How Managers Perceive and (Do Not) Participate in Health Promotion Measures—Results from a Cross-Sectional Mixed-Methods Survey in a Large ICT Company
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Context
2.2. Survey Development
2.3. Sample and Data Collection
2.4. Measures
2.4.1. Sociodemographic Characteristics, Health- and Work-Related Scales
2.4.2. HPM Participation and Working Conditions
2.5. Data Analysis
2.5.1. Quantitative Analysis
2.5.2. Qualitative Analysis
3. Results
3.1. Sociodemographic, Health-, and Work-Related Characteristics
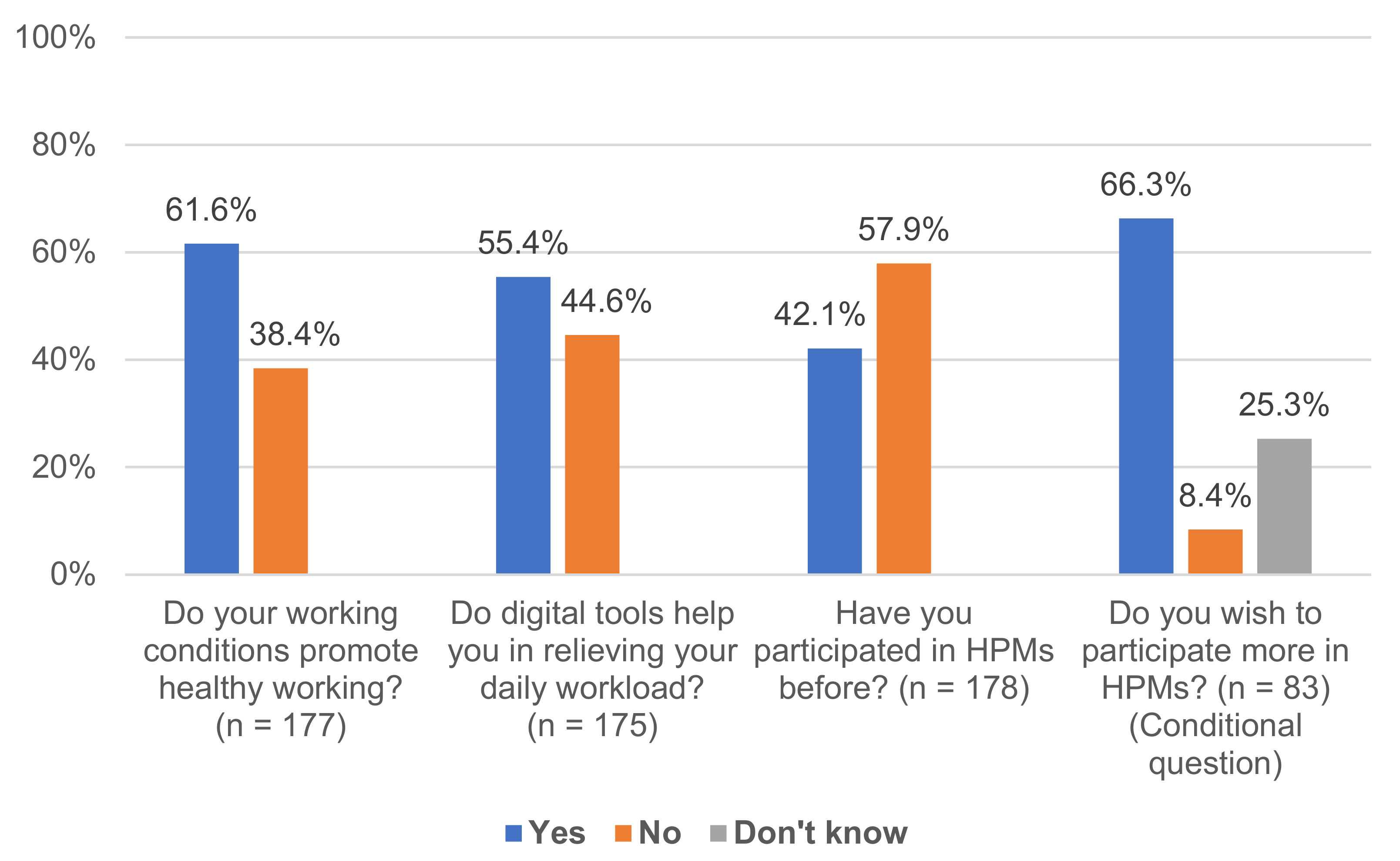
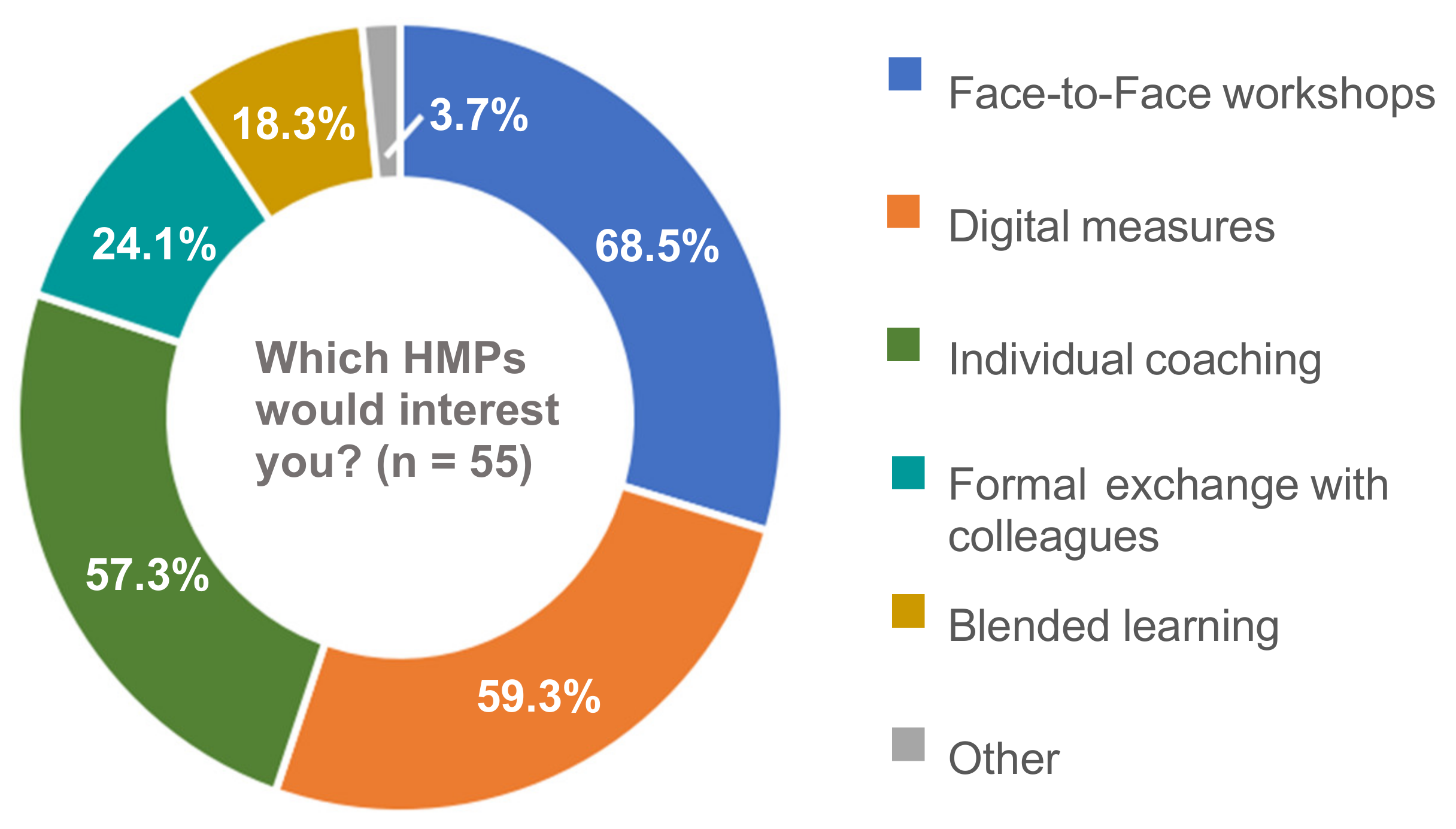
3.2. Quantitative Descriptive Findings: Working Conditions and HPM Participation
3.3. Logistic Regression: Association of Individual and Organizational Variables with HPM Participation
3.4. Qualitative Findings: Working Conditions and HPM Participation
4. Discussion
4.1. Managers’ HPM Participation (1)
4.2. Association of Individual and Organizational Factors with Managers’ HPM Participation (1)
4.3. Managers’ Working Conditions (2)
5. Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HPMs | Health Promotion Measures |
| ICT | Information and Communication Technologies |
References
- Yao, L.; Li, P.; Wildy, H. Health-Promoting Leadership: Concept, Measurement, and Research Framework. Front. Psychol. 2021, 12, 602333. [Google Scholar] [CrossRef]
- Scully-Russ, E.; Torraco, R. The Changing Nature and Organization of Work: An Integrative Review of the Literature. Hum. Resour. Dev. Rev. 2020, 19, 66–93. [Google Scholar] [CrossRef]
- World Bank. World Development Report 2019: The Changing Nature of Work; World Bank: Washington, DC, USA, 2019; ISBN 978-1-4648-1328-3. [Google Scholar]
- Eurofound. Telework and ICT-Based Mobile Work: Flexible Working in the Digital Age. New Forms of Employment Series; Publications Office of the European Union: Luxembourg, 2020. Available online: https://www.eurofound.europa.eu/sites/default/files/ef_publication/field_ef_document/ef19032en.pdf (accessed on 3 May 2021).
- Tsiga, E.; Panagopoulou, E.; Niakas, D. Health promotion across occupational groups: One size does not fit all. Occup. Med. 2015, 65, 552–557. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eurofound. Sixth European Working Conditions Survey: Overview Report (2017 Update); Publications Office of the European Union: Luxembourg, 2017.
- Bundesanstalt für Arbeitsschutz und Arbeitsmedizin. Stressreport Deutschland 2019: Psychische Anforderungen, Ressourcen und Befinden. [Stress Report Germany 2019. Mental Demands, Resources and Well-Being]. 2020. Available online: https://www.baua.de/DE/Angebote/Publikationen/Berichte/Stressreport-2019.pdf?__blob=publicationFile&v=8 (accessed on 3 May 2021).
- Stadin, M.; Nordin, M.; Broström, A.; Magnusson Hanson, L.L.; Westerlund, H.; Fransson, E.I. Technostress operationalised as information and communication technology (ICT) demands among managers and other occupational groups—Results from the Swedish Longitudinal Occupational Survey of Health (SLOSH). Comput. Hum. Behav. 2021, 114, 106486. [Google Scholar] [CrossRef]
- Harms, P.D.; Credé, M.; Tynan, M.; Leon, M.; Jeung, W. Leadership and stress: A meta-analytic review. Leadersh. Q. 2017, 28, 178–194. [Google Scholar] [CrossRef]
- Thomson, B.; Steidelmüller, C.; Schröder, T.; Wittmers, A.; Pundt, F.; Weber, C. Erste Ergebnisse des BAuA-Projekts “Führung und Organisation im Wandel”. Sonderheft Führungsforschung [First results of the BAuA project “Leadership and Organization in Transition”. Special Issue in Leadership research]. ASU Z. Med. Prävent. 2020, 55, 1–43. [Google Scholar]
- Berman, S.; Marshall, A. The next digital transformation: From an individual-centered to an everyone-to-everyone economy. Strategy Leadersh. 2014, 42, 9–17. [Google Scholar] [CrossRef]
- Westerman, G.; Bonnet, D.; McAfee, A. Leading Digital: Turning Technology into Business Transformation; Harvard Business Review Press: Boston, MA, USA, 2015; ISBN 9781625272485. [Google Scholar]
- European Network for Workplace Health Promotion. Luxembourg Declaration on Workplace Health Promotion in the European Union. Available online: https://www.enwhp.org/resources/toolip/doc/2018/05/04/luxembourg_declaration.pdf (accessed on 24 May 2021).
- GKV-Spitzenverband. Leitfaden Prävention: Handlungsfelder und Kriterien nach §20 Abs. 2 SGB V zur Umsetzung der §§20, 20a und 20b SGB V vom 21. Juni 2000 in der Fassung vom 14. Dezember 2020 [Guideline Prevention: Fields of action and criteria according to §20 para. 2 SGB V for the implementation of §§20, 20a and 20b SGB V of June 21, 2000 in the version of December 14, 2020]. Available online: https://www.gkv-spitzenverband.de/media/dokumente/krankenversicherung_1/praevention__selbsthilfe__beratung/praevention/praevention_leitfaden/Leitfaden_Pravention_2020_barrierefrei.pdf (accessed on 24 May 2021).
- Robroek, S.J.W.; van Lenthe, F.J.; van Empelen, P.; Burdorf, A. Determinants of participation in worksite health promotion programmes: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 26. [Google Scholar] [CrossRef] [Green Version]
- Ludwig, S.; Starker, A.; Hermann, S.; Jordan, S. The use of workplace health promotion interventions in Germany—Results of the study “German Health Update” (GEDA 2014/2015-EHIS). Bundesgesundheitsblatt 2020, 63, 1491–1501. [Google Scholar] [CrossRef]
- Tsai, R.; Alterman, T.; Grosch, J.W.; Luckhaupt, S.E. Availability of and Participation in Workplace Health Promotion Programs by Sociodemographic, Occupation, and Work Organization Characteristics in US Workers. Am. J. Health Promot. 2019, 33, 1028–1038. [Google Scholar] [CrossRef]
- Kilpatrick, M.; Blizzard, L.; Sanderson, K.; Teale, B.; Venn, A. Factors Associated with Availability of, and Employee Participation in, Comprehensive Workplace Health Promotion in a Large and Diverse Australian Public Sector Setting: A Cross-Sectional Survey. J. Occup. Environ. Med. 2015, 57, 1197–1206. [Google Scholar] [CrossRef] [PubMed]
- Stein, A.D.; Shakour, S.K.; Zuidema, R.A. Financial incentives, participation in employer-sponsored health promotion, and changes in employee health and productivity: HealthPlus Health Quotient Program. J. Occup. Environ. Med. 2000, 42, 1148–1155. [Google Scholar] [CrossRef]
- Justesen, J.B.; Eskerod, P.; Christensen, J.R.; Sjøgaard, G. Implementing workplace health promotion—Role of middle managers. Int. J. Workplace Health Manag. 2017, 10, 164–178. [Google Scholar] [CrossRef] [Green Version]
- Hasson, H.; Villaume, K.; von Thiele Schwarz, U.; Palm, K. Managing implementation: Roles of line managers, senior managers, and human resource professionals in an occupational health intervention. J. Occup. Environ. Med. 2014, 56, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Beck, D.; Lenhardt, U.; Schmitt, B.; Sommer, S. Patterns and predictors of workplace health promotion: Cross-sectional findings from a company survey in Germany. BMC Public Health 2015, 15, 343. [Google Scholar] [CrossRef] [Green Version]
- Linnan, L.; Weiner, B.; Graham, A.; Emmons, K. Manager Beliefs regarding Worksite Health Promotion: Findings from the Working Healthy Project 2. Am. J. Health Promot. 2007, 21, 521–528. [Google Scholar] [CrossRef] [PubMed]
- Sargent, G.M.; Banwell, C.; Strazdins, L.; Dixon, J. Time and participation in workplace health promotion: Australian qualitative study. Health Promot. Int. 2018, 33, 436–447. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sigblad, F.; Savela, M.; Okenwa Emegwa, L. Managers’ Perceptions of Factors Affecting Employees’ Uptake of Workplace Health Promotion (WHP) Offers. Front. Public Health 2020, 8. [Google Scholar] [CrossRef] [PubMed]
- Frykman, M.; Lundmark, R.; von Thiele Schwarz, U.; Villaume, K.; Hasson, H. Line managers’ influence on employee usage of a web-based system for occupational health management. Int. J. Workplace Health Manag. 2018, 11, 193–209. [Google Scholar] [CrossRef]
- Passey, D.G.; Brown, M.C.; Hammerback, K.; Harris, J.R.; Hannon, P.A. Managers’ Support for Employee Wellness Programs: An Integrative Review. Am. J. Health Promot. 2018, 32, 1789–1799. [Google Scholar] [CrossRef]
- Passey, D.G.; Hammerback, K.; Huff, A.; Harris, J.R.; Hannon, P.A. The Role of Managers in Employee Wellness Programs: A Mixed-Methods Study. Am. J. Health Promot. 2018, 32, 1697–1705. [Google Scholar] [CrossRef] [PubMed]
- Weiner, B.J.; Lewis, M.A.; Linnan, L.A. Using organization theory to understand the determinants of effective implementation of worksite health promotion programs. Health Educ. Res. 2009, 24, 292–305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Linnan, L.A.; Sorensen, G.; Colditz, G.; Klar, D.N.; Emmons, K.M. Using theory to understand the multiple determinants of low participation in worksite health promotion programs. Health Educ. Behav. 2001, 28, 591–607. [Google Scholar] [CrossRef]
- Andersen, R.M. Revisiting the Behavioral Model and Access to Medical Care: Does it Matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef]
- Reinhardt, A.; Adams, J.; Schöne, K.; Rose, D.-M.; Sammito, S. Do working characteristics influence the participation at health measures? Findings from a trial phase of workplace health promotion. J. Occup. Med. Toxicol. 2020, 15, 11. [Google Scholar] [CrossRef]
- Beck, D.; Lenhardt, U. Workplace Health Promotion in Germany: Prevalence and Utilisation. Analyses on Labour Force Surveys of the Federal Institute for Occupational Safety and Health in 2006 and 2012. Gesundheitswesen 2016, 78, 56–62. [Google Scholar] [CrossRef] [Green Version]
- Rongen, A.; Robroek, S.J.W.; van Ginkel, W.; Lindeboom, D.; Pet, M.; Burdorf, A. How needs and preferences of employees influence participation in health promotion programs: A six-month follow-up study. BMC Public Health 2014, 14, 1277. [Google Scholar] [CrossRef] [Green Version]
- Hall, M.E.; Bergman, R.J.; Nivens, S. Worksite health promotion program participation: A study to examine the determinants of participation. Health Promot. Pract. 2014, 15, 768–776. [Google Scholar] [CrossRef]
- Barthelmes, I.; Bödeker, W.; Sörensen, J.; Kleinlercher, K.-M.; Odoy, J. iga.Report 40. Wirksamkeit und Nutzen arbeitsweltbezogener Gesundheitsförderung und Prävention: Zusammenstellung der wissenschaftlichen Evidenz 2012 bis 2018. [iga.Report 40. Effectiveness and Benefits of Workplace-Related Health Promotion and Prevention. Compilation of scientific evidence 2012 to 2018]. 2019. Available online: https://www.iga-info.de/fileadmin/redakteur/Veroeffentlichungen/iga_Reporte/Dokumente/iga-Report_40_Wirksamkeit_und_Nutzen_Gesundheitsfoerderung_Praevention.pdf (accessed on 10 September 2021).
- Kilpatrick, M.; Blizzard, L.; Sanderson, K.; Teale, B.; Jose, K.; Venn, A. Barriers and facilitators to participation in workplace health promotion (WHP) activities: Results from a cross-sectional survey of public-sector employees in Tasmania, Australia. Health Promot. J. Aust. 2017, 28, 225–232. [Google Scholar] [CrossRef]
- Rojatz, D.; Merchant, A.; Nitsch, M. Factors influencing workplace health promotion intervention: A qualitative systematic review. Health Promot. Int. 2017, 32, 831–839. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lier, L.M.; Breuer, C.; Dallmeyer, S. Organizational-level determinants of participation in workplace health promotion programs: A cross-company study. BMC Public Health 2019, 19, 268. [Google Scholar] [CrossRef]
- van der Put, A.C.; van der Lippe, T. Work Environment and Worksite Health Promotion in Nine European Countries. J. Occup. Environ. Med. 2020, 62, 272–278. [Google Scholar] [CrossRef] [Green Version]
- Schubin, K.; Schlomann, L.; Lindert, L.; Pfaff, H.; Choi, K.-E. Occupational Physicians’ Perspectives on Determinants of Employee Participation in a Randomized Controlled Musculoskeletal Health Promotion Measure: A Qualitative Study. Int. J. Environ. Res. Public Health 2020, 17, 7445. [Google Scholar] [CrossRef]
- Gingerich, S.B.; Anderson, D.R.; Koland, H. Impact of financial incentives on behavior change program participation and risk reduction in worksite health promotion. Am. J. Health Promot. 2012, 27, 119–122. [Google Scholar] [CrossRef]
- O’Cathain, A.; Murphy, E.; Nicholl, J. Why, and how, mixed methods research is undertaken in health services research in England: A mixed methods study. BMC Health Serv. Res. 2007, 7, 85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schoonenboom, J.; Johnson, R.B. How to Construct a Mixed Methods Research Design. Koln. Z. Soz. Sozpsychol. 2017, 69, 107–131. [Google Scholar] [CrossRef]
- Creswell, J.W.; Plano Clark, V.L. Designing and Conducting Mixed Methods Research, 2nd ed.; SAGE: Los Angeles, CA, USA; London, UK; New Delhi, India; Singapore; Washington, DC, USA, 2011; ISBN 9781412975179. [Google Scholar]
- WHO Collaborating Center for Mental Health. WHO (Fünf)—Fragebogen zum Wohlbefinden (Version 1998) [WHO (Five)—Well-Being Questionnaire (Version 1998)]. 1998. Available online: https://www.psykiatri-regionh.dk/who-5/Documents/WHO5_German.pdf (accessed on 3 May 2021).
- Sischka, P.E.; Costa, A.P.; Steffgen, G.; Schmidt, A.F. The WHO-5 well-being index—Validation based on item response theory and the analysis of measurement invariance across 35 countries. J. Affect. Disord. Rep. 2020, 1, 100020. [Google Scholar] [CrossRef]
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The WHO-5 Well-Being Index: A systematic review of the literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef] [PubMed]
- SOEP-IS Group. SOEP-IS 2018—Questionnaire for the SOEP Innovation Sample: SOEP Survey Papers 890: Series A—Survey Instruments (Erhebungsinstrumente); SOEP Survey Papers No. 890. 2020. Available online: https://www.diw.de/documents/publikationen/73/diw_01.c.798098.de/diw_ssp0890.pdf (accessed on 10 September 2021).
- Pfaff, H.; Pühlhofer, F.; Brinkmann, A.; Lütticke, J.; Nitzsche, A.; Steffen, P.; Stoll, A.; Richter, P. Der Mitarbeiterkennzahlenbogen (MIKE) Kompendium valider Kennzahlen: Kennzahlenhandbuch [The Compendium of Valid Employee Key Performance Indicators (MIKE)]; Institut für Medizinsoziologie, Versorgungsforschung und Rehabilitation (IMVR): Köln, Germany, 2004. [Google Scholar]
- Richter, P.; Hemmann, E.; Merboth, H.; Fritz, S.; Hansgen, C.; Rudolf, M. Das Erleben von Arbeitsintensität und Tätigkeitsspielraum—Entwicklung und Validierung eines Fragebogens zur orientierenden Analyse (FIT) [Perceived work intensity and activity latitude: Development and validation of a questionnaire]. ASU Z. Med. Prävent. 2000, 44, 129–139. [Google Scholar] [CrossRef]
- Sandoval-Reyes, J.; Acosta-Prado, J.C.; Sanchís-Pedregosa, C. Relationship Amongst Technology Use, Work Overload, and Psychological Detachment from Work. Int. J. Environ. Res. Public Health 2019, 16, 4602. [Google Scholar] [CrossRef] [Green Version]
- Chesley, N. Information and communication technology use, work intensification and employee strain and distress. Work Employ. Soc. 2014, 28, 589–610. [Google Scholar] [CrossRef]
- Dragano, N.; Lunau, T. Technostress at work and mental health: Concepts and research results. Curr. Opin. Psychiatry 2020, 33, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, H.-F.; Shannon, S.E. Three approaches to qualitative content analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988; ISBN 9780805802832. [Google Scholar]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- Eurostat. Employed Women Being in Managerial Positions by Age. Available online: https://ec.europa.eu/eurostat/databrowser/view/tqoe1c2/default/table (accessed on 27 May 2021).
- Holst, E.; Friedrich, M. Führungskräfte-Monitor 2017: Update 1995–2015. [Manager Monitor 2017. Update 1995–2015]; DIW Berlin Deutsches Institut für Wirtschaftsforschung: Berlin, Germany, 2017; ISBN 9783946417132. [Google Scholar]
- Bürgel Wirtschaftsinformationen GmbH & Co. KG. Führungspositionen in Deutschland [Management Positions in Germany]. Available online: https://www.crifbuergel.de/pr-events/studien-und-fachartikel/2015/may/07/fuehrungspositionen-in-deutschland/ (accessed on 27 May 2021).
- Eurofound. Fifth European Working Conditions Survey. Publications Office of the European Union: Luxembourg, 2012. Available online: https://op.europa.eu/en/publication-detail/-/publication/29b6dc38-0107-49ae-a22b-8a1415b3c73e/language-en (accessed on 27 May 2021).
- Zeike, S.; Choi, K.-E.; Lindert, L.; Pfaff, H. Managers’ Well-Being in the Digital Era: Is it Associated with Perceived Choice Overload and Pressure from Digitalization? An Exploratory Study. Int. J. Environ. Res. Public Health 2019, 16, 1746. [Google Scholar] [CrossRef] [Green Version]
- Fiedler, S.; Pfaff, H.; Soellner, R.; Pförtner, T.-K. Exploring the Association Between Health Literacy and Psychological Well-Being Among Industry Managers in Germany. J. Occup. Environ. Med. 2018, 60, 743–753. [Google Scholar] [CrossRef] [PubMed]
- Dillman, D.A. Mail and Telephone Surveys: The Total Design Method; Wiley: New York, NY, USA, 1978; ISBN 0471215554. [Google Scholar]
- Anseel, F.; Lievens, F.; Schollaert, E.; Choragwicka, B. Response Rates in Organizational Science, 1995–2008: A Meta-analytic Review and Guidelines for Survey Researchers. J. Bus. Psychol. 2010, 25, 335–349. [Google Scholar] [CrossRef] [Green Version]
- Babitsch, B.; Gohl, D.; von Lengerke, T. Re-revisiting Andersen’s Behavioral Model of Health Services Use: A systematic review of studies from 1998–2011. Psychosoc. Med. 2012, 9, Doc11. [Google Scholar] [CrossRef]
| Variable | n | Item | Distribution | % | ||
|---|---|---|---|---|---|---|
| Sociodemographic Characteristics | ||||||
| Age Group (yrs) | 178 | 100 | ||||
| 25–44 | 26 | 14.6 | ||||
| 45–64 | 150 | 84.3 | ||||
| n. s. | 2 | 1.1 | ||||
| Gender | 173 | 100 | ||||
| Female | 57 | 32.9 | ||||
| Male | 116 | 67.1 | ||||
| Management Level | 178 | 100 | ||||
| Top | 39 | 21.9 | ||||
| Middle | 116 | 65.2 | ||||
| Low | 19 | 10.7 | ||||
| n. s. | 4 | 2.2 | ||||
| n (%) | Mean | SD | Minimum | Maximum | Median | |
| Managerial Experience (yrs) | 178 (100) | 11.94 | 6.67 | 1 | 35 | 11.00 |
| Health- and Work-Related Characteristics | ||||||
| n (%) | Mean | SD | Minimum | Maximum | Median | |
| Wellbeing | 174 (100) | 59.98 | 20.99 | 0 | 100 | 64.0 |
| Low | 56 (32.2) | |||||
| High | 118 (67.8) | |||||
| Health Status | 175 (100) | 3.56 | 0.86 | 1 | 5 | 4 |
| Work Intensity | 179 (100) | 3.15 | 0.4 | 2 | 4 | 3.14 |
| Model 1 (Crude Model) | Model 2 | Model 3(Full Model) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables (n = 160) | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p |
| Age (refcat: 45–64 yrs) | 0.527 | [0.206, 1.346] | 0.181 | 0.528 | [0.206, 1.348] | 0.181 | 0.437 | [0.166, 1.153] | 0.094 |
| Gender (refcat: male) | 1.700 | [0.859, 3.366] | 0.128 | 1.718 | [0.866, 3.411] | 0.122 | 1.528 | [0.752, 3.104] | 0.241 |
| Management level (refcat: low) | 0.828 | [0.378, 1.811] | 0.636 | 0.820 | [0.374, 1.797] | 0.621 | 0.742 | [0.330, 1.668] | 0.471 |
| Wellbeing (refcat: low) | 1.163 | [0.584, 2.313] | 0.668 | 0.905 | [0.427, 1.918] | 0.794 | |||
| Workload relief through digital tools (refcat: no) | 2.838 | [1.422, 5.661] | 0.003 * | ||||||
| Work intensity | 0.843 | [0.353, 2.013] | 0.700 | ||||||
| Goodness of fit | Model 1 | Model 2 | Model 3 | ||||||
| Cox–Snell pseudo-R2 | 0.025 | 0.026 | 0.081 | ||||||
| Nagelkerke’s pseudo-R2 | 0.034 | 0.035 | 0.108 | ||||||
| Category | % (n) | Example Responses |
|---|---|---|
| Suggested improvements for more health-promoting working conditions | 100 (194) | |
| Work facilities, commute, and HPM offers | 37.1 (72) | Fixed workplaces; better (open-plan) office design—more quiet zones, better indoor climate, more foliage plants; less traveling; more sports and exercise offers (during working hours); significant improvement of culinary selection for healthier nutrition; water dispensers instead of coffee machines |
| Workload and time | 32.0 (62) | High workload, too many simultaneous topics; less stress and pressure; reduction in complexity and ambiguity; clearer prioritization; conflicting schedules; less work compression on each individual; less but better prepared information; breaks and rest periods are still often considered a weakness…; better work–life balance for managers, too; respect private times; no calls and mails after 6 p.m. |
| Leadership, teamwork, and social support | 17.5 (34) | Rules for teamwork; more appreciation; more respect towards staff; positive, motivating, inspiring atmosphere—even in hard times; more face-to-face meetings and less virtual teamwork; interaction with colleagues; selfishness of individuals should be fought instead of encouraged; change in management style of some colleagues |
| Corporate culture | 10.3 (20) | The company should develop a culture in which employee health is a real value; the human being must be emphasized in the company again; improve feedback culture; rejuvenation of the organization; more digitalization in the ENTIRE company, not only in parts; we do a lot regarding overtime compensation for employees, for managers there are no comparable compensations. In my opinion, it always comes across as somewhat strange when managers say to their manager, “But I have worked quite a lot of overtime now…”, that is not our corporate culture |
| Working conditions are ideal | 3.1 (6) | Nothing. It is already ideal; I think the shortage rather lies within me, less within the employer/working conditions; There are few things to improve regarding working conditions. I should improve my mindfulness, awareness, and health orientation (taking breaks, eating, managing my energy)… |
| Barriers to HPM participation CQ | 100 (97) | |
| Conflicting schedules and daily workload | 25.8 (25) | Too many other things to do; scheduling conflicts; constant need to prioritize daily business and special tasks; high workload |
| Lack of time | 24.7 (24) | TIME!; time shortage; time resources not available |
| Lack of specific information and knowledge | 24.7 (24) | There is a lack of targeted addressing and targeted appointment offers; Appointments + offers not known, no communication about offers across locations; I did not know this existed |
| No perceived demand | 12.4 (12) | Need not recognized |
| Other | 12.4 (12) | I wonder, whether the real working conditions in the company allow an implementation of what has been learned; no offer at the location or in working vicinity |
| Previous HPM participation CQ | 100 (115) | |
| Resilience, mindfulness, and stress relief | 31.3 (36) | Resilience workshop; mindfulness workshop; work–life balance seminar; stress management seminar |
| Physical fitness and health at work | 25.5 (29) | Mobile fitness coach; back training; company fitness center; company health days |
| Medical measures and occupational safety | 20.9 (24) | Medical checkup at the workplace; vaccinations; ergonomics and safety training |
| Leadership | 12.2 (14) | Healthy leadership; virtual leadership; leading in agile environments |
| Other | 10.5 (12) | Personal coaching; coaching for business unit; online training |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schubin, K.; Pfaff, H.; Zeike, S. How Managers Perceive and (Do Not) Participate in Health Promotion Measures—Results from a Cross-Sectional Mixed-Methods Survey in a Large ICT Company. Int. J. Environ. Res. Public Health 2021, 18, 9708. https://doi.org/10.3390/ijerph18189708
Schubin K, Pfaff H, Zeike S. How Managers Perceive and (Do Not) Participate in Health Promotion Measures—Results from a Cross-Sectional Mixed-Methods Survey in a Large ICT Company. International Journal of Environmental Research and Public Health. 2021; 18(18):9708. https://doi.org/10.3390/ijerph18189708
Chicago/Turabian StyleSchubin, Kristina, Holger Pfaff, and Sabrina Zeike. 2021. "How Managers Perceive and (Do Not) Participate in Health Promotion Measures—Results from a Cross-Sectional Mixed-Methods Survey in a Large ICT Company" International Journal of Environmental Research and Public Health 18, no. 18: 9708. https://doi.org/10.3390/ijerph18189708
APA StyleSchubin, K., Pfaff, H., & Zeike, S. (2021). How Managers Perceive and (Do Not) Participate in Health Promotion Measures—Results from a Cross-Sectional Mixed-Methods Survey in a Large ICT Company. International Journal of Environmental Research and Public Health, 18(18), 9708. https://doi.org/10.3390/ijerph18189708







