 5 |
| 44 | Singh (2012) | India | 1hospital | Immunization (n = 60), E: 30, C: 30 | 1.5–2 | No | No | Quasi | Audial distraction (musical distraction) | Standard care | Pain: FLACC (0–10) | 5 |
| 45 | Minute et al. (2012) | Italy | 1hospital | Immunization (n = 97), E: 47, C: 50 | 4–10 (median: 7) | Yes | No | RCT | Visual distraction (Wii videogame+ EMLA cream) | EMLA cream | Pain: FLACC (0–10), FPS-R | 9 |
| Characteristics | Subgroup | K | N | Overall ES | 95% CI | Z (p) | I2 (%) | |
|---|---|---|---|---|---|---|---|---|
| Lower Limit | Upper Limit | |||||||
| Age (year) | <10 | 15 | 1419 | 0.27 | −0.18 | 0.73 | 1.17 (0.242) | 95.4 |
| ≥10 | 26 | 1761 | −1.07 | −1.60 | −0.53 | −3.92 (<0.001) | 85.3 | |
| Center | One | 38 | 2671 | −0.51 | −0.85 | −0.17 | −2.96 (0.003) | 92.7 |
| Multi-center | 3 | 509 | −0.43 | −0.96 | 0.09 | −1.61 (0.108) | 0.0 | |
| IRB | No | 4 | 233 | 1.97 | −4.31 | 8.25 | 0.61 (0.539) | 98.7 |
| Yes | 37 | 2947 | −0.64 | −0.89 | −0.39 | −5.04 (<0.001) | 84.9 | |
| Fund | Yes | 15 | 1340 | −0.83 | −1.20 | −0.46 | −4.41 (<0.001) | 90.5 |
| No | 26 | 1840 | −0.18 | −0.84 | 0.47 | −0.55 (0.581) | 93.0 | |
| Study design | RCT | 37 | 2932 | −0.61 | −0.92 | −0.30 | −3.85 (<0.001) | 91.3 |
| Quasi-E | 4 | 248 | 0.94 | −3.60 | 5.48 | 0.40 (0.685) | 96.9 | |
| Type of intervention | Audial | 7 | 394 | −0.38 | −2.10 | 1.33 | −0.44 (0.661) | 94.9 |
| Visual | 17 | 1790 | −0.76 | −1.15 | −0.37 | −3.86 (<0.001) | 89.6 | |
| Clown | 2 | 119 | −3.64 | −4.76 | −2.52 | −6.36 (<0.001) | 91.9 | |
| Cognitive | 2 | 107 | −0.47 | −1.64 | 0.70 | −0.79 (0.428) | 0.0 | |
| Multi methods | 12 | 703 | 0.31 | −0.35 | 0.97 | 0.92 (0.360) | 93.4 | |
| Local anesthesia | 1 | 67 | 0.67 | |||||
| Quality assessment score | <10 | 24 | 2077 | −0.35 | −1.16 | 0.46 | −0.84 (0.400) | 93.6 |
| ≥10 | 17 | 1103 | −0.65 | −0.98 | −0.32 | −3.84 (<0.001) | 89.3 | |
| Variables | K | N | Overall ES | 95% CI | Z (p) | I2 (%) | |
|---|---|---|---|---|---|---|---|
| Lower Limit | Upper Limit | ||||||
| Observer pain (parent) | 23 | 1891 | −0.40 | −1.26 | 0.45 | −0.93 (0.355) | 94.1 |
| Observer pain (nurse) | 28 | 2173 | 1.43 | −1.96 | 4.82 | 0.83 (0.408) | 99.7 |
| Child-reported anxiety | 3 | 207 | −0.33 | −1.27 | 0.62 | −0.68 (0.496) | 0.0 |
| Observer anxiety (parent) | 15 | 1163 | −0.68 | −1.13 | −0.23 | −2.96 (0.003) | 85.9 |
| Observer anxiety (nurse) | 14 | 1330 | −1.03 | −1.67 | −0.40 | −3.20 (0.001) | 94.0 |
| Cortisol | 5 | 340 | −1.11 | −2.09 | −0.12 | −2.20 (0.274) | 66.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, M.-K.; Choi, M.-Y. Effect of Distraction Intervention for Needle-Related Pain and Distress in Children: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 9159. https://doi.org/10.3390/ijerph18179159
Cho M-K, Choi M-Y. Effect of Distraction Intervention for Needle-Related Pain and Distress in Children: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2021; 18(17):9159. https://doi.org/10.3390/ijerph18179159
Chicago/Turabian StyleCho, Mi-Kyoung, and Mi-Young Choi. 2021. "Effect of Distraction Intervention for Needle-Related Pain and Distress in Children: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 18, no. 17: 9159. https://doi.org/10.3390/ijerph18179159
APA StyleCho, M.-K., & Choi, M.-Y. (2021). Effect of Distraction Intervention for Needle-Related Pain and Distress in Children: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 18(17), 9159. https://doi.org/10.3390/ijerph18179159






