Users’ Intention to Continue Using Online Mental Health Communities: Empowerment Theory Perspective
Abstract
1. Introduction
1.1. Background
1.2. Empowerment Theory
1.3. Research Questions
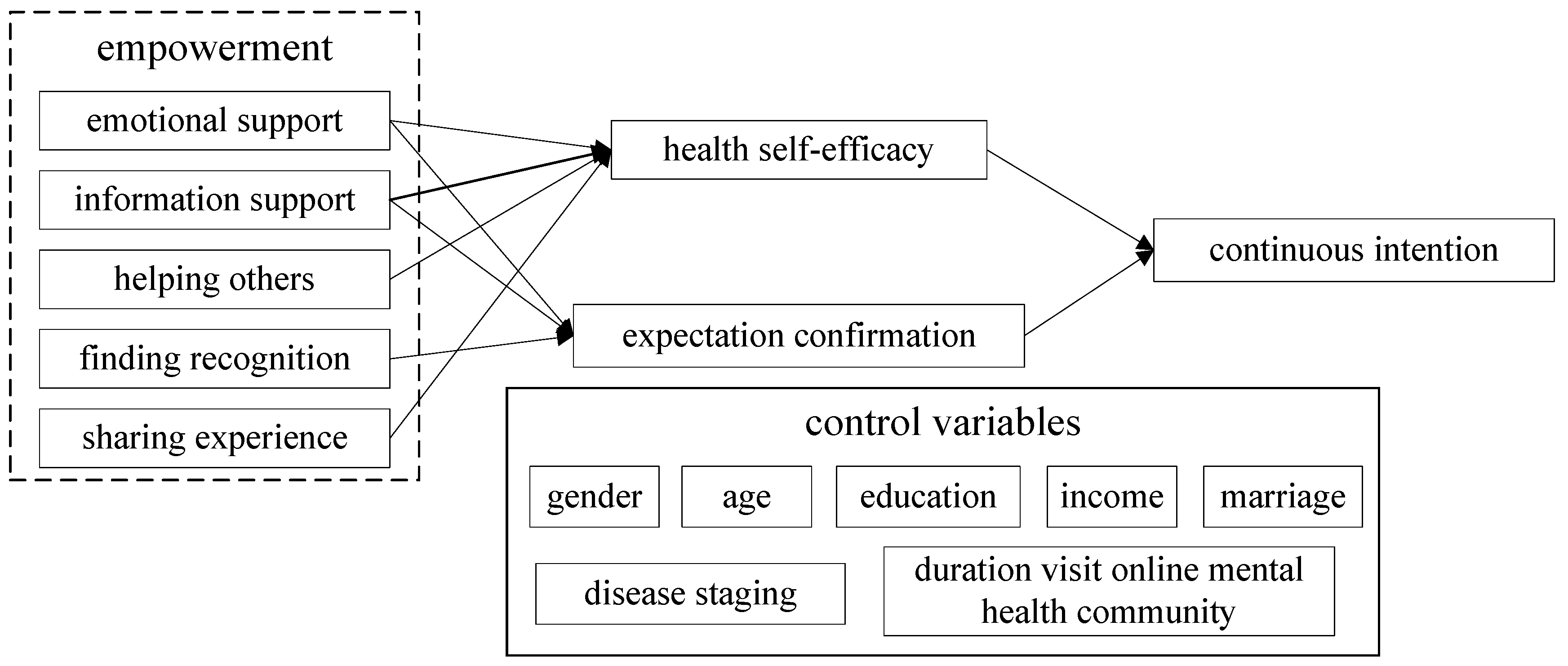
2. Research Hypothesis and Research Model
3. Research Methodology
3.1. Research Context
3.2. Measurement
3.3. Data Collection
4. Data Analysis and Results
4.1. Measurement Model
4.2. Structural Model
5. Research Analysis and Discussion
5.1. Key Findings
5.2. Theoretical Contribution
5.3. Implications
5.4. Limitations and Future Research
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Lawlor, A.; Kirakowski, J. Online support groups for mental health: A space for challenging self-stigma or a means of social avoidance? Comput. Hum. Behav. 2014, 32, 152–161. [Google Scholar] [CrossRef]
- Uden-Kraan, C.; Drossaert, C.; Taal, E.; Seydel, E.R.; van de Laar, M.A.F.J. Participation in online patient support groups endorses patients’ empowerment. Patient Educ. Couns. 2009, 74, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Uden-Kraan, C.V.; Drossaert, C.; Taal, E.; Shaw, B.R.; Seydel, E.R.; van de Laar, M.A.F.J. Empowering processes and outcomes of participation in online support groups for patients with breast cancer, arthritis, or fibromyalgia. Qual. Health Res. 2008, 18, 405. [Google Scholar] [CrossRef]
- Mo, P.K.; Coulson, N.S. Are online support groups always beneficial? A qualitative exploration of the empowering and disempowering processes of participation within HIV/AIDS-related online support groups. Int. J. Nurs. Stud. 2014, 51, 983–993. [Google Scholar] [CrossRef] [PubMed]
- Ziebland, S.; Wyke, S. Health and Illness in a Connected World: How Might Sharing Experiences on the Internet Affect People’s Health? Milbank Q. 2012, 90, 219–249. [Google Scholar] [CrossRef]
- Lehman, A.F.; Kernan, E.; Deforge, B.R.; Dixon, L. Effects of homelessness on the quality of life of persons with severe mental illness. Psychiatr. Serv. 1995, 46, 922–926. [Google Scholar] [PubMed]
- Folsom, D.P.; Hawthorne, W.; Lindamer, L.; Gilmer, T.; Jeste, D.V. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. Am. J. Psychiatry 2005, 162, 370–376. [Google Scholar] [CrossRef] [PubMed]
- Pompili, M.; Lester, D.; Innamorati, M.; Tatarelli, R.; Girardi, P. Assessment and treatment of suicide risk in schizophrenia. Expert Rev. Neurother. 2008, 8, 51–74. [Google Scholar] [CrossRef] [PubMed]
- Coursaris, C.K.; Ming, L. An analysis of social support exchanges in online HIV/AIDS self-help groups. Comput. Hum. Behav. 2009, 25, 911–918. [Google Scholar] [CrossRef]
- McCormack, A. Individuals With Eating Disorders and the Use of Online Support Groups as a Form of Social Support. CIN Comput. Inform. Nurs. 2010, 28, 12–19. [Google Scholar] [CrossRef]
- Uden-Kraan, C.; Drossaert, C.; Taal, E.; Seydel, E.R.; van de Laar, M.A.F.J. Self-Reported Differences in Empowerment Between Lurkers and Posters in Online Patient Support Groups. J. Med. Internet Res. 2008, 10, e18. [Google Scholar] [CrossRef]
- Malik, S.H.; Coulson, N.S. A Comparison of Lurkers and Posters Within Infertility Online Support Groups. CIN Comput. Inform. Nurs. 2011, 29, 564–573. [Google Scholar] [CrossRef] [PubMed]
- Winzelberg, A. The analysis of an electronic support group for individuals with eating disorders. Comput. Hum. Behav. 1997, 13, 393–407. [Google Scholar] [CrossRef]
- Prescott, J.; Rathbone, A.L.; Brown, G. Online peer to peer support: Qualitative analysis of UK and US open mental health Facebook groups. Digit. Health 2020, 6, 2055207620979209. [Google Scholar] [CrossRef]
- Naslund, J.A.; Aschbrenner, K.A.; Marsch, L.A.; Bartels, S.J. The future of mental health care: Peer-to-peer support and social media. Epidemiol. Psychiatr. Sci. 2016, 25, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Conger, J.A.; Kanungo, R.N. The empowerment process. Integration theory and practice. Acad. Manag. J. 1998, 13, 471–482. [Google Scholar]
- Corrigan, P.W.; Giffort, D.; Rashid, F.; Leary, M.; Okeke, I. Recovery as a Psychological Construct. Community Ment. Health J. 1999, 35, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Rogers, E.S.; Chamberlin, J.; Ellison, M.L.; Crean, T. A consumer-constructed scale to measure empowerment among users of mental health services. Psychiatr. Serv. 1997, 48, 1042–1047. [Google Scholar] [CrossRef] [PubMed]
- Rogers, E.S.; Ralph, R.O.; Salzer, M.S. Validating the empowerment scale with a multisite sample of consumers of mental health services. Psychiatr. Serv. 2010, 61, 933. [Google Scholar] [CrossRef]
- Jerry, F. An Exploration of Helping Processes in an Online Self-Help Group Focusing on Issues of Disability. Health Soc. Work 1999, 24, 220–231. [Google Scholar]
- Klemm, P.; Bunnell, D.; Cullen, M.; Soneji, R.; Gibbons, P.; Holecek, A. Online cancer support groups: A review of the research literature. Comput. Inform. Nurs. 2003, 21, 136–142. [Google Scholar] [CrossRef]
- Perron, B. Online support for caregivers of people with a mental illness. Psychiatr. Rehabil. J. 2002, 26, 70. [Google Scholar] [CrossRef] [PubMed]
- Sharf, B.F. Communicating breast cancer on-line: Support and empowerment on the Internet. Women Health 1997, 26, 65–84. [Google Scholar] [CrossRef] [PubMed]
- Broom, A. Virtually Healthy: The Impact of Internet Use on Disease Experience and the Doctor-Patient Relationship. Qual. Health Res. 2005, 15, 325–345. [Google Scholar] [CrossRef]
- Hill, W.; Weinert, C.; Cudney, S. Influence of a computer intervention on the psychological status of chronically ill rural women: Preliminary results. Nurs. Res. 2006, 55, 34–42. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hoybye, M.T.; Johansen, C. Online interaction. Effects of storytelling in an internet breast cancer support group. Psycho-Oncology 2009, 17, 211. [Google Scholar] [CrossRef] [PubMed]
- Powell, J.; Mccarthy, N.; Eysenbach, G. Cross-sectional survey of users of Internet depression communities. BMC Psychiatry 2004, 3, 19. [Google Scholar] [CrossRef] [PubMed]
- Mo, P.K.H.; Coulson, N.S. Empowering processes in online support groups among people living with HIV/AIDS: A comparative analysis of ‘lurkers’ and ‘posters’. Comput. Hum. Behav. 2010, 26, 1183–1193. [Google Scholar] [CrossRef]
- Barak, A.; Boniel-Nissim, M.; Suler, J. Fostering empowerment in online support groups. Comput. Hum. Behav. 2008, 24, 1867–1883. [Google Scholar] [CrossRef]
- Corrigan, P.W.; Larson, J.E.; Ruesch, N. Self-stigma and the “why try” effect: Impact on life goals and evidence-based practices. World Psychiatry 2013, 8, 75–81. [Google Scholar] [CrossRef]
- Corrigan, P.W.; Mark, S.; Ralph, R.O.; Yvette, S.; Lorraine, K. Examining the Factor Structure of the Recovery Assessment Scale. Schizophr. Bull. 2004, 30, 1035–1041. [Google Scholar] [CrossRef]
- Mo, P.K.; Coulson, N.S. Developing a model for online support group use, empowering processes and psychosocial outcomes for individuals living with HIV/AIDS. Psychol. Health 2012, 27, 445–459. [Google Scholar] [CrossRef]
- Hossain, M.A. Assessing m-Health success in Bangladesh: An empirical investigation using IS success models. J. Enterp. Inf. Manag. 2016, 29, 774–796. [Google Scholar] [CrossRef]
- Liu, W.; Fan, X.; Ji, R.; Jiang, Y. Perceived Community Support, Users’ Interactions, and Value Co-Creation in Online Health Community: The Moderating Effect of Social Exclusion. Int. J. Environ. Res. Public Health 2019, 17, 204. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.L.; Hwang, H.; Hawkins, R.; Pingree, S. Interplay of Negative Emotion and Health Self-Efficacy on the Use of Health Information and Its Outcomes. Commun. Res. 2008, 35, 358–381. [Google Scholar]
- Bandura, A. Self-Efficacy: Toward a Unifying Theory of Behavioral Change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef]
- Clark, N.M.; Dodge, J.A. Exploring Self-Efficacy as a Predictor of Disease Management. Health Educ. Behav. 1999, 26, 72–89. [Google Scholar] [CrossRef]
- Andersonbill, E.S. Social Cognitive Determinants of Nutrition and Physical Activity Among Web-Health Users Enrolling in an Online Intervention: The Influence of Social Support, Self-Efficacy, Outcome Expectations, and Self-Regulation. J. Med. Internet Res. 2011, 13, e28. [Google Scholar] [CrossRef]
- Pálsdóttir, A. Information behaviour, health self-efficacy beliefs and health behaviour in Icelanders’ everyday life. Inf. Res. 2008, 13, 334. [Google Scholar]
- Rana, N.P.; Dwivedi, Y.K. Citizen’s adoption of an e-government system: Validating extended social cognitive theory (SCT). Gov. Inf. Q. 2015, 32, 172–181. [Google Scholar] [CrossRef]
- Mo, X.; Deng, Z. Analysis of the Influence of Health Self-efficacy on Health Information Adoption via SNS. Chin. J. Health Stat. 2015, 32, 753–757. [Google Scholar]
- Peng, Y.; Deng, Z.; Wu, J. Analysis of Knowledge Sharing Behavior of Medical Professional Users in Online Health Communities Based on Social Capital and Motivation Theory. Data Anal. Knowl. Discov. 2019, 3, 63–70. [Google Scholar]
- Wu, T.L.; Deng, Z.H.; Feng, Z.C.; Gaskin, D.J.; Zhang, D.L.; Wang, R.X. The Effect of Doctor-Consumer Interaction on Social Media on Consumers’ Health Behaviors: Cross-Sectional Study. J. Med. Internet Res. 2018, 20, e9003. [Google Scholar] [CrossRef]
- Imlawi, J.; Gregg, D. Understanding the satisfaction and continuance intention of knowledge contribution by health professionals in online health communities. Inform. Health Soc. Care 2020, 45, 151–167. [Google Scholar] [CrossRef] [PubMed]
- Oh, H.J.; Lauckner, C.; Boehmer, J.; Fewins-Bliss, R.; Li, K. Facebooking for health: An examination into the solicitation and effects of health-related social support on social networking sites. Comput. Hum. Behav. 2013, 29, 2072–2080. [Google Scholar] [CrossRef]
- Oliver, R.L. A Cognitive Model of the Antecedents and Consequences of Satisfaction Decisions. J. Mark. Res. 1980, 17, 460–469. [Google Scholar] [CrossRef]
- Mittal, V.A.; Tessner, K.D.; Walker, E.F. Elevated social Internet use and schizotypal personality disorder in adolescents. Schizophr. Res. 2007, 94, 50–57. [Google Scholar] [CrossRef]
- Molinillo, S.; Anaya-Sánchez, R.; Liébana-Cabanillas, F. Analyzing the effect of social support and community factors on customer engagement and its impact on loyalty behaviors toward social commerce websites. Comput. Hum. Behav. 2020, 108, 105980. [Google Scholar] [CrossRef]
- Naslund, J.A.; Grande, S.W.; Aschbrenner, K.A.; Elwyn, G. Naturally occurring peer support through social media: The experiences of individuals with severe mental illness using YouTube. PLoS ONE 2014, 9, e110171. [Google Scholar] [CrossRef]
- Frank, R. The “Helper” Therapy Principle. Soc. Work 1965, 10, 27–32. [Google Scholar]
- Wallston, K.A.; Mcminn, M.; Katahn, M.; Pleas, J. The helper-therapy principle applied to weight management specialists. J. Community Psychol. 1983, 11, 58–66. [Google Scholar] [CrossRef]
- Harvey, K.J.; Brown, B.; Crawford, P.; Macfarlane, A.; McPherson, A. ‘Am I normal?’ Teenagers, sexual health and the internet. Soc. Sci. Med. 2007, 65, 771–781. [Google Scholar] [CrossRef] [PubMed]
- Burns, J.M.; Durkin, L.A.; Nicholas, J. Mental health of young people in the United States: What role can the internet play in reducing stigma and promoting help seeking? J. Adolesc. Health 2009, 45, 95–97. [Google Scholar] [CrossRef] [PubMed]
- Turner, G. A method in search of a theory: Peer education and health promotion. Health Educ. Res. 1999, 14, 235–247. [Google Scholar] [CrossRef]
- Liu, X.; Pan, M.; Li, J. Does Sharing Your Emotion Make You Feel Better? An Empirical Investigation on the Association Between Sharing Emotions on a Virtual Mood Wall and the Relief of Patients’ Negative Emotions. Telemed. E-Health 2019, 25, 987–995. [Google Scholar] [CrossRef]
- Kim, J.; Lee, J.E. The Facebook paths to happiness: Effects of the number of Facebook friends and self-presentation on subjective well-being. Cyberpsychol. Behav. Soc. Netw. 2011, 14, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Bazarova, N.N.; Choi, Y.H. Self-Disclosure in Social Media: Extending the Functional Approach to Disclosure Motivations and Characteristics on Social Network Sites. J. Commun. 2014, 64, 635–657. [Google Scholar] [CrossRef]
- Mckenna, K.; Bargh, J.A. Coming out in the age of the Internet: Identity “demarginalization” through virtual group participation. J. Personal. Soc. Psychol. 1998, 75, 681–694. [Google Scholar] [CrossRef]
- Whitley, R.; Campbell, R.D. Stigma, agency and recovery amongst people with severe mental illness. Soc. Sci. Med. 2014, 107, 1–8. [Google Scholar] [CrossRef]
- Bargh, J.A.; Mckenna, K. The internet and social life. Annu. Rev. Psychol. 2004, 55, 573–590. [Google Scholar] [CrossRef]
- Castelein, S.; van der Gaag, M.; Bruggeman, R.; van Busschbach, J.T.; Wiersma, D. Measuring Empowerment Among People With Psychotic Disorders: A Comparison of Three Instruments. Psychiatr. Serv. 2008, 59, 1338–1342. [Google Scholar] [CrossRef]
- Wu, B. Patient Continued Use of Online Health Care Communities: Web Mining of Patient-Doctor Communication. J. Med. Internet Res. 2018, 20, e126. [Google Scholar] [CrossRef] [PubMed]
- Oliver, R.L. Effect of expectation and disconfirmation on postexposure product evaluations: An alternative interpretation. Psychol. Rep. 1977, 45, 803–810. [Google Scholar] [CrossRef]
- Weber, R. Understanding information systems continuance: An expectation-confirmation model. MIS Q. 2001, 25, 351–370. [Google Scholar]
- Wynne, C.W. Issues and Opinion on Structural Equation Modeling. MIS Q. 1998, 22, vii–xvi. [Google Scholar]
- Mcknight, D.H.; Choudhury, V.; Kacmar, C. Developing and Validating Trust Measures for e-Commerce: An Integrative Typology. Inf. Syst. Res. 2002, 13, 344–359. [Google Scholar] [CrossRef]
- Anderson, J.; Gerbing, C.; David, W. Structural equation modeling in practice: A review and recommended two-step approach. Psychol. Bull. 1988, 103, 411. [Google Scholar] [CrossRef]
- Komiak, S.Y.X.; Benbasat, I. The Effects of Personalization and Familiarity on Trust and Adoption of Recommendation Agents. MIS Q. 2006, 30, 941–960. [Google Scholar] [CrossRef]
- O’Leary-Kelly, S.W.; Vokurka, R.J. The empirical assessment of construct validity. J. Oper. Manag. 1998, 16, 387–405. [Google Scholar] [CrossRef]
- Preacher, K.J.; Hayes, A.F. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Methods Instrum. Comput. 2004, 36, 717–731. [Google Scholar] [CrossRef]
- Bhattacherjee, A.; Hikmet, N. Physicians’ resistance toward healthcare information technology: A theoretical model and empirical test. Eur. J. Inf. Syst. 2007, 16, 725–737. [Google Scholar] [CrossRef]
- Baron, R.M.; Kenny, D.A. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Chapman Hall 1986, 51, 1173–1182. [Google Scholar] [CrossRef]

| Constructs | Definition | Source |
|---|---|---|
| Emotional support | Receiving encouragement, comfort, and understanding from others | [45] |
| Information support | Receiving information about health | [45] |
| Helping others | Providing information and emotional support to others | [2] |
| Finding recognition | Feeling accepted and connected | [2] |
| Sharing experiences | Sharing experiences of treatment and daily life | [2] |
| Health self-efficacy | Belief in their ability to manage health and control disease | [35] |
| Expectation confirmation | Perception of the outcome is consistent with established expectations | [64] |
| Continuous intention | Intention to continue using online mental health communities | [64] |
| Constructs | Items | Literature | |
|---|---|---|---|
| Emotional support | ES1 | Provide encouragement to me | [45] |
| ES2 | Show me empathy | ||
| ES3 | Make me feel relieved | ||
| Information support | IS1 | Ask for health information or treatment advice | [45] |
| IS2 | Search and find a lot of health information | ||
| IS3 | The exchange of health information and advice meets the need | ||
| IS4 | Add extra value to the information I obtain from my doctor | ||
| Helping others | HO1 | I can offer advice and support to others | [2] |
| HO2 | I can be an example to other participants | ||
| Finding recognition | FR1 | I recognize myself in the stories of others | [2] |
| FR2 | I experience the sense of ‘not being the only one’ | ||
| FR3 | Others are an example to me | ||
| FR4 | I realize that I am not so bad off after all | ||
| Sharing experiences | SE1 | I can share my experiences with my illness with others | [2] |
| SE2 | I can share my everyday experiences with others | ||
| Expectation confirmation | EC1 | My experience with the community has been better than I expected | [64] |
| EC2 | The service provided by the community was better than I had expected | ||
| EC3 | The community can meet demand beyond my expectations | ||
| Health self-efficacy | SEF1 | I am confident that I can make a positive impact on my health | [45] |
| SEF2 | I have set some definite goals to improve my health | ||
| SEF3 | I am taking active treatment to improve my health | ||
| Continuous intention | CI1 | I will continue to be involved in this community in the future | [35] |
| CI2 | I will be coming back to this community often | ||
| CI3 | I will recommend others with depression be involved in this community |
| Variables | Value | Frequency | Percentage |
|---|---|---|---|
| Gender | male | 37 | 13.6 |
| female | 235 | 86.4 | |
| Age | <18 | 87 | 32 |
| 18–29 | 176 | 64.7 | |
| 30–40 | 8 | 2.9 | |
| >40 | 1 | 0.4 | |
| Marriage | unmarried | 263 | 96.7 |
| married | 9 | 3.3 | |
| Education | Junior or less | 48 | 17.6 |
| Senior high school | 80 | 29.4 | |
| Junior college | 45 | 16.5 | |
| Undergraduate | 92 | 33.8 | |
| Postgraduate | 7 | 2.6 | |
| Income | <1000 | 198 | 72.8 |
| 1000–3000 | 27 | 9.9 | |
| 3001–5000 | 23 | 8.5 | |
| 5001–8000 | 16 | 5.9 | |
| 8001–15,000 | 6 | 2.2 | |
| >15,000 | 2 | 0.7 | |
| Disease staging | Mild depressed | 63 | 23.2 |
| Moderate depressed | 94 | 34.6 | |
| Severe depressed | 107 | 39.3 | |
| Cured | 8 | 2.9 | |
| Duration visit online mental health community | <10 min | 73 | 26.8 |
| 10 min–30 min | 140 | 51.5 | |
| 30 min–1 h | 40 | 14.7 | |
| >1 h | 19 | 7 |
| Variables | Items | Standard Loads | Cronbach’s α | CR | AVE |
|---|---|---|---|---|---|
| Emotional support | ES1 | 0.887 | 0.833 | 0.9 | 0.75 |
| ES2 | 0.847 | ||||
| ES3 | 0.863 | ||||
| Information support | IS1 | 0.806 | 0.879 | 0.917 | 0.734 |
| IS2 | 0.879 | ||||
| IS3 | 0.859 | ||||
| IS4 | 0.881 | ||||
| Helping others | HO1 | 0.961 | 0.905 | 0.954 | 0.913 |
| HO2 | 0.95 | ||||
| Finding recognition | FR1 | 0.754 | 0.793 | 0.862 | 0.61 |
| FR2 | 0.762 | ||||
| FR3 | 0.808 | ||||
| FR4 | 0.799 | ||||
| Sharing experiences | SE1 | 0.937 | 0.85 | 0.93 | 0.869 |
| SE2 | 0.927 | ||||
| Health self-efficacy | SEF1 | 0.872 | 0.772 | 0.868 | 0.688 |
| SEF2 | 0.829 | ||||
| SEF3 | 0.785 | ||||
| Expectation confirmation | EC1 | 0.9 | 0.903 | 0.939 | 0.837 |
| EC2 | 0.929 | ||||
| EC3 | 0.916 | ||||
| Continuous intention | CI1 | 0.933 | 0.873 | 0.923 | 0.799 |
| CI2 | 0.905 | ||||
| CI3 | 0.842 |
| CI | EC | ES | FR | HO | IS | SE | SEF | |
|---|---|---|---|---|---|---|---|---|
| CI | 0.894 | |||||||
| EC | 0.447 | 0.915 | ||||||
| ES | 0.472 | 0.371 | 0.866 | |||||
| FR | 0.463 | 0.411 | 0.61 | 0.786 | ||||
| HO | 0.374 | 0.303 | 0.421 | 0.559 | 0.955 | |||
| IS | 0.485 | 0.428 | 0.608 | 0.58 | 0.473 | 0.862 | ||
| SE | 0.377 | 0.31 | 0.434 | 0.584 | 0.569 | 0.502 | 0.932 | |
| SEF | 0.815 | 0.394 | 0.586 | 0.545 | 0.492 | 0.566 | 0.512 | 0.829 |
| Variables | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Gender | –0.077 (0.059) | −0.085 (0.049) | −0.063 (0.042) |
| Age | −0.161 * (0.077) | −0.124 (0.065) | −0.086 (0.044) |
| Education | −0.046 (0.072) | −0.077 (0.068) | −0.005 (0.043) |
| Income | −0.055 (0.072) | −0.035 (0.059) | 0.011 (0.034) |
| Marriage | 0.018 (0.07) | 0.046 (0.05) | 0.007 (0.026) |
| Depression degree | −0.017 (0.063) | −0.008 (0.057) | −0.02 (0.045) |
| Duration visit online support group | −0.026 (0.072) | 0.043 (0.065) | −0.053 (0.046) |
| Emotional support | 0.074 (0.062) | 0.323 *** (0.057) | |
| Information support | 0.27 *** (0.064) | 0.184 ** (0.067) | |
| Helping others | 0.16 * (0.07) | ||
| Finding recognition | 0.243 *** (0.058) | ||
| Sharing experience | 0.191 ** (0.068) | ||
| Health self-efficacy | 0.796 *** (0.049) | ||
| Confirmation | 0.433 *** (0.056) | ||
| Observations | 272 | 272 | 272 |
| R2 | 0.084 | 0.265 | 0.668 |
| IV | M | DV | IV—>DV | IV—>M | IV + M—>DV | Mediating | |
|---|---|---|---|---|---|---|---|
| IV—>DV | M—>DV | ||||||
| ES | SEF | CI | 0.480 *** | 0.594 *** | −0.006 | 0.822 *** | completely |
| IS | SEF | CI | 0.480 ** | 0.558 * | 0.037 | 0.798 *** | completely |
| HO | SEF | CI | 0.387 *** | 0.497 *** | −0.032 | 0.834 *** | completely |
| SE | SEF | CI | 0.388 *** | 0.518 ** | −0.054 | 0.846 *** | completely |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, J.; Wang, J. Users’ Intention to Continue Using Online Mental Health Communities: Empowerment Theory Perspective. Int. J. Environ. Res. Public Health 2021, 18, 9427. https://doi.org/10.3390/ijerph18189427
Liu J, Wang J. Users’ Intention to Continue Using Online Mental Health Communities: Empowerment Theory Perspective. International Journal of Environmental Research and Public Health. 2021; 18(18):9427. https://doi.org/10.3390/ijerph18189427
Chicago/Turabian StyleLiu, Jingfang, and Jiayu Wang. 2021. "Users’ Intention to Continue Using Online Mental Health Communities: Empowerment Theory Perspective" International Journal of Environmental Research and Public Health 18, no. 18: 9427. https://doi.org/10.3390/ijerph18189427
APA StyleLiu, J., & Wang, J. (2021). Users’ Intention to Continue Using Online Mental Health Communities: Empowerment Theory Perspective. International Journal of Environmental Research and Public Health, 18(18), 9427. https://doi.org/10.3390/ijerph18189427






