Do Patients Residing in Provincial Areas Transport and Spend More on Cancer Treatment in Korea?
Abstract
1. Introduction
2. Methods
2.1. Data and Study Population
2.2. Outcome Measure
2.3. Interesting Variable
2.4. Covariates
2.5. Research Ethical Approval
2.6. Statistical Analysis
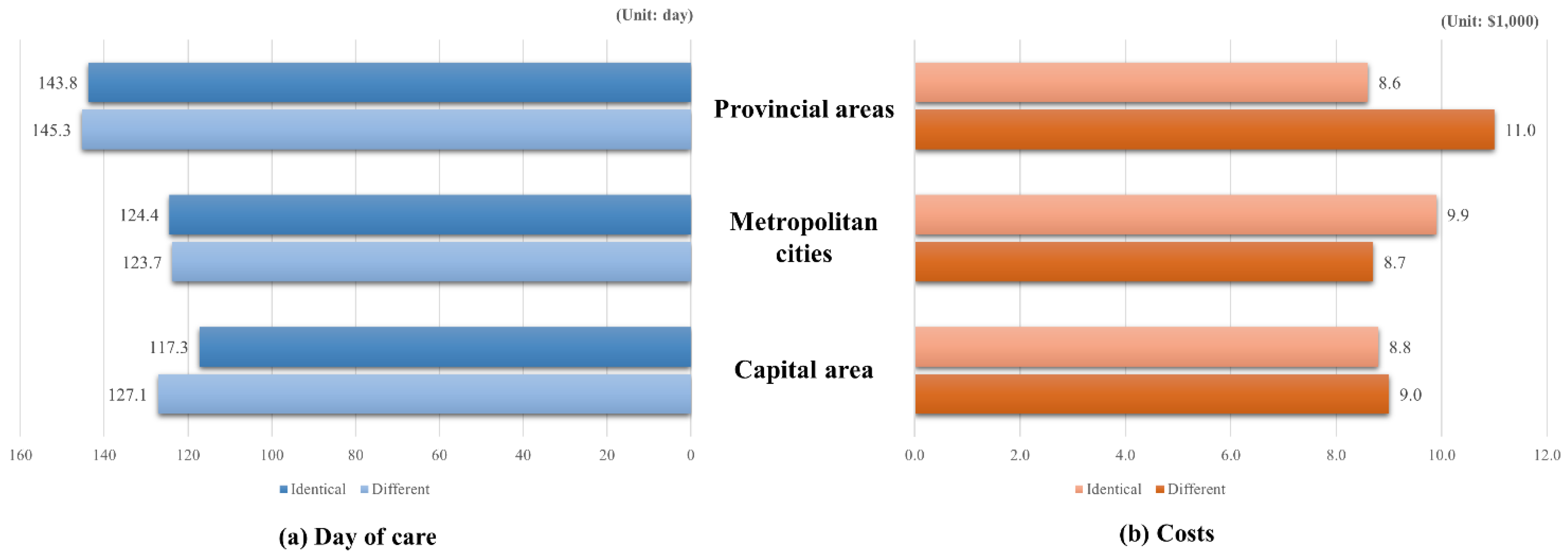
3. Results
4. Discussions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Global Health Estimates 2020: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2019. Available online: https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-leading-causes-of-death (accessed on 31 January 2021).
- Choi, H.C.W.; Lam, K.O.; Pang, H.H.M.; Tsang, S.K.C.; Ngan, R.K.C.; Lee, A.W.M. Global comparison of cancer outcomes: Standardization and correlation with healthcare expenditures. BMC Public Health 2019, 19, 1065. [Google Scholar] [CrossRef]
- Prager, G.W.; Braga, S.; Bystricky, B.; Qvortrup, C.; Criscitiello, C.; Esin, E.; Sonke, G.S.; Martinez, G.A.; Frenel, J.S.; Karamouzis, M.; et al. Global cancer control: Responding to the growing burden, rising costs and inequalities in access. ESMO Open 2018, 3, e000285. [Google Scholar] [CrossRef] [PubMed]
- Disease, G.B.D.; Injury, I.; Prevalence, C. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the global burden of disease study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar]
- Hong, S.; Won, Y.J.; Park, Y.R.; Jung, K.W.; Kong, H.J.; Lee, E.S. Community of population-based regional cancer, r. cancer statistics in Korea: Incidence, mortality, survival, and prevalence in 2017. Cancer Res. Treat. 2020, 52, 335–350. [Google Scholar] [CrossRef]
- Park, M.; Song, I. Medical care costs of cancer in the last year of life using national health insurance data in Korea. PLoS ONE 2018, 13, e0197891. [Google Scholar] [CrossRef]
- Lee, K.S.; Chang, H.S.; Lee, S.M.; Park, E.C. Economic burden of cancer in Korea during 2000–2010. Cancer Res. Treat. 2015, 47, 387–398. [Google Scholar] [CrossRef]
- Kim, L.; Kim, J.A.; Kim, S. A guide for the utilization ofs. Epidemiol. Health 2014, 36, e2014008. [Google Scholar] [CrossRef]
- Song, Y. The South Korean health care system. Jpn. Med Assoc. J. 2009, 52, 206–209. [Google Scholar]
- Cho, S.; Chang, Y.; Kim, Y. Cancer patients’ utilization of tertiary hospitals in seoul before and after the benefit expansion policy. J. Prev. Med. Public Health 2019, 52, 41. [Google Scholar] [CrossRef]
- Park, S.; Park, I.K.; Kim, E.R.; Hwang, Y.; Lee, H.J.; Kang, C.H.; Kim, Y.T. Current trends of lung cancer surgery and demographic and social factors related to changes in the trends of lung cancer surgery: An analysis of the national database from 2010 to 2014. Cancer Res. Treat. 2017, 49, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Mooney, C.; Zwanziger, J.; Phibbs, C.; Schmitt, S. Is travel distance a barrier to veterans’ use of VA hospitals for medical surgical care? Soc. Sci Med. 2000, 50, 1743–1755. [Google Scholar] [CrossRef]
- Nemet, G.; Bailey, A. Distance and health care utilization among the rural elderly. Soc. Sci. Med. 2000, 50, 1197–1208. [Google Scholar] [CrossRef]
- Siciliani, L.; Hurst, J. Tackling excessive waiting times for elective surgery: A comparative analysis of policies in 12 OECD countries. Health Policy 2005, 72, 201–215. [Google Scholar] [CrossRef]
- Kelly, C.; Hulme, C.; Farragher, T.; Clarke, G. Are differences in travel time or distance to healthcare for adults in global north countries associated with an impact on health outcomes? A systematic review. BMJ Open 2016, 6, e013059. [Google Scholar] [CrossRef] [PubMed]
- Chan, L.; Hart, L.G.; Goodman, D.C. Geographic access to health care for rural medicare beneficiaries. J. Rural Health 2006, 22, 140–146. [Google Scholar] [CrossRef]
- Billi, J.E.; Pai, C.-W.; Spahlinger, D.A. The effect of distance to primary care physician on health care utilization and disease burden. Health Care Manag. Rev. 2007, 32, 22–29. [Google Scholar] [CrossRef]
- Choi, H.; Yang, S.-Y.; Cho, H.-S.; Kim, W.; Park, E.-C.; Han, K.-T. Mortality differences by surgical volume among patients with stomach cancer: A threshold for a favorable volume-outcome relationship. World J. Surg. Oncol. 2017, 15, 1–9. [Google Scholar] [CrossRef]
- Bristow, R.E.; Chang, J.; Ziogas, A.; Gillen, D.L.; Bai, L.; Vieira, V.M. Spatial analysis of advanced-stage ovarian cancer mortality in California. Am. J. Obstet. Gynecol. 2015, 213, 43.e1–43.e8. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, A.; Lewis, D.; Charman, S.C.; Mason, M.; Clarke, N.; Sullivan, R.; van der Meulen, J. Determinants of patient mobility for prostate cancer surgery: A population-based study of choice and competition. Eur. Urol. 2018, 73, 822–825. [Google Scholar] [CrossRef]
- Aggarwal, A.; Lewis, D.; Mason, M.; Purushotham, A.; Sullivan, R.; van der Meulen, J. Effect of patient choice and hospital competition on service configuration and technology adoption within cancer surgery: A national, population-based study. Lancet Oncol. 2017, 18, 1445–1453. [Google Scholar] [CrossRef]
- Kim, M.; Park, J.; Kim, S.; Choi, S.; Yoon, S.; Lee, S. Feasibility of gastric cancer surgery at low volume hospitals. J. Gastric Cancer 2010, 10, 234–240. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kim, J.; Kim, S.; Yun, S.; Chung, J.; Choi, H.; Yu, H.; Ha, Y.; Cho, I.; Kim, H.; Chung, H.; et al. Medical Travel among non-seoul residents to seek prostate cancer treatment in medical facilities of seoul. Cancer Res. Treat. 2019, 51, 53–64. [Google Scholar] [CrossRef]
- Trinh, Q.D.; Bjartell, A.; Freedland, S.J.; Hollenbeck, B.K.; Hu, J.C.; Shariat, S.F.; Sun, M.; Vickers, A.J. A systematic review of the volume-outcome relationship for radical prostatectomy. Eur. Urol. 2013, 64, 786–798. [Google Scholar] [CrossRef] [PubMed]
- Nadpara, P.; Madhavan, S.S.; Tworek, C. Guideline-concordant timely lung cancer care and prognosis among elderly patients in the United States: A population-based study. Cancer Epidemiol. 2015, 39, 1136–1144. [Google Scholar] [CrossRef]
- Owonikoko, T.K.; Ragin, C.C.; Belani, C.P.; Oton, A.B.; Gooding, W.E.; Taioli, E.; Ramalingam, S.S. Lung cancer in elderly patients: An analysis of the surveillance, epidemiology, and end results database. J. Clin. Oncol. 2007, 25, 5570–5577. [Google Scholar] [CrossRef]
- Samson, P.; Patel, A.; Garrett, T.; Crabtree, T.; Kreisel, D.; Krupnick, A.S.; Patterson, G.A.; Broderick, S.; Meyers, B.F.; Puri, V. Effects of delayed surgical resection on short-term and long-term outcomes in clinical stage i non-small cell lung cancer. Ann. Thorac. Surg. 2015, 99, 1906–1912. [Google Scholar] [CrossRef]

| Variables | Total | Area of Residence vs. Location of Hospital Visited for Treatment | ||||
|---|---|---|---|---|---|---|
| Different | Identical | p-Value | ||||
| N | % | N | % | |||
| Residing area | ||||||
| Capital area | 23,633 | 6208 | 26.3 | 17,425 | 73.7 | <0.0001 |
| Metropolitan cities | 14,064 | 3366 | 23.9 | 10,698 | 76.1 | |
| Provincial areas | 26,808 | 10,401 | 38.8 | 16,407 | 61.2 | |
| Institution of main treatment | ||||||
| General hospital | 44,108 | 16,507 | 37.4 | 27,601 | 62.6 | <0.0001 |
| Hospital | 4641 | 1067 | 23.0 | 3574 | 77.0 | |
| Long-term care hospital | 2959 | 761 | 25.7 | 2198 | 74.3 | |
| Clinic | 12,797 | 1640 | 12.8 | 11,157 | 87.2 | |
| Sex | ||||||
| Male | 36,991 | 11,781 | 31.8 | 25,210 | 68.2 | <0.0001 |
| Female | 27,514 | 8194 | 29.8 | 19,320 | 70.2 | |
| Age | ||||||
| ~69 | 7084 | 2694 | 38.0 | 4390 | 62.0 | <0.0001 |
| 70~74 | 22,666 | 7643 | 33.7 | 15,023 | 66.3 | |
| 75~79 | 19,589 | 5727 | 29.2 | 13,862 | 70.8 | |
| 80~ | 15,166 | 3911 | 25.8 | 11,255 | 74.2 | |
| Types of insurance coverage | ||||||
| NHI self-employed | 6333 | 1275 | 20.1 | 5058 | 79.9 | <0.0001 |
| NHI employed | 18,084 | 5441 | 30.1 | 12,643 | 69.9 | |
| Medical Aid | 40,088 | 13,259 | 33.1 | 26,829 | 66.9 | |
| Economic status | ||||||
| Low | 17,316 | 4444 | 25.7 | 12,872 | 74.3 | <0.0001 |
| Mid-low | 11,525 | 3531 | 30.6 | 7994 | 69.4 | |
| Mid | 10,920 | 3499 | 32.0 | 7421 | 68.0 | |
| Mid-high | 10,619 | 3692 | 34.8 | 6927 | 65.2 | |
| High | 14,125 | 4809 | 34.0 | 9316 | 66.0 | |
| Time since first diagnosis | ||||||
| ~1 y | 25,297 | 8976 | 35.5 | 16,321 | 64.5 | <0.0001 |
| 1~2 y | 13,583 | 4264 | 31.4 | 9319 | 68.6 | |
| 2~3 y | 10,545 | 3024 | 28.7 | 7521 | 71.3 | |
| 3~4 y | 8422 | 2133 | 25.3 | 6289 | 74.7 | |
| 4~5 y | 6658 | 1578 | 23.7 | 5080 | 76.3 | |
| Diagnosed cancer type | ||||||
| Gastric cancer | 22,417 | 7068 | 31.5 | 15,349 | 68.5 | <0.0001 |
| Colorectal cancer | 22,636 | 6739 | 29.8 | 15,897 | 70.2 | |
| Hepatocellular carcinoma | 6030 | 1951 | 32.4 | 4079 | 67.6 | |
| Lung cancer | 13,422 | 4217 | 31.4 | 9205 | 68.6 | |
| Charlson Comorbidity Index (excluded Cancer) | ||||||
| ~2 | 33,904 | 10,301 | 30.4 | 23,603 | 69.6 | <0.0001 |
| 3~5 | 15,337 | 4480 | 29.2 | 10,857 | 70.8 | |
| 6~ | 15,264 | 5194 | 34.0 | 10,070 | 66.0 | |
| Died during observed year | ||||||
| Yes | 6564 | 1936 | 29.5 | 4628 | 70.5 | 0.0065 |
| No | 57,941 | 18,039 | 31.1 | 39,902 | 68.9 | □ |
| Total | 64,505 | 19,975 | 31.0 | 44,530 | 69.0 | □ |
| Variables | Treatment at Hospital Outside of Residing Area | |||
|---|---|---|---|---|
| OR | 95% CI | p-Value | ||
| Residing area | ||||
| Capital area | 1.000 | - | - | - |
| Metropolitan cities | 0.938 | 0.866 | 1.015 | 0.1125 |
| Provincial areas | 2.202 | 2.068 | 2.344 | <0.0001 |
| Institution of main treatment | ||||
| General hospital | 4.396 | 4.056 | 4.765 | <0.0001 |
| Hospital | 2.118 | 1.891 | 2.373 | <0.0001 |
| Long-term care hospital | 2.940 | 2.577 | 3.354 | <0.0001 |
| Clinic | 1.000 | - | - | - |
| Sex | ||||
| Male | 1.000 | - | - | - |
| Female | 1.071 | 1.014 | 1.132 | 0.0141 |
| Age | ||||
| ~69 | 1.287 | 1.172 | 1.413 | <0.0001 |
| 70~74 | 1.304 | 1.219 | 1.395 | <0.0001 |
| 75~79 | 1.140 | 1.068 | 1.216 | <0.0001 |
| 80~ | 1.000 | - | - | - |
| Type of insurance coverage | ||||
| NHI self-employed | 0.578 | 0.515 | 0.649 | <0.0001 |
| NHI employed | 0.880 | 0.829 | 0.935 | <0.0001 |
| Medical Aid | 1.000 | - | - | - |
| Economic status | ||||
| Low | 1.000 | - | - | - |
| Mid-low | 1.058 | 0.978 | 1.144 | 0.1589 |
| Mid | 1.097 | 1.010 | 1.192 | 0.0273 |
| Mid-high | 1.289 | 1.185 | 1.402 | <0.0001 |
| High | 1.351 | 1.246 | 1.465 | <0.0001 |
| Time since first diagnosis | ||||
| ~1 y | 1.221 | 1.138 | 1.310 | <0.0001 |
| 1~2 y | 1.176 | 1.101 | 1.256 | <0.0001 |
| 2~3 y | 1.133 | 1.065 | 1.205 | <0.0001 |
| 3~4 y | 1.012 | 0.957 | 1.069 | 0.6841 |
| 4~5 y | 1.000 | - | - | - |
| Diagnosed cancer type | ||||
| Gastric cancer | 1.000 | - | - | - |
| Colorectal cancer | 0.985 | 0.922 | 1.052 | 0.6510 |
| Hepatocellular carcinoma | 0.995 | 0.907 | 1.093 | 0.9223 |
| Lung cancer | 0.996 | 0.927 | 1.069 | 0.9035 |
| Charlson Comorbidity Index (excluded Cancer) | ||||
| ~2 | 1.114 | 1.055 | 1.176 | 0.0001 |
| 3~5 | 0.988 | 0.930 | 1.049 | 0.6844 |
| 6~ | 1.000 | - | - | - |
| Died during observed year | ||||
| Yes | 1.000 | - | - | - |
| No | 1.379 | 1.291 | 1.472 | <0.0001 |
| Year | 0.930 | 0.919 | 0.940 | <0.0001 |
| Variables | Days of Care | Costs | ||||||
|---|---|---|---|---|---|---|---|---|
| RR | 95% CI | p-Value | RR | 95% CI | p-Value | |||
| Treatment at hospital outside of residing area | ||||||||
| Yes | 1.021 | 0.986 | 1.058 | 0.2431 | 1.054 | 1.017 | 1.093 | 0.0037 |
| No | 1.000 | - | - | - | 1.000 | - | - | - |
| Residential area | ||||||||
| Capital area | 1.000 | - | - | - | 1.000 | - | - | - |
| Metropolitan cities | 0.998 | 0.948 | 1.051 | 0.9439 | 1.007 | 0.960 | 1.056 | 0.7863 |
| Provincial areas | 1.178 | 1.129 | 1.231 | <0.0001 | 1.002 | 0.961 | 1.044 | 0.9254 |
| Types of main treatment institution | ||||||||
| General hospital | 1.019 | 0.970 | 1.070 | 0.4598 | 3.111 | 2.949 | 3.282 | <0.0001 |
| Hospital | 1.102 | 1.038 | 1.170 | 0.0015 | 2.471 | 2.312 | 2.641 | <0.0001 |
| Long-term care hospital | 2.108 | 1.985 | 2.238 | <0.0001 | 7.396 | 6.854 | 7.980 | <0.0001 |
| Clinic | 1.000 | - | - | - | 1.000 | - | - | - |
| Sex | ||||||||
| Male | 1.000 | - | - | - | 1.000 | - | - | - |
| Female | 1.000 | 0.961 | 1.040 | 0.9953 | 0.969 | 0.934 | 1.004 | 0.0845 |
| Age (years) | ||||||||
| ~69 | 1.000 | - | - | - | 1.000 | - | - | - |
| 70~74 | 0.887 | 0.828 | 0.951 | 0.0007 | 1.149 | 1.079 | 1.222 | <0.0001 |
| 75~79 | 0.920 | 0.874 | 0.968 | 0.0014 | 1.049 | 0.997 | 1.103 | 0.068 |
| 80~ | 0.966 | 0.921 | 1.013 | 0.1546 | 1.021 | 0.969 | 1.075 | 0.4408 |
| Types of Insurance coverage | ||||||||
| NHI self-employed | 1.178 | 1.095 | 1.268 | <0.0001 | 1.119 | 1.045 | 1.197 | 0.0012 |
| NHI employed | 0.972 | 0.932 | 1.014 | 0.1936 | 0.966 | 0.929 | 1.004 | 0.0764 |
| Medical-Aid | 1.000 | - | - | - | 1.000 | - | - | - |
| Economic status | ||||||||
| Low | 1.000 | - | - | - | 1.000 | - | - | - |
| Mid-low | 0.980 | 0.925 | 1.037 | 0.478 | 1.070 | 1.007 | 1.138 | 0.0296 |
| Mid | 0.980 | 0.923 | 1.041 | 0.5179 | 1.003 | 0.955 | 1.055 | 0.8975 |
| Mid-high | 0.984 | 0.925 | 1.047 | 0.6071 | 0.990 | 0.939 | 1.044 | 0.7103 |
| High | 0.969 | 0.914 | 1.028 | 0.299 | 1.043 | 0.991 | 1.097 | 0.1086 |
| Period after first diagnosis | ||||||||
| ~1 y | 1.403 | 1.329 | 1.482 | <0.0001 | 2.877 | 2.685 | 3.082 | <0.0001 |
| 1~2 y | 1.015 | 0.973 | 1.058 | 0.4995 | 1.259 | 1.204 | 1.316 | <0.0001 |
| 2~3 y | 1.001 | 0.967 | 1.036 | 0.9451 | 1.120 | 1.073 | 1.169 | <0.0001 |
| 3~4 y | 1.025 | 0.998 | 1.053 | 0.0732 | 1.086 | 1.043 | 1.132 | <0.0001 |
| 4~5 y | 1.000 | - | - | - | 1.000 | - | - | - |
| Types of cancer which diagnosed | ||||||||
| Gastric cancer | 1.000 | - | - | - | 1.000 | - | - | - |
| Colorectal cancer | 1.086 | 1.033 | 1.142 | 0.0013 | 1.065 | 1.018 | 1.115 | 0.0068 |
| Hepatocellular carcinoma | 1.184 | 1.107 | 1.268 | <0.0001 | 1.323 | 1.244 | 1.406 | <0.0001 |
| Lung cancer | 1.232 | 1.174 | 1.292 | <0.0001 | 1.188 | 1.132 | 1.247 | <0.0001 |
| Charlson Comorbidity Index (excluded Cancer) | ||||||||
| ~2 | 0.552 | 0.530 | 0.574 | <0.0001 | 0.404 | 0.387 | 0.423 | <0.0001 |
| 3~5 | 0.769 | 0.741 | 0.799 | <0.0001 | 0.625 | 0.600 | 0.650 | <0.0001 |
| 6~ | 1.000 | - | - | - | 1.000 | - | - | - |
| Died in the observed year | ||||||||
| Dead | 1.000 | - | - | - | 1.000 | - | - | - |
| Alive | 0.398 | 0.386 | 0.412 | <0.0001 | 0.171 | 0.161 | 0.180 | <0.0001 |
| Year | 0.989 | 0.980 | 0.998 | 0.0 | 1.078 | 1.066 | 1.091 | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, W.; Han, K.-T.; Kim, S. Do Patients Residing in Provincial Areas Transport and Spend More on Cancer Treatment in Korea? Int. J. Environ. Res. Public Health 2021, 18, 9247. https://doi.org/10.3390/ijerph18179247
Kim W, Han K-T, Kim S. Do Patients Residing in Provincial Areas Transport and Spend More on Cancer Treatment in Korea? International Journal of Environmental Research and Public Health. 2021; 18(17):9247. https://doi.org/10.3390/ijerph18179247
Chicago/Turabian StyleKim, Woorim, Kyu-Tae Han, and Seungju Kim. 2021. "Do Patients Residing in Provincial Areas Transport and Spend More on Cancer Treatment in Korea?" International Journal of Environmental Research and Public Health 18, no. 17: 9247. https://doi.org/10.3390/ijerph18179247
APA StyleKim, W., Han, K.-T., & Kim, S. (2021). Do Patients Residing in Provincial Areas Transport and Spend More on Cancer Treatment in Korea? International Journal of Environmental Research and Public Health, 18(17), 9247. https://doi.org/10.3390/ijerph18179247






