An In Vitro Analysis on Polyurethane Foam Blocks of the Insertion Torque (IT) Values, Removal Torque Values (RTVs), and Resonance Frequency Analysis (RFA) Values in Tapered and Cylindrical Implants
Abstract
:1. Introduction
2. Materials and Methods
2.1. Implants Characteristics
- -
- Group I: Cylindrical implants (Cyroth, AoN Implants, Grisignano di Zocco, VI, Italy) with 4 mm diameter and 10 mm length;
- -
- Group II: Tapered implants (Is-Four, AoN Implants, Grisignano di Zocco, VI, Italy) with 4.20 mm diameter and 10 mm length.
2.2. Polyurethane Foam Blocks
- -
- 10 pounds per cubic foot (PCF) polyurethane density without a cortical layer;
- -
- 10 pounds per cubic foot (PCF) polyurethane density with a 1-mm cortical layer (30 PCF);
- -
- 20 pounds per cubic foot (PCF) polyurethane density without a cortical layer;
- -
- 20 pounds per cubic foot (PCF) polyurethane density with a 1-mm cortical layer (30 PCF).
2.3. Implant Site Drilling Protocol
2.4. Primary Stability Assessment
2.5. Statistical Analysis
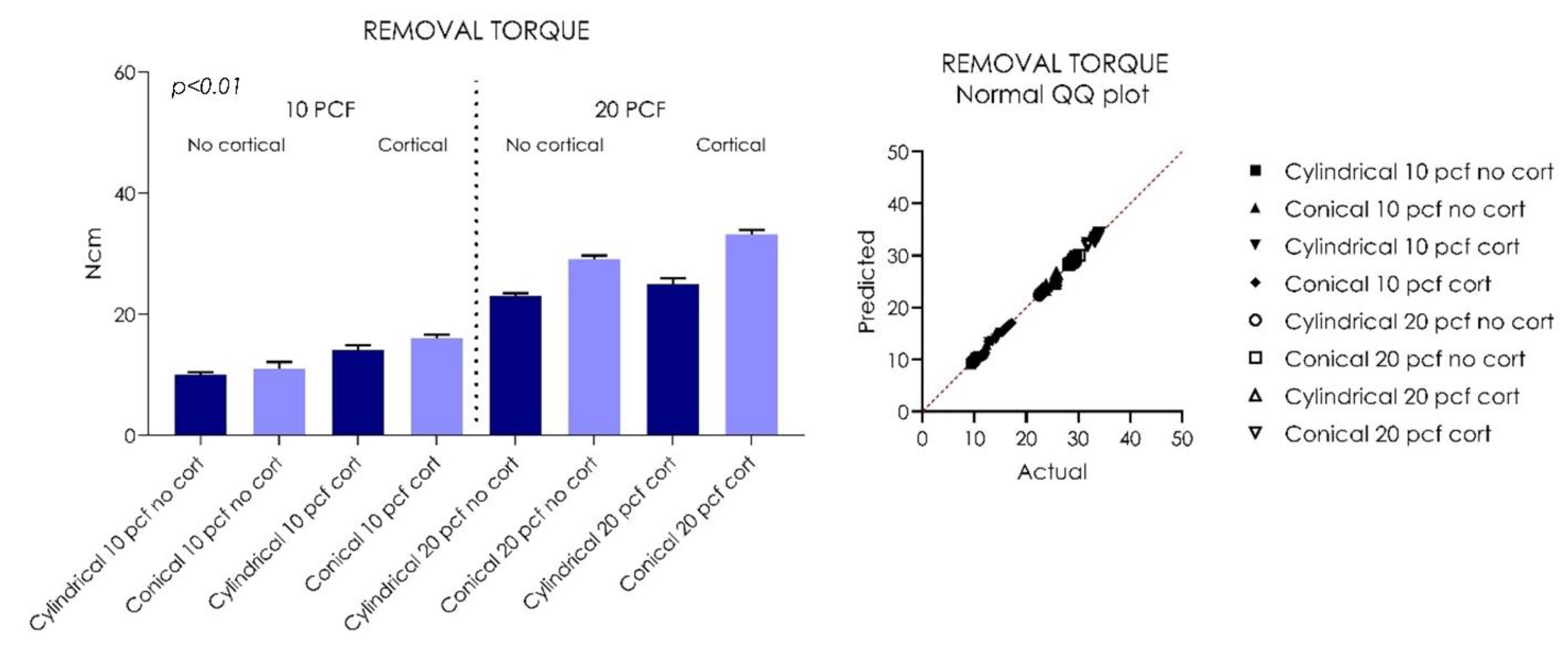
3. Results
3.1. 10 PCF Artificial Bone Density
3.2. 20 PCF Artificial Bone Density
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Atieh, M.A.; Alsabeeha, N.; Duncan, W.J. Stability of Tapered and Parallel-Walled Dental Implants: A Systematic Review and Meta-Analysis. Clin. Implant. Dent. Relat. Res. 2018, 20, 634–645. [Google Scholar] [CrossRef] [PubMed]
- Wilson, T.G., Jr.; Miller, R.J.; Trushkowsky, R.; Dard, M. Tapered Implants in Dentistry: Revitalizing Concepts with Technology: A Review. Adv. Dent. Res. 2016, 28, 4–9. [Google Scholar] [CrossRef]
- Zonfrillo, G.; Matteoli, S.; Ciabattini, A.; Dolfi, M.; Lorenzini, L.; Corvi, A. Analysis and Comparison of Clutch Techniques of Two Dental Implants. J. Mech. Behav. Biomed. Mater. 2014, 34, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Sierra-Rebolledo, A.; Allais-Leon, M.; Maurette-O’Brien, P.; Gay-Escoda, C. Primary Apical Stability of Tapered Implants Through Reduction of Final Drilling Dimensions in Different Bone Density Models: A Biomechanical Study. Implant. Dent. 2016, 25, 775–782. [Google Scholar] [CrossRef]
- Waechter, J.; Leite, F.R.; Nascimento, G.G.; Filho, L.C.C.; Faot, F. The Split Crest Technique and Dental Implants: A Systematic Review and Meta-Analysis. Int. J. Oral. Maxillofac. Surg. 2017, 46, 116–128. [Google Scholar] [CrossRef]
- Möhlhenrich, S.C.; Kniha, K.; Heussen, N.; Hölzle, F.; Modabber, A. Effects on Primary Stability of Three Different Techniques for Implant Site Preparation in Synthetic Bone Models of Different Densities. Br. J. Oral Maxillofac. Surg. 2016, 54, 980–986. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Serrano, J.; Ortega-Aranegui, R.; Lopez-Quiles, J. In Vitro Comparison of Primary Stability of Two Implant Designs in D3 Bone. Med. Oral Patol. Oral Cir. Bucal 2017, 22, e473–e477. [Google Scholar] [CrossRef] [PubMed]
- Möhlhenrich, S.C.; Heussen, N.; Elvers, D.; Steiner, T.; Hölzle, F.; Modabber, A. Compensating for Poor Primary Implant Stability in Different Bone Densities by Varying Implant Geometry: A Laboratory Study. Int. J. Oral Maxillofac. Surg. 2015, 44, 1514–1520. [Google Scholar] [CrossRef]
- Herrero-Climent, M.; Lemos, B.F.; Herrero-Climent, F.; Falcao, C.; Oliveira, H.; Herrera, M.; Gil, F.J.; Ríos-Carrasco, B.; Ríos-Santos, J.-V. Influence of Implant Design and Under-Preparation of the Implant Site on Implant Primary Stability. An In Vitro Study. Int. J. Environ. Res. Public Health 2020, 17, 4436. [Google Scholar] [CrossRef]
- Waechter, J.; de Matos Madruga, M.; do Carmo Filho, L.C.; Leite, F.R.M.; Schinestsck, A.R.; Faot, F. Comparison between Tapered and Cylindrical Implants in the Posterior Regions of the Mandible: A Prospective, Randomized, Split-Mouth Clinical Trial Focusing on Implant Stability Changes during Early Healing. Clin. Implant. Dent. Relat. Res. 2017, 19, 733–741. [Google Scholar] [CrossRef]
- Romanos, G.E.; Delgado-Ruiz, R.A.; Sacks, D.; Calvo-Guirado, J.L. Influence of the Implant Diameter and Bone Quality on the Primary Stability of Porous Tantalum Trabecular Metal Dental Implants: An in Vitro Biomechanical Study. Clin. Oral Implant. Res. 2018, 29, 649–655. [Google Scholar] [CrossRef] [PubMed]
- Staedt, H.; Palarie, V.; Staedt, A.; Wolf, J.M.; Lehmann, K.M.; Ottl, P.; Kämmerer, P.W. Primary Stability of Cylindrical and Conical Dental Implants in Relation to Insertion Torque-A Comparative Ex Vivo Evaluation. Implant. Dent. 2017, 26, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Attanasio, F.; Antonelli, A.; Brancaccio, Y.; Averta, F.; Figliuzzi, M.M.; Fortunato, L.; Giudice, A. Primary Stability of Three Different Osteotomy Techniques in Medullary Bone: An in Vitro Study. Dent. J. 2020, 8, 21. [Google Scholar] [CrossRef] [Green Version]
- Giudice, A.; Bennardo, F.; Antonelli, A.; Barone, S.; Wagner, F.; Fortunato, L.; Traxler, H. Influence of Clinician’s Skill on Primary Implant Stability with Conventional and Piezoelectric Preparation Techniques: An Ex-Vivo Study. J. Biol. Regul. Homeost. Agents 2020, 34, 739–745. [Google Scholar] [CrossRef] [PubMed]
- Antonelli, A.; Bennardo, F.; Brancaccio, Y.; Barone, S.; Femiano, F.; Nucci, L.; Minervini, G.; Fortunato, L.; Attanasio, F.; Giudice, A. Can Bone Compaction Improve Primary Implant Stability? An In Vitro Comparative Study with Osseodensification Technique. Appl. Sci. 2020, 10, 8623. [Google Scholar] [CrossRef]
- Toyoshima, T.; Tanaka, H.; Ayukawa, Y.; Howashi, M.; Masuzaki, T.; Kiyosue, T.; Koyano, K.; Nakamura, S. Primary Stability of a Hybrid Implant Compared with Tapered and Cylindrical Implants in an Ex Vivo Model. Clin. Implant. Dent. Relat. Res. 2015, 17, 950–956. [Google Scholar] [CrossRef]
- Falco, A.; Berardini, M.; Trisi, P. Correlation Between Implant Geometry, Implant Surface, Insertion Torque, and Primary Stability: In Vitro Biomechanical Analysis. Int. J. Oral Maxillofac. Implant. 2018, 33, 824–830. [Google Scholar] [CrossRef]
- Tumedei, M.; Piattelli, A.; Falco, A.; De Angelis, F.; Lorusso, F.; Di Carmine, M.; Iezzi, G. An In Vitro Evaluation on Polyurethane Foam Sheets of the Insertion Torque, Removal Torque Values, and Resonance Frequency Analysis (RFA) of a Self-Tapping Threads and Round Apex Implant. Cell. Polym. 2021, 40, 20–30. [Google Scholar] [CrossRef]
- Gehrke, S.A.; Tumedei, M.; Aramburú Júnior, J.; Treichel, T.L.E.; Kolerman, R.; Lepore, S.; Piattelli, A.; Iezzi, G. Histological and Histomorphometrical Evaluation of a New Implant Macrogeometry. A Sheep Study. Int. J. Environ. Res. Public Health 2020, 17, 3477. [Google Scholar] [CrossRef]
- Comuzzi, L.; Tumedei, M.; Pontes, A.E.; Piattelli, A.; Iezzi, G. Primary Stability of Dental Implants in Low-Density (10 and 20 Pcf) Polyurethane Foam Blocks: Conical vs. Cylindrical Implants. Int. J. Environ. Res. Public Health 2020, 17, 2617. [Google Scholar] [CrossRef] [Green Version]
- Comuzzi, L.; Tumedei, M.; Piattelli, A.; Iezzi, G. Short vs. Standard Length Cone Morse Connection Implants: An In Vitro Pilot Study in Low Density Polyurethane Foam. Symmetry 2019, 11, 1349. [Google Scholar] [CrossRef] [Green Version]
- Fanali, S.; Tumedei, M.; Pignatelli, P.; Inchingolo, F.; Pennacchietti, P.; Pace, G.; Piattelli, A. Implant Primary Stability with an Osteocondensation Drilling Protocol in Different Density Polyurethane Blocks. Comput. Methods Biomech. Biomed. Eng. 2021, 24, 14–20. [Google Scholar] [CrossRef]
- ASTM F1839-01. Standard Specification for Rigid Polyurethane Foam for Use as a Standard Material for Testing Orthopedic Devices and Instruments; ASTM: West Conshohcken, PA, USA, 1839. [Google Scholar]
- Kotsu, M.; Velez, J.U.; Bengazi, F.; Tumedei, M.; Fujiwara, S.; Kato, S.; Botticelli, D. Healing at Implants Installed from ~ 70- to < 10-Ncm Insertion Torques: An Experimental Study in Dogs. Oral Maxillofac. Surg. 2021, 25, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Fujiwara, S.; Kato, S.; Bengazi, F.; Urbizo Velez, J.; Tumedei, M.; Kotsu, M.; Botticelli, D. Healing at Implants Installed in Osteotomies Prepared Either with a Piezoelectric Device or Drills: An Experimental Study in Dogs. Oral Maxillofac. Surg. 2021, 25, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Comuzzi, L.; Tumedei, M.; Piattelli, A.; Iezzi, G. Osseodensification Drilling vs. Standard Protocol of Implant Site Preparation: An In Vitro Study on Polyurethane Foam Sheets. Prosthesis 2020, 2, 76–86. [Google Scholar] [CrossRef]
- Matějka, L.; Špírková, M.; Dybal, J.; Kredatusová, J.; Hodan, J.; Zhigunov, A.; Šlouf, M. Structure Evolution during Order–Disorder Transitions in Aliphatic Polycarbonate Based Polyurethanes. Self-Healing Polymer. Chem. Eng. J. 2019, 357, 611–624. [Google Scholar] [CrossRef]
- Misch, C.E. Bone Density: A Key Determinant for Treatment Planning. In Contemporary Implant Dentistry, 3rd ed.; Mosby: St Louis, MO, USA, 2007; pp. 130–146. [Google Scholar]
- Jung, B.A.; Yildizhan, F.; Wehrbein, H. Bone-to-Implant Contact of Orthodontic Implants in Humans—A Histomorphometric Investigation. Eur. J. Orthod. 2008, 30, 552–557. [Google Scholar] [CrossRef] [Green Version]
- Jokstad, A.; Sanz, M.; Ogawa, T.; Bassi, F.; Levin, L.; Wennerberg, A.; Romanos, G.E. A Systematic Review of the Role of Implant Design in the Rehabilitation of the Edentulous Maxilla. Int. J. Oral Maxillofac. Implant. 2016, 31, s43–s99. [Google Scholar] [CrossRef]
- Marquezan, M.; Osório, A.; Sant’Anna, E.; Souza, M.M.; Maia, L. Does Bone Mineral Density Influence the Primary Stability of Dental Implants? A Systematic Review. Clin. Oral Implant. Res. 2012, 23, 767–774. [Google Scholar] [CrossRef]
- Comuzzi, L.; Iezzi, G.; Piattelli, A.; Tumedei, M. An In Vitro Evaluation, on Polyurethane Foam Sheets, of the Insertion Torque (IT) Values, Pull-Out Torque Values, and Resonance Frequency Analysis (RFA) of NanoShort Dental Implants. Polymers 2019, 11, 1020. [Google Scholar] [CrossRef] [Green Version]
- Neto, R.T.M.; Hiramatsu, D.A.; Suedam, V.; Conti, P.C.R.; Rubo, J.H. Validation of an Experimental Polyurethane Model for Biomechanical Studies on Implant-Supported Prosthesis–Compression Tests. J. Appl. Oral Sci. Rev. FOB 2011, 19, 47–51. [Google Scholar] [CrossRef] [Green Version]
- Arosio, P.; Greco, G.B.; Zaniol, T.; Iezzi, G.; Perrotti, V.; Di Stefano, D.A. Sinus Augmentation and Concomitant Implant Placement in Low Bone-Density Sites. A Retrospective Study on an Undersized Drilling Protocol and Primary Stability. Clin. Implant. Dent. Relat. Res. 2018, 20, 151–159. [Google Scholar] [CrossRef]
- Anitua, E.; Murias-Freijo, A.; Alkhraisat, M.H. Implant Site Under-Preparation to Compensate the Remodeling of an Autologous Bone Block Graft. J. Craniofacial Surg. 2015, 26, e374–e377. [Google Scholar] [CrossRef]
- Abuhussein, H.; Pagni, G.; Rebaudi, A.; Wang, H.-L. The Effect of Thread Pattern upon Implant Osseointegration. Clin. Oral Implant. Res. 2010, 21, 129–136. [Google Scholar] [CrossRef] [Green Version]
- Tumedei, M.; Piattelli, A.; Degidi, M.; Mangano, C.; Iezzi, G. A Narrative Review of the Histological and Histomorphometrical Evaluation of the Peri-Implant Bone in Loaded and Unloaded Dental Implants. A 30-Year Experience (1988–2018). Int. J. Environ. Res. Public Health 2020, 17, 2088. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tumedei, M.; Piattelli, A.; Degidi, M.; Mangano, C.; Iezzi, G. A 30-Year (1988–2018) Retrospective Microscopical Evaluation of Dental Implants Retrieved for Different Causes: A Narrative Review. Int. J. Periodontics Restor. Dent. 2020, 40, e211–e227. [Google Scholar] [CrossRef]
- Fuster-Torres, M.Á.; Peñarrocha-Diago, M.; Peñarrocha-Oltra, D.; Peñarrocha-Diago, M. Relationships between Bone Density Values from Cone Beam Computed Tomography, Maximum Insertion Torque, and Resonance Frequency Analysis at Implant Placement: A Pilot Study. Int. J. Oral Maxillofac. Implant. 2011, 26, 1051–1056. [Google Scholar]
- Scarano, A.; Lorusso, F.; Staiti, G.; Sinjari, B.; Tampieri, A.; Mortellaro, C. Sinus Augmentation with Biomimetic Nanostructured Matrix: Tomographic, Radiological, Histological and Histomorphometrical Results after 6 Months in Humans. Front. Physiol. 2017, 8, 565. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gehrke, S.A.; Mazón, P.; Del Fabbro, M.; Tumedei, M.; Júnior, J.A.; Pérez-Díaz, L.; De Aza, P.N. Histological and Histomorphometric Analyses of Two Bovine Bone Blocks Implanted in Rabbit Calvaria. Symmetry 2019, 11, 641. [Google Scholar] [CrossRef] [Green Version]
- Scarano, A.; Noumbissi, S.; Gupta, S.; Inchingolo, F.; Stilla, P.; Lorusso, F. Scanning Electron Microscopy Analysis and Energy Dispersion X-Ray Microanalysis to Evaluate the Effects of Decontamination Chemicals and Heat Sterilization on Implant Surgical Drills: Zirconia vs. Steel. Appl. Sci. 2019, 9, 2837. [Google Scholar] [CrossRef] [Green Version]
- Maglione, M.; Bevilacqua, L.; Dotto, F.; Costantinides, F.; Lorusso, F.; Scarano, A. Observational Study on the Preparation of the Implant Site with Piezosurgery vs. Drill: Comparison between the Two Methods in Terms of Postoperative Pain, Surgical Times, and Operational Advantages. BioMed Res. Int. 2019, 2019, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Insertion Torque | 10 PCF | 20 PCF | ||||||
|---|---|---|---|---|---|---|---|---|
| No cortical layer | Cortical layer | No cortical layer | Cortical layer | |||||
| Cylindrical | Conical | Cylindrical | Conical | Cylindrical | Conical | Cylindrical | Conical | |
| Mean | 10.92 | 13.80 | 20.23 | 24.62 | 32.07 | 39.37 | 37.34 | 43.80 |
| Std. Deviation | 0.8522 | 1.244 | 0.5851 | 0.8979 | 1.191 | 0.9129 | 0.6963 | 0.9274 |
| Lower 95% CI | 10.31 | 12.91 | 19.81 | 23.98 | 31.22 | 38.72 | 36.84 | 43.14 |
| Upper 95% CI | 11.53 | 14.69 | 20.65 | 25.26 | 32.92 | 40.02 | 37.84 | 44.46 |
| Removal Torque | 10 PCF | 20 PCF | ||||||
|---|---|---|---|---|---|---|---|---|
| No cortical layer | Cortical layer | No cortical layer | Cortical layer | |||||
| Cylindrical | Conical | Cylindrical | Conical | Cylindrical | Conical | Cylindrical | Conical | |
| Mean | 9.980 | 10.98 | 14.09 | 16.01 | 23.07 | 29.12 | 25.03 | 33.19 |
| Std. Deviation | 0.4077 | 1.121 | 0.8157 | 0.6226 | 0.4029 | 0.5731 | 0.9274 | 0.7564 |
| Lower 95% CI | 9.688 | 10.18 | 13.51 | 15.56 | 22.78 | 28.71 | 24.37 | 32.65 |
| Upper 95% CI | 10.27 | 11.78 | 14.67 | 16.46 | 23.36 | 29.53 | 25.69 | 33.73 |
| RFA | 10 PCF | 20 PCF | ||||||
|---|---|---|---|---|---|---|---|---|
| No cortical layer | Cortical layer | No cortical layer | Cortical layer | |||||
| Cylindrical | Conical | Cylindrical | Conical | Cylindrical | Conical | Cylindrical | Conical | |
| Mean | 51.55 | 54.45 | 60.85 | 62.35 | 65.00 | 64.35 | 68.85 | 69.20 |
| Std. Deviation | 0.3689 | 0.4972 | 0.4743 | 0.7091 | 0.8498 | 0.4743 | 0.6258 | 0.7888 |
| Lower 95% CI | 51.29 | 54.09 | 60.51 | 61.84 | 64.39 | 64.01 | 68.40 | 68.64 |
| Upper 95% CI | 51.81 | 54.81 | 61.19 | 62.86 | 65.61 | 64.69 | 69.30 | 69.76 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Comuzzi, L.; Tumedei, M.; D’Arcangelo, C.; Piattelli, A.; Iezzi, G. An In Vitro Analysis on Polyurethane Foam Blocks of the Insertion Torque (IT) Values, Removal Torque Values (RTVs), and Resonance Frequency Analysis (RFA) Values in Tapered and Cylindrical Implants. Int. J. Environ. Res. Public Health 2021, 18, 9238. https://doi.org/10.3390/ijerph18179238
Comuzzi L, Tumedei M, D’Arcangelo C, Piattelli A, Iezzi G. An In Vitro Analysis on Polyurethane Foam Blocks of the Insertion Torque (IT) Values, Removal Torque Values (RTVs), and Resonance Frequency Analysis (RFA) Values in Tapered and Cylindrical Implants. International Journal of Environmental Research and Public Health. 2021; 18(17):9238. https://doi.org/10.3390/ijerph18179238
Chicago/Turabian StyleComuzzi, Luca, Margherita Tumedei, Camillo D’Arcangelo, Adriano Piattelli, and Giovanna Iezzi. 2021. "An In Vitro Analysis on Polyurethane Foam Blocks of the Insertion Torque (IT) Values, Removal Torque Values (RTVs), and Resonance Frequency Analysis (RFA) Values in Tapered and Cylindrical Implants" International Journal of Environmental Research and Public Health 18, no. 17: 9238. https://doi.org/10.3390/ijerph18179238







