Hypertension in Children with Obstructive Sleep Apnea Syndrome—Age, Weight Status, and Disease Severity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data Collection
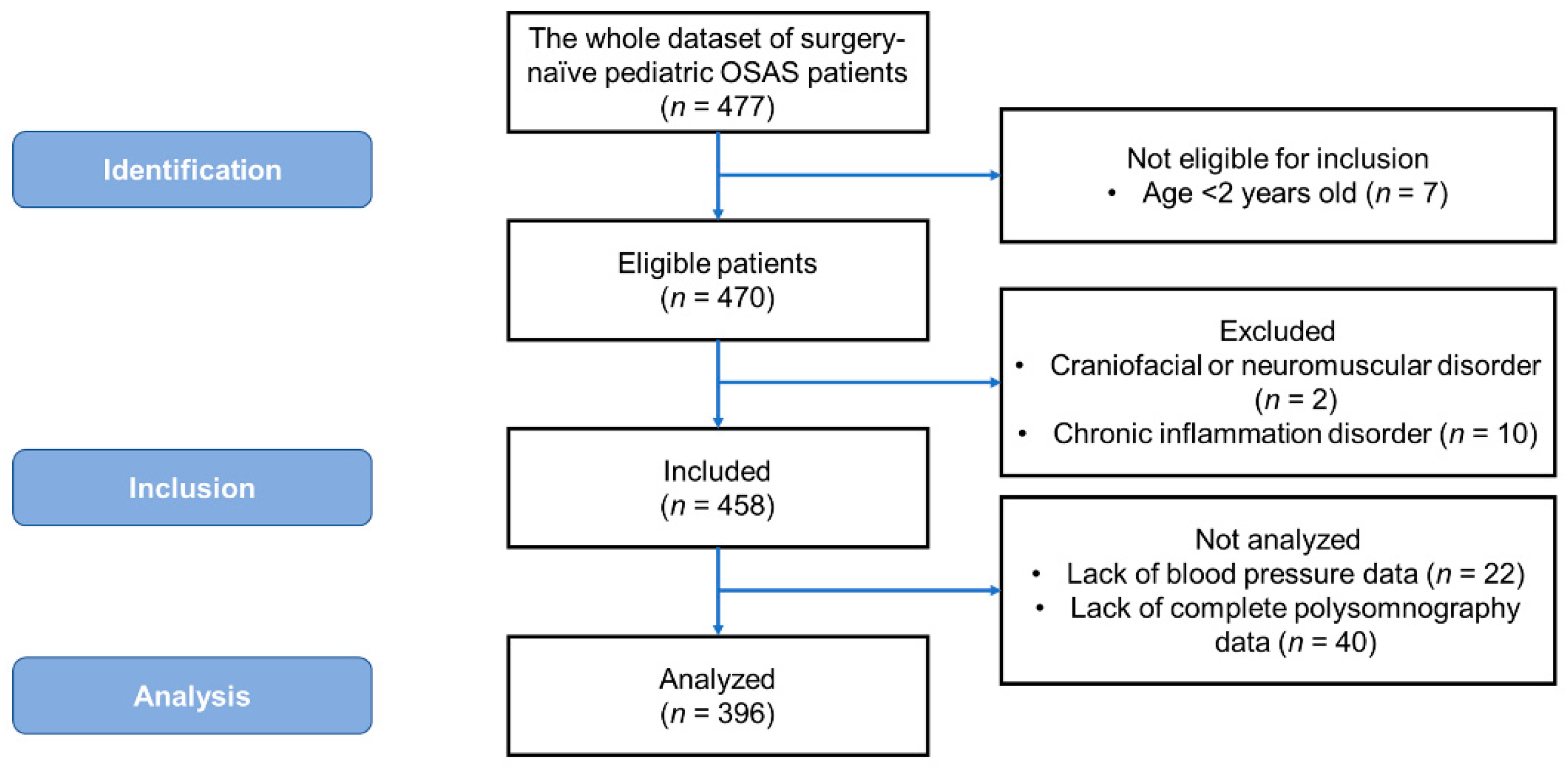
2.2. Patient Selection
2.3. Measurements
2.3.1. Demographic and Anthropometric Variables
2.3.2. Polysomnography
2.3.3. Blood Pressure
2.4. Outcome Variables and Covariates
2.5. Statistical Analysis
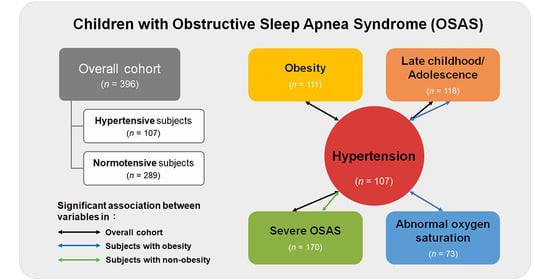
3. Results
3.1. Demographic, Anthropometric, Polysomnographic, and Blood Pressure Characteristics
3.2. Differences in Clinical Variables between the Hypertensive and Normotensive Groups
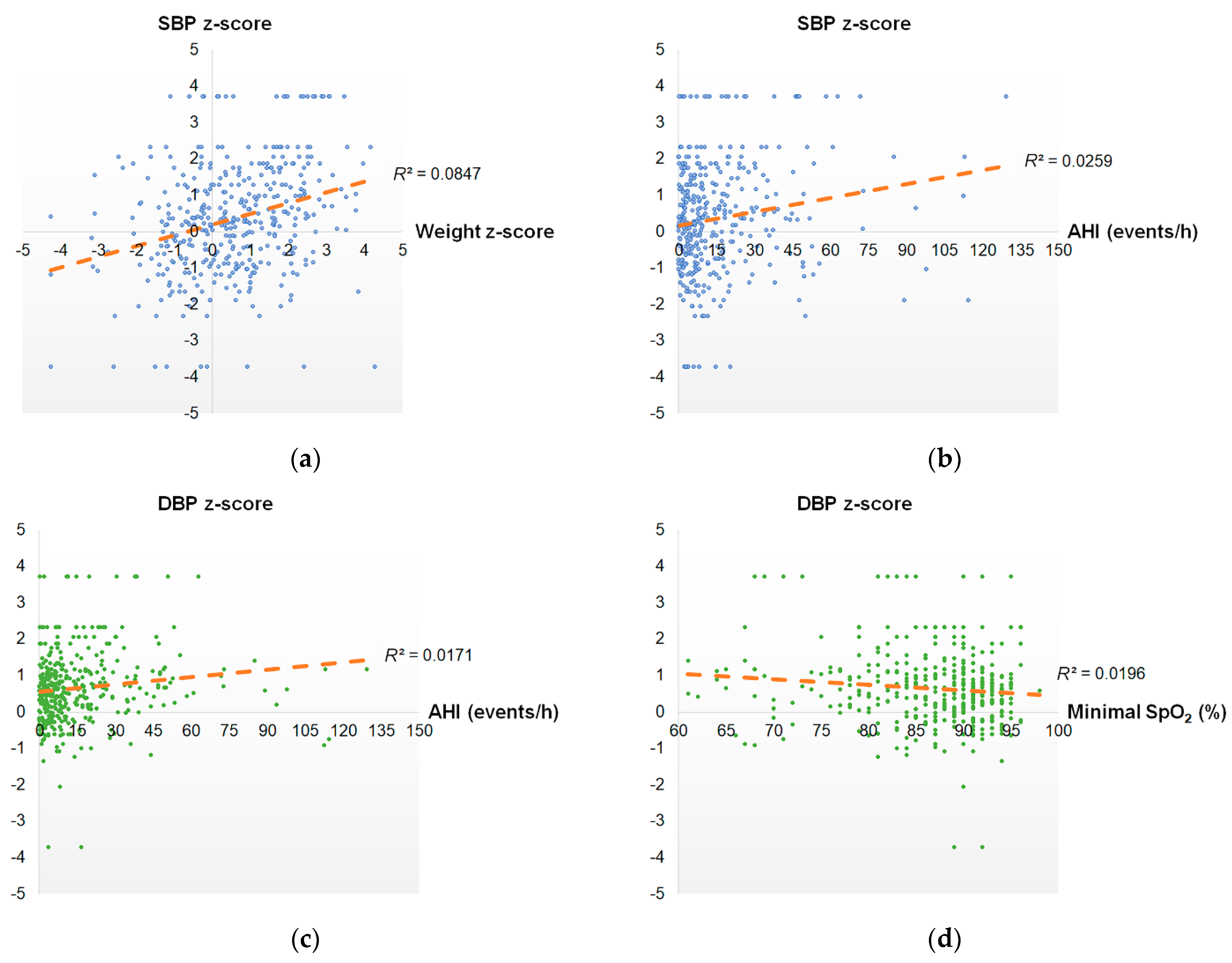
3.3. Associations between Systolic Blood Pressure, Diastolic Blood Pressure, and Clinical Variables
3.4. Variables for Predicting Pediatric Hypertension
3.5. Variables Independently Associated with Hypertension in Obese and Non-Obese Children with OSAS Using Logistic Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lumeng, J.C.; Chervin, R.D. Epidemiology of pediatric obstructive sleep apnea. Proc. Am. Thorac. Soc. 2008, 5, 242–252. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, H.Y.; Lee, L.A. Sleep-disordered breathing in children. Chang. Gung. Med. J. 2009, 32, 247–257. [Google Scholar] [PubMed]
- O’Brien, L.M.; Mervis, C.B.; Holbrook, C.R.; Bruner, J.L.; Klaus, C.J.; Rutherford, J.; Raffield, T.J.; Gozal, D. Neurobehavioral implications of habitual snoring in children. Pediatrics 2004, 114, 44–49. [Google Scholar] [CrossRef] [Green Version]
- Katz, E.S.; D’Ambrosio, C.M. Pathophysiology of pediatric obstructive sleep apnea. Proc. Am. Thorac. Soc. 2008, 5, 253–262. [Google Scholar] [CrossRef]
- Chuang, H.H.; Hsu, J.F.; Chuang, L.P.; Chen, N.H.; Huang, Y.S.; Li, H.Y.; Chen, J.Y.; Lee, L.A.; Huang, C.G. Differences in Anthropometric and Clinical Features among Preschoolers, School-Age Children, and Adolescents with Obstructive Sleep Apnea-A Hospital-Based Study in Taiwan. Int. J. Environ. Res. Publ. Health 2020, 17, 4663. [Google Scholar] [CrossRef]
- Jackman, A.R.; Biggs, S.N.; Walter, L.M.; Embuldeniya, U.S.; Davey, M.J.; Nixon, G.M.; Anderson, V.; Trinder, J.; Horne, R.S. Sleep-disordered breathing in preschool children is associated with behavioral, but not cognitive, impairments. Sleep Med. 2012, 13, 621–631. [Google Scholar] [CrossRef]
- Horne, R.S.; Yang, J.S.; Walter, L.M.; Richardson, H.L.; O’Driscoll, D.M.; Foster, A.M.; Wong, S.; Ng, M.L.; Bashir, F.; Patterson, R.; et al. Elevated blood pressure during sleep and wake in children with sleep-disordered breathing. Pediatrics 2011, 128, e85–e92. [Google Scholar] [CrossRef]
- Song, P.; Zhang, Y.; Yu, J.; Zha, M.; Zhu, Y.; Rahimi, K.; Rudan, I. Global Prevalence of Hypertension in Children: A Systematic Review and Meta-analysis. JAMA Pediatr. 2019, 173, 1154–1163. [Google Scholar] [CrossRef]
- Rao, G. Diagnosis, Epidemiology, and Management of Hypertension in Children. Pediatrics 2016, 138. [Google Scholar] [CrossRef] [Green Version]
- Hardy, S.T.; Urbina, E.M. Blood Pressure in Childhood and Adolescence. Am. J. Hypertens 2021, 34, 242–249. [Google Scholar] [CrossRef] [PubMed]
- Young, T.; Peppard, P.E.; Gottlieb, D.J. Epidemiology of obstructive sleep apnea: A population health perspective. Am. J. Respir. Crit. Care Med. 2002, 165, 1217–1239. [Google Scholar] [CrossRef] [PubMed]
- Nisbet, L.C.; Yiallourou, S.R.; Walter, L.M.; Horne, R.S. Blood pressure regulation, autonomic control and sleep disordered breathing in children. Sleep Med. Rev. 2014, 18, 179–189. [Google Scholar] [CrossRef]
- Brooks, D.M.; Kelly, A.; Sorkin, J.D.; Koren, D.; Chng, S.Y.; Gallagher, P.R.; Amin, R.; Dougherty, S.; Guo, R.; Marcus, C.L.; et al. The relationship between sleep-disordered breathing, blood pressure, and urinary cortisol and catecholamines in children. J. Clin. Sleep Med. 2020, 16, 907–916. [Google Scholar] [CrossRef]
- Gonzaga, C.; Bertolami, A.; Bertolami, M.; Amodeo, C.; Calhoun, D. Obstructive sleep apnea, hypertension and cardiovascular diseases. J. Hum. Hypertens 2015, 29, 705–712. [Google Scholar] [CrossRef] [PubMed]
- Bixler, E.O.; Vgontzas, A.N.; Lin, H.M.; Liao, D.; Calhoun, S.; Fedok, F.; Vlasic, V.; Graff, G. Blood pressure associated with sleep-disordered breathing in a population sample of children. Hypertension 2008, 52, 841–846. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Archbold, K.H.; Vasquez, M.M.; Goodwin, J.L.; Quan, S.F. Effects of sleep patterns and obesity on increases in blood pressure in a 5-year period: Report from the Tucson Children’s Assessment of Sleep Apnea Study. J. Pediatr. 2012, 161, 26–30. [Google Scholar] [CrossRef] [Green Version]
- Zintzaras, E.; Kaditis, A.G. Sleep-disordered breathing and blood pressure in children: A meta-analysis. Arch Pediatr. Adolesc Med. 2007, 161, 172–178. [Google Scholar] [CrossRef]
- Tagetti, A.; Bonafini, S.; Zaffanello, M.; Benetti, M.V.; Vedove, F.D.; Gasperi, E.; Cavarzere, P.; Gaudino, R.; Piacentini, G.; Minuz, P.; et al. Sleep-disordered breathing is associated with blood pressure and carotid arterial stiffness in obese children. J. Hypertens 2017, 35, 125–131. [Google Scholar] [CrossRef]
- Kang, K.T.; Lee, P.L.; Weng, W.C.; Hsu, W.C. Body weight status and obstructive sleep apnea in children. Int. J. Obes. (Lond) 2012, 36, 920–924. [Google Scholar] [CrossRef] [Green Version]
- Walter, L.M.; Tamanyan, K.; Limawan, A.P.; Biggs, S.N.; Weichard, A.J.; Davey, M.J.; Nixon, G.M.; Horne, R.S.C. Overweight and obese children with sleep disordered breathing have elevated arterial stiffness. Sleep Med. 2018, 48, 187–193. [Google Scholar] [CrossRef]
- Evans, C.A.; Selvadurai, H.; Baur, L.A.; Waters, K.A. Effects of obstructive sleep apnea and obesity on exercise function in children. Sleep 2014, 37, 1103–1110. [Google Scholar] [CrossRef] [Green Version]
- Chuang, H.H.; Huang, C.G.; Chuang, L.P.; Huang, Y.S.; Chen, N.H.; Li, H.Y.; Fang, T.J.; Hsu, J.F.; Lai, H.C.; Chen, J.Y.; et al. Relationships Among and Predictive Values of Obesity, Inflammation Markers, and Disease Severity in Pediatric Patients with Obstructive Sleep Apnea Before and After Adenotonsillectomy. J. Clin. Med. 2020, 9, 579. [Google Scholar] [CrossRef] [Green Version]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. PLoS Med. 2007, 4, e296. [Google Scholar] [CrossRef] [Green Version]
- Gottlieb, D.J.; Vezina, R.M.; Chase, C.; Lesko, S.M.; Heeren, T.C.; Weese-Mayer, D.E.; Auerbach, S.H.; Corwin, M.J. Symptoms of sleep-disordered breathing in 5-year-old children are associated with sleepiness and problem behaviors. Pediatrics 2003, 112, 870–877. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.S.; Guilleminault, C.; Hwang, F.M.; Cheng, C.; Lin, C.H.; Li, H.Y.; Lee, L.A. Inflammatory cytokines in pediatric obstructive sleep apnea. Medicine 2016, 95, e4944. [Google Scholar] [CrossRef]
- Flegal, K.M.; Cole, T.J. Construction of LMS parameters for the Centers for Disease Control and Prevention 2000 growth charts. Nat. Health Stat. Rep. 2013, 63, 1–3. [Google Scholar]
- Kuczmarski, R.J.; Ogden, C.L.; Guo, S.S.; Grummer-Strawn, L.M.; Flegal, K.M.; Mei, Z.; Wei, R.; Curtin, L.R.; Roche, A.F.; Johnson, C.L. 2000 CDC Growth Charts for the United States: Methods and development. Vit. Health Stat. 2002, 11, 1–190. [Google Scholar]
- Huang, Y.S.; Guilleminault, C.; Lee, L.A.; Lin, C.H.; Hwang, F.M. Treatment outcomes of adenotonsillectomy for children with obstructive sleep apnea: A prospective longitudinal study. Sleep 2014, 37, 71–76. [Google Scholar] [CrossRef] [Green Version]
- Berry, R.B.; Budhiraja, R.; Gottlieb, D.J.; Gozal, D.; Iber, C.; Kapur, V.K.; Marcus, C.L.; Mehra, R.; Parthasarathy, S.; Quan, S.F.; et al. Rules for scoring respiratory events in sleep: Update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J. Clin. Sleep Med. JCSM Off. Publ. Am. Acad. Sleep Med. 2012, 8, 597–619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004, 114, 555–576. [Google Scholar] [CrossRef]
- Flynn, J.T.; Kaelber, D.C.; Baker-Smith, C.M.; Blowey, D.; Carroll, A.E.; Daniels, S.R.; de Ferranti, S.D.; Dionne, J.M.; Falkner, B.; Flinn, S.K.; et al. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics 2017, 140, e20171904. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steyerberg, E.W.; Eijkemans, M.J.C.; Harrell, F.E.; Habbema, J.D.F. Prognostic modelling with logistic regression analysis: A comparison of selection and estimation methods in small data sets. Stat. Med. 2000, 19, 1059–1079. [Google Scholar] [CrossRef]
- Chang, I.S.; Kang, K.T.; Tseng, C.C.; Weng, W.C.; Hsiao, T.Y.; Lee, P.L.; Hsu, W.C. Revisits after adenotonsillectomy in children with sleep-disordered breathing: A retrospective single-institution study. Clin. Otolaryngol. 2018, 43, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Dehlink, E.; Tan, H.L. Update on paediatric obstructive sleep apnoea. J. Thorac. Dis. 2016, 8, 224–235. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.A.; Laferriere, A.; Lakheeram, I.; Moss, I.R. Recurrent hypoxemia in children is associated with increased analgesic sensitivity to opiates. Anesthesiology 2006, 105, 665–669. [Google Scholar] [CrossRef]
- Wühl, E. Hypertension in childhood obesity. Acta Paediatr. 2019, 108, 37–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pavlyshyn, H.; Furdela, V.; Kovalchuk, T.; Haliyash, N.; Luchyshyn, N. Epidemiological aspects of obesity and systemic hypertension amongschool children of Western Ukraine. Pediatr. Endocrinol. Diabetes Metab. 2017, 23, 181–187. [Google Scholar] [CrossRef]
- Horne, R.S.C. Endothelial Damage in Children with Sleep-disordered Breathing. Am. J. Respir. Crit. Care Med. 2020, 202, 1497–1499. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.Y.; Lin, R.H.; Lin, Y.C.; Chen, J.Y.; Li, W.C.; Lee, L.A.; Liu, K.H.; Chuang, H.H. Are Body Composition Parameters Better than Conventional Anthropometric Measures in Predicting Pediatric Hypertension? Int. J. Environ. Res. Public Health 2020, 17, 5771. [Google Scholar] [CrossRef]
- Díaz, A.; Calandra, L. High blood pressure in school children and adolescents in Argentina over the past 25 years: A systematic review of observational studies. Arch Argent Pediatr. 2017, 115, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Chan, K.C.; Au, C.T.; Hui, L.L.; Ng, S.K.; Wing, Y.K.; Li, A.M. How OSA Evolves From Childhood to Young Adulthood: Natural History From a 10-Year Follow-up Study. Chest 2019, 156, 120–130. [Google Scholar] [CrossRef]
- Kimura, H.; Ota, H.; Kimura, Y.; Takasawa, S. Effects of Intermittent Hypoxia on Pulmonary Vascular and Systemic Diseases. Int. J. Environ. Res. Publ. Health 2019, 16, 3101. [Google Scholar] [CrossRef] [Green Version]
- Battu, H.S.; Bhopal, R.; Agyemang, C. Heterogeneity in blood pressure in UK Bangladeshi, Indian and Pakistani, compared to White, populations: Divergence of adults and children. J. Hum. Hyper. 2018, 32, 725–744. [Google Scholar] [CrossRef] [PubMed]
- Qian, K.; Tan, L.; Li, S.; Li, Z.; Yu, F.; Liang, H.; Gao, S.; Ren, X.; Zhang, J.; Zhang, Z. Comparison of different BMI cut-offs to screen for child and adolescent obesity in urban China. Publ. Health Nutr. 2020, 23, 2485–2493. [Google Scholar] [CrossRef] [PubMed]
- de Wilde, J.A.; van Dommelen, P.; Middelkoop, B.J. Appropriate body mass index cut-offs to determine thinness, overweight and obesity in South Asian children in the Netherlands. PLoS ONE 2013, 8, e82822. [Google Scholar] [CrossRef]
- Liu, A.; Byrne, N.M.; Kagawa, M.; Ma, G.; Poh, B.K.; Ismail, M.N.; Kijboonchoo, K.; Nasreddine, L.; Trinidad, T.P.; Hills, A.P. Ethnic differences in the relationship between body mass index and percentage body fat among Asian children from different backgrounds. Br. J. Nutr. 2011, 106, 1390–1397. [Google Scholar] [CrossRef] [Green Version]
- Cai, A.; Wang, L.; Zhou, Y. Hypertension and obstructive sleep apnea. Hyper. Res. 2016, 39, 391–395. [Google Scholar] [CrossRef]
- May, A.M.; Van Wagoner, D.R.; Mehra, R. OSA and Cardiac Arrhythmogenesis: Mechanistic Insights. Chest 2017, 151, 225–241. [Google Scholar] [CrossRef]
- Kleiger, R.E.; Stein, P.K.; Bigger, J.T., Jr. Heart rate variability: Measurement and clinical utility. Ann. Noninv. Electrocardiol. 2005, 10, 88–101. [Google Scholar] [CrossRef] [PubMed]
- Fan, X.; Wang, H.; Xu, F.; Zhao, Y.; Tsui, K.-L. Homecare-Oriented Intelligent Long-Term Monitoring of Blood Pressure Using Electrocardiogram Signals. IEEE Trans. Ind. Inf. 2020, 16, 7150–7158. [Google Scholar] [CrossRef]
- Shen, Q.; Qin, H.; Wei, K.; Liu, G. Multiscale Deep Neural Network for Obstructive Sleep Apnea Detection Using RR Interval From Single-Lead ECG Signal. IEEE Trans. Inst. Meas. 2021, 70, 1–13. [Google Scholar] [CrossRef]
- de Chazal, P.; Penzel, T.; Heneghan, C. Automated detection of obstructive sleep apnoea at different time scales using the electrocardiogram. Physiol. Meas. 2004, 25, 967–983. [Google Scholar] [CrossRef] [Green Version]
- Wu, S.; Liang, D.; Yang, Q.; Liu, G. Regularity of heart rate fluctuations analysis in obstructive sleep apnea patients using information-based similarity. Biomed. Sig. Proc. Control 2021, 65. [Google Scholar] [CrossRef]
- Hussain, S.F.; Zahid, S.; Haqqee, R.; Khan, J.A. General physicians’ perspective of sleep apnea from a developing country. Southeast Asian J. Trop. Med. Public Health 2003, 34, 420–423. [Google Scholar] [PubMed]
- Lee, L.A.; Li, H.Y.; Lin, Y.S.; Fang, T.J.; Huang, Y.S.; Hsu, J.F.; Wu, C.M.; Huang, C.G. Severity of childhood obstructive sleep apnea and hypertension improved after adenotonsillectomy. Otolaryngol. Head Neck Surg. 2015, 152, 553–560. [Google Scholar] [CrossRef]
- Lee, C.H.; Kang, K.T.; Chiu, S.N.; Chang, I.S.; Weng, W.C.; Lee, P.L.; Hsu, W.C. Association of Adenotonsillectomy With Blood Pressure Among Hypertensive and Nonhypertensive Children With Obstructive Sleep Apnea. JAMA Otolaryngol. Head Neck Surg. 2018, 144, 300–307. [Google Scholar] [CrossRef] [Green Version]
- Brady, T.M. Obesity-Related Hypertension in Children. Front. Pediatr. 2017, 5, 197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hagman, E.; Danielsson, P.; Elimam, A.; Marcus, C. The effect of weight loss and weight gain on blood pressure in children and adolescents with obesity. Int. J. Obes. 2019, 43, 1988–1994. [Google Scholar] [CrossRef]
- Grote, L.; McNicholas, W.T.; Hedner, J.; Collaborators, E. Sleep apnoea management in Europe during the COVID-19 pandemic: Data from the European Sleep Apnoea Database (ESADA). Eur. Respir J. 2020, 55. [Google Scholar] [CrossRef]
- Hsieh, H.S.; Kang, C.J.; Chuang, H.H.; Zhuo, M.Y.; Lee, G.S.; Huang, Y.S.; Chuang, L.P.; Kuo, T.B.J.; Yang, C.C.H.; Lee, L.A.; et al. Screening Severe Obstructive Sleep Apnea in Children with Snoring. Diagnostics 2021, 11, 1168. [Google Scholar] [CrossRef]
- Altman, D.G.; Royston, P. The cost of dichotomising continuous variables. BMJ 2006, 332, 1080. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pepe, M.S.; Janes, H.; Longton, G.; Leisenring, W.; Newcomb, P. Limitations of the odds ratio in gauging the performance of a diagnostic, prognostic, or screening marker. Am. J. Epidemiol. 2004, 159, 882–890. [Google Scholar] [CrossRef] [PubMed]
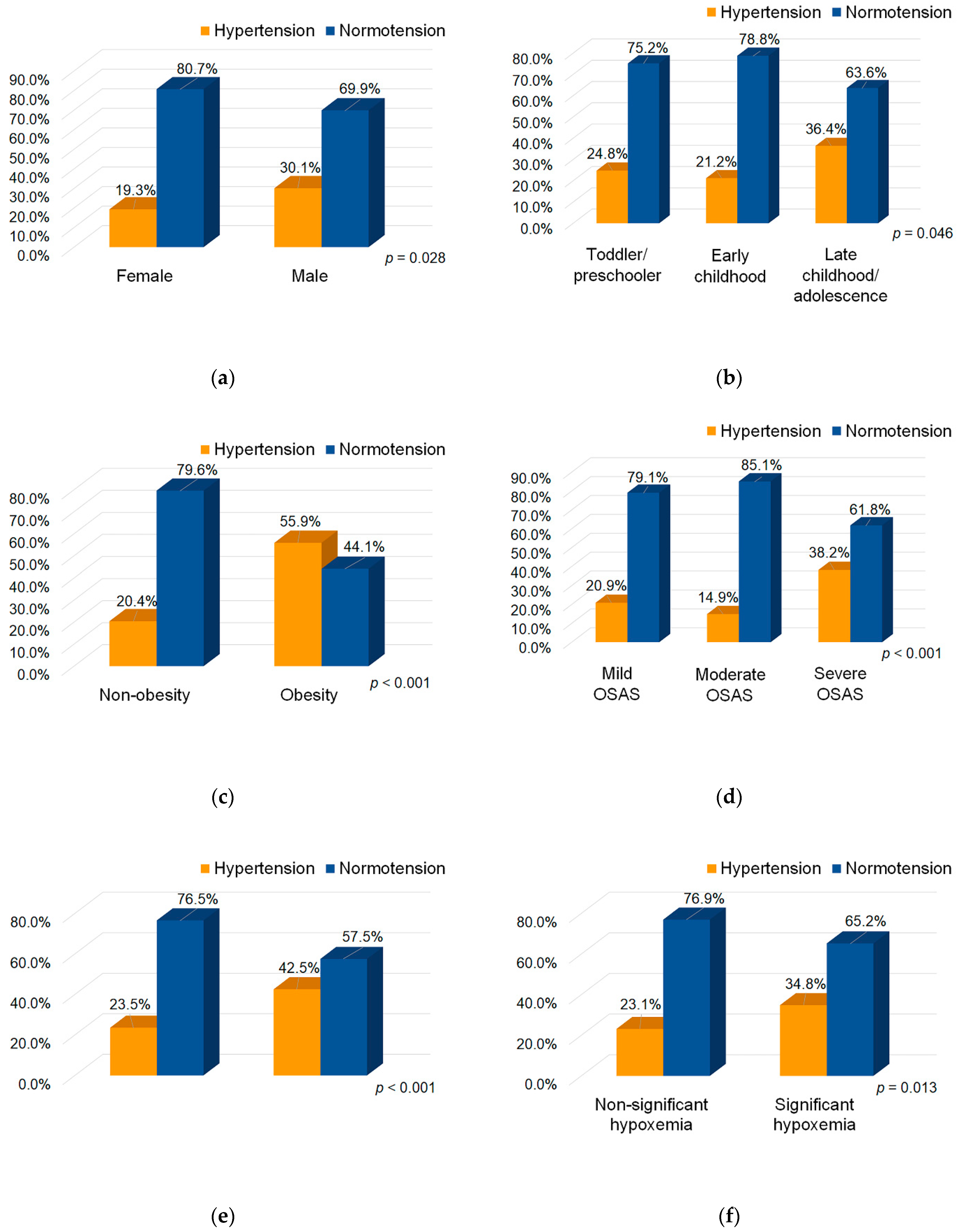
| Variables | Hypertensive Group | Normotensive Group | p-Value |
|---|---|---|---|
| Patients | n = 107 | n = 289 | |
| Blood pressure measures | |||
| SBP z-score | 2.019 (1.258) | −0.250 (1.102) | <0.001 1 |
| DBP z-score | 1.554 (1.178) | 0.317 (0.671) | <0.001 1 |
| Demographic measures | |||
| Sex | |||
| Female, n (%) | 22 (19.3) | 92 (80.7) | 0.028 2 |
| Male, n (%) | 85 (30.1) | 197 (69.9) | |
| Age, years | 7.88 (3.01) | 7.36 (2.60) | 0.115 1 |
| Development stage | |||
| Toddler/preschooler, n (%) | 35 (24.8) | 106 (75.2) | 0.046 3 |
| Early childhood, n (%) | 29 (21.2) | 108 (78.8) | |
| Late childhood/adolescence, n (%) | 43 (36.4) | 75 (63.6) | |
| Anthropometric measures | |||
| Weight z-score | 1.066 (1.486) | 0.362 (1.458) | <0.001 1 |
| Height z-score | 0.345 (1.133) | 0.102 (1.166) | 0.064 1 |
| BMI z-score | 1.088 (1.459) | 0.429 (1.434) | <0.001 1 |
| Obesity | |||
| Non-obesity, n (%) | 58 (20.4) | 227 (79.6) | <0.001 2 |
| Obesity, n (%) | 62 (55.9) | 49 (44.1) | |
| Polysomnographic measures | |||
| AHI, events/h | 20.59 (21.50) | 13.37 (17.72) | 0.003 1 |
| Disease severity | |||
| Mild OSAS, n (%) | 29 (20.9) | 110 (79.1) | <0.001 3 |
| Moderate OSAS, n (%) | 13 (14.9) | 74 (85.1) | |
| Severe OSAS, n (%) | 65 (38.2) | 105 (61.8) | |
| Mean SpO2, % | 95.15 (3.18) | 96.01 (2.85) | 0.015 1 |
| Abnormal SpO2 | |||
| Normal SpO2, n (%) | 76 (23.5) | 247 (76.5) | 0.001 2 |
| Abnormal SpO2, n (%) | 31 (42.5) | 42 (57.5) | |
| Minimal SpO2, % | 83.02 (11.39) | 86.32 (8.00) | 0.007 1 |
| Significant hypoxemia | |||
| Non-significant hypoxemia, n (%) | 61 (23.1) | 203 (76.9) | 0.013 2 |
| Significant hypoxemia, n (%) | 46 (34.8) | 86 (65.2) | |
| Family history of hypertension | |||
| Absence, n (%) | 89 (25.9) | 254 (74.1) | 0.221 2 |
| Presence, n (%) | 18 (34.0) | 35 (66.0) | |
| Family history of OSAS | |||
| Absence, n (%) | 106 (27.2) | 283 (72.8) | 0.680 4 |
| Presence, n (%) | 1 (14.3) | 6 (85.7) | |
| Family history of obesity | |||
| Absence, n (%) | 104 (26.6) | 287 (73.4) | 0.125 4 |
| Presence, n (%) | 3 (60.0) | 2 (40.0) | |
| Predictors | Regression Coefficient (95% CI) | p-Value 1 | Regression Coefficient (95% CI) | p-Value 1 |
|---|---|---|---|---|
| Full model | Parsimonious model | |||
| Systolic blood pressure z-score | ||||
| Weight z-score | 0.27 (0.17–0.37) | <0.001 | 0.27 (0.18–0.37) | <0.001 |
| AHI, events/h | 0.01 (−0.01–0.02) | 0.314 | 0.01 (0.001–0.02) | 0.043 |
| Mean SpO2, % | −0.002 (−0.07–0.06) | 0.959 | NI 2 | |
| Minimal SpO2, % | −0.01 (−0.03–0.02) | 0.505 | NI 2 | |
| Model summary | R2 = 0.095 | R2 = 0.090 | ||
| Diastolic blood pressure z-score | ||||
| Weight z-score | 0.06 (−0.01–0.12) | 0.100 | NI 2 | |
| AHI, events/h | 0.003 (−0.004–0.01) | 0.401 | NI 2 | |
| Minimal SpO2, % | −0.01 (−0.02–0.01) | 0.210 | −0.02 (−0.03–−0.01) | 0.005 |
| Model summary | R2 = 0.029 | R2 = 0.020 | ||
| Predictors | Odds Ratio (95%CI) | p-Value 1 |
|---|---|---|
| Sex | ||
| Female | reference | |
| Male | 1.80 (1.06–3.07) | 0.029 |
| Developmental stage | ||
| Toddler/preschooler | reference | |
| Early childhood | 0.81 (0.46–1.42) | 0.470 |
| Late childhood/adolescence | 1.74 (1.02–2.97) | 0.043 |
| Obesity | ||
| Non-obesity | reference | |
| Obesity | 3.09 (1.93–4.96) | <0.001 |
| Disease severity | ||
| Mild OSAS | reference | |
| Moderate OSAS | 0.67 (0.33–1.37) | 0.267 |
| Severe OSAS | 2.35 (1.41–3.92) | 0.001 |
| Abnormal SpO2 | ||
| Normal SpO2 | reference | |
| Abnormal SpO2 | 2.40 (1.41–4.08) | 0.001 |
| Significant hypoxemia | ||
| Non-significant hypoxemia | reference | |
| Significant hypoxemia | 1.78 (1.13–2.82) | 0.014 |
| Family history of hypertension | ||
| Absence | reference | |
| Presence | 1.47 (0.79–2.72) | 0.223 |
| Family history of OSAS | ||
| Absence | reference | |
| Presence | 0.45 (0.05–3.74) | 0.456 |
| Family history of obesity | ||
| Absence | reference | |
| Presence | 4.14 (0.68–25.1) | 0.123 |
| Predictors | Odds Ratio (95%CI) | p-Value 1 | Odds Ratio (95%CI) | p-Value 1 |
|---|---|---|---|---|
| Full model | Parsimonious model | |||
| Female sex | reference | |||
| Male sex | 1.61 (0.91–2.82) | 0.101 | NI 2 | |
| Toddler/preschooler/early childhood | reference | reference | ||
| Late childhood/adolescence | 1.67 (1.02–2.74) | 0.044 | 1.72 (1.05–2.81) | 0.031 |
| Non-obesity | reference | reference | ||
| Obesity | 2.58 (1.51–4.07) | <0.001 | 2.58 (1.58–4.22) | <0.001 |
| Non-severe OSAS | reference | reference | ||
| Severe OSAS | 1.99 (1.20–3.32) | 0.008 | 2.38 (1.48–3.81) | <0.001 |
| Normal SpO2 | reference | |||
| Abnormal SpO2 | 1.70 (0.93–3.11) | 0.084 | NI 2 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chuang, H.-H.; Hsu, J.-F.; Wang, C.-Y.; Chuang, L.-P.; Chen, M.-C.; Chen, N.-H.; Huang, Y.-S.; Li, H.-Y.; Lee, L.-A. Hypertension in Children with Obstructive Sleep Apnea Syndrome—Age, Weight Status, and Disease Severity. Int. J. Environ. Res. Public Health 2021, 18, 9602. https://doi.org/10.3390/ijerph18189602
Chuang H-H, Hsu J-F, Wang C-Y, Chuang L-P, Chen M-C, Chen N-H, Huang Y-S, Li H-Y, Lee L-A. Hypertension in Children with Obstructive Sleep Apnea Syndrome—Age, Weight Status, and Disease Severity. International Journal of Environmental Research and Public Health. 2021; 18(18):9602. https://doi.org/10.3390/ijerph18189602
Chicago/Turabian StyleChuang, Hai-Hua, Jen-Fu Hsu, Chao-Yung Wang, Li-Pang Chuang, Min-Chi Chen, Ning-Hung Chen, Yu-Shu Huang, Hsueh-Yu Li, and Li-Ang Lee. 2021. "Hypertension in Children with Obstructive Sleep Apnea Syndrome—Age, Weight Status, and Disease Severity" International Journal of Environmental Research and Public Health 18, no. 18: 9602. https://doi.org/10.3390/ijerph18189602
APA StyleChuang, H.-H., Hsu, J.-F., Wang, C.-Y., Chuang, L.-P., Chen, M.-C., Chen, N.-H., Huang, Y.-S., Li, H.-Y., & Lee, L.-A. (2021). Hypertension in Children with Obstructive Sleep Apnea Syndrome—Age, Weight Status, and Disease Severity. International Journal of Environmental Research and Public Health, 18(18), 9602. https://doi.org/10.3390/ijerph18189602