Permanent Supportive Housing Design Characteristics Associated with the Mental Health of Formerly Homeless Adults in the U.S. and Canada: An Integrative Review
Abstract
:1. Introduction
2. Background
2.1. Chronic Homelessness in the U.S. and Canada
2.2. Homelessness and Mental Health
2.3. Permanent Supportive Housing (PSH) and Service Models
2.4. Architecture, Design, the Built Environment, and Mental Health
3. Methods
3.1. Review Aims and Design
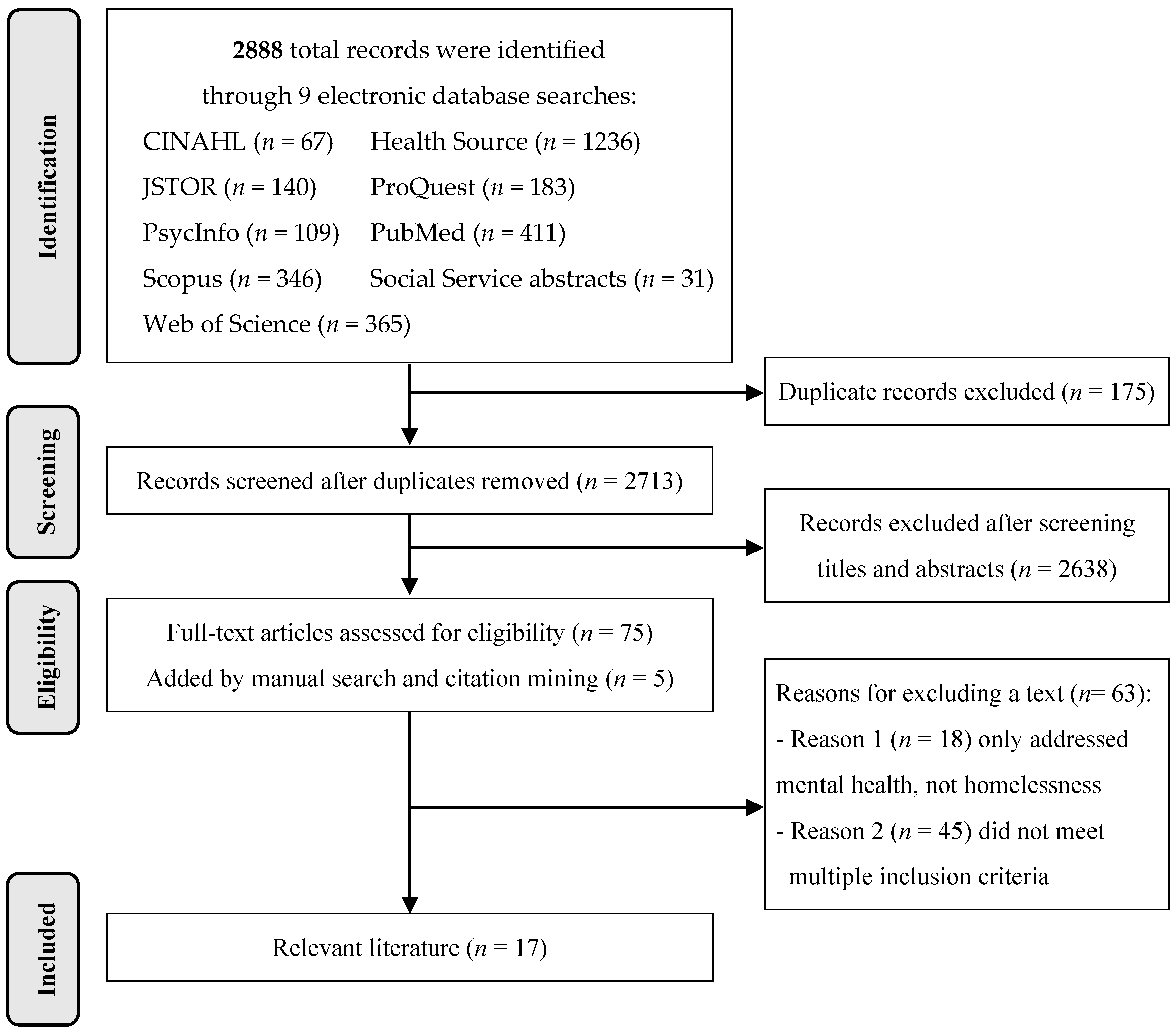
3.2. Literature Search Strategy and Inclusion Criteria
3.3. Literature Evaluation and Analysis
4. Results
4.1. Overview of the Included Literature
4.1.1. Research Design, Participants, and Rigor
4.1.2. Housing Type, Service Model, and Spatial Scale
4.1.3. Built Environment (BE) Relevance
4.1.4. Built Environment Findings, Properties, Place Attributes, and Integrative Domains
4.2. A Home Is More Than Housing
4.2.1. Sense of Home and Ontological Security
4.2.2. Safe Haven
4.2.3. Trauma Sensitivity, Trauma-Informed Care, and Trauma-Informed Design
4.3. Dwelling as a Vessel for Autonomous Daily Life
4.3.1. Having One’s Own Space, Single Occupancy, and an Apartment versus a Room
4.3.2. Preferences for Not Sharing a Bathroom
4.3.3. Safety and Security
4.3.4. Housing (and Location) Quality
4.3.5. Access to Storage, Facilities, and Nearby Amenities
4.4. Shared Common Space and Sociality within Single-Site PSH
4.4.1. Setting Facilitates Community
4.4.2. Promising and Contested Shared Common Spaces
4.4.3. Sociality and Trauma Sensitivity
4.4.4. Sociality by Design
5. Discussion
5.1. Interpretation and Implications of Findings
5.2. Strengths and Limitations
5.3. Directions for Future PSH Research
5.3.1. Increasing the Quantity and Quality of Research
5.3.2. Topics for Future Research
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Extracted Data | Categories and Definitions |
|---|---|
| Housing type (Table 3) | Permanent supportive housing (PSH) provides affordable, safe, and stable housing to people experiencing homelessness, mental and substance use disorders, and/or disability (see Background). |
| Service model (Table 3) | Housing First (HF) offers immediate housing and supportive services to individuals regardless of substance use and psychiatric treatment status; individuals are encouraged to define their own recovery-oriented goals [1,24]. Treatment First (TF), also referred to as Sober Living, Sober Living Housing, and Treatment as Usual, offers temporary housing to individuals experiencing homelessness, mental illness, and/or substance use issues with the requirement that they receive treatment and progress through a hierarchy of housing options based on “housing readiness” [1]. |
| Site approach [1] (Table 3) | Single site (SS) refers to one dedicated site (through new purpose-built construction, purchase of an existing building, or a master lease of an existing building) that primarily serves formerly homeless individuals with service needs. Dwelling units can be located within the same building, block, or neighborhood, and supportive services are usually available on site. Dwelling units can be independent apartments, shared independent apartments, shared rooms, or SROs with shared bathrooms kitchens. Scattered site (Scat) refers to private market apartments or general affordable housing dispersed throughout the community and leased by residents who are no longer experiencing homelessness via rental subsidies. Supportive staff may visit dwellings or provide services off-site. |
| Dwelling unit type (Table 3 and Table S1a,b) | Independent apartments: A dwelling unit with a lockable entry door, full bathroom, kitchen with refrigeration and cooking capability, and living/sleeping areas (e.g., a studio/one-bedroom apartment). Shared independent apartment: An independent apartment that is shared by two or more individuals. Congregate housing: Clustered arrangements of individual sleeping rooms with shared bathroom and kitchen facilities for each cluster of several residents. Rooms can be shared or single-occupancy. SRO (single-room occupancy): A single-occupancy dwelling unit with a bed that may or may not have a sink or small refrigerator. An SRO usually does not have its own bathroom or cooking facilities; instead, common bathrooms and cooking areas are shared. |
| Spatial scales (Table 3 and Table S4) | Room scale: Interior spaces that were divided into two subscales. Dwelling units referred to individual or shared rooms and apartments where residents lived. Shared common spaces referred to areas such as community rooms, kitchens, media rooms, laundry facilities, and outdoor spaces. Building scale: The building scale included factors such as the overall floor plan layout, adjacencies and arrangements of spaces, and the number of units. Location scale: Factors related to PSH location including access to transportation, amenities, and services; condition; and safety. |
| Built environment properties [68] (Table S2) | Ambient properties: Environmental conditions relating to the senses, also often included in measures of indoor environmental quality, such as lighting, sound, odor, temperature, humidity and ventilation. Physical properties: Built or natural elements that create and are contained within space such as the structure and enclosure (floors, walls, roof, windows), environmental control systems (heating and cooling, plumbing, electric, security), furnishings, fixtures, equipment, materials, and finishes. This paper included single and aggregated measures of quality (housing, environmental, and physical) and condition in this category. Spatial properties: Quantifiable spatial characteristics within and between physical spaces such as size, shape, proportion, volume, spatial and social densities, adjacency, proximity, layout, and arrangement. |
| Place Attribute | Definition | Reference |
|---|---|---|
| Safety and security | A state in which hazards and environmental conditions leading to physical, psychological, and material harm are controlled in order to preserve individual and group well-being. Security is the process and equipment that protects safety and well-being. Alternate definitions of security referring to maintaining consistent possession of personal items and housing were not coded as place attributes. | [109] |
| Control | The extent to which an environment facilitates personalization and territorial claims to a space, as well as the ability to alter one’s physical environment or regulate exposure to surroundings. | [68,69] |
| Choice | The provision of options in the physical environment, such as the ability to select a space or pathway (spatial choice), that leads to positive outcomes. | [110] |
| Privacy | The process of regulating the flow of visual and auditory information to and from others. When regulatory processes (e.g., territoriality, personal space) fail, social isolation and withdrawal can occur. Social isolation is the absence of positive social relationships resulting from restriction of contact with most or all other people (and/or activity, services, programs, stimulation) and is imposed by others. Social withdrawal is the restriction of contact with most or all other people (and/or activity, services, programs, stimulation) and is self-imposed due to, for example, over-stimulation or fear of harm (e.g., violence, substance abuse influences). | [68,94,95,111] |
| Territoriality | A boundary-regulation mechanism used to achieve desired levels of privacy that involves personalization or marking of a place or object and communicating that the place or object is “owned” by a person or group. | [94] |
| Sociality | The degree to which an environment facilitates or inhibits social interaction among people. | [68] |
| Sense of community | The feelings of belonging or affiliation to a group, that individual members matter to each other and the group, and that members’ needs will be met via commitment to that group. | [112,113] |
| Sense of “home” | A place for refuge, protection, security, safety, and centering described by comfort, privacy, familiarity, multiple layers of meaning, and a sense of self-expression, identity, responsibility, ownership, and being “at one” within the setting; the absence of mistreatment, alienation, and discomfort. | [70,85] |
| Comfort | The extent to which an environment provides both sensory and mobility fit and facilitates task performance. | [68] |
| Legibility | The ease with which people can conceptualize key spatial relationships within an environment. | [68] |
| Wayfinding | How people orient themselves and navigate to destinations in spaces within rooms, buildings, and cities. | [68] |
| Accessibility | The ease in locomotion through and use of an environment or space by users of varying abilities; addressed by ADA, universal, inclusive, and barrier-free design. | [68] |
| Adaptability | The ease with which an environment or space and its components can be reorganized to accommodate different patterns of use. | [68] |
| Sensory stimulation | The quality and quantity of information in a setting or object that impinges upon human users as experienced by the various senses. | [68,69] |
| Restoration | An environment’s ability to provide relief and recovery from mental fatigue often resulting from overstimulation and stress. | [102] |
| Crowding | The psychological response to high density based on perceptions of spatial restriction due to too little space (spatial density) or too many people present in a space (social density). | [114] |
| Meaning | The extent to which an environment holds individual or collective significance for people (e.g., attachment, challenge, beauty). | [68] |
Appendix B
| Citation | Housing Quality Measure (Data Collection Methods) | Subscales (# items) | Measure Reference | Outcomes Related to Mental Health |
|---|---|---|---|---|
| Adair et al., 2016 [38] | Observer-Rated Housing Quality Scale (Observations, interview questions, publicly available data) Perceived Housing Quality Scale (Participant-rated Likert scales) | Dwelling unit (18) Building (7) Neighborhood (9) Comfort, Safety, Privacy, Spaciousness, Overall Quality, Proximity (24) | Adair, 2014 [115] Tsemberis et al., 2003 [116] Toro et al., 1997 [117] | Housing stability |
| Brown et al., 2015 [72] | Housing Environment Survey (Participant-rated Likert scales and 5 semi-open-ended questions) | Physical quality (11) Neigh. quality (9) Neigh. social climate (10) Neigh. safety (8) Neighbor relationships (7) Landlord relationship (6) Roommate relationship (6) * | Kloos and Shah, 2009 [118] | Housing satisfaction |
| Nelson et al., 2007 [74] | Housing Quality Assessment ** (Participants rated 4-point scales for their previous residence and residences at baseline and follow-up) | Comfort, Safety, Privacy, Spaciousness, Overall Quality (5) | Toro, 1997 [117] | Self-reported quality of life, adaptation to community living |
| Tsai 2010 [75] | Housing Environment Survey-Physical Quality Scale (Participant-rated Likert scale) | Physical Quality (14) | Wright and Kloos, 2007 [119] | Housing satisfaction, residential satisfaction, social support |
| SAMSHA Housing Satisfaction Scale (Participant-rated Likert scales) | Choice, Safety, Privacy, Proximity (19) | Tsemberis et al., 2003 [116] | ||
| Tsai 2012 [76] | SAMSHA Housing Satisfaction Scale (Participant-rated Likert scales) | Choice, Safety, Privacy, Proximity (19) | Tsemberis et al., 2003 [116] | Housing satisfaction, self-reported quality of life, mental health, social support, psychological distress |
References
- National Academies of Sciences, Engineering, and Medicine. Permanent Supportive Housing: Evaluating the Evidence for Improving Health Outcomes among People Experiencing Chronic Homelessness; National Academy of Sciences: Washington, DC, USA, 2018. [Google Scholar]
- Woodhall-Melnik, J.R.; Dunn, J.R. A systematic review of outcomes associated with participation in Housing First programs. Hous. Stud. 2016, 31, 287–304. [Google Scholar] [CrossRef]
- Henry, M.; de Sousa, T.; Roddey, C.; Gayen, S.; Bednar, T.J.; Associates, A. The 2020 Annual Homeless Assessment Report (AHAR) to Congress, Part 1: Point-in-Time Estimates of Homelessness; U.S. Department of Housing and Urban Development: Washington, DC, USA, 2020. [Google Scholar]
- Gaetz, S.; Dej, E.; Richter, T.; Redman, M. The State of Homelessness in Canada 2016 COH Research Paper #12; Canadian Observatory on Homelessness Press: Toronto, ON, Canada, 2016. [Google Scholar]
- Bebout, R.R. Trauma-informed approaches to housing. New Dir. Ment. Health Serv. 2001, 2001, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Evans, G.W.; Wells, N.M.; Chan, H.-Y.E.; Saltzman, H. Housing quality and mental health. J. Consul Clin. Psychol. 2000, 68, 526–530. [Google Scholar] [CrossRef]
- Fazel, S.; Khosla, V.; Doll, H.; Geddes, J. The Prevalence of Mental Disorders among the Homeless in Western Countries: Systematic Review and Meta-Regression Analysis. PLoS Med. 2008, 5, e225. [Google Scholar] [CrossRef] [Green Version]
- Aljunaidy, M.M.; Adi, M.N. Architecture and Mental Disorders: A Systematic Study of Peer-Reviewed Literature. HERD Health Environ. Res. Des. J. 2021, 14, 320–330. [Google Scholar] [CrossRef]
- Padgett, D.K.; Stanhope, V.; Henwood, B.; Stefancic, A. Substance Use Outcomes Among Homeless Clients with Serious Mental Illness: Comparing Housing First with Treatment First Programs. Community Ment. Health J. 2010, 47, 227–232. [Google Scholar] [CrossRef] [Green Version]
- Caton, C.L.M.; Dominguez, B.; Schanzer, B.; Hasin, D.S.; Shrout, P.E.; Felix, A.; McQuistion, H.; Opler, L.A.; Hsu, E. Risk Factors for Long-Term Homelessness: Findings From a Longitudinal Study of First-Time Homeless Single Adults. Am. J. Public Health 2005, 95, 1753–1759. [Google Scholar] [CrossRef]
- Kertesz, S.G.; Larson, M.J.; Horton, N.J.; Winter, M.; Saitz, R.; Samet, J.H. Homeless chronicity and health-related quality of life trajectories among adults with addictions. Med. Care 2005, 43, 574–585. [Google Scholar] [CrossRef] [PubMed]
- Padgett, D.K.; Gulcur, L.; Tsemberis, S. Housing First Services for People Who Are Homeless with Co-Occurring Serious Mental Illness and Substance Abuse. Res. Soc. Work. Pract. 2006, 16, 74–83. [Google Scholar] [CrossRef]
- Henry, M.; Watt, R.; Rosenthal, L.; Shivji, A.; Associates, A. The 2016 Annual Homeless Assessment Report (AHAR) to Congress November 2016 PART 1: Point-in-Time Estimates of Homelessness; U.S. Department of Housing and Urban Development: Washington, DC, USA, 2016. [Google Scholar]
- Bloomfield, M.A. My Eyes Feel They Need to Cry: Stories from the Formerly Homeless; Michigan State University Press: Lansing, MI, USA, 2013. [Google Scholar]
- Wright, J.D. Address Unknown: The Homeless in America; Routledge: New York, NY, USA, 2009. [Google Scholar]
- Ly, A.; Latimer, E. Housing First impact on costs and associated cost offsets: A review of the literature. Canadian J. Psychiatry 2015, 60, 475–487. [Google Scholar] [CrossRef] [Green Version]
- Nelson, G.; MacLeod, T. The evolution of housing for people with serious mental illness. In Housing, Citizenship, and Communities for People with Serious Mental Illness: Theory, Research, Practice, and Policy Perspectives; Sylvestre, J., Nelson, G., Aubry, T., Eds.; Oxford University Press: Oxford, UK, 2017; pp. 3–22. [Google Scholar]
- Parsell, C.; Petersen, M.; Moutou, O. Single-site Supportive Housing: Tenant Perspectives. Hous. Stud. 2015, 30, 1189–1209. [Google Scholar] [CrossRef]
- Rog, D.J.; Marshall, T.; Dougherty, R.H.; George, P.; Daniels, A.S.; Ghose, S.S.; Delphin-Rittmon, M.E. Permanent Supportive Housing: Assessing the Evidence. Psychiatr. Serv. 2014, 65, 287–294. [Google Scholar] [CrossRef]
- Gubits, D.; Shinn, M.; Wood, M.; Brown, S.R.; Dastrup, S.R.; Bell, S.H. What Interventions Work Best for Families Who Experience Homelessness? Impact Estimates from the Family Options Study. J. Policy Anal. Manag. 2018, 37, 835–866. [Google Scholar] [CrossRef]
- Tsemberis, S.; Eisenberg, R.F. Pathways to Housing: Supported Housing for Street-Dwelling Homeless Individuals with Psychiatric Disabilities. Psychiatr. Serv. 2000, 51, 487–493. [Google Scholar] [CrossRef] [PubMed]
- Parsell, C.; Moutou, O.; Lucio, E.; Parkinson, S. Supportive housing to address homelessness. In AHURI Final Report No. 240; Australian Housing and Urban Research Institute: Melbourne, Australia, 2015; pp. 1–121. [Google Scholar]
- Tsemberis, S. Housing First: Basic tenets of the definition across cultures. Eur. J. Homelessness 2012, 6, 169–173. [Google Scholar]
- U.S. Interagency Commission on Homelessness. Investing in the End of Homelessness: The President’s 2017 Budget, Fact Sheet; U.S. Interagency Commission on Homelessness: Washington, DC, USA, 2017. [Google Scholar]
- Ridgway, P.; Zipple, A.M. The paradigm shift in residential services: From the linear continuum to supported housing approaches. Psychosoc. Rehabil. J. 1990, 13, 11–31. [Google Scholar] [CrossRef]
- Huffman, T. Built community: Architecture, community, and participation in a permanent supportive housing project. J. Soc. Distress Homeless 2017, 27, 44–52. [Google Scholar] [CrossRef]
- McLane, Y.; Pable, J. Architectural Design Characteristics, Uses, and Perceptions of Community Spaces in Permanent Supportive Housing. J. Inter. Des. 2020, 45, 33–52. [Google Scholar] [CrossRef]
- Connellan, K.; Gaardboe, M.; Riggs, D.; Due, C.; Reinschmidt, A.; Mustillo, L. Stressed Spaces: Mental Health and Architecture. HERD: Health Environ. Res. Des. J. 2013, 6, 127–168. [Google Scholar] [CrossRef]
- Sullivan, C.W.; Chang, C.Y. Mental health and the built environment. In Making Healthy Places; Dannenberg, A., Frumkin, H., Jackson, R., Eds.; Island Press: Washington, DC, USA, 2011; pp. 106–116. [Google Scholar]
- Friesinger, J.; Topor, A.; Bøe, T.D.; Larsen, I.B. Studies regarding supported housing and the built environment for people with mental health problems: A mixed-methods literature review. Health Place 2019, 57, 44–53. [Google Scholar] [CrossRef]
- Parr, H. Interpreting the ‘hidden social geographies’ of mental health: Ethnographies of inclusion and exclusion in semi-institutional places. Health Place 2000, 6, 225–237. [Google Scholar] [CrossRef]
- Halpern, D. Mental Health & the Built Environment: More Than Bricks & Mortar; Routledge: London, UK, 1995. [Google Scholar]
- Frumkin, H. Healthy places: Exploring the evidence. Am. J. Public Health 2003, 93, 1451–1456. [Google Scholar] [CrossRef]
- Evans, G.W.; Wells, N.M.; Moch, A. Housing and Mental Health: A Review of the Evidence and a Methodological and Conceptual Critique. J. Soc. Issues 2003, 59, 475–500. [Google Scholar] [CrossRef]
- Johansson, M.; Brunt, D. The Physical Environment of Purpose-Built and Non-Purpose-Built Supported Housing for Persons with Psychiatric Disabilities in Sweden. Issues Ment. Health Nurs. 2012, 33, 223–235. [Google Scholar] [CrossRef] [PubMed]
- Knight, K.R.; Lopez, A.M.; Comfort, M.; Shumway, M.; Cohen, J.; Riley, E.D. Single room occupancy (SRO) hotels as mental health risk environments among impoverished women: The intersection of policy, drug use, trauma, and urban space. Int. J. Drug Policy 2014, 25, 556–561. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pevalin, D.J.; Reeves, A.; Baker, E.; Bentley, R. The impact of persistent poor housing conditions on mental health: A longitudinal population-based study. Prev. Med. 2017, 105, 304–310. [Google Scholar] [CrossRef] [Green Version]
- Adair, C.E.; Kopp, B.; Distasio, J.; Hwang, S.W.; Lavoie, J.; Veldhuizen, S.; Voronka, J.; Kaufman, A.F.; Somers, J.M.; Leblanc, S.R.; et al. Housing Quality in a Randomized Controlled Trial of Housing First for Homeless Individuals with Mental Illness: Correlates and Associations with Outcomes. J. Hered. 2016, 93, 682–697. [Google Scholar] [CrossRef] [PubMed]
- Liddell, C.; Guiney, C. Living in a cold and damp home: Frameworks for understanding impacts on mental well-being. Public Health 2015, 129, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Rautio, N.; Filatova, S.; Lehtiniemi, H.; Miettunen, J. Living environment and its relationship to depressive mood: A systematic review. Int. J. Soc. Psychiatry 2018, 64, 92–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shah, S.N.; Fossa, A.; Steiner, A.; Kane, J.; Levy, J.I.; Adamkiewicz, G.; Bennett-Fripp, W.M.; Reid, M. Housing Quality and Mental Health: The Association between Pest Infestation and Depressive Symptoms among Public Housing Residents. J. Hered. 2018, 95, 691–702. [Google Scholar] [CrossRef]
- Lindberg, R.A.; Shenassa, E.D.; Acevedo-Garcia, D.; Popkin, S.J.; Villaveces, A.; Morley, R.L. Housing Interventions at the Neighborhood Level and Health. J. Public Health Manag. Pract. 2010, 16, S44–S52. [Google Scholar] [CrossRef]
- Sommer, R. Sociofugal Space. Am. J. Sociol. 1967, 72, 654–660. [Google Scholar] [CrossRef]
- Marcus, C.C. House as a Mirror of Self: Exploring the Deeper Meaning of Home; Conari Press: Berkeley, CA, USA, 1995. [Google Scholar]
- Baum, A.; Valins, S. Architecture and Social Behavior: Psychological Study of Social Density; Wiley: New York, NY, USA, 1977. [Google Scholar]
- Baum, A.; Valins, S. Architectural mediation of residential density and control: Crowding and the regulation of social contact. Adv. Exp. Soc. Psychol. 1979, 12, 131–175. [Google Scholar]
- Baum, A.; Gatchel, R. Cognitive mediation of environmental stress. In Cognition, Social Behavior, and the Environment; Erlbaum: Hillsdale, NJ, USA, 1981; pp. 513–533. [Google Scholar]
- Hillier, B.; Hanson, J. The Social Logic. of Space; Cambridge University Press: Cambridgeshire, UK, 1984. [Google Scholar]
- Festinger, L.; Schachter, S.; Back, K. Social Pressures in Informal Groups; a Study of Human Factors in Housing; Stanford University Press: Stanford, CA, USA, 1950. [Google Scholar]
- Wells, M.N.; Rollings, K.A. The natural environment in residential settings: Influences on human health and function. In The Oxford Handbook of Environmental and Conservation Psychology; Clayton, S., Ed.; Oxford University Press: Oxford, UK, 2012. [Google Scholar]
- Pable, J. Interior Design Homeless shelter design: A psychologically recuperative approach. J. Inter. Des. 2007, 32, 93–108. [Google Scholar] [CrossRef]
- Pable, J. The Homeless Shelter Family Experience: Examining the Influence of Physical Living Conditions on Perceptions of Internal Control, Crowding, Privacy, and Related Issues. J. Inter. Des. 2012, 37, 9–37. [Google Scholar] [CrossRef]
- Pable, J. Possessions in the homeless shelter experience: The built environment’s potential role in self-restoration. Interiors 2013, 4, 267–293. [Google Scholar] [CrossRef]
- Liddicoat, S.; Badcock, P.; Killackey, E. Principles for designing the built environment of mental health services. Lancet Psychiatry 2020, 7, 915–920. [Google Scholar] [CrossRef]
- Shepley, M.M.; Pasha, S. Design for Mental and Behavioral Health; Routledge: Abingdon, UK, 2017. [Google Scholar]
- Shepley, M.M.; Pasha, S. Design Research and Behavioral Health Facilities; The Center for Health Design: Concord, CA, USA, 2013; pp. 1–81. [Google Scholar]
- Lundqvist, L.-O.; Rask, M.; Brunt, D.; Ivarsson, A.-B.; Schröder, A. Measuring quality in community based housing support—The QPC-H instrument. Int. J. Health Care Qual. Assur. 2016, 29, 267–275. [Google Scholar] [CrossRef]
- Marcheschi, E.; Laike, T.; Brunt, D.; Hansson, L.; Johansson, M. Quality of life and place attachment among people with severe mental illness. J. Environ. Psychol. 2015, 41, 145–154. [Google Scholar] [CrossRef] [Green Version]
- Marcheschi, E.; Johansson, M.; Laike, T.; Brunt, D. Housing design and people with severe mental illness: An observational approach to the investigation of supported housing facilities. Scand. J. Psychol. 2016, 57, 12–21. [Google Scholar] [CrossRef]
- Whittemore, R.; Knafl, K. The integrative review: Updated methodology. J. Adv. Nurs. 2005, 52, 546–553. [Google Scholar] [CrossRef]
- Miles, B.M.; Huberman, A.M. Qualitative Data Analysis; Sage Publications: Thousand Oaks, CA, USA, 1994. [Google Scholar]
- Bollo, C.; Donofrio, A. From principles to patterns: Trauma-informed design for Permanent Supportive Housing. In Housing and Society; under review.
- Goering, P.N.; Streiner, D.; Adair, C.; Aubry, T.; Barker, J.; Distasio, J.; Hwang, S.W.; Komaroff, J.; Latimer, E.; Somers, J.; et al. The At Home/Chez Soi trial protocol: A pragmatic, multi-site, randomised controlled trial of a Housing First intervention for homeless individuals with mental illness in five Canadian cities. BMJ Open 2011, 1, e000323. [Google Scholar] [CrossRef] [Green Version]
- Clark, C.; Myron, R.; Stansfeld, S.; Candy, B. A systematic review of the evidence on the effect of the built and physical environment on mental health. J. Public Ment. Health 2007, 6, 14–27. [Google Scholar] [CrossRef]
- Greenwood, R.M.; Manning, R.M.; O’Shaughnessy, B.R.; Vargas-Moniz, M.J.; Loubière, S.; Spinnewijn, F.; Lenzi, M.; Wolf, J.R.; Bokszczanin, A.; Bernad, R.; et al. Homeless Adults’ Recovery Experiences in Housing First and Traditional Services Programs in Seven European Countries. Am. J. Community Psychol. 2020, 65, 353–368. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Garrard, J. Health Sciences Literature Review Made Easy: The Matrix Method, 5th ed.; Jones & Bartlett Learning: Burlington, MA, USA, 2016. [Google Scholar]
- Weisman, G. The place of people in architectural design. In Architectural Design Portable Handbook: A Guide to Excellent Practices; McGraw-Hill: New York, NY, USA, 2001; pp. 158–170. [Google Scholar]
- Evans, G.W.; McCoy, J.M. When buildings don’t work: The role of architecture in human health. J. Environ. Psychol. 1998, 18, 85–94. [Google Scholar] [CrossRef] [Green Version]
- Rivlin, L.G.; Moore, J. Home-Making: Supports and Barriers to the Process of Home. J. Soc. Distress Homeless 2001, 10, 323–336. [Google Scholar] [CrossRef]
- Wittman, F.D.; Polcin, U.L.; Sheridan, D. The architecture of recovery: Two kinds of housing assistance for chronic homeless persons with substance use disorders. Drugs Alcohol Today 2017, 17, 157–167. [Google Scholar] [CrossRef] [Green Version]
- Brown, M.; Malone, D.; Jordan, N. Tenant Satisfaction with a Single-Site Housing First Program. J. Soc. Serv. Res. 2015, 41, 1–10. [Google Scholar] [CrossRef]
- Hsu, H.-T.; Simon, J.D.; Henwood, B.F.; Wenzel, S.L.; Couture, S.L.W. Location, Location, Location: Perceptions of Safety and Security Among Formerly Homeless Persons Transitioned to Permanent Supportive Housing. J. Soc. Soc. Work. Res. 2016, 7, 65–88. [Google Scholar] [CrossRef]
- Nelson, G.; Sylvestre, J.; Aubry, T.; George, L.; Trainor, J. Housing Choice and Control, Housing Quality, and Control over Professional Support as Contributors to the Subjective Quality of Life and Community Adaptation of People with Severe Mental Illness. Adm. Policy Ment. Health Ment. Health Serv. Res. 2006, 34, 89–100. [Google Scholar] [CrossRef] [PubMed]
- Tsai, J.; Bond, G.R.; Davis, K.E. Housing Preferences Among Adults with Dual Diagnoses in Different Stages of Treatment and Housing Types. Am. J. Psychiatr. Rehabil. 2010, 13, 258–275. [Google Scholar] [CrossRef] [Green Version]
- Tsai, J.; Mares, A.S.; Rosenheck, R.A. Housing Satisfaction Among Chronically Homeless Adults: Identification of its Major Domains, Changes Over Time, and Relation to Subjective Well-being and Functional Outcomes. Community Ment. Health J. 2011, 48, 255–263. [Google Scholar] [CrossRef]
- Anucha, U. We are not just rent receipts: Housing, neighbourhood, and community re-imagined by formerly homeless people. Rev. Can. Serv. Soc. 2005, 22, 189–209. [Google Scholar]
- Burns, V.F.; LeDuc, J.D.-; St-Denis, N.; Walsh, C.A. Finding home after homelessness: Older men’s experiences in single-site permanent supportive housing. Hous. Stud. 2019, 35, 290–309. [Google Scholar] [CrossRef]
- Chan, D.V. Safe Spaces, Agency, and Connections to “Regular Stuff”: What Makes Permanent Supportive Housing Feel Like “Home”. Rehabil. Couns. Bull. 2018, 63, 102–114. [Google Scholar] [CrossRef]
- Henwood, B.F.; Lahey, J.; Harris, T.; Rhoades, H.; Wenzel, S.L. Understanding Risk Environments in Permanent Supportive Housing for Formerly Homeless Adults. Qual. Health Res. 2018, 28, 2011–2019. [Google Scholar] [CrossRef]
- Henwood, B.F.; Redline, B.; Semborski, S.; Rhoades, H.; Rice, E.; Wenzel, S.L. What’s next? A theory on identity preservation for young adults in supportive housing. Cityscape 2018, 20, 87–100. [Google Scholar]
- Padgett, D.K. There’s no place like (a) home: Ontological security among persons with serious mental illness in the United States. Soc. Sci. Med. 2007, 64, 1925–1936. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adame, A.L.; Perry, C.; Pierce, E. Community and Housing First: A qualitative analysis of USA residents’ perspectives. Health Soc. Care Comm. 2020, 28, 1292–1300. [Google Scholar] [CrossRef] [PubMed]
- Rykwert, J. House and home. Soc. Res. 1991, 58, 51–62. Available online: https://www.jstor.org/stable/40970630 (accessed on 18 March 2021).
- Rowles, G.D. Housing for older adults. In Environmental Psychology and Human Well-Being: Effects of Built and Natural Settings; Devlin, A.S., Ed.; Academic Press: Cambridge, MA, USA, 2018; pp. 77–106. [Google Scholar]
- Dupuis, A.; Thorns, D.C. Home, Home Ownership and the Search for Ontological Security. Sociol. Rev. 1998, 46, 24–47. [Google Scholar] [CrossRef]
- Wong, Y.I.; Hadley, T.R.; Culhane, D.P.; Poulin, S.R.; Davis, M.R. Predicting Staying in or Leaving Permanent Supportive Housing That Serves Homeless People with Serious Mental Illness; U.S. Department of Housing and Urban Development, Office of Policy Development and Research: Washington, DC, USA, 2006. [Google Scholar]
- Hetling, A.; Dunford, A.; Botein, H. Community in the Permanent Supportive Housing Model: Applications to Survivors of Intimate Partner Violence. Housing, Theory Soc. 2020, 37, 400–416. [Google Scholar] [CrossRef]
- Bridgman, R. Housing chronically homeless women: “Inside” a safe haven. Hous. Policy Debate 2002, 13, 51–81. [Google Scholar] [CrossRef]
- Hopper, E.K.; Bassuk, E.L.; Olivet, J. Shelter from the Storm: Trauma-Informed Care in Homelessness Services Settings. Open Health Serv. Policy J. 2010, 3, 80–100. [Google Scholar] [CrossRef]
- Fallot, D.R.; Harris, M. Trauma-informed approaches to systems of care. Trauma Psychol. Newsl. 2008, 3, 6–7. [Google Scholar]
- Farrell, J. The Committee on Temporary Shelter. Trauma-Informed Design: How the Physical Environment Supports Recovery from Homelessness. 2018. Available online: http://cotsonline.org/wp-content/uploads/2018/04/Trauma-Informed-Design.BOD_.pdf (accessed on 18 March 2021).
- Henwood, B.F.; Lahey, J.; Rhoades, H.; Winetrobe, H.; Wenzel, S.L. Examining the health status of homeless adults entering permanent supportive housing. J. Public Health 2017, 40, 415–418. [Google Scholar] [CrossRef] [Green Version]
- Altman, I. The Environment and Social Behavior: Privacy, Personal Space, Territory, Crowding; Brooks/Cole Publishing Company: Monterey, CA, USA, 1975. [Google Scholar]
- Cacioppo, T.J.; Cacioppo, S. Social relationships and health: The toxic effects of perceived social isolation. Soc. Personal. Psychol. Compass 2014, 8, 58–72. [Google Scholar] [CrossRef]
- Appleton, J. The Experience of Landscape; Wiley: London, UK, 1975. [Google Scholar]
- Evans, G.W.; Rhee, E.; Forbes, C.; Allen, K.M.; Lepore, S. The meaning and efficacy of social withdrawal as a strategy for coping with chronic residential crowding. J. Environ. Psychol. 2000, 20, 335–342. [Google Scholar] [CrossRef]
- Li, D.; Menotti, T.; Ding, Y.; Wells, N. Life Course Nature Exposure and Mental Health Outcomes: A Systematic Review and Future Directions. Int. J. Environ. Res. Public Health 2021, 18, 5146. [Google Scholar] [CrossRef]
- Devlin, A.S. Wayfinding in Healthcare Facilities: Contributions from Environmental Psychology. Behav. Sci. 2014, 4, 423–436. [Google Scholar] [CrossRef] [Green Version]
- The Center for Universal Design. The Principles of Universal Design; Version 2.0; North Carolina State University: Raleigh, NC, USA, 1997. [Google Scholar]
- Henwood, B.F.; Lahey, J.; Rhoades, H.; Pitts, D.B.; Pynoos, J.; Brown, R.T. Geriatric Conditions Among Formerly Homeless Older Adults Living in Permanent Supportive Housing. J. Gen. Intern. Med. 2019, 34, 802–803. [Google Scholar] [CrossRef] [Green Version]
- Kaplan, S.; Kaplan, R. Cognition and Environment: Functioning in an Uncertain World; Praeger: New York, NY, USA, 1989. [Google Scholar]
- Schweitzer, M.; Gilpin, L.; Frampton, S. Healing Spaces: Elements of Environmental Design That Make an Impact on Health. J. Altern. Complement. Med. 2004, 10, 71–83. [Google Scholar] [CrossRef]
- Abdelaal, M.S.; Soebarto, V. Biophilia and Salutogenesis as restorative design approaches in healthcare architecture. Arch. Sci. Rev. 2019, 62, 195–205. [Google Scholar] [CrossRef]
- Aboujaoude, E.; Salame, W.; Naim, L. Telemental health: A status update. World Psychiatry 2015, 14, 223–230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsai, J.; Rosenheck, R.A. Racial Differences Among Supported Housing Clients in Outcomes and Therapeutic Relationships. Psychiatr. Q. 2011, 83, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Omerov, P.; Craftman, Å.G.; Mattsson, E.; Klarare, A. Homeless persons’ experiences of health- and social care: A systematic integrative review. Health Soc. Care Community 2020, 28, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henwood, B.F.; Cabassa, L.J.; Craig, C.M.; Padgett, D.K. Permanent Supportive Housing: Addressing Homelessness and Health Disparities? Am. J. Public Health 2013, 103, S188–S192. [Google Scholar] [CrossRef]
- Maurice, P.; Lavoie, M.; Laflamme, L.; Svanström, L.; Romer, C.; Anderson, R. Safety and safety promotion: Definitions for operational developments. Inj. Control. Saf. Promot. 2001, 8, 237–240. [Google Scholar] [CrossRef]
- Gifford, R. Environmental Psychology: Principles and Practice; Allyn and Bacon Inc.: Boston, MA, USA, 1987. [Google Scholar]
- Wener, R.E. Can correctional environments be humane? A case for evidence and value-based design. In Environmental Psychology and Human Well-Being: Effects of Built and Natural Settings; Devlin, A.S., Ed.; Academic Press: Cambridge, MA, USA, 2018; pp. 281–312. [Google Scholar]
- McMillan, W.D.; Chavis, D.M. Sense of community: A definition and theory. J. Community Psychol. 1986, 14, 6–23. [Google Scholar] [CrossRef]
- Francis, J.; Giles-Corti, B.; Wood, L.; Knuiman, M. Creating sense of community: The role of public space. J. Environ. Psychol. 2012, 32, 401–409. [Google Scholar] [CrossRef]
- Rollings, K.A.; Evans, G.W. Design Moderators of Perceived Residential Crowding and Chronic Physiological Stress Among Children. Environ. Behav. 2019, 51, 590–621. [Google Scholar] [CrossRef]
- Adair, C.E.; Kopp, B.; Lavoie, J.; Distasio, J.; Hwang, S.W.; Watson, A.; Veldhuizen, S.; Chislett, K.; Voronka, J.; Ahmad, M.; et al. Development and Initial Validation of the Observer-Rated Housing Quality Scale (OHQS) in a Multisite Trial of Housing First. J. Hered. 2014, 91, 242–255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsemberis, S.; Rogers, E.S.; Rodis, E.; Dushuttle, P.; Skryha, V. Housing satisfaction for persons with psychiatric disabilities. J. Community Psychol. 2003, 31, 581–590. [Google Scholar] [CrossRef]
- Toro, P.A.; Rabideau, J.M.P.; Bellavia, C.W.; Daeschler, C.V.; Wall, D.D.; Thomas, D.M.; Smith, S.J. Evaluating an intervention for homeless persons: Results of a field experiment. J. Consul Clin. Psychol. 1997, 65, 476–484. [Google Scholar] [CrossRef]
- Kloos, B.; Shah, S. A Social Ecological Approach to Investigating Relationships Between Housing and Adaptive Functioning for Persons with Serious Mental Illness. Am. J. Community Psychol. 2009, 44, 316–326. [Google Scholar] [CrossRef] [PubMed]
- Wright, P.A.; Kloos, B. Housing environment and mental health outcomes: A levels of analysis perspective. J. Environ. Psychol. 2007, 27, 79–89. [Google Scholar] [CrossRef] [Green Version]

| Search Concepts | Search Terms 1 |
|---|---|
| Supportive(ed) Housing 2 | Housing, residential |
| Mental Health | Mental health, mental illness/es, mental disorder/s, mental well-being, psychological illness/es, behavioral health, psychiatric disabilities, loneliness, trauma, psychological health |
| Architecture/Design | Built environment, interior design, architecture, physical environment, environmental design, environment design, design attributes, design features, architectural, spatial characteristics, design characteristics, safety, security, surveillance, wayfinding, territoriality, crowding, privacy, housing quality, environment quality, environmental quality |
| Excluded | Children, older adults, later life, elderly, aged, disabled, older people, care facilities, board home, care home, nursing home, nursing homes, city, cities, urban, eating disorder, eating disorders, mental retardation, prison, prisons, jail, jails, HIV, AIDS, refugee, refugees, asylum, youth, adolescent, adolescents, workplace, workplaces, COVID-19 |
| a. Built Environment Relevance | b. Methodological Rigor Ratings [60] |
|---|---|
| Design driven (DD): Studies contained independent and/or dependent variables addressing built environment factors associated with design (e.g., size, location, adjacency); study aims included evaluating and/or informing architectural design. Built environment focused (BE): Studies included BE independent and/or dependent variables (e.g., housing quality), without aims to evaluate or inform architectural design. Inductive (IN): Qualitative studies that indirectly addressed built environment factors in research questions (e.g., aspects of “home”) and yielded findings or responses relevant to design. Mentions (ME): Qualitative studies that did not include the built environment in the research design, but findings (i.e., participant responses) frequently “mentioned” built environment factors consistent with studies in the other three relevance categories. | Quantitative: Rigor was rated on a three-point scale (high, medium, or low) based on research design (e.g., longitudinal or cross-sectional, control or comparison group), sampling technique (random,, purposeful, or convenience) and size, data collection methods and measures (e.g., single or multiple, self-reported and/or objective, tested or newly created) including reported psychometrics (e.g., reliability and validity), and analysis methods (advanced statistical analysis vs. descriptive statistics) and reported measures of effect size with results. Qualitative: Rigor was rated on a three-point scale (high, medium, or low) based on the research design (cross-sectional, repeated measures, or longitudinal), sampling technique (purposeful or convenience), data collection methods and measures (e.g., cited instrument, accuracy check), and coding and analysis techniques (e.g., iterative, multiple coders, cited method, end-stage validation). Mixed Methods: After rating the quantitative and qualitative components of mixed-methods studies according to the rigor definitions, an overall rigor rating was discussed by researchers based on whether the study was primarily quantitative or qualitative. Review: Rigor was assessed based on reported search processes and analyses procedures (neither were reported in the single review). |
| Citation Location | Purpose 1 | Research Design 2 STUDY TYPE (Research Design)
| Rigor | Housing 3
| Scale 4 Dwelling, Room, Building, Location | |||
|---|---|---|---|---|---|---|---|---|
| D | R | B | L | |||||
| Relevance: Design Driven (2) | ||||||||
| McLane et al., 2020 [27] U.S. (Tallahassee); UK (Southampton) | Recorded and explored socio-spatial and design factors, policies and programming, and resident perceptions of shared community gathering space location, design, and use in two PSH facilities with the aim of presenting new analysis methods and improving future shared spaces. | MIXED (Dual case study; CS)
| Medium QUAN-Low QUAL-Med |
| • | • | ||
| Wittman et al., 2017 [71] U.S. (review article) | Provided an overview of Housing First (HF) and Sober Living Housing (SLH) models and recommendations for practice based on an approach to architectural planning that emphasized the interaction between settings and operations on resident experiences. | REVIEW (not specified)
| Low |
| • | • | • | • |
| Relevance: BE Focus (8) | ||||||||
| Adair et al., 2016 [38] Canada (Moncton, Montreal, Toronto, Winnipeg, Vancouver) | Assessed housing quality in Housing First (HF) and Treatment as Usual (TAU) facilities, examined differences between participants in each group, and studied associations between housing quality and housing stability. | QUANTITATIVE (Quasi-Experimental, Longitudinal—2 yrs)
| High |
| • | • | • | |
| Brown et al., 2015 [72] U.S. (Seattle) | Explored perceptions of housing and neighborhood environments and associations with satisfaction (high/low desire to stay) among single-site Housing First residents via the Housing Environment Survey. | MIXED (2-group comparison, CS)
| Low QUAN-Med QUAL-Low |
| • | • | • | |
| Hsu et al., 2016 [73] U.S. (Los Angeles) | Examined perceptions of safety and security among residents living in and surrounding the Skid Row area of Los Angeles and how those perceptions correlated with objective measures of neighborhood environment. | MIXED (Explanatory sequential; CS)
| Low QUAN-Low QUAL-Med |
| • | • | • | |
| Huffman, 2018 [26] U.S. (Los Angeles) | Investigated the connection between PSH social spaces, participation, and community based on resident experiences in a housing organization on Skid Row in Los Angeles, California. | QUALITATIVE (Case study, CS)
| High |
| • | |||
| Knight et al., 2014 [36] U.S. (San Francisco) | Explored how SROs can operate as “mental health risk environments” in which macro-structural factors (housing policies shaping the built environment) interact with meso-level factors (social relations within SROs) and micro-level, behavioral coping strategies to affect women’s mental health. | QUALITATIVE (Longitudinal, Ethnography—4 yrs) #
| High |
| • | • | ||
| Nelson et al., 2007 [74] Canada (Toronto, Hamilton, Ottawa) | Examined whether consumer choice and control over housing, support, and housing quality contributed to self-reported quality of life and adaptation to community living among people with mental illness, and whether individual apartments provided more choice and control than group living arrangements. | QUANTITATIVE (Repeated measures, CS) *
| Med |
| • | • | ||
| Tsai et al., 2010 [75] U.S. (Chicago) | Examined whether housing preferences differed between substance abuse treatment stages, whether dual-diagnoses consumers who prefer certain housing types preferred certain characteristics, and whether consumers residing in different housing types reported differences in choice, social support, and housing satisfaction. | QUANTITATIVE (Group comparison, CS)
| Med |
| • | • | • | |
| Tsai et al., 2012 [76] U.S. (11 sites, locations not specified) | Identified primary domains of housing satisfaction (HS), tracked HS over time, and assessed relations between HS and subjective and functional outcomes. | QUANTITATIVE (Longitudinal: quarterly for 2 yrs)
| High |
| • | • | ||
| Relevance: Inductive (6) | ||||||||
| Anucha, 2005 [77] Canada (Toronto) | Explored the needs of the formerly homeless, from their perspective, and how housing, neighborhood, and community can meet their needs more effectively to avoid a return to homelessness. | QUALITATIVE (Exploratory, CS)
| Low |
| • | • | • | |
| Burns et al., 2020 [78] Canada (Montreal) | Explored everyday experiences of formerly homeless older men residing in single-site PSH based on the concepts of home and social exclusion. | QUALITATIVE (Const. grounded theory, CS)
| High |
| • | • | ||
| Chan, 2020 [79] U.S. (Boston, Cambridge) | Explored what makes supportive housing feel like “home” for individuals who were once homeless related to constructing new, non-homeless identities, social isolation, and community integration. | QUALITATIVE (Repeated measures, CS)
| Med |
| • | • | • | |
| Henwood et al., 2018a [80] U.S. (Los Angeles) | Considered how contextual factors generate or reduce risk for substance use among adults who recently moved into PSH. | QUALITATIVE (Case summary matrix, CS)
| Med |
| • | • | ||
| Henwood et al., 2018b [81] U.S. (Los Angeles) | Used ontological security (well-being rooted in a sense of constancy in the social and material environment) as a sensitizing framework to examine the perspectives and experiences of young adult PSH residents. | QUALITATIVE (Grounded theory, CS)
| Med |
| • | |||
| Padgett, 2007 [82] U.S. (New York City) | Explored how study participants who obtained independent housing experience, enact and describe having a “home” and to what extent their experiences reflect markers of ontological security. | QUALITATIVE (Grounded theory, CS)
| High |
| • | • | • | |
| Relevance: Mentions (1) | ||||||||
| Adame et al., 2020 [83] U.S. (Seattle) | Interviewed residents of a Housing First organization about their experiences of community and gathered suggestions for improving community building efforts. | QUALITATIVE (Exploratory, CS)
| Med |
| • | • | ||
| Table Notes and Abbreviations * = Psychometrics were reported for the quantitative measure(s) used to collect independent and/or dependent variables. # = Qualitative methods included procedures that addressed rigor in data collection, coding, and/or analysis. 1 = “Purpose” column: HF = Housing First; HQ = housing quality; PSH = permanent supportive housing; TF = Treatment First; SLH = Sober Living Housing; TAU = Treatment as Usual | 2 = “Research Design” column: MIXED= mixed methods; CS= cross-sectional 3 = “Housing” column: Type/Program: PSH= permanent supportive housing; HF = Housing First; TF = Treatment First; TAU = Treatment as Usual; SL = Sober Living Site approach: SS = single site; Scat = scattered site; Priv Mkt = private market Dwelling type: SRO = single-room occupancy; Cong = congregate housing; Apt = apartment; Ind = independent; Shrd = shared 4 = “Spatial Scale” column: D = dwelling unit; R = room (shared common area); B = building; L = location | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rollings, K.A.; Bollo, C.S. Permanent Supportive Housing Design Characteristics Associated with the Mental Health of Formerly Homeless Adults in the U.S. and Canada: An Integrative Review. Int. J. Environ. Res. Public Health 2021, 18, 9588. https://doi.org/10.3390/ijerph18189588
Rollings KA, Bollo CS. Permanent Supportive Housing Design Characteristics Associated with the Mental Health of Formerly Homeless Adults in the U.S. and Canada: An Integrative Review. International Journal of Environmental Research and Public Health. 2021; 18(18):9588. https://doi.org/10.3390/ijerph18189588
Chicago/Turabian StyleRollings, Kimberly A., and Christina S. Bollo. 2021. "Permanent Supportive Housing Design Characteristics Associated with the Mental Health of Formerly Homeless Adults in the U.S. and Canada: An Integrative Review" International Journal of Environmental Research and Public Health 18, no. 18: 9588. https://doi.org/10.3390/ijerph18189588






