Selecting Thresholds of Heat-Warning Systems with Substantial Enhancement of Essential Population Health Outcomes for Facilitating Implementation
Abstract
1. Introduction
2. Materials and Methods
2.1. Health Records
2.2. Heat Indicator and Air Pollutant Data
2.3. Models for Threshold Selection
3. Results
3.1. Health Risks Associated with Increased WBGT and Temperature
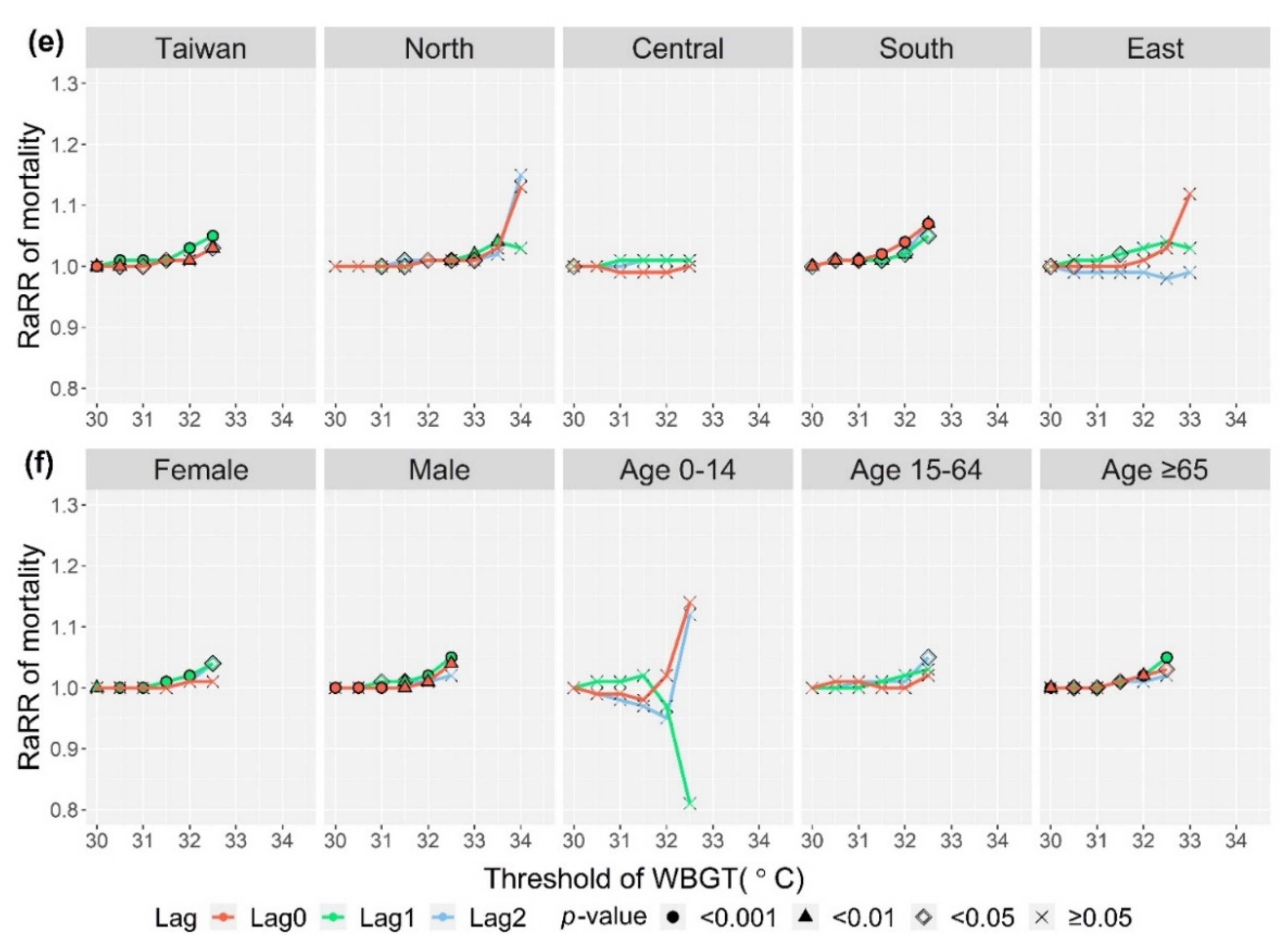
3.2. RaRR Comparison among Different Categories
3.3. Potential WBGT Threshold Candidates
4. Discussion
4.1. Heat-Warning Threshold Selection and Advantages of Our Method
4.2. Consideration for Different Sex and Age Groups
4.3. Applicability and Limitation of Our Method
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nation Environmental Programme (UNEP). 2020. Available online: https://www.unenvironment.org/explore-topics/climate-change/facts-about-climate-emergency (accessed on 26 January 2021).
- IPCC (Intergovernmental Panel on Climate Change). Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part A: Global and Sectoral Aspects: Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; Field, C.B., Barros, V.R., Dokken, D.J., Mach, K.J., Mastrandrea, M.D., Bilir, T.E., Chatterjee, M., Ebi, K.L., Estrada, Y.O., Genova, R.C., et al., Eds.; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2014; p. 1132. [Google Scholar]
- Watts, N.; Adger, W.N.; Ayeb-Karlsson, S.; Bai, Y.; Byass, P.; Campbell-Lendrum, D.; Colbourn, T.; Cox, P.; Davies, M.; Depledge, M.; et al. The Lancet Countdown: Tracking progress on health and climate change. Lancet 2017, 389, 1151–1164. [Google Scholar] [CrossRef]
- World Meteorological Organization (WMO). 2020. Available online: https://public.wmo.int/en/media/news/2020-closes-decade-of-exceptional-heat (accessed on 26 January 2021).
- UN (United Nations). Sustainable Development Goals (SDGs). 2018. Available online: https://www.un.org/sustainabledevelopment/ (accessed on 26 January 2021).
- Intergovernmental Panel on Climate Change (IPCC). Climate Change 2014—Impacts, Adaptation and Vulnerability: Part A: Global and Sectoral Aspects: Working Group II Contribution to the IPCC Fifth Assessment Report; Cambridge University Press: Cambridge, UK, 2014; Volume 1, pp. 709–754. [Google Scholar]
- Cheng, Y.-T.; Lung, S.-C.C.; Hwang, J.-S. New approach to identifying proper thresholds for a heat warning system using health risk increments. Environ. Res. 2019, 170, 282–292. [Google Scholar] [CrossRef] [PubMed]
- Ghumman, U.; Horney, J. Characterizing the Impact of Extreme Heat on Mortality, Karachi, Pakistan, June 2015. Prehospital Disaster Med. 2016, 31, 263–266. [Google Scholar] [CrossRef] [PubMed]
- Chandran, M.A.S.; Rao, A.V.M.S.; Sandeep, V.M.; Pramod, V.P.; Pani, P.; Rao, V.U.M.; Visha Kumari, V.; Srinivasa Rao, C. Indian summer heat wave of 2015: A biometeorological analysis using half hourly automatic weather station data with special reference to Andhra Pradesh. Int. J. Biometeorol. 2017, 61, 1063–1072. [Google Scholar] [CrossRef] [PubMed]
- Sung, T.I.; Wu, P.C.; Lung, S.C.; Lin, C.Y.; Chen, M.J.; Su, H.J. Relationship between heat index and mortality of 6 major cities in Taiwan. Sci. Total Environ. 2013, 442, 275–281. [Google Scholar] [CrossRef]
- Changnon, S.A.; Kunkel, K.E.; Reinke, B.C. Impacts and responses to the 1995 heat wave: A call to action. Bull. Am. Meteorol. Soc. 1996, 77, 1497–1506. [Google Scholar] [CrossRef]
- Semenza, J.C.; Rubin, C.H.; Falter, K.H.; Selanikio, J.D.; Flanders, W.D.; Howe, H.L.; Wilhelm, J.L. Heat-related deaths during the July 1995 heat wave in Chicago. N. Engl. J. Med. 1996, 335, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Burgstall, A.; Casanueva, A.; Kotlarski, S.; Schwierz, C. Heat warnings in Switzerland: Reassessing the choice of the current heat stress index. Int. J. Environ. Res. Public Health 2019, 16, 2684. [Google Scholar] [CrossRef]
- Toloo, G.; Fitzgerald, G.; Aitken, P.; Verrall, K.; Tong, S. Are heat warning systems effective? Environ. Health 2013, 12, 27. [Google Scholar] [CrossRef]
- Toloo, G.; Fitzgerald, G.; Aitken, P.; Verrall, K.; Tong, S. Evaluating the effectiveness of heat warning systems: Systematic review of epidemiological evidence. Int. J. Public Health 2013, 58, 667–681. [Google Scholar] [CrossRef] [PubMed]
- Casanueva, A.; Burgstall, A.; Kotlarski, S.; Messeri, A.; Morabito, M.; Flouris, A.D.; Nybo, L.; Spirig, C.; Schwierz, C. Overview of existing heat-health warning systems in Europe. Int. J. Environ. Res. Public Health 2019, 16, 2657. [Google Scholar] [CrossRef]
- Morabito, M.; Messeri, A.; Noti, P.; Casanueva, A.; Crisci, A.; Kotlarski, S.; Orlandini, S.; Schwierz, C.; Spirig, C.; Kingma, B.R.M.; et al. An occupational heat–health warning system for Europe: The HEAT-SHIELD Platform. Int. J. Environ. Res. Public Health 2019, 16, 2890. [Google Scholar] [CrossRef] [PubMed]
- Lang, D.J.; Wiek, A.; Bergmann, M.; Stauffacher, M.; Martens, P.; Moll, P.; Swilling, M.; Thomas, C.J. Transdisciplinary research in sustainability science: Practice, principles, and challenges. Sustain. Sci. 2012, 7, 25–43. [Google Scholar] [CrossRef]
- Mauser, W.; Klepper, G.; Rice, M.; Schmalzbauer, B.S.; Hackmann, H.; Leemans, R.; Moore, H. Transdisciplinary global change research: The co-creation of knowledge for sustainability. Curr. Opin. Environ. Sustain. 2013, 5, 420–431. [Google Scholar] [CrossRef]
- Petitti, D.B.; Hondula, D.M.; Yang, S.; Harlan, S.L.; Chowell, G. Multiple Trigger Points for Quantifying Heat-Health Impacts: New Evidence from a Hot Climate. Environ. Health Perspect. 2016, 124, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Bernard, T.E. Thermal stress. In Fundamentals of Industrial Hygene, 6th ed.; Plog, B.A., Quinlan, P., Eds.; National Safety Council: Itasca, IL, USA, 2012; Chapter 12; pp. 335–361. [Google Scholar]
- Błażejczyk, K.; Baranowski, J.; Błażejczyk, A. Heat stress and occupational health and safety—Spatial and temporal differentiation. Misc. Geogr. Reg. Stud. Dev. 2014, 1, 61–67. [Google Scholar] [CrossRef]
- Brode, P.; Fiala, D.; Lemke, B.; Kjellstrom, T. Estimated work ability in warm outdoor environments depends on the chosen heat stress assessment metric. Int. J. Biometeorol. 2018, 62, 331–345. [Google Scholar] [CrossRef]
- ISO (International Standards Organization). Ergonomics of the Thermal Environment—Assessment of Heat Stress Using the WBGT (Wet Bulb Globe Temperature) Index. 2017. Available online: https://www.iso.org/standard/67188.html (accessed on 26 January 2021).
- Spector, J.T.; Sheffield, P.E. Re-evaluating Occupational Heat Stress in a Changing Climate. Ann. Occup. Hyg. 2014, 58, 936–942. [Google Scholar] [CrossRef][Green Version]
- Yaglou, C.P.; Minard, D. Control of heat casualties at military training centers. A.M.A. Arch. Ind. Health 1957, 16, 302–316. [Google Scholar]
- Hyatt, O.M.; Lemke, B.; Kjellstrom, T. Regional maps of occupational heat exposure: Past, present, and potential future. Glob. Health Action 2010, 3, 10. [Google Scholar] [CrossRef] [PubMed]
- Kakamu, T.; Wada, K.; Smith, D.R.; Endo, S.; Fukushima, T. Preventing heat illness in the anticipated hot climate of the Tokyo 2020 Summer Olympic Games. Environ. Health Prev. 2017, 22, 68. [Google Scholar] [CrossRef]
- Lin, Y.-K.; Chang, C.-K.; Li, M.-H.; Wu, Y.-C.; Wang, Y.-C. High-temperature indices associated with mortality and outpatient visits: Characterizing the association with elevated temperature. Sci. Total Environ. 2012, 427, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, S.; Iwamoto, M.; Inoue, M.; Harada, N. Evaluation of the effect of heat exposure on the autonomic nervous system by heart rate variability and urinary catecholamines. J. Occup. Health 2007, 49, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Liljegren, J.C.; Carhart, R.A.; Lawday, P.; Tschopp, S.; Sharp, R. Modeling the wet bulb globe temperature using standard meteorological measurements. J. Occup. Environ. Hyg. 2008, 5, 645–655. [Google Scholar] [CrossRef] [PubMed]
- Ye, X.; Wolff, R.; Yu, W.; Vaneckova, P.; Pan, X.; Tong, S. Ambient Temperature and Morbidity: A Review of Epidemiological Evidence. Environ. Health Perspect. 2012, 120, 19–28. [Google Scholar] [CrossRef]
- Lee, K.L.; Chan, Y.H.; Lee, T.C.; Goggins, W.B.; Chan, E.Y.Y. The development of the Hong Kong Heat Index for enhancing the heat stress information service of the Hong Kong Observatory. Int. J. Biometeorol. 2016, 60, 1029–1039. [Google Scholar] [CrossRef]
- Australian Government—Bureau of Meteorology. Homepage: Heatwave Service for Australia. 2018. Available online: http://www.bom.gov.au/australia/heatwave/index.shtml (accessed on 26 January 2021).
- Japanese Ministry of the Environment. Homepage: Heat Illness Prevention Information. 2018. Available online: http://www.wbgt.env.go.jp/en/ (accessed on 26 January 2021).
- Astrom, D.O.; Forsberg, B.; Rocklov, J. Heat wave impact on morbidity and mortality in the elderly population: A review of recent studies. Maturitas 2011, 69, 99–105. [Google Scholar] [CrossRef]
- Li, M.; Gu, S.; Bi, P.; Yang, J.; Liu, Q. Heat Waves and Morbidity: Current Knowledge and Further Direction-A Comprehensive Literature Review. Int. J. Environ. Res. Public Health 2015, 12, 5256–5283. [Google Scholar] [CrossRef]
- Kang, C.; Park, C.; Lee, W.; Pehlivan, N.; Choi, M.; Jang, J.; Kim, H. Heatwave-Related Mortality Risk and the Risk-Based Definition of Heat Wave in South Korea: A Nationwide Time-Series Study for 2011–2017. Int. J. Environ. Res. Public Health 2020, 17, 5720. [Google Scholar] [CrossRef]
- Xing, Q.; Sun, Z.; Tao, Y.; Zhang, X.; Miao, S.; Zheng, C.; Tong, S. Impacts of urbanization on the temperature-cardiovascular mortality relationship in Beijing, China. Environ. Res. 2020, 191, 110234. [Google Scholar] [CrossRef]
- Arbuthnott, K.; Hajat, S.; Heaviside, C.; Vardoulakis, S. Years of life lost and mortality due to heat and cold in the three largest English cities. Environ. Int. 2020, 144, 105966. [Google Scholar] [CrossRef] [PubMed]
- Honda, Y.; Kabuto, M.; Ono, M.; Uchiyama, I. Determination of optimum daily maximum temperature using climate data. Environ. Health Prev. 2007, 12, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Honda, Y.; Kondo, M.; McGregor, G.; Kim, H.; Guo, Y.L.; Hijioka, Y.; Yoshikawa, M.; Oka, K.; Takano, S.; Hales, S.; et al. Heat-related mortality risk model for climate change impact projection. Environ. Health Prev. 2014, 19, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.-K.; Ho, T.-J.; Wang, Y.-C. Mortality risk associated with temperature and prolonged temperature extremes in elderly populations in Taiwan. Environ. Res. 2011, 111, 1156–1163. [Google Scholar] [CrossRef]
- Lin, Y.-K.; Sung, F.-C.; Honda, Y.; Chen, Y.-J.; Wang, Y.-C. Comparative assessments of mortality from and morbidity of circulatory diseases in association with extreme temperatures. Sci. Total Environ. 2020, 723, 138012. [Google Scholar] [CrossRef]
- Bai, L.; Ding, G.; Gu, S.; Bi, P.; Su, B.; Qin, D.; Xu, G.; Liu, Q. The effects of summer temperature and heat waves on heat-related illness in a coastal city of China, 2011–2013. Environ. Res. 2014, 132, 212–219. [Google Scholar] [CrossRef]
- Ellena, M.; Ballester, J.; Mercogliano, P.; Ferracin, E.; Barbato, G.; Costa, G.; Ingole, V. Social inequalities in heat-attributable mortality in the city of Turin, northwest of Italy: A time series analysis from 1982 to 2018. Environ. Health 2020, 19, 116. [Google Scholar] [CrossRef]
- Pyrgou, A.; Santamouris, M. Probability Risk of Heat- and Cold-Related Mortality to Temperature, Gender, and Age Using GAM Regression Analysis. Climate 2020, 8, 40. [Google Scholar] [CrossRef]
- Le Tertre, A.; Lefranc, A.; Eilstein, D.; Declercq, C.; Medina, S.; Blanchard, M.; Chardon, B.; Fabre, P.; Filleul, L.; Jusot, J.F.; et al. Impact of the 2003 heatwave on all-cause mortality in 9 French cities. Epidemiology 2006, 17, 75–79. [Google Scholar] [CrossRef]
- Xu, Z.; Etzel, R.A.; Su, H.; Huang, C.; Guo, Y.; Tong, S. Impact of ambient temperature on children’s health: A systematic review. Environ. Res. 2012, 117, 120–131. [Google Scholar] [CrossRef]
- Wu, C.D.; Lung, S.C.C. Application of 3-D Urbanization Index to assess impact of urbanization on air temperature. Sci. Rep. 2016, 6, 24351. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.S.; Lung, S.C.C. Can green structure reduce the mortality of cardiovascular diseases? Sci. Total Environ. 2016, 566, 1159–1167. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.S.; Lung, S.C.C. Multiple impacts and pathways of urban form and environmental factors on cardiovascular mortality. Sci. Total Environ. 2020, 738, 139512. [Google Scholar] [CrossRef] [PubMed]
- Tong, S.; Wang, X.Y.; FitzGerald, G.; McRae, D.; Neville, G.; Tippett, V.; Aitken, P.; Verrall, K. Development of health risk-based metrics for defining a heatwave: A time series study in Brisbane, Australia. BMC Public Health 2014, 14, 435. [Google Scholar] [CrossRef]
- Watts, N.; Amann, M.; Ayeb-Karlsson, S.; Belesova, K.; Bouley, T.; Boykoff, M.; Byass, P.; Cai, W.; Campbell-Lendrum, D.; Chambers, J.; et al. The Lancet Countdown on health and climate change: From 25 years of inaction to a global transformation for public health. Lancet 2018, 391, 581–630. [Google Scholar] [CrossRef]
- Taiwan National Development Council. Government Website Open Information Announcement. 2018. Available online: https://data.gov.tw/en/ (accessed on 26 January 2021).





| Variable | Taiwan | North | Central | South | East | |
|---|---|---|---|---|---|---|
| Population | 23,316,818 | 10,776,529 | 4,570,579 | 6,964,326 | 1,005,384 | |
| Area (km2) | 355,887 | 7030 | 7396 | 11,174 | 10,287 | |
| Population density (Pop. per km2) | 650 | 1533 | 618 | 623 | 98 | |
| WBGT | 99.5th percentile (2000–2017) | 33.1 | 34.3 | 33.0 | 33.2 | 33.4 |
| 99.5th percentile (2008–2017) a | 33.2 | 34.3 | 33.5 | 33.2 | 33.4 | |
| Chosen upper limit | 33.0 | 34.5 | 33.0 | 33.0 | 33.5 | |
| Temperature | 99.5th percentile (2000–2017) | 34.1 | 35.5 | 34.3 | 34.3 | 34.0 |
| 99.5th percentile (2008–2017) a | 34.2 | 35.6 | 34.4 | 34.3 | 33.9 | |
| Chosen upper limit | 34.0 | 35.5 | 34.5 | 34.5 | 34.0 | |
| (a) Category | Daily Emergency Visits (n b) | Daily Hospital Visits (n b) | Daily All-Cause Mortality a (n = 1840) | |||||||||
| Mean | SD | Min | Max | Mean | SD | Min | Max | Mean | SD | Min | Max | |
| Whole of Taiwan | 8 | 9 | 0 | 73 | 222 | 266 | 1 | 1533 | 357 | 56 | 187 | 510 |
| Sex | ||||||||||||
| Female | 2 | 3 | 0 | 26 | 126 | 155 | 0 | 855 | 145 | 26 | 67 | 230 |
| Male | 6 | 6 | 0 | 45 | 93 | 109 | 0 | 673 | 212 | 33 | 113 | 291 |
| Age (years) | ||||||||||||
| 0–14 | 1 | 1 | 0 | 7 | 9 | 9 | 0 | 63 | 3 | 2 | 0 | 10 |
| 15–64 | 6 | 7 | 0 | 51 | 189 | 231 | 0 | 1351 | 94 | 16 | 42 | 140 |
| ≥65 | 1 | 2 | 0 | 19 | 23 | 28 | 0 | 176 | 260 | 44 | 131 | 390 |
| Sub-region | ||||||||||||
| North Taiwan | 3 | 4 | 0 | 41 | 117 | 149 | 0 | 917 | 148 | 19 | 93 | 218 |
| Central Taiwan | 2 | 2 | 0 | 24 | 81 | 94 | 0 | 510 | 67 | 16 | 15 | 113 |
| South Taiwan | 2 | 3 | 0 | 23 | 17 | 20 | 0 | 152 | 121 | 30 | 25 | 182 |
| East Taiwan c | 1 | 2 | 0 | 15 | 9 | 11 | 0 | 67 | 21 | 5 | 7 | 40 |
| (b) Category | Daily Maximum WBGT (°C) (n b) | Daily Maximum Temperature (°C) (n b) | Daily Mean PM2.5 (μg/m3) (n d) | |||||||||
| Mean | SD | Min | Max | Mean | SD | Min | Max | Mean | SD | Min | Max | |
| Whole Taiwan island | 29.6 | 2.4 | 19.5 | 33.6 | 30.7 | 2.2 | 21.0 | 34.7 | 25.4 | 11.1 | 5.9 | 92.0 |
| North Taiwan | 29.4 | 3.3 | 16.3 | 35.5 | 30.6 | 3.2 | 18.3 | 37.1 | 22.1 | 10.7 | 2.1 | 106.5 |
| Central Taiwan | 29.3 | 2.2 | 19.2 | 34.3 | 30.7 | 2.1 | 19.9 | 37.9 | 27.8 | 14.9 | 5.0 | 139.7 |
| South Taiwan | 30.0 | 1.9 | 21.1 | 34.0 | 31.3 | 1.8 | 22.2 | 34.9 | 28.1 | 15.6 | 5.9 | 207.1 |
| East Taiwan c | 29.7 | 2.6 | 19.0 | 33.8 | 30.3 | 2.2 | 21.4 | 34.7 | 14.7 | 7.6 | 4.3 | 72.7 |
| (a) WBGT | RR (95%CI) a | |||||
| Threshold(°C) | 30 | 31 | 31.5 | 32 | 32.5 | |
| Heat-related emergency visits | ||||||
| Lag 0 | 1.27 *** (1.26,1.29) | 1.34 *** (1.32,1.36) | 1.38 *** (1.35,1.42) | 1.49 *** (1.44,1.54) | 1.83 *** (1.68,1.99) | |
| Lag 1 | 1.08 *** (1.07,1.10) | 1.10 *** (1.08,1.13) | 1.13 *** (1.10,1.16) | 1.17 *** (1.13,1.22) | 1.25 *** (1.14,1.37) | |
| Lag 2 | 1.00 (0.99,1.01) | 1.02 * (1.00,1.04) | 1.04 *** (1.02,1.07) | 1.07 *** (1.03,1.11) | 1.09 (0.99,1.20) | |
| Heat-related hospital visits | ||||||
| Lag 0 | 1.08 *** (1.08,1.09) | 1.09 *** (1.09,1.10) | 1.11 *** (1.10,1.11) | 1.15 *** (1.14,1.16) | 1.29 *** (1.27,1.31) | |
| Lag 1 | 1.04 *** (1.04,1.05) | 1.07 *** (1.07,1.07) | 1.09 *** (1.09,1.10) | 1.12 *** (1.12,1.13) | 1.21 *** (1.19,1.23) | |
| Lag 2 | 1.05 *** (1.05,1.05) | 1.07 *** (1.06,1.07) | 1.08 *** (1.08,1.09) | 1.11 *** (1.11,1.12) | 1.17 *** (1.15,1.19) | |
| All-cause mortality | ||||||
| Lag 0 | 1.00 *** (1.00,1.01) | 1.00 * (1.00,1.01) | 1.01 * (1.00,1.01) | 1.01 ** (1.00,1.02) | 1.03 ** (1.01,1.05) | |
| Lag 1 | 1.00 ** (1.00,1.01) | 1.01 *** (1.00,1.01) | 1.01 *** (1.01,1.02) | 1.03 *** (1.02,1.04) | 1.05 *** (1.03,1.08) | |
| Lag 2 | 1.00 (1.00,1.00) | 1.00 * (1.00,1.01) | 1.01 * (1.00,1.01) | 1.01 (1.00,1.02) | 1.03 * (1.00,1.05) | |
| (b) Temperature | RR (95%CI) a | |||||
| Threshold(°C) | 30 | 31 | 32 | 32.5 | 33 | 33.5 |
| Heat-related emergency visits | ||||||
| Lag 0 | 1.25 *** (1.24,1.26) | 1.28 *** (1.26,1.29) | 1.32 *** (1.29,1.34) | 1.33 *** (1.30,1.36) | 1.37 *** (1.33,1.42) | 1.66 *** (1.52,1.81) |
| Lag 1 | 1.06 *** (1.04,1.07) | 1.07 *** (1.05,1.08) | 1.08 *** (1.06,1.10) | 1.09 *** (1.07,1.12) | 1.11 *** (1.06,1.15) | 1.18 *** (1.07,1.29) |
| Lag 2 | 0.97 *** (0.96,0.98) | 0.97 *** (0.96,0.98) | 0.98 ** (0.96,0.99) | 0.99 (0.96,1.01) | 1.04 * (1.00,1.08) | 1.11 * (1.01,1.22) |
| Heat-related hospital visits | ||||||
| Lag 0 | 1.10 *** (1.10,1.10) | 1.11 *** (1.10,1.11) | 1.12 *** (1.12,1.12) | 1.14 *** (1.13,1.14) | 1.18 *** (1.17,1.19) | 1.31 *** (1.29,1.33) |
| Lag 1 | 1.03 *** (1.03,1.03) | 1.04 *** (1.04,1.04) | 1.06 *** (1.06,1.07) | 1.08 *** (1.08,1.09) | 1.10 *** (1.09,1.11) | 1.12 *** (1.10,1.14) |
| Lag 2 | 1.04 *** (1.04,1.04) | 1.04 *** (1.04,1.04) | 1.04 *** (1.04,1.04) | 1.05 *** (1.04,1.05) | 1.07 *** (1.06,1.08) | 1.15 *** (1.13,1.18) |
| All-cause mortality | ||||||
| Lag 0 | 1.00 *** (1.00,1.01) | 1.00 *** (1.00,1.01) | 1.01 *** (1.00,1.01) | 1.01 *** (1.01,1.02) | 1.02 *** (1.01,1.03) | 1.05 *** (1.02,1.07) |
| Lag 1 | 1.00 (1.00,1.00) | 1.00 * (1.00,1.01) | 1.01 ** (1.00,1.01) | 1.01 * (1.00,1.02) | 1.01 * (1.00,1.02) | 1.04 ** (1.01,1.07) |
| Lag 2 | 1.00 * (1.00,1.00) | 1.00 * (1.00,1.01) | 1.01 *** (1.00,1.01) | 1.01 *** (1.01,1.02) | 1.02 *** (1.01,1.03) | 1.04 ** (1.02,1.07) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lung, S.-C.C.; Yeh, J.-C.J.; Hwang, J.-S. Selecting Thresholds of Heat-Warning Systems with Substantial Enhancement of Essential Population Health Outcomes for Facilitating Implementation. Int. J. Environ. Res. Public Health 2021, 18, 9506. https://doi.org/10.3390/ijerph18189506
Lung S-CC, Yeh J-CJ, Hwang J-S. Selecting Thresholds of Heat-Warning Systems with Substantial Enhancement of Essential Population Health Outcomes for Facilitating Implementation. International Journal of Environmental Research and Public Health. 2021; 18(18):9506. https://doi.org/10.3390/ijerph18189506
Chicago/Turabian StyleLung, Shih-Chun Candice, Jou-Chen Joy Yeh, and Jing-Shiang Hwang. 2021. "Selecting Thresholds of Heat-Warning Systems with Substantial Enhancement of Essential Population Health Outcomes for Facilitating Implementation" International Journal of Environmental Research and Public Health 18, no. 18: 9506. https://doi.org/10.3390/ijerph18189506
APA StyleLung, S.-C. C., Yeh, J.-C. J., & Hwang, J.-S. (2021). Selecting Thresholds of Heat-Warning Systems with Substantial Enhancement of Essential Population Health Outcomes for Facilitating Implementation. International Journal of Environmental Research and Public Health, 18(18), 9506. https://doi.org/10.3390/ijerph18189506







