Scapular Retraction under Adduction Load: An Alternative to Overhead Exercises to Activate Infraspinatus, Upper, and Lower Trapezius in Subjects with and without Shoulder Pain
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
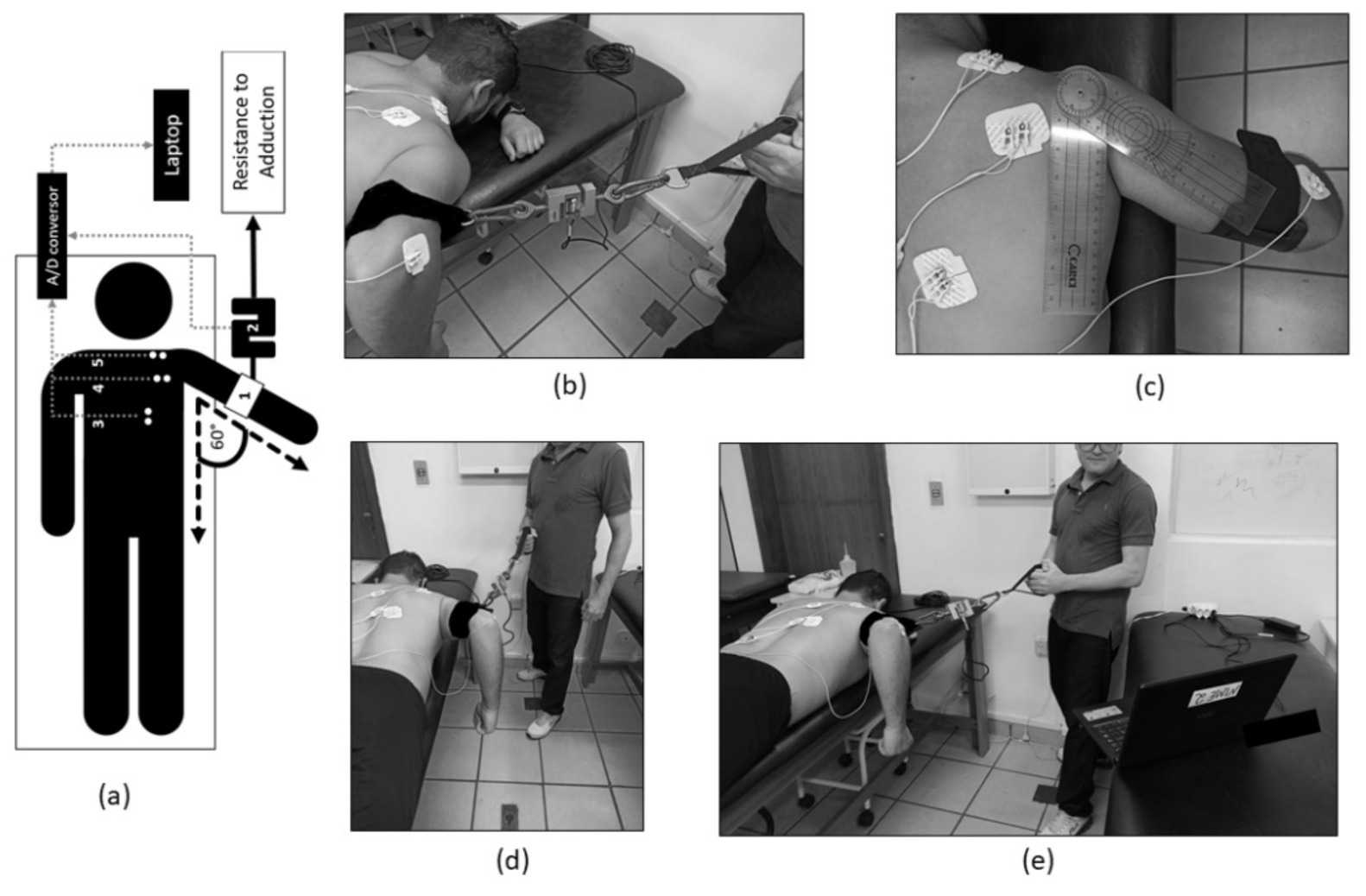
2.2. Instruments
2.3. Maximal Voluntary Isometric Contraction for Electromyography Normalization Purposes
2.4. Maximal Voluntary Isometric Contraction to Control the Adduction Resistance
2.5. Exercise Description
2.6. Data Extraction
2.7. Statistics
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hawk, C.; Minkalis, A.L.; Khorsan, R.; Daniels, C.J.; Homack, D.; Gliedt, J.A.; Hartman, J.A.; Bhalerao, S. Systematic Review of Nondrug, Nonsurgical Treatment of Shoulder Conditions. J. Manip. Physiol. Ther. 2017, 40, 293–319. [Google Scholar] [CrossRef] [Green Version]
- Castelein, B.; Cools, A.M.J.J.; Parlevliet, T.; Cagnie, B.; Shire, A.R.; Stæhr, T.A.B.B.; Overby, J.B.; Bastholm Dahl, M.; Sandell Jacobsen, J.; Høyrup Christiansen, D.; et al. Prevalence of upper limb pain and disability and its correlates with demographic and personal factors. Cochrane Database Syst. Rev. 2019, 18, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Reijneveld, A.E.E.; Noten, S.; Michener, A.L.; Cools, A.; Struyf, F. Clinical outcomes of a scapular-focused treatment in patients with subacromial pain syndrome: A systematic review. Br. J. Sports Med. 2017, 51, 436–441. [Google Scholar] [CrossRef]
- Khosravi, F.; Amiri, Z.; Masouleh, N.A.; Kashfi, P.; Panjizadeh, F.; Hajilo, Z.; Shanayii, S.; Khodakarim, S.; Rahnama, L. Shoulder pain prevalence and risk factors in middle-aged women: A cross-sectional study. J. Bodyw. Mov. Ther. 2019, 23, 752–757. [Google Scholar] [CrossRef]
- Luime, J.J.; Koes, B.W.; Hendriksen, I.J.M.; Burdorf, A.; Verhagen, A.P.; Miedema, H.S.; Verhaar, J.A.N. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand. J. Rheumatol. 2004, 33, 73–81. [Google Scholar] [CrossRef]
- Pribicevic, M. The epidemiology of shoulder Pain: A narrative review of the literature. In Pain in Perspective; IntechOpen: London, UK, 2012. [Google Scholar]
- Facci, L.M. Síndromes Dolorosas do Ombro: Análise de sua Incidência e Características; Arq Ciências da Saúde da UNIPAR: Paraná, Brazil, 2000; Available online: https://revistas.unipar.br/index.php/saude/article/view/1028 (accessed on 27 February 2021).
- Garzedin, D.D.D.S.; Matos, M.A.A.; Daltro, C.H.; Barros, R.M.; Guimarães, A. Pain severity in patients with painful shoulder syndrome. Acta Ortop. Bras. 2008, 16, 165–167. [Google Scholar] [CrossRef] [Green Version]
- Hanvold, T.N.; Wærsted, M.; Mengshoel, A.M.; Bjertness, E.; Twisk, J.; Veiersted, K.B. A longitudinal study on risk factors for neck and shoulder pain among young adults in the transition from technical school to working life. Scand. J. Work. Environ. Health 2014, 40, 597–609. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Littlewood, C.; Cools, A.M.J. Scapular dyskinesis and shoulder pain: The devil is in the detail. Br. J. Sports Med. 2017, 52, 72–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Djade, C.D.; Porgo, T.V.; Zomahoun, H.T.V.; Perrault-Sullivan, G.; Dionne, C. Incidence of shoulder pain in 40 years old and over and associated factors: A systematic review. Eur. J. Pain 2020, 24, 39–50. [Google Scholar] [CrossRef]
- Han, D.-S.; Wu, W.-T.; Hsu, P.-C.; Chang, H.-C.; Huang, K.-C.; Chang, K.-V. Sarcopenia Is Associated with Increased Risks of Rotator Cuff Tendon Diseases Among Community-Dwelling Elders: A Cross-Sectional Quantitative Ultrasound Study. Front. Med. 2021, 8, 566. [Google Scholar] [CrossRef]
- Ellenbecker, T.S.; Cools, A. Rehabilitation of shoulder impingement syndrome and rotator cuff injuries: An evidence-based review. Br. J. Sports Med. 2010, 44, 319–327. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holmgren, T.; Hallgren, H.B.; Öberg, B.; Adolfsson, L.; Johansson, K. Effect of specific exercise strategy on need for surgery in patients with subacromial impingement syndrome: Randomised controlled study. Br. J. Sports Med. 2014, 48, 1456–1457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Page, P. Shoulder muscle imbalance and subacromial impingement syndrome in overhead athletes. Int. J. Sports Phys. Ther. 2011, 6, 51–58. [Google Scholar]
- Steuri, R.; Sattelmayer, K.M.; Elsig, S.; Kolly, C.; Tal, A.; Taeymans, J.; Hilfiker, R. Effectiveness of conservative interventions including exercise, manual therapy and medical management in adults with shoulder impingement: A systematic review and meta-analysis of RCTs. Br. J. Sports Med. 2017, 51, 1340–1347. [Google Scholar] [CrossRef] [Green Version]
- Juel, N.G.; Natvig, B. Shoulder diagnoses in secondary care, a one year cohort. BMC Musculoskelet. Disord. 2014, 15, 89. [Google Scholar] [CrossRef] [Green Version]
- Camargo, P.R.; Alburquerque-Sendín, F.; Avila, M.; Haik, M.; Vieira, A.; Salvini, T. Effects of Stretching and Strengthening Exercises, with and without Manual Therapy, on Scapular Kinematics, Function, and Pain in Individuals with Shoulder Impingement: A Randomized Controlled Trial. J. Orthop. Sports Phys. Ther. 2015, 45, 984–997. [Google Scholar] [CrossRef]
- Saito, H.; Harrold, M.E.; Cavalheri, V.; McKenna, L. Scapular focused interventions to improve shoulder pain and function in adults with subacromial pain: A systematic review and meta-analysis. Physiother. Theory Pr. 2018, 34, 653–670. [Google Scholar] [CrossRef]
- Struyf, F.; Cagnie, B.; Cools, A.; Baert, I.; Van Brempt, J.; Struyf, P.; Meeus, M. Scapulothoracic muscle activity and recruitment timing in patients with shoulder impingement symptoms and glenohumeral instability. J. Electromyogr. Kinesiol. 2014, 24, 277–284. [Google Scholar] [CrossRef]
- Lawrence, R.L.; Braman, J.P.; Laprade, R.F.; Ludewig, P. Comparison of 3-Dimensional Shoulder Complex Kinematics in Individuals with and without Shoulder Pain, Part 1: Sternoclavicular, Acromioclavicular, and Scapulothoracic Joints. J. Orthop. Sports Phys. Ther. 2014, 44, 636–645. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reddy, A.S.; Mohr, K.J.; Pink, M.M.; Jobe, F.W. Electromyographic analysis of the deltoid and rotator cuff muscles in persons with subacromial impingement. J. Shoulder Elb. Surg. 2000, 9, 519–523. [Google Scholar] [CrossRef]
- Pyndt, L.; Nørregaard, J.; Dyhre-poulsen, P.; Winther, A. The activity pattern of shoulder muscles in subjects with and without subacromial impingement The activity pattern of shoulder muscles in subjects with and without subacromial impingement. J. Electromyogr. Kinesiol. 2010, 19, 789–799. [Google Scholar] [CrossRef]
- Klintberg, I.H.; Cools, A.M.J.; Holmgren, T.M.; Holzhausen, A.-C.G.; Johansson, K.; Maenhout, A.G.; Moser, J.S.; Spunton, V.; Ginn, K. Consensus for physiotherapy for shoulder pain. Int. Orthop. 2015, 39, 715–720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harput, G.; Güney-Deniz, H.; Düzgün, I. Upper to middle trapezius muscle activation ratio during scapular retraction exercise at different shoulder abduction ancles. Fiz. Rehabil. 2017, 28, 111–117. [Google Scholar]
- Kara, D.; Harput, G.; Duzgun, I. Trapezius muscle activation levels and ratios during scapular retraction exercises: A comparative study between patients with subacromial impingement syndrome and healthy controls. Clin. Biomech. 2019, 67, 119–126. [Google Scholar] [CrossRef]
- Castelein, B.; Cools, A.; Parlevliet, T.; Cagnie, B. Modifying the shoulder joint position during shrugging and retraction exercises alters the activation of the medial scapular muscles. Man. Ther. 2016, 21, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Skolimowski, J.; Winiarski, S.; Anwajler, J.; Skolimowska, B.; Barczyk, K.; Dudek, K. Bioelectric activity of selected muscle groups in people with impingement syndrome. Acta Bioeng. Biomech. 2009, 11, 37–45. [Google Scholar] [PubMed]
- Page, M.J.; Green, S.; McBain, B.; Surace, S.J.; Deitch, J.; Lyttle, N.; Mrocki, A.M.; Buchbinder, R. Manual therapy and exercise for rotator cuff disease. Cochrane Database Syst. Rev. 2016, 6. [Google Scholar] [CrossRef] [PubMed]
- Dong, W.; Goost, H.; Lin, X.B.; Burger, C.; Paul, C.; Wang, Z.L.; Zhang, T.Y.; Jiang, Z.C.; Welle, K.; Kabir, K. Treatments for shoulder impingement syndrome a prisma systematic review and network meta-analysis. Medicine 2015, 94, 1–17. [Google Scholar] [CrossRef]
- Heron, S.R.; Woby, S.R.; Thompson, D.P. Comparison of three types of exercise in the treatment of rotator cuff tendinopathy/shoulder impingement syndrome: A randomized controlled trial. Physiotherapy 2017, 103, 167–173. [Google Scholar] [CrossRef]
- Arias-Buría, J.L.; Fernández-De-Las-Peñas, C.; Ceña, M.P.; Koppenhaver, S.L.; Salom-Moreno, J. Exercises and Dry Needling for Subacromial Pain Syndrome: A Randomized Parallel-Group Trial. J. Pain 2017, 18, 11–18. [Google Scholar] [CrossRef] [Green Version]
- Bury, J.; West, M.; Chamorro-Moriana, G.; Littlewood, C. Effectiveness of scapula-focused approaches in patients with rotator cuff related shoulder pain: A systematic review and meta-analysis. Man. Ther. 2016, 25, 35–42. [Google Scholar] [CrossRef]
- Lewis, J.; McCreesh, K.; Roy, J.-S.; Ginn, K. Rotator Cuff Tendinopathy: Navigating the Diagnosis-Management Conundrum. J. Orthop. Sports Phys. Ther. 2015, 45, 923–937. [Google Scholar] [CrossRef] [Green Version]
- Seitz, A.L.; McClure, P.W.; Finucane, S.; Boardman, N.D.; Michener, L.A. Mechanisms of rotator cuff tendinopathy: Intrinsic, extrinsic, or both? Clin. Biomech. 2011, 26, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Lunden, J.B.; Braman, J.P.; Laprade, R.F.; Ludewig, P.M. Shoulder kinematics during the wall push-up plus exercise. J. Shoulder Elb. Surg. 2010, 19, 216–223. [Google Scholar] [CrossRef] [Green Version]
- Muething, A.; Acocello, S.; Pritchard, K.A.; Brockmeier, S.F.; Saliba, S.A.; Hart, J.M.; Rupp, K. Shoulder-Muscle Activation in Individuals With Previous Shoulder Injuries. J. Sport Rehabil. 2015, 24, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Schory, A.; Bidinger, E.; Wolf, J.; Murray, L. A systematic review of the exercises that produce optimal muscle ratios of the scapular stabilizers in normal shoulders. Int. J. Sports Phys. Ther. 2016, 11, 321–336. [Google Scholar] [PubMed]
- Cools, A.M.; Declercq, G.A.; Cambier, D.C.; Mahieu, N.N.; Witvrouw, E.E. Trapezius activity and intramuscular balance during isokinetic exercise in overhead athletes with impingement symptoms. Scand. J. Med. Sci. Sports 2006, 17, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Martins, J.; Napoles, B.V.; Hoffman, C.B.; Oliveira, A.S. Versão brasileira do shoulder pain and disability index: Tradução, adaptação cultural e confiabilidade. Rev. Bras. Fisioter. 2010, 14, 527–536. [Google Scholar] [CrossRef] [Green Version]
- Orfale, A.G.; Araújo, P.M.P.; Ferraz, M.B.; Natour, J. Translation into Brazilian Portuguese, cultural adaptation and evaluation of the reliability of the Disabilities of th Arm, Shoulder and Hand Questionnaire. Brazilian J. Med. Biol. Res. 2005, 38, 293–302. [Google Scholar] [CrossRef] [Green Version]
- Franchignoni, F.; Vercelli, S.; Giordano, A.; Sartorio, F.; Bravini, E.; Ferriero, G. Minimal Clinically Important Difference of the Disabilities of the Arm, Shoulder and Hand Outcome Measure (DASH) and Its Shortened Version (QuickDASH). J. Orthop. Sports Phys. Ther. 2014, 44, 30–39. [Google Scholar] [CrossRef] [Green Version]
- Thoomes-de Graaf, M.; Scholten-Peeters, W.; Duijn, E.; Karel, Y.; de Vet, H.C.W.; Koes, B.; Verhagen, A. The Responsiveness and Interpretability of the Shoulder Pain and Disability Index. J. Orthop. Sport. Phys. Ther. 2017, 47, 278–286. [Google Scholar] [CrossRef]
- La, A.M.; Mk, W.; Wc, D. Reliability and Diagnostic Accuracy of 5 Physical Examination. YAPMR 2009, 90, 1898–1903. [Google Scholar]
- Ribeiro, D.C.; De Castro, M.P.; Sole, G.; Vicenzino, B. The initial effects of a sustained glenohumeral postero-lateral glide during elevation on shoulder muscle activity: A repeated measures study on asymptomatic shoulders. Man. Ther. 2016, 22, 101–108. [Google Scholar] [CrossRef] [Green Version]
- Toonstra, J.; Mattacola, C.G. Test-Retest Reliability and Validity of Isometric Knee-Flexion and -Extension Measurement Using 3 Methods of Assessing Muscle Strength. J. Sport Rehabil. 2013, 22, 1–5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alpert, S.W.; Pink, M.M.; Jobe, F.W.; McMahon, P.J.; Mathiyakom, W. Electromyographic analysis of deltoid and rotator cuff function under varying loads and speeds. J. Shoulder Elb. Surg. 2000, 9, 47–58. [Google Scholar] [CrossRef]
- Ben Kibler, W.; Sciascia, A.; Uhl, T.L.; Tambay, N.; Cunningham, T. Electromyographic Analysis of Specific Exercises for Scapular Control in Early Phases of Shoulder Rehabilitation. Am. J. Sports Med. 2008, 36, 1789–1798. [Google Scholar] [CrossRef] [PubMed]
- Michener, L.A.; Sharma, S.; Cools, A.M.; Timmons, M.K. Relative scapular muscle activity ratios are altered in subacromial pain syndrome. J. Shoulder Elb. Surg. 2016, 25, 1861–1867. [Google Scholar] [CrossRef]
- Fennell, J.; Phadke, C.P.; Mochizuki, G.; Ismail, F.; Boulias, C. Shoulder Retractor Strengthening Exercise to Minimize Rhomboid Muscle Activity and Subacromial Impingement. Physiother. Can. 2016, 68, 24–28. [Google Scholar] [CrossRef] [Green Version]
- DiGiovine, N.M.; Jobe, F.W.; Pink, M.; Perry, J. An electromyographic analysis of the upper extremity in pitching. J. Shoulder Elb. Surg. 1992, 1, 15–25. [Google Scholar] [CrossRef]
- Contemori, S.; Panichi, R.; Biscarini, A. Effects of scapular retraction/protraction position and scapular elevation on shoulder girdle muscle activity during glenohumeral abduction. Hum. Mov. Sci. 2019, 64, 55–66. [Google Scholar] [CrossRef]
- Forbush, S.W.; Bandy, W.D.; Garrison, M.K.; Graves, L.C.; Roberts, R. Testing infraspinatus and deltoid muscles with new technique to decrease deltoid activity during testing using emg analysis. Int. J. Sports Phys. Ther. 2018, 13, 896–904. [Google Scholar] [CrossRef]
- Sciascia, A.; Kibler, W.B. Current concepts: Scapular dyskinesis. Br. J. Sports Med. 2010, 44, 300–305. [Google Scholar]
- Mottram, S.; Woledge, R.C.; Morrissey, D. Motion analysis study of a scapular orientation exercise and subjects’ ability to learn the exercise. Man. Ther. 2009, 14, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Larsen, C.; Juul-Kristensen, B.; Olsen, H.; Holtermann, A.; Søgaard, K. Selective activation of intra-muscular compartments within the trapezius muscle in subjects with Subacromial Impingement Syndrome. A case-control study. J. Electromyogr. Kinesiol. 2014, 24, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Hickey, D.; Solvig, V.; Cavalheri, V.; Harrold, M.; McKenna, L. Scapular dyskinesis increases the risk of future shoulder pain by 43% in asymptomatic athletes: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 102–110. [Google Scholar] [CrossRef] [PubMed]
| Outcome | SP Group | nSP Group | p |
|---|---|---|---|
| n (male/female) | 26 (7/19) | 16 (5/11) | 0.630 a |
| Age (years) | 26 ± 8 | 22 ± 2 | 0.138 b |
| Weight (kg) | 67 ± 12 | 57 ± 10 | 0.018 b |
| Height (m) | 1.69 ± 8 | 1.66 ± 10 | 0.286 b |
| BMI (kg/m2) | 23 ± 5 | 21 ± 5 | 0.036 b |
| Dyskinesis (yes/no [%]) | 9/91 | 7/93 | 0.837 a |
| QuickDASH score | 25 ± 3 | 2 ± 1.7 | >0.001 c |
| SPADI-total | 31 ± 16 | 2.4 ± 0.5 | >0.001 c |
| SPADI-pain | 40 ± 4.4 | 3.6 ± 1.9 | >0.001 c |
| Muscle | Adduction Load Condition | SP Group (%) | nSP Group (%) | Between-Group (F; p-Value) | Within-Group Pairwise Comparison for Condition Effect (p-Value) |
|---|---|---|---|---|---|
| Upper Trapezius | 20% | 6 ± 4 | 6 ± 5 | 0.39; 0.537 | 20% < 50% (p = 0.004) |
| 30% | 8 ± 7 | 6 ± 5 | |||
| 40% | 7 ± 6 | 6 ± 3 | |||
| 50% | 9 ± 7 | 7 ± 4 | |||
| Lower Trapezius | 20% | 34 ± 16 | 49 ± 29 | 1.14; 0.294 | 20% < 40% (p = 0.001) |
| 30% | 46 ± 26 | 54 ± 35 | 20% < 50% (p = 0.001) | ||
| 40% | 58 ± 40 | 66 ± 37 | 30% < 40% (p = 0.006) | ||
| 50% | 72 ± 44 | 87 ± 42 | 30% < 50% (p = 0.001) | ||
| Infraspinatus | 20% | 23 ± 14 | 18 ± 6 | 1.96; 0.171 | 20% < 40% (p = 0.040) |
| 30% | 25 ± 17 | 17 ± 6 | 20% < 50% (p = 0.001) | ||
| 40% | 29 ± 21 | 21 ± 6 | 30% < 50% (p = 0.001) | ||
| 50% | 37 ± 27 | 27 ± 8 | 40% < 50% (p = 0.001) | ||
| UT:LT | 20% | 0.22 ± 0.18 | 0.16 ± 0.13 | 1.82; 0.186 |
20% < 50% (p = 0.001) 30% < 50% (p = 0.016) |
| 30% | 0.22 ± 0.20 | 0.14 ± 0.08 | |||
| 40% | 0.18 ± 0.15 | 0.13 ± 0.11 | |||
| 50% | 0.16 ± 0.14 | 0.10 ± 0.06 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
dos Santos, J.J.; Nagy, R.O.; Souza, M.A.; Intelangelo, L.; Barbosa, M.A.; Silveira-Nunes, G.; Barbosa, A.C. Scapular Retraction under Adduction Load: An Alternative to Overhead Exercises to Activate Infraspinatus, Upper, and Lower Trapezius in Subjects with and without Shoulder Pain. Int. J. Environ. Res. Public Health 2021, 18, 9251. https://doi.org/10.3390/ijerph18179251
dos Santos JJ, Nagy RO, Souza MA, Intelangelo L, Barbosa MA, Silveira-Nunes G, Barbosa AC. Scapular Retraction under Adduction Load: An Alternative to Overhead Exercises to Activate Infraspinatus, Upper, and Lower Trapezius in Subjects with and without Shoulder Pain. International Journal of Environmental Research and Public Health. 2021; 18(17):9251. https://doi.org/10.3390/ijerph18179251
Chicago/Turabian Styledos Santos, Jefferson James, Rebeca Orozco Nagy, Matheus Almeida Souza, Leonardo Intelangelo, Michelle Almeida Barbosa, Gabriela Silveira-Nunes, and Alexandre Carvalho Barbosa. 2021. "Scapular Retraction under Adduction Load: An Alternative to Overhead Exercises to Activate Infraspinatus, Upper, and Lower Trapezius in Subjects with and without Shoulder Pain" International Journal of Environmental Research and Public Health 18, no. 17: 9251. https://doi.org/10.3390/ijerph18179251
APA Styledos Santos, J. J., Nagy, R. O., Souza, M. A., Intelangelo, L., Barbosa, M. A., Silveira-Nunes, G., & Barbosa, A. C. (2021). Scapular Retraction under Adduction Load: An Alternative to Overhead Exercises to Activate Infraspinatus, Upper, and Lower Trapezius in Subjects with and without Shoulder Pain. International Journal of Environmental Research and Public Health, 18(17), 9251. https://doi.org/10.3390/ijerph18179251






