Abstract
People with dementia (PwD) occupy around 25% of the hospital beds. Once PwD are admitted to hospitals, their cognitive impairment is not considered in most of the cases. Thus, it causes an impact on the development of the disease becoming a stressful situation as care plans are not adapted to PwD. The aim of this study was to explore the published core elements when designing a dementia care pathway for hospital settings. A scoping review was conducted to provide an overview of the available research evidence and identify the knowledge gaps regarding the topic. This review highlights person-centered care, compassionate care and end-of-life process as some of the key elements that should integrate the framework when designing a dementia care pathway. Architectonical outdoor and indoor hospital elements have also been found to be considered when adapting the healthcare context to PwD. Findings provide information about the key points to focus on to successfully design dementia interventions in hospital environments within available resources, mostly in those contexts in which national dementia plans are in its infancy. Hospitals should transform their patients’ routes and processes considering the increasing demographic changes of people with cognitive impairment.
1. Introduction
1.1. Background
Dementia population data predictions will continue to increase in the next decades. The International Alzheimer’s Association estimates that 75.6 million people will live with dementia in 2030, reaching 135.5 million in 2050 [1]. The world economic impact of neurodegenerative diseases in 2020 was estimated in more than 1.2 trillion US dollars corresponding to the 80% of such investments to Europe and North America [2]. Alzheimer’s disease and other dementias represent the highest percentage of neurodegenerative diseases [3]. Consistent with this, several healthcare systems worldwide have implemented specific Dementia National Plans [4] for years, while countries such as Spain, among other European nations, are still in its early stages with its first Alzheimer’s and Dementia Plan for the period 2019–2023 [5].
The number of people with dementia (PwD) being admitted in emergency services continues rising. In countries, such as England, the number of admitted PwD has increased more than 35% in five years [6]. Furthermore, PwD are three-fold higher than those without a diagnosis of any type of dementia of contracting COVID-19, with a higher risk associated to develop a severe form of COVID-19 requiring hospitalization [7]. Therefore, the need of transforming health environments into dementia-oriented settings remains urgent. Governments at worldwide level have expressed their commitment to share systematic approaches to prevent, diagnose and treat dementia and are developing plans to achieve specific goals to create dementia-friendly environments in healthcare facilities and outdoors environments [8].
1.2. Dementia Care Pathways
Care pathways (CP) are implemented by adapting clinical practice guidelines or protocols to the actual and specific functioning in one health institution [9], in order to provide the sequence of actions necessary to achieve objectives efficiently reducing variability in clinical practice [10,11]. CPs are developed by multidisciplinary teams, therefore guiding professionals to better understand their roles and responsibilities in improving the level of care provided [12].
Hospitalization has shown to be a challenging time for those whose dementia disease makes it difficult for them to adapt to an unfamiliar environment and unknown people, such as healthcare staff [13]. This situation contributes in making PwD have almost double hospital stays per year than any other group of older people [14]. In terms of economic analysis, cost-related dementia hospitalization is estimated to be almost three times higher compared with non-dementia patients [15]. Thus, evidence has shown that implementation of clinical pathways (CP) in hospitals decreases the length of stay as well as other avoidable medical costs [16,17]. However, most of the literature about dementia care pathways has been studied and piloted in those 15% worldwide countries that account for a concise dementia national plan [18]. These national plans are of high importance as compared with international or any other initiative. These are culturally and demographically the most specific strategies to promote public awareness of dementia, improving the quality of health care, social care and support for PwD and their families. Table 1 shows the list of countries that account for a dementia national plan.

Table 1.
Countries with a national dementia plan [18].
1.3. Dementia-Friendly Interventions
Dementia-friendly environment interventions have helped to design adapted environments for PwD considering their experiences, common behaviors, habits and enablers to facilitate their daily routines [19]. These interventions have contributed to tackle the belief of considering health organizations as unknown and not friendly environments. Different initiatives have been successfully implemented in North European countries for being inclusive with this population, where laws, policies and strategies to support PwD are stablished [20,21]. In these regions, dementia-friendly hospitals and healthcare centres can be found as an architectonical and cultural adaptation to PwD [22].
Findings from studies conducted in those dementia culturally friendly contexts cannot be always generalized to all countries, as the healthcare systems are likely to be different in terms of healthcare staff training and ratios per patient, work practices, social and economic administrations, infrastructure, legislations and regulations and the culture of each country.
Thus, the present scoping review aimed to determine the scope and volume of available research conducted about care pathways and hospital friendly interventions for people with dementia that can be implemented in those contexts and settings in which these interventions at national level are still in their early stages.
2. Materials and Methods
The scoping review was the type of literature search selected by following the PRISMA Extension for Scoping Reviews-PRISMA-ScR [23] and the Joanna Briggs Institute guidance [24], with the purpose to identify relevant publications, both scientific and grey literature, regarding the key concepts of the topic explored with direct implications into healthcare settings. This review aims to explore how the design of specific interventions for PwD in healthcare settings can contribute to the wellbeing of PwD during their stay in a hospital, according to the available literature published [25]. Researchers understood that publications could have been generated within specific contexts either as a white paper or as a protocol or guideline format. Scoping reviews are particularly useful to answer a broader and more flexible question, characterized by elements of the population, concepts, and contexts [26]. The search was divided in two subphases: (1) dementia care pathway search and (2) dementia-friendly hospital search. Three different databases (Pubmed, Scopus and Web of Science-WoS) were used to analyze evidence published in English and Spanish during the second quarter of 2020. Two researchers independently reviewed titles and abstracts of the identified articles. Researchers did not use any software for collecting data from manuscripts. Inclusion criteria were studies related to dementia care pathways and dementia-friendly hospital environments that were published in peer-reviewed journals. The inclusion criteria for the grey literature search were national and international associations, societies, and entities that support PwD and families.
Results gathered from this review may support healthcare staff to identify the critical points of healthcare institutions to be transformed into dementia-friendly settings. It is also part of a broader project that aims to design and pilot a dementia care pathway into hospital settings in Spain toward improving the wellbeing of PwD and their family caregivers during hospitalization.
2.1. Data Extraction and Analysis
A standardized form was used to summarize the content of each article. The variables extracted were authors, year, topic, place, participants/studies, type of study, methods and findings. Search results for all databases were compiled. Duplicates and nonrelated papers were excluded. Titles and abstracts of the remaining papers were assessed against the inclusion and exclusion criteria independently by both authors. The resulting papers were clustered, and disagreements were resolved through discussion based on the full text article.
2.2. Study Selection
2.2.1. Subphase 1. Dementia Care Pathway Review
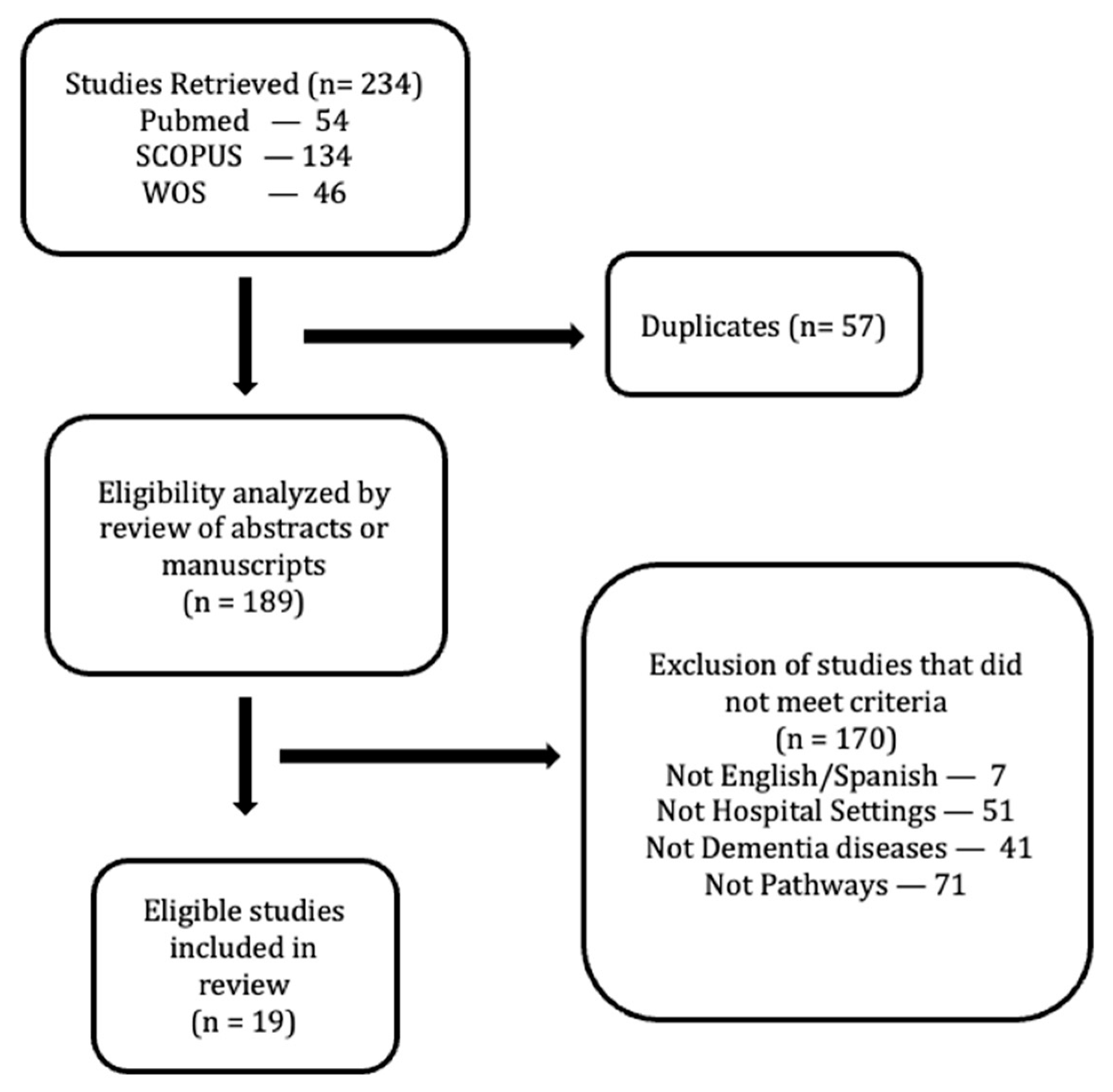
The first step consisted of a literature review about clinical pathways in relation to PwD by using the following keywords in English and Spanish: (“dementia” OR “Alzheimer”) AND (“care pathway” OR “integrated care pathway” OR “critical pathway” OR “clinical pathway”). The exclusion criteria were studies not directly or indirectly related with dementia as well as processes and procedures focused on non-dementia syndromes, interventions related to pharmacological treatments and those not oriented to hospital pathways. The inclusion criteria were studies directly or indirectly related with the evaluation, implementation and design of care pathways for PwD in healthcare settings. There was no limitation in years and other categories. A total amount of 19 research articles were selected and reviewed in depth (Figure 1).
Figure 1.
Inclusion search flow diagram for studies in dementia care pathway in this review.
2.2.2. Subphase 2. Review of Evidence about Dementia Friendly Hospital
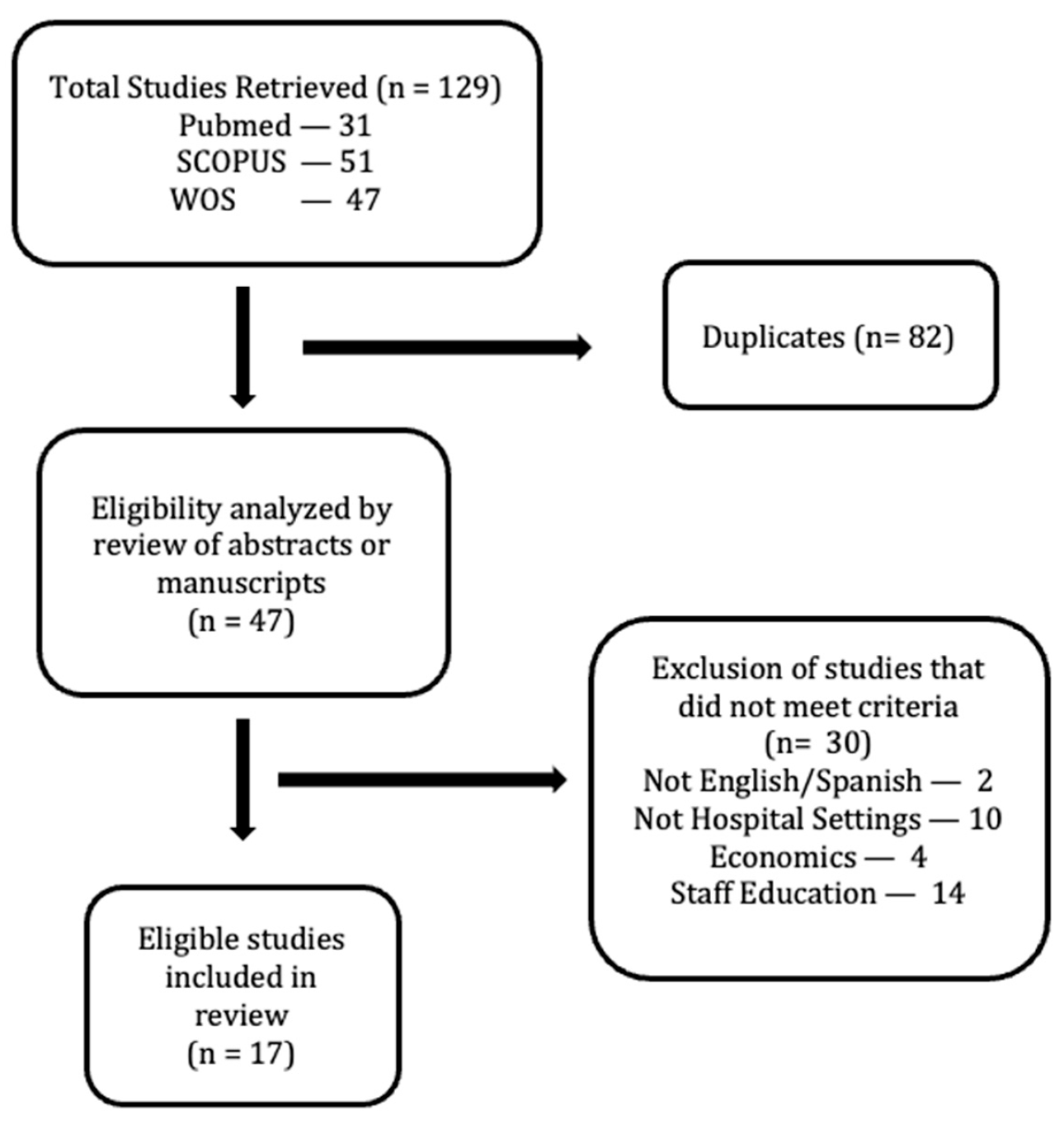
At this part, the keywords used in English and Spanish were: (“dementia-friendly”) AND (“dementia” OR “Alzheimer”) AND (“hospital” OR “clinical setting” OR “healthcare setting”). The searches were completed in the same databases: PubMed, Scopus and WoS. Inclusion criteria were studies that discussed the implementation and evaluation of dementia-friendly actions directly or indirectly related with healthcare settings. The exclusion criteria were those articles not directly or indirectly related with healthcare settings. There was no limitation in years and other categories. A total amount of 17 research articles were selected and reviewed in depth (Figure 2).
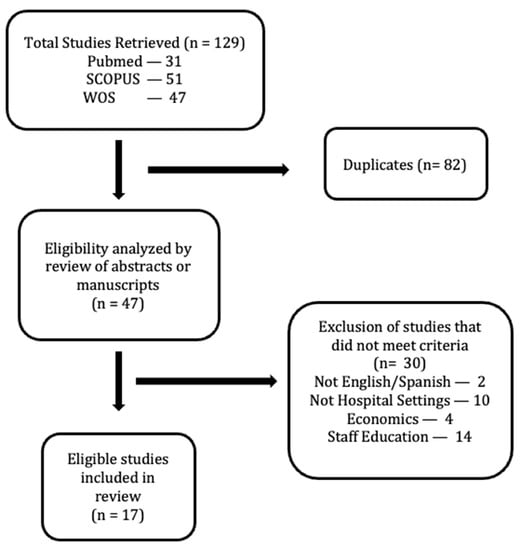
Figure 2.
Inclusion search flow diagram for studies in dementia-friendly hospital adaptation in this review.
2.2.3. Grey Literature Review
Guidelines and Protocols about dementia care interventions in different countries as well as white papers, best practice statements and reports from scientific organizations and funded projects regarding the topic were searched. Web based resources, reports and other documents were explored in order to complete the findings from the databases. The keywords were introduced in Google and Google scholar. The search was conducted in Spanish and English, collecting complementary resources to be used in the later design of the care pathway.
3. Results
3.1. Dementia Care Pathway
Most of the published literature about clinical pathways are focused on the medical approach of diagnosis and treatment [27,28,29] while others are focused on the statistical impact of dementia in health economics [13,30]. It is due to the differences between countries and institutions about precise diagnosis, treatment and care based on the healthcare system organization in the different levels of care. Although it is a relevant issue, it is not the main scope of this review.
One of the most important issues about PwD admission to clinical settings is the length of stay in hospitalization, as it is directly related with unintentional harmful events. However, little attention is paid about what determines wellbeing and length of stay in hospitals for PwD in care pathways. According to the findings, the key points that directly impact hospital stay of PwD are: medication for neurological, cognitive and psychiatric disturbance, visits to other departments within hospital, and invasive procedures [31,32]. But facilitators that contributed to the early discharge of the patient were: family members living with PwD, caregivers supporting the primary caregiver and living in their own home. Another identified element in literature that can contribute to the earlier discharge from hospital facilities of PwD was staff organization. Successful activities organized by those interdisciplinary teams were: establishing a diagnosis, regular meetings led by physicians & nurses with the caregiver & patient to explain future and daily tasks, cares and other activities during hospital stay [33,34,35]. In those examples, nurses are involved in education and symptom management or behavior problems more than physicians, which results in an important role when talking about building confident relationships [36].
One of the most common situations lived by PwD in hospital settings corresponds with the last stages of their lives. Authors stressed end-of-life process as a relevant topic in literature when searching information about dementia care pathways. Scientific societies that support this issue advocate for (a) clear communication, (b) compassionate care, (c) multidisciplinary approach and (d) debriefing sessions for staff. Clear communication is needed in the last period of life from staff to relatives, tutors and the affected person. It facilitates decision-making in accordance with the person’s wishes and needs, including the possibility of choosing the settings, considering the situation of the person. Compassionate care is the gold standard when performing palliative care and healthcare staff should be trained in order to be able to understand PwD and relatives’ needs. This care should be performed by multidisciplinary teams, whose members need to be trained in approaching the person and relatives from different perspectives to ensure quality end-of-life care. This stage of care may increase stress in healthcare staff. Debriefing sessions may help them confront and discuss the lived situation to perform new strategies as a process of continuous improvement [37,38,39,40]. As it has been mentioned before, it is necessary to evaluate PwD from a multidisciplinary perspective and take decisions based on PwD wishes and last evidence. Thus, in advance stages of the disease, medical interventions may not improve quality of life of PwD and neither extend years of life but may cause more suffering to PwD and caregivers along the process such as using PEG feeding [31]. It is a relevant issue as not all countries and rural areas count with structured and equipped healthcare services to attend end-of-life processes at home, and therefore they live their last days in hospital settings.
But barriers should be considered when implementing new initiatives for PwD in healthcare facilities. The negative indirect outcomes found by implementing dementia CPs was that staff usually reports higher workload as processes take longer, delaying other activities. Another common issue found is the lack of primary care coordination. Prevention is not performed equally in all cultures and contexts, thus adapting processes to prevent unnecessary hospital admissions requiring collaboration from primary care institutions forcing unnecessary admissions of PwD in hospital settings. At the same time, many difficulties have been described about care coordination between outpatient and inpatient services, as aligning goals between different healthcare facilities is a challenge in healthcare systems worldwide [41,42].
Evidence published specifically about Dementia CPs in Spanish were not found. Table 2 Dementia Care Pathway Search shows the literature findings about the dementia care pathway.

Table 2.
Dementia Care Pathway Search.
3.2. Dementia-Friendly Hospital
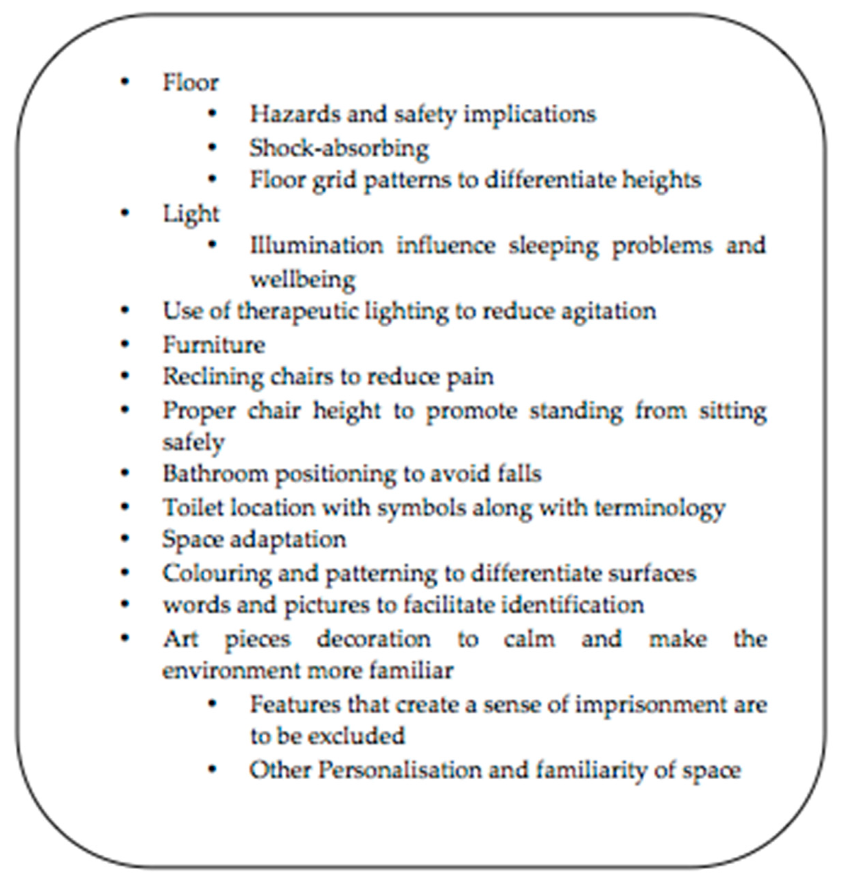
As stated by Innes [43] in a comparative prospective study including PwD and healthcare staff, dementia-friendly interventions in hospital settings should start from changing the culture of the institution. Staff training and architectonical adaptation to PwD are specific actions to take when changing the culture of institutions to be more dementia inclusive. Following the perspective of Waller & Masterson [44], the key elements to be considered when adapting an acute hospital environment should encourage meaningful activities, including caregivers, fostering easy decision-making based on PwDs’ wishes. Regarding signposting, legibility (big letters with colorful contrasts), wayfinding, and familiarity of the environment contribute to PwD independency, safety and reduce agitation during hospital stay. Dementia-friendly program implementation in healthcare settings have the potential of preventing aggression and incidents in healthcare settings. In order to adapt the physical environment, authors outlined the following items in Figure 3 Key elements for adapting PwD environments [45,46,47].
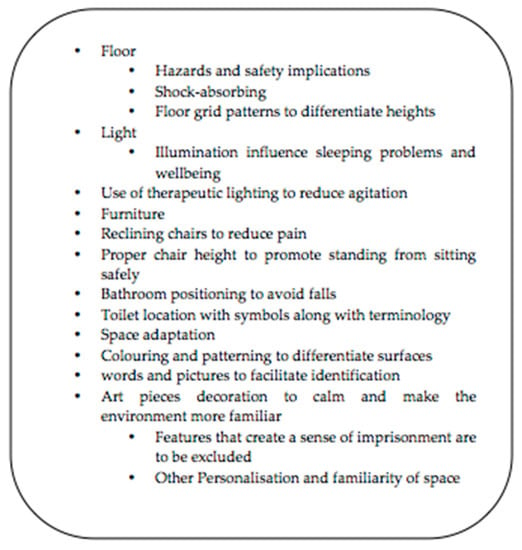
Figure 3.
Key elements for adapting PwD environments.
Not only indoor changes are required when adapting hospital settings to PwD. Outdoor hospital adaptation has to be considered when adapting healthcare settings. Public transport, easy entrance, and physical barriers that surround the hospital infrastructure influence the environment to be more inclusive with PwD and caregivers. Car parking and lack of outdoor seating were difficulties that participants remarked as important for them when accessing hospital facilities in different literature reviews and case studies [48,49], although outdoor spaces, gardens or green and natural spaces have also shown therapeutic effects on PwD, as they promote active engagement and physical and social interaction [50,51,52].
Another important issue when adapting practice to become more friendly with PwD is that staff has to be trained in order to recognize, care and treat signs and symptoms as stated by Palmer [53] in a prospective intervention focused on an educational intervention with 355 healthcare staff. A considerable amount of PwD develops an episode of delirium that can be manifested by “alertness, poor concentration, disorientation, behavior and speech changes, changes in sleeping patterns, mood swings, paranoia and hallucinations” [54], while hospitalized, usually deriving in late hospital discharge and in satisfaction. The impact of a hospital or other healthcare settings not being adapted to PwD is not only negative when the patient accesses the building, but also once the person is hospitalized. In the Okamura study [55], 78.8% of a sample of 74,171 participants over 65 years old responded that they felt anxious about having dementia and not being properly cared. This still occurs when people are diagnosed with dementia, as evidenced by Møller [56] in a qualitative study in which PwD repeated the sentence “if only they could understand me”. Those people believed that staff were not employing enough time to know them and their actions were misunderstood under the umbrella of being diagnosed with dementia. Further than knowing how to care for the different diseases that involve dementia, authors found that healthcare staff needs to develop and train more than just skills and competencies to care for PwD properly but also attitudes for acting one step beyond and elaborating individualized care plans, which are related to compassionate care principles [57]. These added values are related to dementia empathy and an understanding behavior as a positive way of communicating unmet needs, staff experiential learning promotion, support from clinical experts in dementia care, individualized care, psychosocial interventions and confidence for risk management. All these identified values are necessary to be included as core elements when training healthcare staff.
The latest qualitative publications about how to transform a hospital into a dementia-friendly environment outline the importance of the presence of caregivers in daily hospital routines while caring for PwD. Caregivers can act as expert advocates for PwD, contributing with staff to find solutions for best caring [54]. At the same time, other research studies evidenced the importance of practicing meaningful activities toward promoting self-realization and keeping the brain active. These tasks are not only related to self-care but also to cognitive stimulation. Chess practice has been investigated as one of the most stimulating tools for PwD, although it may be difficult for people that are in moderate to advance stages [58].
To achieve all these mentioned adaptations in healthcare settings is necessary to involve different players, not only those who are directly involved in caring for PwD such as healthcare staff and caregivers. Thus, other reviews about dementia-friendly interventions in hospitals have highlighted the importance of the role of the changing agents. The main characteristics identified for this role are (1) supportive peer facilitator, (2) organizational authority, and (3) clinical expertise. These roles need to be present when changing a complete process in a hospital in order to have a positive effect not only in the clinical approach but in the architectonical, economic and cultural situation of the institution once it has been decided to become a dementia-friendly environment [59,60]. Table 3: Dementia Friendly Hospital Search shows the search findings.

Table 3.
Dementia Friendly Hospital Search.
3.3. Dementia Care Pathway & Dementia Friendly Hospital Grey Literature Search
While searching for evidence about how to implement a dementia care pathway in a hospital setting, grey literature emerged as useful information, although none came from the Spanish context. Published care pathways for dementia are usually focused on specific areas such as end-of-life care or primary care [61,62], although less about hospital pathways. However, clinical guidelines and websites detail information about the steps that the PwD and caregiver should follow before, during and after visiting a hospital. Guidelines about how to prepare for a surgery in the case of PwD, what to bring in case you are admitted to the hospital, or how to facilitate the work of hospital staff are available on certain platforms that may also be helpful for other healthcare institutions when building a dementia-friendly culture [63,64]. Institutions such as Alzheimer’s Scotland [65] has available tools that help PwD and caregivers when they are admitted to healthcare facilities. Knowing the person that staff is caring for is important in order to promote person-centered care instead of impersonalized care. Alzheimer Scotland introduced the tool “Getting to know me” in order to collect relevant information about what really matters to the cared person, in order to have different tools and resources to perform individualized care, based on information provided by the patient or the caregiver.
National and international guidelines found were mostly based on the implementation and practical information when designing a dementia care pathway. Relevant guidelines were found such as the ones by Grey [66] and Halsall & Mcdonald [67] designed for healthcare centers and other living spaces for PwD and paying special attention to users’ feedback and architectonical elements. However other institutions have published information focused not only on the design but in the care process such as by the National Collaborating Centre for Mental Health [68]. It remarks dementia key principals from NHS England’s Well Pathway for Dementia (diagnosing, living, supporting and dying well). Under this paradigm, a complete dementia care pathway was developed following the main quality statements of NICE Quality Standards on dementia [69]. Seven quality statements are the mandates for caring for PwD: (1) raising awareness-health promotion interventions, (2) diagnosis, (3) advanced care planning, (4) coordinating care, (5) activities to promote wellbeing, (6) managing distress, and (7) supporting caregivers. Additionally, the Palliare Best Practice Statement used by the Alzheimer’s Europe and produced by the partners of a European funded Project called Palliare Project as a white paper was included in our search. This document reflects about six overarching principles used as a reference when caring for PwD [70]. It advocates for the rights, advanced dementia care, symptoms management, quality of life, family support and advancing practice.
4. Discussion
According to the literature reviewed, different, although not many, initiatives have been conducted in practice in relation to the development of dementia care pathways worldwide. PwD are differently cared for depending on the country, context and culture. Thus, available resources may be different in order to perform the best care possible that directly depends on the level of professional health care training, settings, available resources, ratios patient per healthcare staff, awareness about dementia, and government support. Staffing levels through the UNISON survey [71] found that 66% of nurses did not have sufficient time to care properly for patients. They thought that ratios of eight or more patients to one registered nurse (RN) resulted in poorer patient outcomes and higher nurse stress. It has been highlighted as one of the most difficult issues to address when approaching care excellence in dementia care, such as Spanish nurse ratios in hospitals are 12.7 patients per nurse [72]. Due to this high workload for healthcare staff in hospitals, caregivers and families play an important role in PwD care within clinical contexts by contributing to the daily basic care such as hygiene, feeding, oral treatment and supervision to avoid physical restraints. As important as to know how the disease affects the brain, it is important to facilitate the decision-making during hospital stay in order to avoid harmful events to the maximum. Caregivers still play an important role in several Hispanic–Latin cultures and therefore need to be taken into consideration when adapting a hospital environment, as they can sometimes express and act on behalf of those affected by dementia in moderate to severe phases of diseases. Caregivers do not only help staff in understanding PwD, but they also contribute to stimulate the patient from a nonpharmacological intervention, using resources such as mindfulness, physical and cognitive stimulation [73]. This means that this theoretical approach of adapting institutions to PwD still seems to be ideal in certain contexts as evidence is also showing that insufficient staff in hospitals will bring negative effects to PwD and other patients hospitalized as higher workload will be present [74].
One of the critical points when adapting healthcare settings to become more dementia-friendly are the standards and evaluation methodology. Along the review, little has been mentioned about how to measure if a healthcare setting meets a minimum criteria to ensure it is a dementia-friendly environment. But implementing best practices from different studies into specific context is not enough. However, the most used tool to transform healthcare settings into dementia-friendly is the King’s Fund tool [44]. Although it is mainly focused on the architectonical design, it provides a clear guideline for designing and evaluating a healthcare setting. It has been widely used in the United Kingdom but initiatives in different European contexts are being piloted [75].
The vast majority of dementia care pathway interventions included in this study have followed similar structures in which communication, coordination of care, evaluation and use of appropriate resources stimulate the transformation of a healthcare setting into a dementia-friendly environment. One of the critical points when adapting and changing the culture of an institution is to identify the changing agents [59]. These main actors have the capability to influence at the different hierarchical levels of the institution in order to facilitate the implementation and use of resources needed to adapt the hospital environment to PwD. As an example of easy decision making in healthcare institutions, those identified as “flat organizations” are used as an example of management in which the implementation of dementia care pathways and dementia friendly initiatives can be easily implemented. Parallel to this situation, those institutions in which evidence-based practice is not fostered and continuously updated, there is a strong hierarchical management structure and culturally there is no support to build dementia inclusive contexts. Thus, it becomes more difficult to successfully implement these initiatives.
The paradigm named as prudent healthcare has been found in literature when talking about efficiency and fostering dementia inclusivity settings [76]. It is clear that improving dementia care is still not a priority in certain cultures due to the lack of specific implementation of dementia plans worldwide. The COVID-19 health, social, economic and political crises make this issue more complex. However, it is important to remark that PwD are one of the most vulnerable population. During hospitalization, they should not be treated only as patients infected by COVID-19. Risk of delirium, self-harm and behavior-difficult situations may cause worsening in dementia disease and COVID-19 infection during isolation. Thus, a different approach and care pathway should be developed in healthcare institutions in order to build a response to COVID-19 in PwD [77]. Several authors have shown their findings highlighting the importance of investing in dementia workforce training, changes in thinking and leadership, continuous improvement, respecting and engaging the workforce as valuable contributors of new ideas, and vigorously pursuing the needs and experiences of service users [78,79]. At the same time, it has been clearly stated the importance of architectonical adaptation in terms of light, floor and furniture, in order to avoid daily routines disturbances [80]. But the combination of the core values promoted by prudent healthcare and dementia friendly paradigms can potentially be useful for all healthcare institutions as it aligns with the strengths of focusing on dementia care but optimizing the available resources with special attention to staff training between other interventions mentioned before. This approach can be an efficient strategy to improve dementia care within available resources in order to perform little steps toward achieving dementia awareness in the different healthcare systems worldwide.
5. Limitations
Despite the intention of including all relevant literature, we assume the possibility that studies and relevant grey literature may not have been identified as it is a limitation in scoping reviews. Furthermore, this review was not intended to be an exhaustive review of the literature but to concentrate on the key themes and necessary elements to focus on when starting to change dementia-friendly healthcare environments. This review includes studies from different methodological designs (qualitative and quantitative studies, questionnaires, reviews, reports, case studies, etc.). Another important limitation is the non-homogeneous time of observation from different geographic areas in the different included studies of this review. Although we have tried to include mostly papers based in hospital settings, studies that have not been conducted in hospitals were included, as it clearly shows interventions that can be potentially applied to any healthcare facility. Thus, this paper brings an overview perspective of the first steps to consider when designing a dementia inclusive intervention in healthcare settings.
6. Conclusions
Developing CPs is a complex, iterative process. Integrated care pathways should be practical, adaptable to different care contexts, and lead to improved patient, family, and staff outcomes. This type of approach will help staff personalize interventions for individuals with dementia and it will make future institutions developing a framework to get to know the patients better, from an individual perspective [81]. Thus, care quality will increase as the current paradigm is changing to become more person-centered. Person recognition, collaboration, and validation of their reality and supporting PwD to live a life with dignity will contribute to switch the current meaning of being hospitalized. This paper summarizes the bullet points to focus on when adapting a healthcare setting to PwD, which are changing the mindset of the staff by developing a clear path that can guide PwD admissions into hospitals, and moreover, the importance of the environment in facilitating or worsening the situation of PwD and their caregivers. According to the NICE [69] quality guidelines, CPs should be focused on end-of-life processes, dementia care training for healthcare, and nonhealthcare staff in order to develop dementia awareness and support for caregivers during admissions and stimulating PwD. Architectonical adaptation needs to be considered, specifically in terms of light, floor, furniture, noise, wayfinding, signposting when referring to indoor settings and green and natural areas, easy entrance, architectonical barriers, and comfort referring to outdoor areas.
Dementia care pathways are involving inclusiveness for PwD and families in developing new ways of care in which joint decisions can be found in order to build a collaborative working strategy. Future research should concentrate on evaluating the implementation of dementia-friendly care pathways in order to find differences and similarities among healthcare settings to help building dementia-friendly healthcare awareness. This literature review may be a readily scalable example for enabling hospitals and healthcare staff to foster dementia care excellence based in the PwD recognition, which can result in significant physical and psycho-social benefits for those living with Alzheimer’s and other dementia diseases and their caregivers.
Author Contributions
Conceptualization, J.R.-G. and M.L.-C.; methodology, J.R.-G. and M.L.-C.; validation J.R.-G. and.; formal analysis, J.R.-G. and M.L.-C.; investigation, J.R.-G. and M.L.-C.; resources, J.R.-G. and M.L.-C.; data curation, J.R.-G. and M.L.-C.; writing—original draft preparation, J.R.-G. and M.L.-C.; writing—review and editing, J.R.-G.; visualization, J.R.-G.; supervision, M.L.-C.; project administration, M.L.-C.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Prince, M.; Comas-Herrera, A.; Knapp, M.; Guerchet, M.; Karagiannidou, M. World Alzheimer Report 2016: Improving Healthcare for People Living with Dementia: Coverage, Quality and Costs Now and in the Future; Alzheimer’s Disease International (ADI): London, UK, 2016. [Google Scholar]
- Prince, M.; Knapp, M.; Guerchet, M.; McCrone, P.; Prina, M.; Comas-Herrera, A.; Wittenberg, R.; Adelaja, B.; Hu, B.; King, D.; et al. Dementia UK: Update Second Edition. Report Produced by King’s College London and the London School of Economics for the Alzheimer’s Society; Alzheimer’s Society: London, UK, 2014. [Google Scholar]
- Alzheimer’s Association Alzheimer’s Disease Facts and Figures. Alzheimer’s Dementia. 2021. Available online: https://www.alz.org/media/documents/alzheimers-facts-and-figures.pdf (accessed on 6 August 2021).
- World Health Organization. Global Action Plan on the Public Health Response to Dementia 2017–2025; World Health Organisation: Geneva, Switzerland, 2017. [Google Scholar]
- Ministerio de Sanidad, Consumo y Bienestar Social. Plan Integral de Alzheimer y Otras Demencias 2019–2023. 2019. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/docs/Plan_Integral_Alhzeimer_Octubre_2019.pdf (accessed on 6 March 2021).
- Torjesen, I. Figures show big increase in emergency admissions for dementia patients. BMJ 2020, 368, m249. [Google Scholar] [CrossRef]
- Numbers, K.; Brodaty, H. The effects of the COVID-19 pandemic on people with dementia. Nat. Rev. Neurol. 2021, 17, 69–70. [Google Scholar] [CrossRef] [PubMed]
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2019: Highlights (ST/ESA/SER.A/430); United Nations: New York, NY, USA, 2019. [Google Scholar]
- Simó, M.R.; Aledo, V.S.; López, P.R.; Cuéllar, E.R.; Albasini, J.L.A. Guías y vías clínicas,¿ existe realmente diferencia? Cirugía Española 2010, 88, 81–84. [Google Scholar] [CrossRef] [PubMed]
- Kinsman, L.; Rotter, T.; James, E.; Snow, P.; Willis, J. What is a clinical pathway? Development of a definition to inform the debate. BMC Med. 2010, 8, 31. [Google Scholar] [CrossRef] [PubMed]
- Panella, M.; Marchisio, S.; Di Stanislao, F. Reducing clinical variations with clinical pathways: Do pathways work? Int. J. Qual. Health Care 2003, 15, 509–521. [Google Scholar] [CrossRef] [PubMed]
- Lawal, A.K.; Rotter, T.; Kinsman, L.; Machotta, A.; Ronellenfitsch, U.; Scott, S.D.; Goodridge, D.; Plishka, C.; Groot, G. What is a clinical pathway? Refinement of an operational definition to identify clinical pathway studies for a Cochrane systematic review. BMC Med. 2016, 14, 35. [Google Scholar] [CrossRef] [PubMed]
- Kazui, H.; Hashimoto, M.; Nakano, Y.; Matsumoto, K.; Yamamura, S.; Nagaoka, K.; Mori, E.; Endo, H.; Tokunaga, H.; Ikejiri, Y.; et al. Effectiveness of a clinical pathway for the diagnosis and treatment of dementia and for the education of families. Int. J. Geriatr. Psychiatry 2004, 19, 892–897. [Google Scholar] [CrossRef]
- Shepherd, H.; Livingston, G.; Chan, J.; Sommerlad, A. Hospitalisation rates and predictors in people with dementia: A systematic review and meta-analysis. BMC Med. 2019, 17, 130. [Google Scholar] [CrossRef]
- Briggs, R.; Coary, R.; Collins, R.; Coughlan, T.; O’Neill, D.; Kennelly, S.P. Acute hospital care: How much activity is attributable to caring for patients with dementia? QJM Int. J. Med. 2016, 109, 41–44. [Google Scholar] [CrossRef]
- Kim, S.; Losina, E.; Solomon, D.H.; Wright, J.; Katz, J.N. Effectiveness of clinical pathways for total knee and total hip arthroplasty: Literature review. J. Arthroplast. 2003, 18, 69–74. [Google Scholar] [CrossRef]
- Stephen, A.E.; Berger, D.L. Shortened length of stay and hospital cost reduction with implementation of an accelerated clinical care pathway after elective colon resection. Surgery 2003, 133, 277–282. [Google Scholar] [CrossRef]
- Alzheimer’s Disease International Dementia Plans: Policy. 2021. Available online: https://www.alzint.org/what-we-do/policy/dementia-plans/ (accessed on 15 December 2020).
- Davis, S.; Byers, S.; Nay, R.; Koch, S. Guiding design of dementia friendly environments in residential care settings: Considering the living experiences. Dementia 2009, 8, 185–203. [Google Scholar] [CrossRef]
- Quasdorf, T.; Riesner, C.; Dichter, M.N.; Dortmann, O.; Bartholomeyczik, S.; Halek, M. Implementing Dementia Care Mapping to develop person-centred care: Results of a process evaluation within the L eben-QD II trial. J. Clin. Nurs. 2017, 26, 751–765. [Google Scholar] [CrossRef] [PubMed]
- Biglieri, S. Implementing dementia-friendly land use planning: An evaluation of current literature and financial implications for greenfield development in suburban Canada. Plan. Pract. Res. 2018, 33, 264–290. [Google Scholar] [CrossRef]
- Rahman, S.; Swaffer, K. Assets-based approaches and dementia-friendly communities. Dementia 2018, 17, 131–137. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Int. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Peters, M.D.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, R.; Hall, B.J.; Doyle, J.; Waters, E. Scoping the scope of a Cochrane review. J. Public Health 2011, 33, 147–155. [Google Scholar] [CrossRef]
- Colquhoun, H.L.; Levac, D.; O’Brien, K.K.; Straus, S.; Tricco, A.C.; Perrier, L.; Kastner, M.; Moher, D. Scoping reviews: Time for clarity in definition, methods, and reporting. J. Clin. Epidemiol. 2014, 67, 1291–1294. [Google Scholar] [CrossRef]
- Filippini, G. Implementation of an integrated care pathway for dementia in clinical practice: Rationale, design and methodology-the REMIND study. Alzheimers Dement. 2004, 10, 207–208. [Google Scholar] [CrossRef]
- Kua, J.; Chiam, P.C.; Hendriks, M.; Vaingankar, J. P-018: A two-year review of the utility of dementia clinical pathway in a psychogeriatric inpatient unit in Singapore. Alzheimer’s Dementia J. Alzheimer’s Assoc. 2007, 3, S100–S101. [Google Scholar]
- Brodaty, H.; Cumming, R. Dementia services in Australia. Int. J. Geriatr. Psychiatry 2010, 25, 887–995. [Google Scholar] [CrossRef]
- Gervasi, G.; Bellomo, G.; Mayer, F.; Zaccaria, V.; Bacigalupo, I.; Lacorte, E.; Canevelli, M.; Corbo, M.; Di Fiandra, T.; Vanacore, N. Integrated care pathways on dementia in Italy: A survey testing the compliance with a national guidance. Neurol. Sci. 2020, 41, 917–924. [Google Scholar] [CrossRef] [PubMed]
- Bouza, C.; Martínez-Alés, G.; López-Cuadrado, T. Effect of dementia on the incidence, short-term outcomes, and resource utilization of invasive mechanical ventilation in the elderly: A nationwide population-based study. Crit. Care 2019, 23, 291. [Google Scholar] [CrossRef]
- Traynor, V.; Britten, N.; Burns, P. Developing the delirium care pathways. J. Res. Nurs. 2016, 21, 582–596. [Google Scholar] [CrossRef]
- Coleman, A.M. End-of-life issues in caring for patients with dementia: The case for palliative care in management of terminal dementia. Am. J. Hosp. Palliat. Med. 2012, 29, 9–12. [Google Scholar] [CrossRef] [PubMed]
- Ghiotti, C. The Dementia End of Life Care Project (DeLCaP): Supporting families caring for people with late stage dementia at home. Dementia 2009, 8, 349–361. [Google Scholar] [CrossRef]
- Volpe, U.; Amin, H.; Ayinde, O.O.; Burns, A.; Chan, W.C.; David, R.; Dejanovic, S.D.; Djokic, G.; Eraslan, D.; Fischer, G.A.L.; et al. Pathways to care for people with dementia: An international multicentre study. Int. J. Geriatr. Psychiatry 2020, 35, 163–173. [Google Scholar] [CrossRef]
- Sampson, E.L.; Ritchie, C.W.; Lai, R.; Raven, P.W.; Blanchard, M.R. A systematic review of the scientific evidence for the efficacy of a palliative care approach in advanced dementia. Int. Psychogeriatr. 2005, 17, 31–40. [Google Scholar] [CrossRef]
- Waterman, L.Z.; Denton, D.; Minton, O. End-of-life care in a psychiatric hospital. BJPsych Bull. 2016, 40, 149–152. [Google Scholar] [CrossRef] [PubMed]
- Martin, A.; O’Connor, S.; Jackson, C. A scoping review of gaps and priorities in dementia care in Europe. Dementia 2020, 19, 2135–2151. [Google Scholar] [CrossRef]
- Minghella, E.; Schneider, K. Rethinking a framework for dementia 2: A new model of care. In Working with Older People; Emerald Group Publishing Limited: Bingley, UK, 2012. [Google Scholar]
- Afzal, N.; Buhagiar, K.; Flood, J.; Cosgrave, M. Quality of end-of-life care for dementia patients during acute hospital admission: A retrospective study in Ireland. Gen. Hosp. Psychiatry 2010, 32, 141–146. [Google Scholar] [CrossRef]
- Tang EY, H.; Price, C.; Stephan BC, M.; Robinson, L.; Exley, C. Gaps in care for patients with memory deficits after stroke: Views of healthcare providers. BMC Health Serv. Res. 2017, 17, 1–9. [Google Scholar] [CrossRef]
- Tropea, J.; LoGiudice, D.; Liew, D.; Roberts, C.; Brand, C. Caring for people with dementia in hospital: Findings from a survey to identify barriers and facilitators to implementing best practice dementia care. Int. Psychogeriatr. 2017, 29, 467–474. [Google Scholar] [CrossRef]
- Innes, A.; Kelly, F.; Scerri, C.; Abela, S. Living with dementia in hospital wards: A comparative study of staff perceptions of practice and observed patient experience. Int. J. Older People Nurs. 2016, 11, 94–106. [Google Scholar] [CrossRef] [PubMed]
- Waller, S.; Masterson, A. Designing dementia-friendly hospital environments. Future Hosp. J. 2015, 2, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Parke, B.; Boltz, M.; Hunter, K.F.; Chambers, T.; Wolf-Ostermann, K.; Adi, M.N.; Feldman, F.; Gutman, G. A scoping literature review of dementia-friendly hospital design. Gerontologist 2017, 57, e62–e74. [Google Scholar] [CrossRef] [PubMed]
- Waller, S.; Masterson, A.; Evans, S.C. The development of environmental assessment tools to support the creation of dementia friendly care environments: Innovative practice. Dementia 2016, 16, 226–232. [Google Scholar] [CrossRef]
- Parke, B.; Hunter, K.F. The dementia-friendly emergency department: An innovation to reducing incompatibilities at the local level. In Healthcare Management Forum; SAGE Publications: Los Angeles, CA, USA, 2017; Volume 30, pp. 26–31. [Google Scholar]
- Van den Berg, M.E.; Winsall, M.; Dyer, S.M.; Breen, F.; Gresham, M.; Crotty, M. Understanding the Barriers and Enablers to Using Outdoor Spaces in Nursing Homes: A Systematic Review. Gerontologist 2020, 60, e254–e269. [Google Scholar] [CrossRef]
- Xidous, D.; Grey, T.; Kennelly, S.P.; McHale, C.; O’Neill, D. Dementia Friendly Hospital Design: Key Issues for Patients and Accompanying Persons in an Irish Acute Care Public Hospital. HERD 2020, 13, 48–67. [Google Scholar] [CrossRef]
- De Boer, B.; Hamers, J.P.; Zwakhalen, S.M.; Tan, F.E.; Beerens, H.C.; Verbeek, H. Green care farms as innovative nursing homes, promoting activities and social interaction for people with dementia. J. Am. Med Dir. Assoc. 2017, 18, 40–46. [Google Scholar] [CrossRef]
- Bossen, A. The importance of getting back to nature for people with dementia. J. Gerontol. Nurs. 2010, 36, 17–22. [Google Scholar] [CrossRef]
- Brawley, E.C. Designing successful gardens and outdoor spaces for individuals with Alzheimer’s disease. J. Hous. Elder. 2007, 21, 265–283. [Google Scholar] [CrossRef]
- Palmer, J.L.; Lach, H.W.; McGillick, J.; Murphy-White, M.; Carroll, M.B.; Armstrong, J.L. The Dementia Friendly Hospital Initiative education program for acute care nurses and staff. J. Contin. Educ. Nurs. 2014, 45, 416–424. [Google Scholar] [CrossRef][Green Version]
- Fitzpatrick, L. Practical strategies to help develop dementia-friendly hospital wards. Nurs. Older People 2018, 30, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Okamura, T.; Sugiyama, M.; Inagaki, H.; Murayama, H.; Ura, C.; Miyamae, F.; Edahiro, A.; Motokawa, K.; Awata, S. Anticipatory anxiety about future dementia-related care needs: Towards a dementia-friendly community. Psychogeriatrics 2019, 19, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Møller, J.; Pedersen, B.D.; Olsen, R.B.; Wilson, R.L.; Hounsgaard, L. “If only they could understand me!” Acute hospital care experiences of patients with Alzheimer’s disease. Dementia 2018, 19, 1471301218820483. [Google Scholar]
- Iaboni, A.; Cockburn, A.; Marcil, M.; Rodrigues, K.; Marshall, C.; Garcia, M.A.; Quirt, H.; Reynoldsm, K.B.; Keren, R.; Flint, A.J. Achieving Safe, Effective and Compassionate Quarantine or Isolation of Older Adults with Dementia in Nursing Homes. Am. J. Geriatr. Psychiatry 2020, 28, 835–838. [Google Scholar] [CrossRef]
- Lillo-Crespo, M.; Forner-Ruiz, M.; Riquelme-Galindo, J.; Ruiz-Fernández, D.; García-Sanjuan, S. Chess Practice as a Protective Factor in Dementia. Int. J. Environ. Res. Public Health 2019, 16, 2116. [Google Scholar] [CrossRef]
- Handley, M.; Bunn, F.; Goodman, C. Dementia-friendly interventions to improve the care of people living with dementia admitted to hospitals: A realist review. BMJ Open 2017, 7, e015257. [Google Scholar] [CrossRef]
- Brooke, J.; Semlyen, J. Exploring the impact of dementia-friendly ward environments on the provision of care: A qualitative thematic analysis. Dementia 2019, 18, 685–700. [Google Scholar] [CrossRef] [PubMed]
- Abbey, J.; Palk, E.; Carlson, L.; Parker, D. Clinical Practice Guidelines and Care Pathways for People with Dementia Living in the Community; QUT: Brisbane, Australia, 2008. [Google Scholar]
- North West Coast Strategic Clinical Network. Palliative Care Guidelines in Dementia, 2nd ed.; Version 3.9–March 2018; NHS: London, UK, 2018.
- National Institute of Health Aging. Going to the Hospital: Tips for Dementia Caregivers. US Department of Health and Social Services. 2020. Available online: https://www.nia.nih.gov/health/alzheimers (accessed on 10 March 2021).
- Weill Institute of Neuroscience Treatment & Stays. University of San Francisco. 2020. Available online: https://memory.ucsf.edu/treatments-stays (accessed on 10 March 2021).
- Alzheimer’s Scotland Getting to Know Me. 2013. Available online: www.alzscot.org/information_and_resources/information_sheet/3472_getting_to_know_me (accessed on 10 March 2021).
- Grey, T.; Xidous, D.; Kennelly, S.; Mahon, S.; Mannion, V.; De Freine, P.; Dockrell, D.; De Siún, A.; Murphy, N.; Craddock, G.; et al. Dementia Friendly Hospitals from a Universal Design Approach: Design Guidelines; Trinity Haus: Dublin, Ireland, 2018. [Google Scholar]
- Halsall, B.; Mcdonald, R. Design for Dementia-A Guide with helpful guidance in the design of exterior and interior environments. In Liverp. Halsall Lloyd Partnersh; The Halsall Lloyd Partnership: Liverpool, UK, 2015; Available online: https://www.findbookprices.com/isbn/9780992923112/ (accessed on 23 August 2021).
- National Collaborating Centre for Mental Health. The Dementia Care Pathway. Full Implementation Guidance; National Collaborating Centre for Mental Health: London, UK, 2018.
- National Institute for Health and Care Excellence. Dementia Quality Standard; NICE: London, UK, 2019.
- Holmerova, I.; Waugh, A.; MacRae, R.; Veprkova, R.; Sandvide, A.; Hanson, E.; Jackson, G.; Watchman, K.; Tolson, D. Dementia Palliare Best Practice Statement; University of the west of Scotland: Paisley, Scotland, 2016. [Google Scholar]
- UNISON. Running on Empty–NHS Staff Stretched to the Limit; UNISON: London, UK, 2014. [Google Scholar]
- Aiken, L.H.; Sloane, D.M.; Bruyneel, L.; Van den Heede, K.; Griffiths, P.; Busse, R.; Diomidous, M.; Kinnunen, J.; Kózka, M.; Lesaffre, E.; et al. Nurse staffing and education and hospital mortality in nine European countries: A retrospective observational study. Lancet 2014, 383, 1824–1830. [Google Scholar] [CrossRef]
- Cheng, S.-T.; Li, K.-K.; Losada, A.; Zhang, F.; Au, A.; Thompson, L.W.; Gallagher-Thompson, D. The effectiveness of nonpharmacological interventions for informal dementia caregivers: An updated systematic review and meta-analysis. Psychol. Aging 2020, 35, 55–77. [Google Scholar] [CrossRef] [PubMed]
- Scerri, A.; Innes, A.; Scerri, C. Dementia care in acute hospitals—A qualitative study on nurse managers’ perceived challenges and solutions. J. Nurs. Manag. 2020, 28, 399–406. [Google Scholar] [CrossRef]
- Riquelme-Galindo, J.; Lillo-Crespo, M. Developing a dementia inclusive hospital environment using an Integrated Care Pathway design: Research protocol. PeerJ 2021, 9, e11589. [Google Scholar] [CrossRef]
- Tolson, D.; Fleming, A.; Hanson, E.; Abreu, W.; Lillo Crespo, M.; MacRae, R.; Jackson, G.; Touzery, S.H.; Routasalo, P.; Holmerová, I. Achieving Prudent Dementia Care (Palliare): An International Policy and Practice Imperative. Int. J. Integr. Care 2016, 16, 18. [Google Scholar] [CrossRef] [PubMed]
- Alzheimer’s Disease International. COVID-19 and Dementia: Difficult Decisions about Hospital Admission and Triage. 2020. Available online: https://www.alzint.org/u/ADI-position-paper-COVID-19-and-dementia.pdf (accessed on 5 August 2021).
- Richardson, B.; Kitchen, G.; Livingston, G. What staff know about elder abuse in dementia and the effect of training. Dementia 2004, 3, 377–384. [Google Scholar] [CrossRef]
- Kuske, B.; Luck, T.; Hanns, S.; Matschinger, H.; Angermeyer, M.C.; Behrens, J.; Riedel-Heller, S.G. Training in dementia care: A cluster-randomized controlled trial of a training program for nursing home staff in Germany. Int. Psychogeriatr. 2009, 21, 295–308. [Google Scholar] [CrossRef]
- Passini, R.; Pigot, H.; Rainville, C.; Tétreault, M.H. Wayfinding in a nursing home for advanced dementia of the Alzheimer’s type. Environ. Behav. 2000, 32, 684–710. [Google Scholar] [CrossRef]
- Schumacher, K.L.; Jones, P.S.; Meleis, A.I. Helping elderly persons in transition: A framework for research and practice. In Life Transitions in the Older Adult: Issues for Nurses and Other Health Professionals; Swanson, E.A., Tripp-Reimer, T., Eds.; Springer: New York, NY, USA, 1999; pp. 1–26. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).