Association between Financial Hardship and Symptom Burden in Patients Receiving Maintenance Dialysis: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
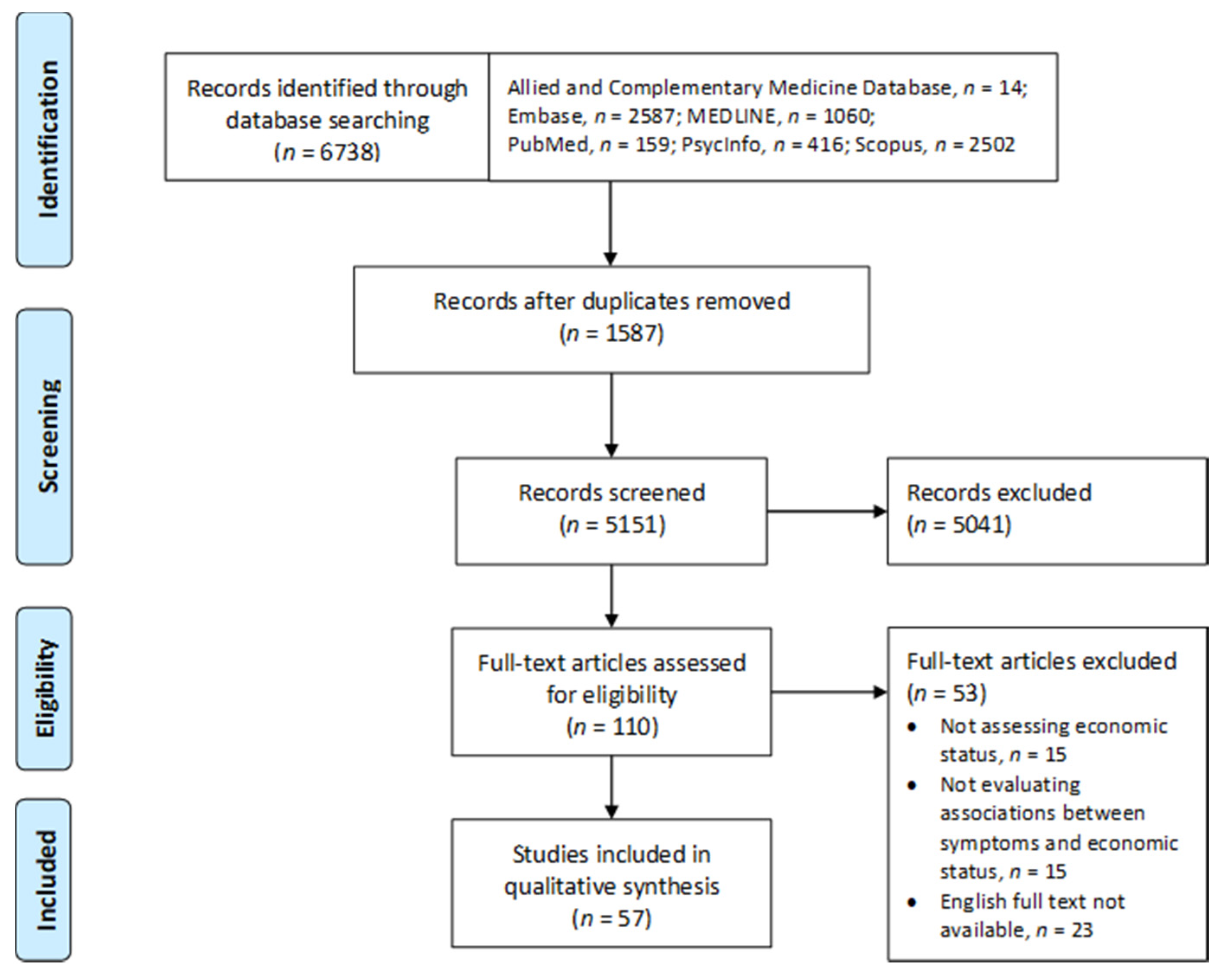
2.1. Search Methods
2.2. Search Outcomes
2.3. Data Abstraction and Synthesis
2.4. Quality Appraisal
3. Results
3.1. Study Characteristics
3.2. Quality Appraisal
3.3. Assessment of Financial Hardship
3.4. Associations with Financial Hardship
3.4.1. Symptom Burden
3.4.2. Depression
3.4.3. Anxiety
3.4.4. Fatigue
3.4.5. Sexual Dysfunction
3.4.6. Sleep Problems
3.4.7. Pain
3.4.8. Itching
4. Discussion
4.1. Limitations and Recommendations
4.2. Relevance to Clinical Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2020, 395, 709–733. [Google Scholar] [CrossRef]
- Luyckx, V.A.; Tonelli, M.; Stanifer, J.W. The global burden of kidney disease and the sustainable development goals. Bull. World Health Organ. 2018, 96, 414–422. [Google Scholar] [CrossRef]
- Silva Junior, G.B.D.; Oliveira, J.G.R.; Oliveira, M.R.B.; Vieira, L.; Dias, E.R. Global costs attributed to chronic kidney disease: A systematic review. Rev. Assoc. Med. Bras. 2018, 64, 1108–1116. [Google Scholar] [CrossRef]
- Krishnan, M. The importance of considering total patient economics for hemodialysis. Kidney Int. Rep. 2019, 4, 365–366. [Google Scholar] [CrossRef]
- van der Tol, A.; Lameire, N.; Morton, R.L.; Van Biesen, W.; Vanholder, R. An international analysis of dialysis services reimbursement. Clin. J. Am. Soc. Nephrol. 2019, 14, 84–93. [Google Scholar] [CrossRef]
- Luyckx, V.A.; Miljeteig, I.; Ejigu, A.M.; Moosa, M.R. Ethical challenges in the provision of dialysis in resource-constrained environments. Semin. Nephrol. 2017, 37, 273–286. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.C.W.; Yu, X.; Chen, H.C.; Kashihara, N.; Park, H.C.; Liew, A.; Goh, B.L.; Nazareth, M.G.C.; Bunnag, S.; Tan, J.; et al. Dialysis care and dialysis funding in Asia. Am. J. Kidney Dis. 2020, 75, 772–781. [Google Scholar] [CrossRef]
- Walker, R.C.; Howard, K.; Tong, A.; Palmer, S.C.; Marshall, M.R.; Morton, R.L. The economic considerations of patients and caregivers in choice of dialysis modality. Hemodial. Int. 2016, 20, 634–642. [Google Scholar] [CrossRef] [PubMed]
- Hallab, A.; Wish, J.B. Employment among patients on dialysis: An unfulfilled promise. Clin. J. Am. Soc. Nephrol. 2018, 13, 203–204. [Google Scholar] [CrossRef]
- Turin, T.C.; Tonelli, M.; Manns, B.J.; Ravani, P.; Ahmed, S.B.; Hemmelgarn, B.R. Chronic kidney disease and life expectancy. Nephrol. Dial. Transpl. 2012, 27, 3182–3186. [Google Scholar] [CrossRef]
- van de Luijtgaarden, M.W.; Jager, K.J.; Segelmark, M.; Pascual, J.; Collart, F.; Hemke, A.C.; Remón, C.; Metcalfe, W.; Miguel, A.; Kramar, R.; et al. Trends in dialysis modality choice and related patient survival in the ERA-EDTA Registry over a 20-year period. Nephrol. Dial. Transpl. 2016, 31, 120–128. [Google Scholar] [CrossRef]
- Janssen, D.J.; Schols, J.M.; Wouters, E.F.; Spruit, M.A. One-year stability of care dependency in patients with advanced chronic organ failure. J. Am. Med. Dir. Assoc. 2014, 15, 127–132. [Google Scholar] [CrossRef]
- Carrera, P.M.; Kantarjian, H.M.; Blinder, V.S. The financial burden and distress of patients with cancer: Understanding and stepping-up action on the financial toxicity of cancer treatment. CA Cancer J. Clin. 2018, 68, 153–165. [Google Scholar] [CrossRef]
- Altice, C.K.; Banegas, M.P.; Tucker-Seeley, R.D.; Yabroff, K.R. Financial hardships experienced by cancer survivors: A systematic review. J. Natl. Cancer Inst. 2017, 109, djw205. [Google Scholar] [CrossRef] [PubMed]
- Caraballo, C.; Valero-Elizondo, J.; Khera, R.; Mahajan, S.; Grandhi, G.R.; Virani, S.S.; Mszar, R.; Krumholz, H.M.; Nasir, K. Burden and consequences of financial hardship from medical bills among nonelderly adults with diabetes mellitus in the United States. Circ. Cardiovasc. Qual. Outcomes 2020, 13, e006139. [Google Scholar] [CrossRef]
- Hobbs, M.; Thakur, K. Financial toxicity as an unforeseen side effect of inflammatory bowel disease. Crohns. Colitis 360 2019, 1, otz024. [Google Scholar] [CrossRef]
- Chan, R.J.; Gordon, L.G.; Tan, C.J.; Chan, A.; Bradford, N.K.; Yates, P.; Agbejule, O.A.; Miaskowski, C. Relationships between financial toxicity and symptom burden in cancer survivors: A systematic review. J. Pain Symptom. Manag. 2019, 57, 646–660. [Google Scholar] [CrossRef] [PubMed]
- Ikonomou, M.; Skapinakis, P.; Balafa, O.; Eleftheroudi, M.; Damigos, D.; Siamopoulos, K.C. The impact of socioeconomic factors on quality of life of patients with chronic kidney disease in Greece. J. Ren. Care 2015, 41, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Tao, S.; Zeng, X.; Liu, J.; Fu, P. Socioeconomic status and mortality among dialysis patients: A systematic review and meta-analysis. Int. Urol. Nephrol. 2019, 51, 509–518. [Google Scholar] [CrossRef]
- Dodd, R.; Palagyi, A.; Guild, L.; Jha, V.; Jan, S. The impact of out-of-pocket costs on treatment commencement and adherence in chronic kidney disease: A systematic review. Health Policy Plan. 2018, 33, 1047–1054. [Google Scholar] [CrossRef]
- Klarenbach, S.W.; Tonelli, M.; Chui, B.; Manns, B.J. Economic evaluation of dialysis therapies. Nat. Rev. Nephrol. 2014, 10, 644–652. [Google Scholar] [CrossRef] [PubMed]
- Chan, R.J.; Gordon, L.; Zafar, S.Y.; Miaskowski, C. Financial toxicity and symptom burden: What is the big deal? Support. Care Cancer 2018, 26, 1357–1359. [Google Scholar] [CrossRef] [PubMed]
- Almutary, H.; Bonner, A.; Douglas, C. Symptom burden in chronic kidney disease: A review of recent literature. J. Ren. Care 2013, 39, 140–150. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Moola, S.; Munn, Z.; Sears, K.; Sfetcu, R.; Currie, M.; Lisy, K.; Tufanaru, C.; Qureshi, R.; Mattis, P.; Mu, P. Conducting systematic reviews of association (etiology): The Joanna Briggs Institute’s approach. Int. J. Evid. Based Healthc. 2015, 13, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Munn, Z.; Barker, T.H.; Moola, S.; Tufanaru, C.; Stern, C.; McArthur, A.; Stephenson, M.; Aromataris, E. Methodological quality of case series studies: An introduction to the JBI critical appraisal tool. JBI Evid. Synth. 2020, 18, 2127–2133. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Zhou, Y.; Guo, C.X.; Zhao, J.F. The relationship among hope, symptom distress, social support, coping style and monthly income in maintenance hemodialysis patients: A structural equation model. Int. J. Clin. Exp. Med. 2016, 9, 19717–19724. [Google Scholar]
- Hu, A.; Xue, Z.; Mwansisya, T.E.; Zhou, A.; Pu, W.; Chen, X.; Sun, M.; Wang, P.; Fan, H.; Wang, Z.; et al. Major depressive disorder in hemodialysis patients in China. Asia Pac. Psychiatry 2015, 7, 78–84. [Google Scholar] [CrossRef]
- Li, Z.J.; An, X.; Mao, H.P.; Wei, X.; Chen, J.H.; Yang, X.; Zhou, S.F.; Li, Z.B.; Yu, X.Q. Association between depression and malnutrition-Inflammation complex syndrome in patients on continuous ambulatory peritoneal dialysis. Int. Urol. Nephrol. 2011, 43, 875–882. [Google Scholar] [CrossRef]
- Wang, S.Y.; Zang, X.Y.; Fu, S.H.; Bai, J.; Liu, J.D.; Tian, L.; Feng, Y.Y.; Zhao, Y. Factors related to fatigue in Chinese patients with end-stage renal disease receiving maintenance hemodialysis: A multi-center cross-sectional study. Ren. Fail. 2016, 38, 442–450. [Google Scholar] [CrossRef]
- Ye, X.Q.; Chen, W.Q.; Lin, J.X.; Wang, R.P.; Zhang, Z.H.; Yang, X.; Yu, X.Q. Effect of social support on psychological-stress-induced anxiety and depressive symptoms in patients receiving peritoneal dialysis. J. Psychosom. Res. 2008, 65, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Huang, C.; Li, Y.; Chen, J.; Shen, F.; Yao, Q.; Qian, J.; Bao, B.; Yao, X. Health-related quality of life in dialysis patients with constipation: A cross-sectional study. Patient Prefer. Adherence 2013, 7, 589–594. [Google Scholar] [CrossRef]
- Zuo, M.; Tang, J.; Xiang, M.; Long, Q.; Dai, J.; Hu, X. Relationship between fatigue symptoms and subjective and objective indicators in hemodialysis patients. Int. Urol. Nephrol. 2018, 50, 1329–1339. [Google Scholar] [CrossRef]
- Araujo, S.M.H.A.; de Bruin, V.M.S.; Daher, E.F.; Almeida, G.H.; Medeiros, C.A.M.; de Bruin, P.F.C. Risk factors for depressive symptoms in a large population on chronic hemodialysis. Int. Urol. Nephrol. 2012, 44, 1229–1235. [Google Scholar] [CrossRef]
- de Alencar, S.B.V.; de Lima, F.M.; Dias, L.D.A.; Dias, V.D.A.; Lessa, A.C.; Bezerra, J.M.; Apolinário, J.F.; de Petribu, K.C. Depression and quality of life in older adults on hemodialysis. Braz. J. Psychiatry 2020, 42, 195–200. [Google Scholar] [CrossRef] [PubMed]
- de Brito, D.C.S.; Machado, E.L.; Reis, I.A.; de Freitas do Carmo, L.P.; Cherchiglia, M.L. Depression and anxiety among patients undergoing dialysis and kidney transplantation: A cross-sectional study. Sao Paulo Med. J. 2019, 137, 137–147. [Google Scholar] [CrossRef]
- Ramirez, S.P.; Macêdo, D.S.; Sales, P.M.G.; Figueiredo, S.M.; Daher, E.F.; Araújo, S.M.; Pargament, K.I.; Hyphantis, T.N.; Carvalho, A.F. The relationship between religious coping, psychological distress and quality of life in hemodialysis patients. J. Psychosom. Res. 2012, 72, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Sesso, R.; Rodrigues-Neto, J.F.; Ferraz, M.B. Impact of socioeconomic status on the quality of life of ESRD patients. Am. J. Kidney Dis. 2003, 41, 186–195. [Google Scholar] [CrossRef]
- Ersoy, N.A.; Akyar, I. Multidimensional pruritus assessment in hemodialysis patients. BMC Nephrol. 2019, 20, 42. [Google Scholar] [CrossRef]
- Karakan, S.; Sezer, S.; Ozdemir, F.N. Factors related to fatigue and subgroups of fatigue in patients with end-stage renal disease. Clin. Nephrol. 2011, 76, 358–364. [Google Scholar] [CrossRef]
- Mollaoglu, M. Fatigue in people undergoing hemodialysis. Dial. Transpl. 2009, 38, 216–220. [Google Scholar] [CrossRef]
- Sezer, S.; Uyar, M.E.; Bal, Z.; Tutal, E.; Ozdemir Acar, F.N. The influence of socioeconomic factors on depression in maintenance hemodialysis patients and their caregivers. Clin. Nephrol. 2013, 80, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Tezel, A.; Karabulutlu, E.; Şahin, O. Depression and perceived social support from family in Turkish patients with chronic renal failure treated by hemodialysis. J. Res. Med. Sci. 2011, 16, 666–673. [Google Scholar]
- Drayer, R.A.; Piraino, B.; Reynolds III, C.F.; Houck, P.R.; Mazumdar, S.; Bernardini, J.; Shear, M.K.; Rollman, B.L. Characteristics of depression in hemodialysis patients: Symptoms, quality of life and mortality risk. Gen. Hosp. Psychiatry 2006, 28, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Jhamb, M.; Argyropoulos, C.; Steel, J.L.; Plantinga, L.; Wu, A.W.; Fink, N.E.; Powe, N.R.; Meyer, K.B.; Unruh, M.L. Correlates and outcomes of fatigue among incident dialysis patients. Clin. J. Am. Soc. Nephrol. 2009, 4, 1779–1786. [Google Scholar] [CrossRef] [PubMed]
- Jhamb, M.; Pike, F.; Ramer, S.; Argyropoulos, C.; Steel, J.; Dew, M.A.; Weisbord, S.D.; Weissfeld, L.; Unruh, M. Impact of fatigue on outcomes in the hemodialysis (HEMO) study. Am. J. Nephrol. 2011, 33, 515–523. [Google Scholar] [CrossRef] [PubMed]
- Kutner, N.G.; Zhang, R.; Huang, Y.; Johansen, K.L. Depressed mood, usual activity level, and continued employment after starting dialysis. Clin. J. Am. Soc. Nephrol. 2010, 5, 2040–2045. [Google Scholar] [CrossRef]
- Song, M.K.; Ward, S.E.; Hladik, G.A.; Bridgman, J.C.; Gilet, C.A. Depressive symptom severity, contributing factors, and self-management among chronic dialysis patients. Hemodial. Int. 2016, 20, 286–292. [Google Scholar] [CrossRef]
- AlShahrani, M.A.; Alayed, A.S.M.; AlShehri, A.H.; Solaiman, O.; Awadalla, N.J.; Alhomrany, M. Depression and impaired work productivity among hemodialysis patients in south region of Saudi Arabia. Saudi J. Kidney Dis. Transpl. 2018, 29, 1133–1138. [Google Scholar] [CrossRef]
- Biniaz, V.; Tayybi, A.; Nemati, E.; Sadeghi Shermeh, M.; Ebadi, A. Different aspects of fatigue experienced by patients receiving maintenance dialysis in hemodialysis units. Nephrourol. Mon. 2013, 5, 897–900. [Google Scholar] [CrossRef]
- Einollahi, B.; Motalebi, M.; Rostami, Z.; Nemati, E.; Salesi, M. Sleep quality among Iranian hemodialysis patients: A multicenter study. Nephrourol. Mon. 2015, 7, e23849. [Google Scholar] [CrossRef]
- Fleishman, T.T.; Dreiher, J.; Shvartzman, P. Pain in maintenance hemodialysis patients: A multicenter study. J. Pain Symptom. Manag. 2018, 56, 178–184. [Google Scholar] [CrossRef]
- Fleishman, T.T.; Dreiher, J.; Shvartzman, P. Patient-reported outcomes in maintenance hemodialysis: A cross-sectional, multicenter study. Qual. Life Res. 2020, 29, 2345–2354. [Google Scholar] [CrossRef]
- Gatmiri, S.M.; Bordbar, M.; Raisi, F.; Nourian, A. Sexual dysfunction in female hemodialysis patients: A cross sectional study in Iran. Acta Med. Iran. 2019, 57, 244–252. [Google Scholar] [CrossRef]
- Ibrahim, S.; El Salamony, O. Depression, quality of life and malnutrition-inflammation scores in hemodialysis patients. Am. J. Nephrol. 2008, 28, 784–791. [Google Scholar] [CrossRef] [PubMed]
- Karasneh, R.; Al-Azzam, S.; Altawalbeh, S.M.; Alshogran, O.Y.; Hawamdeh, S. Predictors of symptom burden among hemodialysis patients: A cross-sectional study at 13 hospitals. Int. Urol. Nephrol. 2020, 52, 959–967. [Google Scholar] [CrossRef] [PubMed]
- Turkistani, I.; Nuqali, A.; Badawi, M.; Taibah, O.; Alserihy, O.; Morad, M.; Kalantan, E. The prevalence of anxiety and depression among end-stage renal disease patients on hemodialysis in Saudi Arabia. Ren. Fail. 2014, 36, 1510–1515. [Google Scholar] [CrossRef]
- Ahlawat, R.; Tiwari, P.; D’Cruz, S. Prevalence of depression and its associated factors among patients of chronic kidney disease in a public tertiary care hospital in India: A cross-sectional study. Saudi J. Kidney Dis. Transpl. 2018, 29, 1165–1173. [Google Scholar] [CrossRef] [PubMed]
- Anees, M.; Barki, H.; Masood, M.; Ibrahim, M.; Mumtaz, A. Depression in hemodialysis patients. Pak. J. Med. Sci. 2008, 24, 560–565. [Google Scholar]
- Anees, M.; Batool, S.; Imtiaz, M.; Ibrahim, M. Socio-economic factors affecting quality of life of hemodialysis patients and its effects on mortality. Pak. J. Med. Sci 2018, 34, 811–816. [Google Scholar] [CrossRef] [PubMed]
- Mathews, T.G.; Mathew, E. A study on anxiety among hemodialysis patients in Kerala. J. Psychol. Res. 2017, 12, 295–303. [Google Scholar]
- Rai, M.; Rustagi, T.; Rustagi, S.; Kohli, R. Depression, insomnia and sleep apnea in patients on maintenance hemodialysis. Indian J. Nephrol. 2011, 21, 223–229. [Google Scholar] [CrossRef]
- Saeed, Z.; Ahmad, A.M.; Shakoor, A.; Ghafoor, F.; Kanwal, S. Depression in patients on hemodialysis and their caregivers. Saudi J. Kidney Dis. Transpl. 2012, 23, 946–952. [Google Scholar] [CrossRef] [PubMed]
- Zubair, U.B.; Butt, B. Assessment of quality of sleep and its relationship with psychiatric morbidity and socio-demographic factors in the patients of chronic renal disease undergoing hemodialysis. J. Coll. Physicians Surg. Pak. 2017, 27, 427–431. [Google Scholar] [PubMed]
- Saglimbene, V.; Natale, P.; Palmer, S.; Scardapane, M.; Craig, J.C.; Ruospo, M.; Gargano, L.; Lucisano, G.; Török, M.; Celia, E.; et al. The prevalence and correlates of low sexual functioning in women on hemodialysis: A multinational, cross-sectional study. PLoS ONE 2017, 12, e0179511. [Google Scholar] [CrossRef]
- Strippoli, G.F.M. Sexual dysfunction in women with ESRD requiring hemodialysis. Clin. J. Am. Soc. Nephrol. 2012, 7, 974–981. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sugisawa, H.; Shimizu, Y.; Kumagai, T.; Sugisaki, H.; Ohira, S.; Shinoda, T. Effects of socioeconomic status on physical and mental health of hemodialysis patients in Japan: Differences by age, period, and cohort. Int. J. Nephrol. Dis. 2016, 9, 171–182. [Google Scholar] [CrossRef] [PubMed]
- Lai, K.Y.; Chan, H.S.Y.; Leung, V.K.H.; Mok, L.Y.H.; Chow, K.M.; Law, M.C.; Chung, K.Y.; Leung, C.B.; Li, P.K.T.; Szeto, C.C. Prevalence of psychological problems in Chinese peritoneal dialysis patients. Hong Kong J. Nephrol. 2005, 7, 82–89. [Google Scholar] [CrossRef][Green Version]
- Ng, M.S.N.; Wong, C.L.; Choi, K.C.; Hui, Y.H.; Ho, E.H.S.; Miaskowski, C.; So, W.K.W. A mixed methods study of symptom experience in patients with end-stage renal disease. Nurs. Res. 2021, 70, 34–43. [Google Scholar] [CrossRef]
- Rebollo Rubio, A.; Morales Asencio, J.M.; Eugenia Pons Raventos, M. Depression, anxiety and health-related quality of life amongst patients who are starting dialysis treatment. J. Ren. Care 2017, 43, 73–82. [Google Scholar] [CrossRef]
- Cheng, H.T.; Ho, M.C.; Hung, K.Y. Affective and cognitive rather than somatic symptoms of depression predict 3-year mortality in patients on chronic hemodialysis. Sci. Rep. 2018, 8, 5868. [Google Scholar] [CrossRef] [PubMed]
- Ng, H.J.; Tan, W.J.; Mooppil, N.; Newman, S.; Griva, K. Prevalence and patterns of depression and anxiety in hemodialysis patients: A 12-month prospective study on incident and prevalent populations. Br. J. Health Psychol. 2015, 20, 374–395. [Google Scholar] [CrossRef] [PubMed]
- Dimova, R.; Keskinova, D.; Tzekov, V.; Ginova-Noncheva, G. Health-Related quality of life in end-stage renal disease patients, using the Missoula-Vitas quality of life index: A multicenter study. Med. Pharm. Rep. 2019, 92, 374–381. [Google Scholar] [CrossRef]
- Čengić, B.; Resić, H. Depression in hemodialysis patients. Bosn. J. Basic Med. Sci. 2010, 10, S73–S78. [Google Scholar] [CrossRef]
- Ganu, V.J.; Boima, V.; Adjei, D.N.; Yendork, J.S.; Dey, I.D.; Yorke, E.; Mate-Kole, C.C.; Mate-Kole, M.O. Depression and quality of life in patients on long term hemodialysis at a national hospital in Ghana: A cross-sectional study. Ghana Med. J. 2018, 52, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Gerogianni, G.; Lianos, E.; Kouzoupis, A.; Polikandrioti, M.; Grapsa, E. The role of socio-demographic factors in depression and anxiety of patients on hemodialysis: An observational cross-sectional study. Int. Urol. Nephrol. 2018, 50, 143–154. [Google Scholar] [CrossRef]
- Jeon, H.O.; Kim, J.; Kim, O. Factors affecting depressive symptoms in employed hemodialysis patients with chronic renal failure. Psychol. Health Med. 2020, 25, 940–949. [Google Scholar] [CrossRef] [PubMed]
- Park, H.C.; Yoon, H.B.; Son, M.J.; Jung, E.S.; Joo, K.W.; Chin, H.J.; Oh, K.H.; Lim, C.S.; Kim, Y.S.; Ahn, C.; et al. Depression and health-related quality of life in maintenance hemodialysis patients. Clin. Nephrol. 2010, 73, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Sousa, L.M.M.; Antunes, A.V.; Marques-Vieira, C.M.A.; Silva, P.C.L.; Valentim, O.M.M.S.; José, H.M.G. Subjective wellbeing, sense of humor and psychological health in hemodialysis patients. Enferm. Nefrol. 2019, 22, 34–41. [Google Scholar] [CrossRef]
- Trbojević-Stanković, J.; Stojimirović, B.; Bukumirić, Z.; Hadzibulić, E.; Andrić, B.; Djordjević, V.; Marjanović, Z.; Birdjozlić, F.; Nesić, D.; Jovanović, D. Depression and quality of sleep in maintenance hemodialysis patients. Srp. Arh. Celok. Lek. 2014, 142, 437–443. [Google Scholar] [CrossRef]
- Yoong, R.K.; Mooppil, N.; Khoo, E.Y.; Newman, S.P.; Lee, V.Y.; Kang, A.W.; Griva, K. Prevalence and determinants of anxiety and depression in end stage renal disease (ESRD). A comparison between ESRD patients with and without coexisting diabetes mellitus. J. Psychosom. Res. 2017, 94, 68–72. [Google Scholar] [CrossRef]
- Bai, Y.L.; Lai, L.Y.; Lee, B.O.; Chang, Y.Y.; Chiou, C.P. The impact of depression on fatigue in patients with haemodialysis: A correlational study. J. Clin. Nurs. 2015, 24, 2014–2022. [Google Scholar] [CrossRef]
- Liu, H.E. Fatigue and associated factors in hemodialysis patients in Taiwan. Res. Nurs. Health 2006, 29, 40–50. [Google Scholar] [CrossRef]
- Huang, C.W.; Wee, P.H.; Low, L.L.; Koong, Y.L.A.; Htay, H.; Fan, Q.; Foo, W.Y.M.; Seng, J.J.B. Prevalence and risk factors for elevated anxiety symptoms and anxiety disorders in chronic kidney disease: A systematic review and meta-analysis. Gen. Hosp. Psychiatry 2021, 69, 27–40. [Google Scholar] [CrossRef] [PubMed]
- Kendall, M.; Carduff, E.; Lloyd, A.; Kimbell, B.; Cavers, D.; Buckingham, S.; Boyd, K.; Grant, L.; Worth, A.; Pinnock, H.; et al. Different experiences and goals in different advanced diseases: Comparing serial interviews with patients with cancer, organ failure, or frailty and their family and professional carers. J. Pain Symptom. Manag. 2015, 50, 216–224. [Google Scholar] [CrossRef]
- Essue, B.M.; Wong, G.; Chapman, J.; Li, Q.; Jan, S. How are patients managing with the costs of care for chronic kidney disease in Australia? A cross-sectional study. BMC Nephrol. 2013, 14, 5. [Google Scholar] [CrossRef] [PubMed]
- Chan, R.; Steel, Z.; Brooks, R.; Heung, T.; Erlich, J.; Chow, J.; Suranyi, M. Psychosocial risk and protective factors for depression in the dialysis population: A systematic review and meta-regression analysis. J. Psychosom. Res. 2011, 71, 300–310. [Google Scholar] [CrossRef] [PubMed]
- Keskin, G.; Babacan Gümüş, A.; Taşdemir Yiğitoğlu, G. Sexual dysfunctions and related variables with sexual function in patients who undergo dialysis for chronic renal failure. J. Clin. Nurs. 2019, 28, 257–269. [Google Scholar] [CrossRef] [PubMed]
- Jeon, Y.H.; Essue, B.; Jan, S.; Wells, R.; Whitworth, J.A. Economic hardship associated with managing chronic illness: A qualitative inquiry. BMC Health Serv. Res. 2009, 9, 182. [Google Scholar] [CrossRef]
- Darby, K.; Davis, C.; Likes, W.; Bell, J. Exploring the financial impact of breast cancer for African American medically underserved women: A qualitative study. J. Health Care Poor Underserved 2009, 20, 721–728. [Google Scholar] [CrossRef]
- Ng, M.S.N.; Wong, C.L.; Ho, E.H.S.; Hui, Y.H.; Miaskowski, C.; So, W.K.W. Burden of living with multiple concurrent symptoms in patients with end-stage renal disease. J. Clin. Nurs. 2020, 29, 2589–2601. [Google Scholar] [CrossRef] [PubMed]
- Ng, M.S.N.; Choi, K.C.; Chan, D.N.S.; Wong, C.L.; Xing, W.; Ho, P.S.; Au, C.; Chan, M.; Tong, M.; Ling, W.M.; et al. Identifying a cut-off score for the COST measure to indicate high financial toxicity and low quality of life among cancer patients. Support. Care Cancer 2021. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.K.H.; Chen, J.; Fung, S.K.S.; Mok, M.M.Y.; Cheng, Y.L.; Kong, I.; Lo, W.K.; Lui, S.L.; Chan, T.M.; Lam, C.L.K. Direct and indirect costs of end-stage renal disease patients in the first and second years after initiation of nocturnal home haemodialysis, hospital haemodialysis and peritoneal dialysis. Nephrol. Dial. Transpl. 2019, 34, 1565–1576. [Google Scholar] [CrossRef]
- OECD; Eurostat; World Health Organization. A System of Health Accounts 2011: Revised Edition. 2017. Available online: http://doi:10.1787/9789264270985-en (accessed on 25 August 2021). [CrossRef]
- Chan, C.T.; Blankestijn, P.J.; Dember, L.M.; Gallieni, M.; Harris, D.C.H.; Lok, C.E.; Mehrotra, R.; Stevens, P.E.; Wang, A.Y.; Cheung, M.; et al. Dialysis initiation, modality choice, access, and prescription: Conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2019, 96, 37–47. [Google Scholar] [CrossRef] [PubMed]
- KidneyWorks. KidneyWorks-A Job Retention Program for People with Chronic Kidney Disease (CKD). 2017. Available online: https://kidneyworks.org/ (accessed on 25 August 2021).
| Studies | Assessment Criteria 1 | Number of Yeses | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | ||
| Anees et al., 2018 [60] | Y | U | Y | Y | Y | N | Y | Y | 6 |
| Dimova et al., 2019 [73] | Y | Y | Y | Y | Y | N | Y | Y | 7 |
| Fleishman et al., 2020 [53] | Y | Y | U | Y | Y | Y | Y | Y | 7 |
| Gao et al., 2016 [27] | Y | U | Y | Y | Y | Y | Y | Y | 7 |
| Karasneh et al., 2020 [56] | Y | U | Y | Y | Y | Y | Y | Y | 7 |
| Ahlawat, Tiwari, and D’Cruz, 2018 [58] | Y | U | Y | Y | Y | Y | Y | Y | 7 |
| AlShahrani et al., 2018 [49] | Y | U | Y | Y | Y | N | Y | U | 5 |
| Anees et al., 2008 [59] | U | U | U | Y | Y | Y | U | Y | 4 |
| Araujo et al., 2012 [34] | U | Y | U | Y | Y | Y | Y | Y | 6 |
| Čengić and Resić, 2010 [74] | U | Y | U | Y | Y | N | N | Y | 4 |
| de Alencar et al., 2020 [35] | Y | Y | Y | Y | Y | Y | U | Y | 7 |
| de Brito et al., 2019 [36] | Y | U | Y | Y | Y | N | Y | Y | 6 |
| Drayer et al., 2006 [44] | U | U | Y | Y | Y | Y | Y | Y | 6 |
| Ganu et al., 2018 [75] | Y | U | N | Y | Y | N | Y | Y | 5 |
| Gerogianni et al., 2018 [76] | Y | Y | U | Y | Y | Y | Y | Y | 7 |
| Hu et al., 2015 [28] | Y | Y | Y | Y | Y | Y | Y | Y | 8 |
| Ibrahim and Salamony, 2008 [55] | U | Y | U | Y | Y | Y | Y | Y | 6 |
| Jeon, Kim, and Kim, 2020 [77] | U | Y | Y | Y | Y | N | Y | Y | 6 |
| Kutner et al., 2010 [47] | Y | U | U | Y | Y | Y | Y | Y | 6 |
| Lai et al., 2005 [68] | Y | Y | U | Y | Y | N | Y | Y | 6 |
| Li et al., 2011 [29] | Y | Y | Y | Y | Y | N | Y | Y | 7 |
| Park et al., 2010 [78] | Y | Y | N | Y | Y | Y | Y | Y | 7 |
| Rai, Rustagi, and Kohli, 2011 [62] | Y | Y | Y | Y | Y | N | Y | Y | 7 |
| Ramirez et al., 2011 [37] | U | Y | Y | Y | Y | Y | Y | Y | 7 |
| Rebollo Rubio et al., 2017 [70] | Y | Y | U | Y | Y | N | Y | Y | 6 |
| Saeed et al., 2012 [63] | Y | U | Y | Y | Y | Y | Y | Y | 7 |
| Sezer et al., 2013 [42] | Y | Y | U | Y | Y | N | Y | Y | 6 |
| Sousa et al., 2019 [79] | Y | U | U | Y | Y | N | Y | Y | 5 |
| Tezel, Karabulutlu, and Şahin, 2011 [43] | Y | Y | Y | Y | Y | N | Y | Y | 7 |
| Trbojević-Stanković et al., 2014 [80] | Y | Y | U | Y | Y | N | Y | Y | 6 |
| Turkistani et al., 2014 [57] | Y | Y | U | Y | Y | Y | Y | Y | 7 |
| Ye et al., 2008 [31] | Y | Y | U | Y | Y | Y | Y | Y | 7 |
| Yoong et al., 2017 [81] | Y | Y | Y | Y | Y | Y | Y | Y | 8 |
| Mathews and Methew, 2017 [61] | U | U | Y | Y | Y | N | Y | Y | 5 |
| Bai et al., 2015 [82] | Y | Y | U | Y | Y | Y | Y | Y | 7 |
| Biniaz et al., 2013 [50] | Y | Y | U | Y | Y | N | Y | U | 5 |
| Jhamb et al., 2011 [46] | Y | U | U | Y | Y | Y | Y | Y | 6 |
| Karakan, Sezer, and Odemir, 2011 [40] | Y | U | Y | Y | Y | Y | Y | Y | 7 |
| Liu, 2006 [83] | Y | U | U | Y | Y | Y | Y | Y | 6 |
| Mollaoglu, 2009 [41] | Y | Y | U | Y | Y | Y | Y | Y | 7 |
| Wang et al., 2016 [30] | Y | Y | U | Y | Y | Y | Y | Y | 7 |
| Zuo et al., 2018 [33] | Y | U | Y | Y | Y | Y | Y | Y | 7 |
| Gatmiri et al., 2018 [54] | Y | Y | Y | Y | Y | N | Y | Y | 7 |
| Saglimbene et al., 2017 [65] | Y | Y | U | Y | Y | Y | Y | Y | 7 |
| Strippoli, 2012 [66] | Y | Y | U | Y | Y | Y | Y | Y | 7 |
| Einollahi et al., 2015 [51] | Y | Y | U | Y | Y | Y | Y | Y | 7 |
| Zubair and Butt, 2017 [64] | Y | Y | U | Y | Y | Y | Y | Y | 7 |
| Fleishman, Dreiher, and Shvartzman, 2018 [52] | Y | Y | U | Y | Y | Y | Y | Y | 7 |
| Zhang et al., 2013 [32] | Y | Y | U | Y | Y | N | Y | Y | 6 |
| Ersoy and Akyar, 2019 [39] | Y | Y | U | Y | Y | N | Y | Y | 6 |
| Number of studies with yes | 35 | 31 | 15 | 42 | 42 | 25 | 40 | 41 | |
| Studies | Assessment Criteria 1 | Number of Yeses | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||
| Ng et al., 2020 [69] | Y | Y | Y | U | N | Y | Y | Y | U | Y | 7 |
| Cheng, Ho, and Hung, 2018 [71] | N | N | N | U | U | Y | Y | Y | N | Y | 4 |
| Ng et al., 2015 [72] | Y | Y | Y | Y | U | Y | Y | Y | U | Y | 8 |
| Song et al., 2016 [48] | Y | N | Y | U | N | Y | Y | N | U | Y | 5 |
| Sugisawa et al., 2016 [67] | N | N | N | N | N | Y | Y | Y | Y | Y | 5 |
| Jhamb et al., 2009 [45] | Y | Y | Y | U | U | Y | U | Y | U | Y | 6 |
| Sesso, Rodrigues-Neto, and Ferraz, 2003 [38] | Y | Y | Y | U | U | Y | Y | Y | U | Y | 7 |
| Number of studies with yes | 5 | 4 | 5 | 1 | 0 | 7 | 6 | 6 | 1 | 7 | |
| Studies | Income Level | Employment Status | Source of Healthcare Funding | Financial Status |
|---|---|---|---|---|
| Anees et al., 2018 [60] | Specific ranges (period not specified) | Multiple choices | Sources of funding: Multiple choice | |
| Dimova et al., 2019 [73] | Multiple choices | |||
| Fleishman et al., 2020 [53] | Below/above average | Multiple choices | ||
| Gao et al., 2016 [27] | Specific ranges | |||
| Karasneh et al., 2020 [56] | Yes/no | Insurance: Yes/no | ||
| Ng et al., 2020 [69] | Specific ranges | Multiple choices | ||
| Ahlawat, Tiwari, and D’Cruz, 2018 [58] | Specific ranges (currency not specified) | Multiple choices | Sources of funding: Multiple choice | Modified Kuppusamy Scale |
| AlShahrani et al., 2018 [49] | Specific ranges | Yes/no | ||
| Anees et al., 2008 [59] | Details not provided | |||
| Araujo et al., 2012 [34] | Yes/no | |||
| Čengić and Resić, 2010 [74] | Yes/no | |||
| Cheng, Ho, and Hung, 2018 [71] | Specific ranges | Yes/no | ||
| de Alencar et al., 2020 [35] | Minimum monthly salary | |||
| de Brito et al., 2019 [36] | Sources of income | Yes/no | ||
| Drayer et al., 2006 [44] | Kidney Disease Quality of Life—Short Form | |||
| Ganu et al., 2018 [75] | Details not provided | Multiple choices | ||
| Gerogianni et al., 2018 [76] | Multiple choices | Perceived levels | ||
| Hu et al., 2015 [28] | Specific ranges | |||
| Ibrahim and Salamony, 2008 [55] | Dichotomized responses | |||
| Jeon, Kim, and Kim, 2020 [77] | Specific ranges | Multiple choices | ||
| Kutner et al., 2010 [47] | Dichotomized responses | Employer group health insurance, disability income: Yes/no | ||
| Lai et al., 2005 [68] | Multiple choices | |||
| Li et al., 2011 [29] | Amount of annual income | Dichotomized responses | Reimbursement: Yes/no | |
| Ng et al., 2015 [72] | Specific ranges (period not specified) | Dichotomized responses | ||
| Park et al., 2010 [78] | Perceived levels | |||
| Rai, Rustagi, and Kohli, 2011 [62] | Specific ranges | Yes/no | ||
| Ramirez et al., 2011 [37] | Amount of monthly income | |||
| Rebollo Rubio et al., 2017 [70] | Multiple choices | |||
| Saeed et al., 2012 [63] | Specific ranges | Yes/no | ||
| Sezer et al., 2013 [42] | Perceived levels | Yes/no | ||
| Song et al., 2016 [48] | Specific ranges | Difficulty in paying for basic needs | ||
| Sousa et al., 2019 [79] | Dichotomized responses | |||
| Sugisawa et al., 2016 [67] | Quartiles of annual income | |||
| Tezel, Karabulutlu, and Şahin, 2011 [43] | Income-expenditure balance | Yes/no | ||
| Trbojević-Stanković et al., 2014 [80] | Yes/no | |||
| Turkistani et al., 2014 [57] | Multiple choices | Financial problems: Yes/no | ||
| Ye et al., 2008 [31] | Job and Family Crisis Subscale | |||
| Yoong et al., 2017 [81] | Specific ranges | Multiple choices | ||
| Mathews and Methew, 2017 [61] | Specific ranges | Multiple choices | ||
| Bai et al., 2015 [82] | Yes/no | |||
| Biniaz et al., 2013 [50] | Perceived levels | Details not reported | ||
| Jhamb et al., 2009 [45] | Yes/no | |||
| Jhamb et al., 2011 [46] | Yes/no | |||
| Karakan, Sezer, and Odemir, 2011 [40] | Specific ranges (period not specified) | Multiple choices | ||
| Liu, 2006 [83] | Yes/no | |||
| Mollaoglu, 2009 [41] | Yes/no | |||
| Sesso, Rodrigues-Neto, and Ferraz, 2003 [38] | Multiple choices | Brazilian classification of socioeconomic status | ||
| Wang et al., 2016 [30] | Yes/no | |||
| Zuo et al., 2018 [33] | Medical expenses: Multiple choices | |||
| Gatmiri et al., 2018 [54] | Specific ranges | Dichotomized responses | ||
| Saglimbene et al., 2017 [65] | Multiple choices | |||
| Strippoli, 2012 [66] | Multiple choices | |||
| Einollahi et al., 2015 [51] | Multiple choices | |||
| Zubair and Butt, 2017 [64] | Income-expenditure balance | Yes/no | ||
| Fleishman, Dreiher, and Shvartzman, 2018 [52] | Below/above average | Yes/no | ||
| Zhang et al., 2013 [32] | Yes/no | Insurance: Yes/no | ||
| Ersoy and Akyar, 2019 [39] | Yes/no |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ng, M.S.N.; Chan, D.N.S.; Cheng, Q.; Miaskowski, C.; So, W.K.W. Association between Financial Hardship and Symptom Burden in Patients Receiving Maintenance Dialysis: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 9541. https://doi.org/10.3390/ijerph18189541
Ng MSN, Chan DNS, Cheng Q, Miaskowski C, So WKW. Association between Financial Hardship and Symptom Burden in Patients Receiving Maintenance Dialysis: A Systematic Review. International Journal of Environmental Research and Public Health. 2021; 18(18):9541. https://doi.org/10.3390/ijerph18189541
Chicago/Turabian StyleNg, Marques Shek Nam, Dorothy Ngo Sheung Chan, Qinqin Cheng, Christine Miaskowski, and Winnie Kwok Wei So. 2021. "Association between Financial Hardship and Symptom Burden in Patients Receiving Maintenance Dialysis: A Systematic Review" International Journal of Environmental Research and Public Health 18, no. 18: 9541. https://doi.org/10.3390/ijerph18189541
APA StyleNg, M. S. N., Chan, D. N. S., Cheng, Q., Miaskowski, C., & So, W. K. W. (2021). Association between Financial Hardship and Symptom Burden in Patients Receiving Maintenance Dialysis: A Systematic Review. International Journal of Environmental Research and Public Health, 18(18), 9541. https://doi.org/10.3390/ijerph18189541






