Spatial Modeling of COVID-19 Vaccine Hesitancy in the United States
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Settings
- (1)
- socioeconomic status: percentage of people below poverty, unemployment rate, per capita income, percentage of people with no high school diploma,
- (2)
- household composition and disability: percentage of people aged 65 and older, percentage of people aged 17 and younger, percentage of non-institutionalized people with a disability, percentage of single-parent households with children,
- (3)
- minority status and language: percentage of minority people (except white and non-Hispanic),
- (4)
- housing type and transportation: percentage of housing in structures with 10+ units, percentage of mobile homes, percentage of over-occupied housing units, percentage of households with no vehicle available, and percentage of institutionalized group quarters (e.g., correctional institutions, nursing homes).
2.2. Ordinary Least Squares Model (OLS)
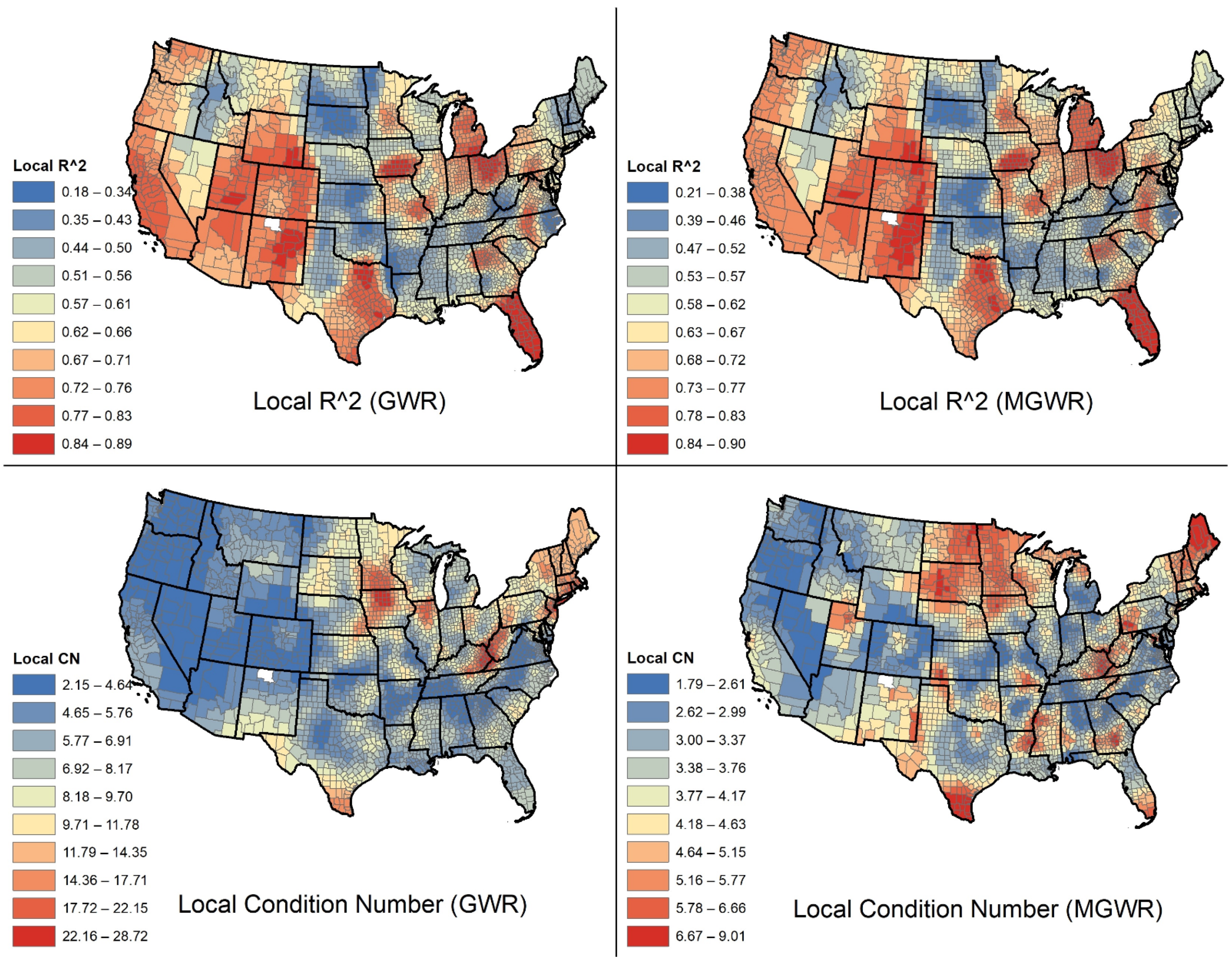
2.3. Geographically Weighted Regression (GWR)
2.4. Multiscale Geographically Weighted Regression (MGWR)
2.5. Model Evaluation
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Center for Systems Science and Engineering (CSSE). Global Cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). 2021. Available online: https://github.com/CSSEGISandData/COVID-19 (accessed on 1 August 2021).
- World Health Organization. Coronavirus Disease 2019 (COVID-19) Situation Report-51. 2020. Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10 (accessed on 1 August 2021).
- Lurie, N.; Sharfstein, J.M.; Goodman, J.L. The development of COVID-19 vaccines: Safeguards needed. JAMA 2020, 324, 439–440. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Trends in Number of COVID-19 Cases and Deaths in the US Reported to CDC, by State/Territory. COVID Data Tracker. 2021. Available online: https://covid.cdc.gov/covid-data-tracker/#trends_dailytrendscases (accessed on 12 August 2021).
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M. COVID-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Estimates of Vaccine Hesitancy for COVID-19. 2021. Available online: https://data.cdc.gov/stories/s/Vaccine-Hesitancy-for-COVID-19/cnd2-a6zw (accessed on 1 August 2021).
- Razai, M.S.; Osama, T.; McKechnie, D.G.; Majeed, A. Covid-19 Vaccine Hesitancy among Ethnic Minority Groups. BMJ 2021, n531. [Google Scholar] [CrossRef]
- Soares, P.; Rocha, J.V.; Moniz, M.; Gama, A.; Laires, P.A.; Pedro, A.R.; Nunes, C. Factors associated with COVID-19 vaccine hesitancy. Vaccines 2021, 9, 300. [Google Scholar] [CrossRef]
- National Governors Association. COVID-19 Vaccine Incentives. Publications. 2021. Available online: https://www.nga.org/center/publications/covid-19-vaccine-incentives/ (accessed on 15 June 2021).
- Endrich, M.M.; Blank, P.R.; Szucs, T.D. Influenza vaccination uptake and socioeconomic determinants in 11 European countries. Vaccine 2009, 27, 4018–4024. [Google Scholar] [CrossRef]
- Mollalo, A.; Vahedi, B.; Rivera, K.M. GIS-based spatial modeling of COVID-19 incidence rate in the continental United States. Sci. Total Environ. 2020, 728, 138884. [Google Scholar] [CrossRef]
- Mollalo, A.; Rivera, K.M.; Vahedi, B. Artificial neural network modeling of novel coronavirus (COVID-19) incidence rates across the continental United States. Int. J. Environ. Res. Public Health 2020, 17, 4204. [Google Scholar] [CrossRef]
- Flanagan, B.E.; Gregory, E.W.; Hallisey, E.J.; Heitgerd, J.L.; Lewis, B. A social vulnerability index for disaster management. J. Homel. Secur. Emerg. Manag. 2011, 8, 3. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. CDC’s Social Vulnerability Index (SVI). 2018. Available online: https://svi.cdc.gov/ (accessed on 1 August 2021).
- Iyanda, A.E.; Adeleke, R.; Lu, Y.; Osayomi, T.; Adaralegbe, A.; Lasode, M.; Osundina, A.M. A retrospective cross-national examination of COVID-19 outbreak in 175 countries: A multiscale geographically weighted regression analysis (January 11-June 28, 2020). J. Infect. Public Health 2020, 13, 1438–1445. [Google Scholar] [CrossRef]
- Iyanda, A.E.; Boakye, K.A.; Lu, Y.; Oppong, J.R. Racial/Ethnic Heterogeneity and Rural-Urban Disparity of COVID-19 Case Fatality Ratio in the USA: A Negative Binomial and GIS-Based Analysis. J. Racial Ethn. Health Disparities 2021, 1–14. [Google Scholar] [CrossRef]
- Al Kindi, K.M.; Al-Mawali, A.; Akharusi, A.; Alshukaili, D.; Alnasiri, N.; Al-Awadhi, T.; El Kenawy, A.M. Demographic and socioeconomic determinants of COVID-19 across Oman-A geospatial modelling approach. Geospat. Health 2021, 16, 145–160. [Google Scholar] [CrossRef] [PubMed]
- Vahabi, N.; Salehi, M.; Duarte, J.D.; Mollalo, A.; Michailidis, G. County-level longitudinal clustering of COVID-19 mortality to incidence ratio in the United States. Sci. Rep. 2021, 11, 1–22. [Google Scholar] [CrossRef]
- Iyanda, A.; Boakye, K.; Lu, Y. COVID-19: Evidenced Health Disparity. Encyclopedia 2021, 1, 57. [Google Scholar] [CrossRef]
- Bansal Lab. Available online: http://www.vaccinetracking.us/ (accessed on 1 August 2021).
- COVID CDC Tracker. Available online: https://covid.cdc.gov/covid-data-tracker/#vaccinations-county-view (accessed on 1 August 2021).
- CDC/ATSDR SVI Data. Available online: https://www.atsdr.cdc.gov/placeandhealth/svi/data_documentation_download.html (accessed on 1 August 2021).
- TIGER/Line. Available online: https://www.census.gov/geographies/mapping-files/time-series/geo/tiger-line-file.html (accessed on 1 August 2021).
- Hutcheson, G.D. Ordinary least-squares regression. In The SAGE Dictionary of Quantitative Management Research; Moutinho, L., Hutcheson, G.D., Eds.; Sage: Los Angeles, CA, USA, 2011; pp. 224–228. [Google Scholar]
- Anselin, L.; Arribas-Bel, D. Spatial fixed effects and spatial dependence in a single cross-section. Pap. Reg. Sci. 2013, 92, 3–17. [Google Scholar] [CrossRef]
- Tu, J.; Xia, Z.G. Examining spatially varying relationships between land use and water quality using geographically weighted regression I: Model design and evaluation. Sci. Total Environ. 2008, 407, 358–378. [Google Scholar] [CrossRef]
- Brunsdon, C.; Fotheringham, A.S.; Charlton, M.E. Geographically weighted regression: A method for exploring spatial nonstationarity. Geogr. Anal. 1996, 28, 281–298. [Google Scholar] [CrossRef]
- Fotheringham, A.S.; Yang, W.; Kang, W. Multiscale geographically weighted regression (MGWR). Ann. Am. Assoc. Geogr. 2017, 107, 1247–1265. [Google Scholar] [CrossRef]
- Oshan, T.M.; Smith, J.P.; Fotheringham, A.S. Targeting the spatial context of obesity determinants via multiscale geographically weighted regression. Int. J. Health Geogr. 2020, 19, 1–17. [Google Scholar] [CrossRef]
- Chen, Y.; Jiao, J. Relationship between Socio-Demographics and COVID-19: A Case Study in Three Texas Regions. 2020. Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3636484 (accessed on 1 August 2021).
- Wu, X.; Zhang, J. Exploration of spatial-temporal varying impacts on COVID-19 cumulative case in Texas using geographically weighted regression (GWR). Environ. Sci. Pollut. Res. 2021, 28, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Maiti, A.; Zhang, Q.; Sannigrahi, S.; Pramanik, S.; Chakraborti, S.; Cerda, A.; Pilla, F. Exploring spatiotemporal effects of the driving factors on COVID-19 incidences in the contiguous United States. Sustain. Cities Soc. 2021, 68, 102784. [Google Scholar] [CrossRef] [PubMed]
- Horse AJ, Y.; Yang, T.C.; Huyser, K.R. Structural inequalities established the architecture for COVID-19 pandemic among native Americans in Arizona: A geographically weighted regression perspective. J. Racial Ethn. Health Disparities 2021, 1–11. [Google Scholar] [CrossRef]
- Zhang, J.; Wu, X.; Chow, T.E. Space-Time Cluster’s Detection and Geographical Weighted Regression Analysis of COVID-19 Mortality on Texas Counties. Int. J. Environ. Res. Public Health 2021, 18, 5541. [Google Scholar] [CrossRef] [PubMed]
- Mansour, S.; Al Kindi, A.; Al-Said, A.; Al-Said, A.; Atkinson, P. Sociodemographic determinants of COVID-19 incidence rates in Oman: Geospatial modelling using multiscale geographically weighted regression (MGWR). Sustain. Cities Soc. 2021, 65, 102627. [Google Scholar] [CrossRef] [PubMed]
- Oshan, T.M.; Li, Z.; Kang, W.; Wolf, L.J.; Fotheringham, A.S. Mgwr: A Python Implementation of Multiscale Geographically Weighted Regression for Investigating Process Spatial Heterogeneity and Scale. ISPRS Int. J. Geo-Inf. 2019, 8, 269. [Google Scholar] [CrossRef] [Green Version]
- Arbona, S.I.; Barro, A.S. Peer Reviewed: Exploring the Spatial Determinants of Late HIV Diagnosis in Texas. Prev. Chronic Dis. 2020, 17, E96. [Google Scholar] [CrossRef]
- Mollalo, A.; Alimohammadi, A.; Shirzadi, M.R.; Malek, M.R. Geographic information system-based analysis of the spatial and spatio-temporal distribution of zoonotic cutaneous leishmaniasis in Golestan Province, north-east of Iran. Zoonoses Public Health 2015, 62, 18–28. [Google Scholar] [CrossRef]
- Mollalo, A.; Rivera, K.M.; Vahabi, N. Spatial statistical analysis of pre-existing mortalities of 20 diseases with COVID-19 mortalities in the continental United States. Sustain. Cities Soc. 2021, 67, 102738. [Google Scholar] [CrossRef] [PubMed]
- Iyanda, A.E.; Osayomi, T. Is there a relationship between economic indicators and road fatalities in Texas? A multiscale geographically weighted regression analysis. GeoJournal 2020, 1–21. [Google Scholar] [CrossRef]
- Mollalo, A.; Vahedi, B.; Bhattarai, S.; Hopkins, L.C.; Banik, S.; Vahedi, B. Predicting the hotspots of age-adjusted mortality rates of lower respiratory infection across the continental United States: Integration of GIS, spatial statistics and machine learning algorithms. Int. J. Med Inform. 2020, 142, 104248. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Ten Threats to Global Health in 2019. 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 10 August 2021).
- Hildreth, J.E.; Alcendor, D.J. Targeting COVID-19 Vaccine Hesitancy in Minority Populations in the US: Implications for Herd Immunity. Vaccines 2021, 9, 489. [Google Scholar] [CrossRef] [PubMed]
- Callaghan, T.; Moghtaderi, A.; Lueck, J.A.; Hotez, P.J.; Strych, U.; Dor, A.; Motta, M. Correlates and Disparities of COVID-19 Vaccine Hesitancy. 2020. Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3667971 (accessed on 1 August 2021).
- Nguyen, L.H.; Joshi, A.D.; Drew, D.A.; Merino, J.; Ma, W.; Lo, C.-H.; Polidori, L. Racial and ethnic differences in COVID-19 vaccine hesitancy and uptake. MedRxiv 2021, 1–49. [Google Scholar] [CrossRef]
- Wagner, A.L.; Masters, N.B.; Domek, G.J.; Mathew, J.L.; Sun, X.; Asturias, E.J.; Boulton, M.L. Comparisons of vaccine hesitancy across five low-and middle-income countries. Vaccines 2019, 7, 155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aw, J.; Seng, J.J.B.; Seah, S.S.Y.; Low, L.L. COVID-19 vaccine hesitancy—A scoping review of literature in high-income countries. Vaccines 2021, 9, 900. [Google Scholar] [CrossRef] [PubMed]
- Household Pulse Survey Data Tables. Available online: https://www.census.gov/programs-surveys/household-pulse-survey/data.html (accessed on 10 August 2021).
- Lindemer, E.; Choudhary, M.; Donadio, G.; Pawlowski, C.; Soundararajan, V. Counties with lower insurance coverage are associated with both slower vaccine rollout and higher COVID-19 incidence across the United States. MedRxiv 2021, 1–19. [Google Scholar] [CrossRef]
- Juhn, Y.J.; Sauver, J.S.; Katusic, S.; Vargas, D.; Weaver, A.; Yunginger, J. The influence of neighborhood environment on the incidence of childhood asthma: A multilevel approach. Soc. Sci. Med. 2005, 60, 2453–2464. [Google Scholar] [CrossRef] [PubMed]
- Bureau, U.C. American Housing Survey for the United States: 2005 Current Housing Reports; Government Printing Office: Washington, DC, USA, 2006. [Google Scholar]
- Jacobs, D.E. Environmental health disparities in housing. Am. J. Public Health 2011, 101, S115–S122. [Google Scholar] [CrossRef] [PubMed]
- Holden, C.D.; Chen, J.; Dagher, R.K. Preventive care utilization among the uninsured by race/ethnicity and income. Am. J. Prev. Med. 2015, 48, 13–21. [Google Scholar] [CrossRef] [PubMed]


| No. | Covariate | Abbreviation | Definition |
|---|---|---|---|
| 1 | Below poverty % | POV | Percentage of persons below federal poverty level |
| 2 | Unemployment rate % | UNEMP | Number of persons who are unemployed but seeking a job |
| 3 | Per capita income | PCI | Per capita annual income in dollars |
| 4 | No high school diploma % | NOHSDP | Percentage of persons with no high school diploma (age 25+) |
| 5 | Age 65 and older % | AGE65 | Percentage of persons aged 65 and older |
| 6 | Age 17 and younger % | AGE17 | Percentage of persons aged 17 and younger |
| 7 | Non-institutionalized with a disability % | DISABL | Percentage of civilian non-institutionalized population with a disability |
| 8 | Single-parent households with children % | SNGPNT | Percentage of single-parent households with children under 18 |
| 9 | Minority (except white, non-Hispanic) % | MINRTY | Percentage minority (all persons except white, non-Hispanic) |
| 10 | Age 5+ who speak limited English % | LIMENG | Percentage of persons (age 5+) who speak English “less than well” estimate |
| 11 | Housing in structures with 10+ units % | MUNIT | Percentage of housing structures with 10 or more units out of all residential housing types |
| 12 | Mobile homes % | MOBILE | Percentage of mobile homes out of all residential housing types |
| 13 | Over-occupied housing units % | CROWD | Percentage of occupied housing units with more occupants than number of rooms |
| 14 | Households with no vehicle available % | NOVEH | Percentage of households with no vehicle ownership |
| 15 | Institutionalized group quarters % | GROUPQ | Percentage of persons residing in institutionalized group quarters (e.g., correctional institutions, nursing homes) |
| 16 | Uninsured people % | UNISUR | Percentage uninsured in the total civilian non-institutionalized population |
| 17 | Population density per square mile | POPDEN | Number of persons per square mile |
| US Region | Fully Vaccinated (%) | Per Capita Income ($) | Age 17 and Younger (%) | Minority (%) | Mobile Homes (%) | Uninsured People (%) |
|---|---|---|---|---|---|---|
| West | 51.22 | 28,274 | 22.63 | 27.29 | 13.12 | 10.08 |
| Midwest | 45.51 | 28,127 | 22.66 | 11.84 | 7.96 | 7.84 |
| South | 42.41 | 24,875 | 22.39 | 31.31 | 17.76 | 12.18 |
| Northeast | 54.86 | 32,605 | 19.97 | 16.60 | 6.36 | 6.09 |
| Covariate | Coefficient (EST.) | SE | T (EST/SE) | p-Value | VIF |
|---|---|---|---|---|---|
| Intercept | 0.000 | 0.013 | 0.000 | 1.000 | – |
| Per capita income | 0.360 | 0.017 | 21.446 | 0.000 | 1.599 |
| Age 17 and younger (%) | –0.244 | 0.015 | –16.643 | 0.000 | 1.217 |
| Minority (%) | 0.338 | 0.016 | 21.471 | 0.000 | 1.408 |
| Mobile homes (%) | –0.259 | 0.017 | –15.510 | 0.000 | 1.587 |
| Uninsured people (%) | –0.190 | 0.018 | –10.761 | 0.000 | 1.763 |
| Model | |||
|---|---|---|---|
| Evaluation Statistic | OLS | GWR | MGWR |
| AICc | 6954.21 | 4676.526 | 4437.25 |
| Adj. R2 | 45.3 | 77.7 | 79.1 |
| RSS | 1697.984 | 598.47 | 569.38 |
| Log-Likelihood | −3469.992 | –1849.97 | –1772.57 |
| Bandwidth (95% CI) | Effective Number of Parameters | Critical t-Value (95%) | ||||
|---|---|---|---|---|---|---|
| GWR | MGWR | GWR | MGWR | GWR | MGWR | |
| Model | n/a | n/a | 420.840 | 388.934 | 3.388 | n/a |
| Intercept | 104 (98, 107) | 44 (44, 46) | n/a | 181.954 | n/a | 3.642 |
| Per capita income | 104 (98, 107) | 95 (88, 107) | n/a | 69.082 | n/a | 3.384 |
| Age 17 and younger (%) | 104 (98, 107) | 74 (67, 82) | n/a | 98.274 | n/a | 3.48 |
| Minority (%) | 104 (98, 107) | 322 (278, 384) | n/a | 14.508 | n/a | 2.927 |
| Mobile homes (%) | 104 (98, 107) | 1283 (1042, 1936) | n/a | 3.77 | n/a | 2.478 |
| Uninsured people (%) | 104 (98, 107) | 245 (213, 278) | n/a | 21.345 | n/a | 3.046 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mollalo, A.; Tatar, M. Spatial Modeling of COVID-19 Vaccine Hesitancy in the United States. Int. J. Environ. Res. Public Health 2021, 18, 9488. https://doi.org/10.3390/ijerph18189488
Mollalo A, Tatar M. Spatial Modeling of COVID-19 Vaccine Hesitancy in the United States. International Journal of Environmental Research and Public Health. 2021; 18(18):9488. https://doi.org/10.3390/ijerph18189488
Chicago/Turabian StyleMollalo, Abolfazl, and Moosa Tatar. 2021. "Spatial Modeling of COVID-19 Vaccine Hesitancy in the United States" International Journal of Environmental Research and Public Health 18, no. 18: 9488. https://doi.org/10.3390/ijerph18189488
APA StyleMollalo, A., & Tatar, M. (2021). Spatial Modeling of COVID-19 Vaccine Hesitancy in the United States. International Journal of Environmental Research and Public Health, 18(18), 9488. https://doi.org/10.3390/ijerph18189488







