Orthodontic Extrusion vs. Surgical Extrusion to Rehabilitate Severely Damaged Teeth: A Literature Review
Abstract
:1. Introduction
- Surgical crown lengthening;
- Orthodontic extrusion;
- Surgical extrusion [11].
2. Materials and Methods
3. Results
4. Discussion
4.1. Orthodontic Extrusion
4.1.1. Advantages
4.1.2. Disadvantages
4.1.3. Complications
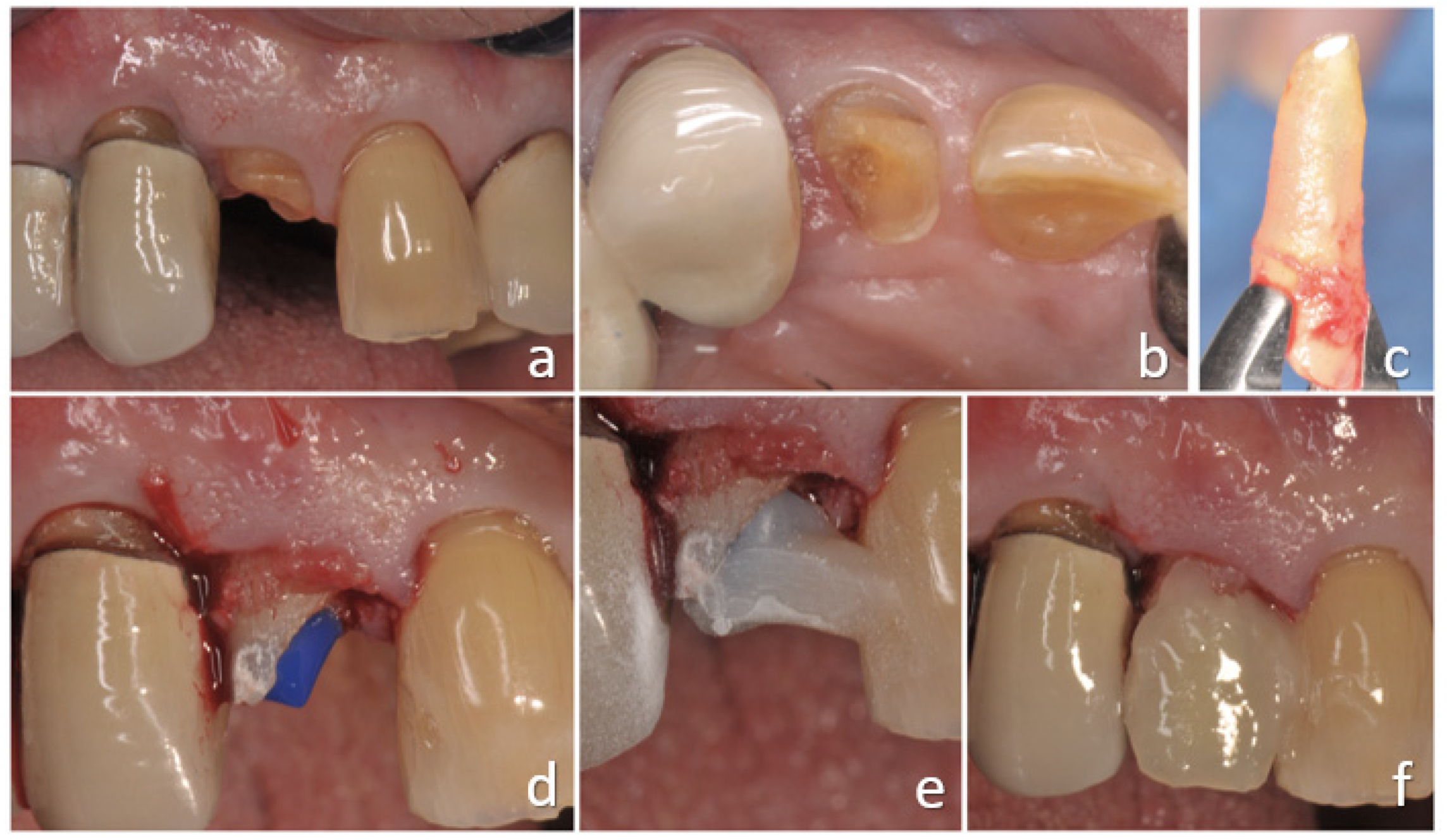
4.2. Surgical Extrusion
4.2.1. Advantages
4.2.2. Disadvantages
4.2.3. Complications
4.3. Combined Therapy
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Choi, Y.H.; Lee, H.J. Surgical extrusion of a maxillary premolar after orthodontic extrusion: A retrospective study. J. Korean Assoc. Oral Maxillofac. Surg. 2019, 45, 254–259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clark, D.; Levin, L. In the dental implant era, why do we still bother saving teeth? Dent. Traumatol. 2019, 35, 368–375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torabinejad, M.; Anderson, P.; Bader, J.; Brown, L.J.; Chen, L.H.; Goodacre, C.J.; Kattadiyil, M.T.; Kutsenko, D.; Lozada, J.; Patel, R.; et al. Outcomes of root canal treatment and restoration, implant-supported single crowns, fixed partial dentures, and extraction without replacement: A systematic review. J. Prosthet. Dent. 2007, 98, 285–311. [Google Scholar] [CrossRef]
- Juloski, J.; Radovic, I.; Goracci, C.; Vulicevic, Z.R.; Ferrari, M. Ferrule effect: A literature review. J. Endod. 2012, 38, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Stankiewicz, N.; Wilson, P. The ferrule effect: A literature review. Int. Endod. J. 2002, 35, 575–581. [Google Scholar] [CrossRef] [PubMed]
- Padbury, A.; Eber, R.; Wang, H.L. Interactions between the gingiva and the margin of restorations. J. Clin. Periodontol. 2003, 30, 379–385. [Google Scholar] [CrossRef]
- Gargiulo, A.; Krajewski, J.; Gargiulo, M. Defining biologic width in crown lengthening. CDS Rev. 1995, 5, 20–23. [Google Scholar]
- Schmidt, J.C.; Sahrmann, P.; Weiger, R.; Schmidlin, P.R.; Walter, C. Biologic width dimensions—A systematic review. J. Clin. Periodontol. 2013, 40, 493–504. [Google Scholar] [CrossRef]
- Hempton, T.; Dominici, J. Contermporary crown-lengthening therapy. J. Am. Dent. Assoc. 2014, 140, 648–654. [Google Scholar]
- Fugazzotto, P.; Parma-Benfenati, S. Preprosthetic periodontal considerations. Crown length and biologic width. Quintessence Int. Dent. Dig. 1984, 15, 1247–1256. [Google Scholar]
- Kelly, R.D.; Addison, O.; Tomson, P.L.; Krastl, G.; Dietrich, T. Atraumatic surgical extrusion to improve tooth restorability: A clinical report. J. Prosthet. Dent. 2016, 115, 649–653. [Google Scholar] [CrossRef]
- Lindhe, J.; Lang, N.P. Parodontologia Clinica e Implantologia Orale, 6th ed.; Edi-ermes: Milan, Italy, 2016. [Google Scholar]
- Planciunas, L.; Puriene, A.; Mackeviciene, G. Surgical lengthening of the clinical tooth crown. Stomatologija 2006, 8, 88–95. [Google Scholar] [PubMed]
- González-Martín, O.; Solano-Hernandez, B.; Torres, A.; González-Martín, S.; Avila-Ortiz, G. Orthodontic Extrusion: Guidelines for Contemporary Clinical Practice. Int. J. Periodontics Restor. Dent. 2020, 40, 667–676. [Google Scholar] [CrossRef] [PubMed]
- Bach, N.; Baylard, J.F.; Voyer, R. Orthodontic extrusion: Periodontal considerations and applications. J. Can. Dent. Assoc. 2004, 70, 775–780. [Google Scholar] [PubMed]
- Quirynen, M.; Op Heij, D.; Adriansens, A.; Opdebeeck, H.; Van Steenberghe, D. Periodontal health of orthodontically extruded impacted teeth. A split-mouth, long term clinical evaluation. J. Periodontol. 2000, 71, 1708–1714. [Google Scholar] [CrossRef]
- Alves, L.D.; Donnelly, J.C.; Lugo, A.; Carter, D.R. Reeruption and extrusion of a traumatically intruded immature permanent incisor: Case report. J. Endod. 1997, 23, 246–248. [Google Scholar] [CrossRef]
- Jacobs, S.G. The treatment of traumatized permanent anterior teeth: Case report & literature review. Part I--Management of intruded incisors. Aust. Orthod. J. 1995, 13, 213–218. [Google Scholar]
- Zyskind, K.; Zyskind, D.; Soskolne, W.A.; Harary, D. Orthodontic forced eruption: Case report of an alternative treatment for subgingivally fractured young permanent incisors. Quintessence Int. 1992, 23, 393–399. [Google Scholar]
- Ingber, J.S. Forced Eruption: Part I. A Method of Treating Isolated One and Two Wall Infrabony Osseous Defects-Rationale and Case Report. J. Periodontol. 1974, 45, 199–206. [Google Scholar] [CrossRef]
- Ogihara, S.; Wang, H.-L. Periodontal Regeneration With or Without Limited Orthodontics for the Treatment of 2- or 3-Wall Infrabony Defects. J. Periodontol. 2010, 81, 1734–1742. [Google Scholar] [CrossRef]
- Mantzikos, T.; Shamus, I. Case report: Forced eruption and implant site development. Angle Orthod. 1998, 68, 179–186. [Google Scholar]
- Paolone, M.G.; Kaitsas, R. Orthodontic-periodontal interactions: Orthodontic extrusion in interdisciplinary regenerative treatments. Int. Orthod. 2018, 16, 217–245. [Google Scholar] [CrossRef] [PubMed]
- Mesquita De Carvalho, P.F.; Joly, J.C.; Carvalho Da Silva, R.; González-Martín, O. Therapeutic alternatives for addressing pink esthetic complications in single-tooth implants: A proposal for a clinical decision tree. J. Esthet. Restor. Dent. 2019, 31, 403–414. [Google Scholar] [CrossRef] [PubMed]
- Salama, H.; Salama, M. The role of orthodontic extrusive remodeling in the enhancement of soft and hard tissue profiles prior to implant placement: A systematic approach to the management of extraction site defects. Int. J. Periodontics Restor. Dent. 1993, 13, 312–333. [Google Scholar]
- Nappen, D.; Kohlan, D. Orthodontic extrusion of premolar teeth: An improved technique. J. Prosthet. Dent. 1989, 61, 549–554. [Google Scholar] [CrossRef]
- Addy, L.D.; Durning, P.; Thomas, M.B.M.; McLaughlin, W.S. Orthodontic extrusion: An interdisciplinary approach to patient management. Dent. Update 2009, 36, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Retain, K. Clinical and histologic observations on tooth movement during and after orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 1967, 53, 721–745. [Google Scholar] [CrossRef]
- Da Silva, V.C.; de Molon, R.S.; Martins, R.P.; Ribeiro, F.S.; Pontes, A.E.F.; Zandim-Barcelos, D.L.; Leite, F.R.M.; Benatti Neto, C.; Marcantonio, R.A.C.; Cirelli, J.A. Effects of orthodontic tooth extrusion produced by different techniques, on the periodontal tissues: A histological study in dogs. Arch. Oral Biol. 2020, 116, 104768. [Google Scholar] [CrossRef]
- Carvalho, C.V.; Bauer, F.P.F.; Romito, G.A.; Pannuti, C.M.; De Micheli, G. Orthodontic extrusion with or without circumferential supracrestal fiberotomy and root planing. Int. J. Periodontics Restor. Dent. 2006, 26, 87–93. [Google Scholar]
- Palomo, F.; Kopczyk, R.A. Rationale and methods for crown lengthening. J. Am. Dent. Assoc. 1978, 96, 257–260. [Google Scholar] [CrossRef]
- Lythgoe, J.R.; Torabinejad, M.; Simon, J.H. Extrusion techniques for the general dentist. Gen Dent. 1980, 28, 42–43+46–49. [Google Scholar]
- Ainamo, J.; Talari, A. The increase with age of the width of attached gingiva. J. Periodontal Res. 1976, 11, 182–188. [Google Scholar] [CrossRef]
- Malmgren, O.; Malmgren, B.; Frykholm, A. Rapid orthodontic extrusion of crown root and cervical root fractured teeth. Dent. Traumatol. 1991, 7, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Horliana, R.F.; Horliana, A.C.R.T.; Do Vale Wuo, A.; Perez, F.E.G.; Abrão, J. Dental extrusion with orthodontic miniscrew anchorage: A case report describing a modified method. Case Rep. Dent. 2015, 2015, 909314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bondemark, L.; Kurol, J.; Hallonsten, A.L.; Andreasen, J.O. Attractive magnets for orthodontic extrusion of crown-root fractured teeth. Am. J. Orthod. Dentofac. Orthop. 1997, 112, 187–193. [Google Scholar] [CrossRef]
- Stevens, B.H.; Levine, R.A. Forced eruption: A multidisciplinary approach for form, function, and biologic predictability. Compend. Contin. Educ. Dent. 1998, 19, 994–998. [Google Scholar] [PubMed]
- Amsterdam, M. Periodontal prosthesis. Twenty-five years in retrospect. Alpha Omegan 1974, 67, 8–52. [Google Scholar] [PubMed]
- Scholtes, E.; Suttorp, C.M.; Loomans, B.A.; Van Elsas, P.; Schols, J.G. Combined orthodontic, surgical, and restorative approach to treat a complicated crown-root fracture in a maxillary central incisor. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 570–582. [Google Scholar] [CrossRef]
- Sabri, R. Crown lengthening by orthodontic extrusion. Principles and technics. J. Parodontol. 1989, 8, 197–204. [Google Scholar]
- Oesterle, L.J.; Wood, L.W. Raising The Root. J. Am. Dent. Assoc. 1991, 122, 193–198. [Google Scholar] [CrossRef]
- Miresmæili, A.F.; Mollabashi, V.; Gholami, L.; Farhadian, M.; Rezaei-Soufi, L.; Javanshir, B.; Malekshoar, M. Comparison of conventional and laser-aided fiberotomy in relapse tendency of rotated tooth: A randomized controlled clinical trial. Int. Orthod. 2019, 17, 103–113. [Google Scholar] [CrossRef] [PubMed]
- Taner, T.U.; Haydar, B.; Kavuklu, I.; Korkmaz, A. Short-term effects of fiberotomy on relapse of anterior crowding. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 617–623. [Google Scholar] [CrossRef] [PubMed]
- Mantzikos, T.; Shamus, I. Forced eruption and implant site development: Soft tissue response. Am. J. Orthod. Dentofac. Orthop. 1997, 112, 596–600. [Google Scholar] [CrossRef]
- Plotino, G.; Abella Sans, F.; Duggal, M.S.; Grande, N.M.; Krastl, G.; Nagendrababu, V.; Gambarini, G. Clinical procedures and outcome of surgical extrusion, intentional replantation and tooth autotransplantation—A narrative review. Int. Endod. J. 2020, 53, 1636–1652. [Google Scholar] [CrossRef]
- Das, B.; Muthu, M.S. Surgical extrusion as a treatment option for crown-root fracture in permanent anterior teeth: A systematic review. Dent. Traumatol. 2013, 29, 423–431. [Google Scholar] [CrossRef]
- Ozer, S.Y.; Uysal, I.; Bahsi, E. Surgical extrusion of a complete crown fractured tooth: A case report. Int. Dent. Res. 2011, 1, 70–74. [Google Scholar] [CrossRef]
- Kahnberg, K. Intraalveolar transplantation of teeth with crown-root fractures. J. Oral Maxillofac. Surg. 1985, 43, 38–42. [Google Scholar] [CrossRef]
- Kratchman, S. Intentional replantation. Dent. Clin. N. Am. 1997, 41, 603–617. [Google Scholar]
- Niemczyk, S.P. Re-inventing intentional replantation: A modification of the technique. Pract. Proced. Aesthet. Dent. 2001, 13, 433–439. [Google Scholar]
- Jang, Y.; Lee, S.-J.; Yoon, T.-C.; Roh, B.-D.; Kim, E. Survival Rate of Teeth with a C-shaped Canal after Intentional Replantation: A Study of 41 Cases for up to 11 Years. J. Endod. 2016, 42, 1320–1325. [Google Scholar] [CrossRef]
- Tegsjo, U.; Valerius-Olsson, H.; Olgart, K. Intra-alveolar transplantation of teeth with cervical root fractures. Swedsh Dent. J. 1978, 2, 73–82. [Google Scholar]
- Grossman, L.I. Intentional replantation of teeth. J. Am. Dent. Assoc. 1966, 72, 1111–1118. [Google Scholar] [CrossRef] [PubMed]
- Cooke, H.G.; Cox, F.L. C-shaped canal configurations in mandibular molars. J. Am. Dent. Assoc. 1979, 99, 836–839. [Google Scholar] [CrossRef] [PubMed]
- Bender, I.B.; Rossman, L.E. Intentional replantation of endodontically treated teeth. Oral Surg. Oral Med. Oral Pathol. 1993, 76, 623–630. [Google Scholar] [CrossRef]
- Lee, S.-J.; Jung, I.-Y.; Lee, C.-Y.; Choi, S.Y.; Kum, K.-Y. Clinical application of computer-aided rapid prototyping for tooth transplantation. Dent. Traumatol. 2001, 17, 114–119. [Google Scholar] [CrossRef]
- Strbac, G.D.; Schnappauf, A.; Giannis, K.; Bertl, M.H.; Moritz, A.; Ulm, C. Guided Autotransplantation of Teeth: A Novel Method Using Virtually Planned 3-dimensional Templates. J. Endod. 2016, 42, 1844–1850. [Google Scholar] [CrossRef]
- Anssari Moin, D.; Verweij, J.P.; Waars, H.; van Merkesteyn, R.; Wismeijer, D. Accuracy of Computer-Assisted Template-Guided Autotransplantation of Teeth With Custom Three-Dimensional Designed/Printed Surgical Tooling: A Cadaveric Study. J. Oral Maxillofac. Surg. 2017, 75, 925.e1–925.e7. [Google Scholar] [CrossRef] [PubMed]
- Gault, P.C.; Warocquier-Clerout, R. Tooth Auto-Transplantation With Double Periodontal Ligament Stimulation to Replace Periodontally Compromised Teeth. J. Periodontol. 2002, 73, 575–583. [Google Scholar] [CrossRef]
- Mejàre, B.; Wannfors, K.; Jansson, L. A prospective study on transplantation of third molars with complete root formation. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2004, 97, 231–238. [Google Scholar] [CrossRef]
- Isa-Kara, M.; Sari, F.; Emre-Coskun, M.; Kustarci, A.; Burak-Polat, H.; Ozdemir, H.; Polat, S. Stabilization of autotransplanted teeth using thermoplastic retainers. Med. Oral Patol. Oral Cir. Bucal 2011, 16, e369–e375. [Google Scholar] [CrossRef]
- Chung, W.-C.; Tu, Y.-K.; Lin, Y.-H.; Lu, H.-K. Outcomes of autotransplanted teeth with complete root formation: A systematic review and meta-analysis. J. Clin. Periodontol. 2014, 41, 412–423. [Google Scholar] [CrossRef]
- Nosonowitz, D.M. On intentional replantation. N. Y. J. Dent. 1972, 42, 44–47. [Google Scholar]
- Hammarstrom, L.; Blomlof, L.; Feiglin, B.; Andersson, L.; Lindskog, S. Replantation of teeth and antibiotic treatment. Dent. Traumatol. 1986, 2, 51–57. [Google Scholar] [CrossRef]
- Andreasen, J.O.; Paulsen, H.U.; Yu, Z.; Schwartz, O. A long-term study of 370 autotransplanted premolars. Part III. Periodontal healing subsequent to transplantation. Eur. J. Orthod. 1990, 12, 25–37. [Google Scholar] [CrossRef]
- Ahmed, H.M.A.; Neelakantan, P.; Dummer, P.M.H. A new system for classifying accessory canal morphology. Int. Endod. J. 2018, 51, 164–176. [Google Scholar] [CrossRef]
- Hupp, J.G.; Mesaros, S.V.; Aukhil, I.; Trope, M. Periodontal ligament vitality and histologic healing of teeth stored for extended periods before transplantation. Dent. Traumatol. 1998, 14, 79–83. [Google Scholar] [CrossRef]
- Krastl, G.; Filippi, A.; Zitzmann, N.; Walter, C.; Weiger, R. Current aspects of restoring traumatically fractured teeth. Eur. J. Esthet. Dent. 2011, 6, 124–141. [Google Scholar]
- Becker, B. Intentional replantation techniques: A critical review. J. Endod. 2018, 44, 14–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asgary, S.; Alim Marvasti, L.; Kolahdouzan, A. Indications and case series of intentional replantation of teeth. Iran. Endod. J. 2014, 9, 71–78. [Google Scholar] [PubMed]
- Elkhadem, A.; Mickan, S.; Richards, D. Adverse events of surgical extrusion in treatment for crown-root and cervical root fractures: A systematic review of case series/reports. Dent. Traumatol. 2014, 30, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Kahler, B.; Hu, J.-Y.; Marriot-Smith, C.; Heithersay, G. Splinting of teeth following trauma: A review and a new splinting recommendation. Aust. Dent. J. 2016, 61, 59–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Plotino, G.; Abella Sans, F.; Duggal, M.S.; Grande, N.M.; Krastl, G.; Nagendrababu, V.; Gambarini, G. European Society of Endodontology position statement: Surgical extrusion, intentional replantation and tooth autotransplantation: European Society of Endodontology developed by: The phrase above to be added with the authors on a line below. See as an exam. Int. Endod. J. 2021, 54, 655–659. [Google Scholar] [CrossRef]
- Kahnberg, K.-E. Surgical extrusion of root-fractured teeth-a follow-up study of two surgical methods. Dent. Traumatol. 1988, 4, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Kahnberg, K.E. Intra-alveolar transplantation. I. A 10-year follow-up of a method for surgical extrusion of root fractured teeth. Swed. Dent. J. 1996, 20, 165–172. [Google Scholar]
- Kahnberg, K.-E.; Warfvinge, J.; Birgersson, B. Intraalveolar transplantation. Int. J. Oral Surg. 1982, 11, 372–379. [Google Scholar] [CrossRef]
- Calisskan, M.K.; Turkun, M.; Gomel, M. Surgical extrusion of crown-root-fractured teeth: A clinical review. Int. Endod. J. 1999, 32, 146–151. [Google Scholar] [CrossRef]
- Khayat, A.; Fatehi, S. Clinical evaluation of forceps eruption: Reestablishing biologic width and restoring no restorable teeth. Iran. Endod. J. 2006, 1, 1–5. [Google Scholar]
- Pham, H.T.; Nguyen, P.A.; Pham, T.A.V. Periodontal status of anterior teeth following clinical crown lengthening by minimally traumatic controlled surgical extrusion. Dent. Traumatol. 2018, 34, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Krug, R.; Connert, T.; Soliman, S.; Syfrig, B.; Dietrich, T.; Krastl, G. Surgical extrusion with an atraumatic extraction system: A clinical study. J. Prosthet. Dent. 2018, 120, 879–885. [Google Scholar] [CrossRef]
- Nethravathy, R.; Vinoth, S.K.; Thomas, A.V. Three different surgical techniques of crown lengthening: A comparative study. J. Pharm. Bioallied Sci. 2013, 5, 14–17. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.-H.; Bae, J.-H. Clinical evaluation of a new extraction method for intentional replantation. J. Korean Acad. Conserv. Dent. 2011, 36, 211. [Google Scholar] [CrossRef] [Green Version]
- Choi, Y.; Bae, J.; Kim, Y.; Kim, H.; Kim, S.; Cho, B. Clinical outcome of intentional replantation with preoperative orthodontic extrusion: A retrospective study. Int. Endod. J. 2014, 47, 1168–1176. [Google Scholar] [CrossRef] [PubMed]
- Hong, B.; Bulsara, Y.; Gorecki, P.; Dietrich, T. Minimally invasive vertical versus conventional tooth extraction: An interrupted time series study. J. Am. Dent. Assoc. 2018, 149, 688–695. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hayashi, H. Ortho-Transplantation; Seoul Narae Publ. Co.: Seoul, Korea, 2006; pp. 8–15. [Google Scholar]




| Orthodontic Extrusion | Surgical Extrusion | |
|---|---|---|
| Indication | Rehabilitation of teeth with subgingival lesions or that are severely damaged; Treatment of restorations that violate the biological width; Correction of angular defects and pink aesthetic; Regeneration of the alveolar ridge (for implant purposes); Orthodontic extraction; Treatment of impacted teeth (canines). | Teeth that cannot be restored with conventional techniques with root anatomy compatible with atraumatic extraction (single-rooted teeth). Teeth with endodontic clinical scenarios difficult to treat through classic procedures that need to be extruded. |
| Contraindications | Ankylosis or hypercementosis; Vertical root fracture; Close proximity to the roots of adjacent teeth;Severe internal or external root resorption; Untreated periodontitis or periapical disease; Short roots and exposition of furcation in multirooted teeth. | Teeth with root anatomy not compatible with atraumatic extraction (e.g. multi-rooted teeth with divergent roots). Medical contraindications to any surgical therapy. |
| Advantages | Minimally invasive treatment: no loss of bone or periodontal tissue. Simple and predictable technique. Better crown/root ratio than surgical crown lengthening. | Rapidity: in just one time it is possible to obtain the extrusion of the desired amount and the correction of endodontic problems, with the possibility to inspect and treat otherwise inaccessible areas without damaging the contiguous elements. Compared to surgical crown lengthening, less bone loss and better maintenance of the interproximal papilla. Compared to orthodontic extrusion: less coronal migration of support tissues and much shorter time of therapy required. |
| Disadvantages | Long time of treatment required; Worsening oral hygiene and aesthetic problems; High patient compliance required if fiberotomy is performed weekly. | Risk of ankylosis and root resorption due to periodontal ligament trauma; Absence of a universal protocol. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cordaro, M.; Staderini, E.; Torsello, F.; Grande, N.M.; Turchi, M.; Cordaro, M. Orthodontic Extrusion vs. Surgical Extrusion to Rehabilitate Severely Damaged Teeth: A Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 9530. https://doi.org/10.3390/ijerph18189530
Cordaro M, Staderini E, Torsello F, Grande NM, Turchi M, Cordaro M. Orthodontic Extrusion vs. Surgical Extrusion to Rehabilitate Severely Damaged Teeth: A Literature Review. International Journal of Environmental Research and Public Health. 2021; 18(18):9530. https://doi.org/10.3390/ijerph18189530
Chicago/Turabian StyleCordaro, Martina, Edoardo Staderini, Ferruccio Torsello, Nicola Maria Grande, Matteo Turchi, and Massimo Cordaro. 2021. "Orthodontic Extrusion vs. Surgical Extrusion to Rehabilitate Severely Damaged Teeth: A Literature Review" International Journal of Environmental Research and Public Health 18, no. 18: 9530. https://doi.org/10.3390/ijerph18189530
APA StyleCordaro, M., Staderini, E., Torsello, F., Grande, N. M., Turchi, M., & Cordaro, M. (2021). Orthodontic Extrusion vs. Surgical Extrusion to Rehabilitate Severely Damaged Teeth: A Literature Review. International Journal of Environmental Research and Public Health, 18(18), 9530. https://doi.org/10.3390/ijerph18189530







