Postcoital Vaginal Perforation and Evisceration in Women with No Prior Pelvic Surgery: Laparoscopic Management and Systematic Review of the Literature
Abstract
1. Introduction
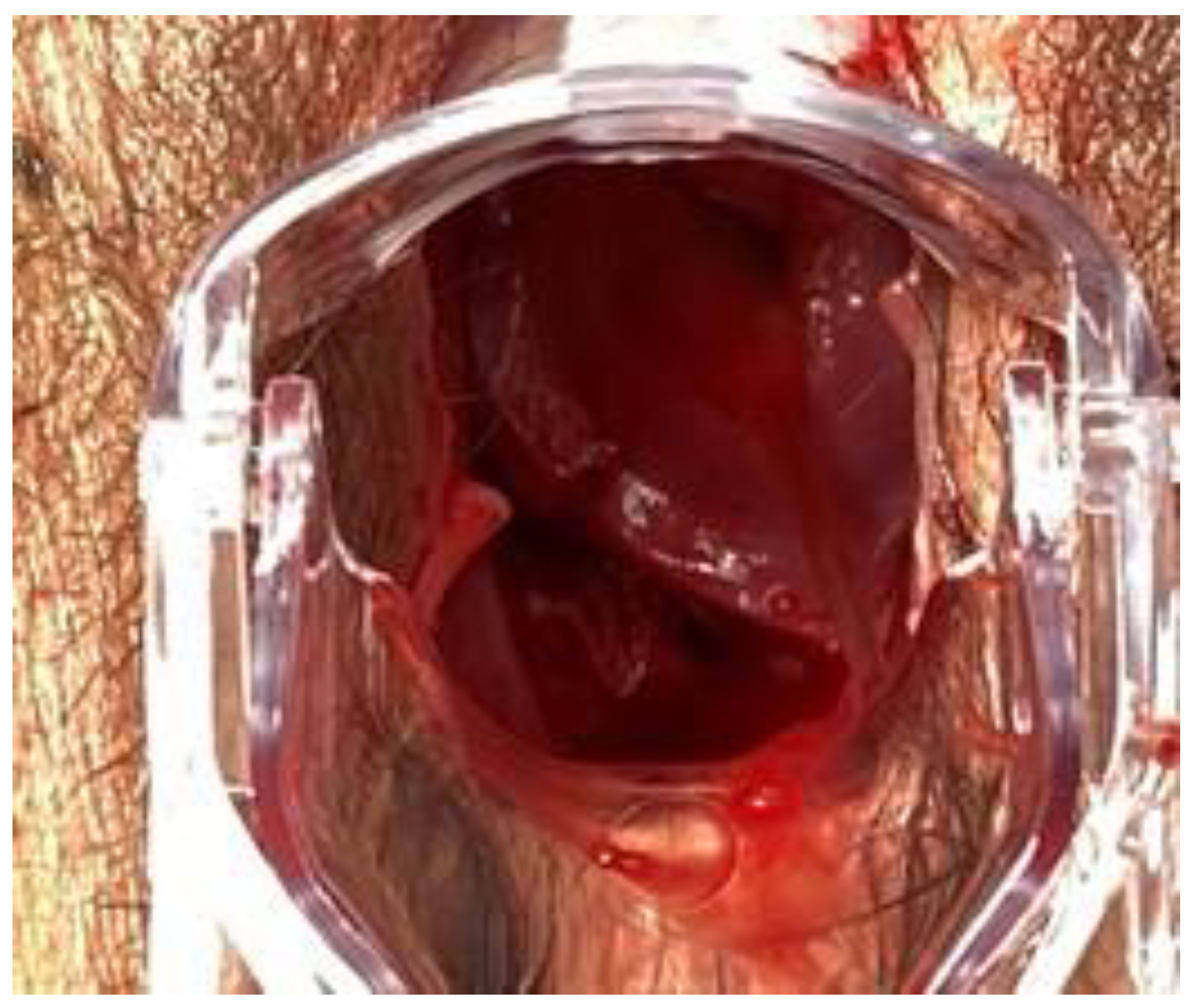
2. Case
3. Materials and Methods
3.1. Eligibility Criteria
3.2. Information Sources
3.3. Study Selection
3.4. Data Extraction
3.5. Assessment of Methodological Quality
3.6. Data Analysis
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Croak, A.J.; Gebhart, J.B.; Klingele, C.J.; Schroeder, G.; Lee, R.A.; Podratz, K.C. Characteristics of Patients With Vaginal Rupture and Evisceration. Obstet. Gynecol. 2004, 103, 572–576. [Google Scholar] [CrossRef] [PubMed]
- Padoa, A.; Fishman, N.G.; Tsviban, A.; Smorgick, N. Vaginal postcoital injuries requiring surgical intervention: A case series and literature review. Int. J. Impot. Res. 2021, 33, 110–117. [Google Scholar] [CrossRef]
- Symeonidis, N.; Ballas, K.; Micha, A.; Psarras, K.; Pavlidis, T. Consensual Intercourse Resulting in an Extensive Rectovaginal Tear: An Extremely Rare Occurrence. J. Sex. Med. 2015, 12, 572–575. [Google Scholar] [CrossRef]
- King, B.M. Average-Size Erect Penis: Fiction, Fact, and the Need for Counseling. J. Sex Marital Ther. 2021, 47, 80–89. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetcu, R. Joanna Briggs Institute Reviewer’s Manual; The Joanna Briggs Institute: Adelaide, Australia, 2017. [Google Scholar]
- Hoffman, R.J.; Ganti, S. Vaginal laceration and perforation resulting from first coitus. Pediatr. Emerg. Care 2001, 17, 113–114. [Google Scholar] [CrossRef] [PubMed]
- Manchanda, R.; Refaie, A. Acute pneumoperitoneum following coitus. Can. J. Emerg. Med. 2005, 7, 51–53. [Google Scholar] [CrossRef]
- Ernest, A.; Emmanuel, M.; Gregory, K. Post-coital posterior fornix perforation with vaginal evisceration. BMC Women’s Health 2014, 14, 141. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jeng, C.-J.; Wang, L.-R. Vaginal Laceration and Hemorrhagic Shock during Consensual Sexual Intercourse. J. Sex Marital Ther. 2007, 33, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Lal, P.; Mohan, P.; Sharma, R.; Sehgal, A.; Aggarwal, A. Postcoital vaginal laceration in a patient presenting with signs of small bowel perforation: Report of a case. Surg. Today 2001, 31, 466–467. [Google Scholar] [CrossRef]
- Austin, J.M.; Cooksey, C.M.; Minikel, L.L.; Zaritsky, E.F. Postcoital Vaginal Rupture in a Young Woman with No Prior Pelvic Surgery. J. Sex. Med. 2013, 10, 2121–2124. [Google Scholar] [CrossRef]
- Cohen, A.; Ulrich, A.; Semenyuk, N. A Laparoscopic Approach to Postcoital Vaginal Perforation in an Adolescent with Peritonitis and Hypovolemic Shock. J. Pediatric Adolesc. Gynecol. 2020, 33, 594–598. [Google Scholar] [CrossRef]
- Fletcher, H.; Bambury, I.; Williams, M. Post-coital posterior fornix perforation with peritonitis and haemoperitoneum. Int. J. Surg. Case Rep. 2013, 4, 153–155. [Google Scholar] [CrossRef][Green Version]
- Usifo, F.; Sharma, R.; MacRae, R.; Hargreaves, C.; Swinhoe, J.R. Posterior vaginal fornix rupture and haemoperitoneum following sexual intercourse. J. Obstet. Gynaecol. 2006, 26, 482–483. [Google Scholar] [CrossRef] [PubMed]
- Khosla, A.H.; Singhal, S. Coital tear: A rare cause of secondary peritonitis. Aust. N. Z. J. Obstet. Gynaecol. 1997, 37, 243–244. [Google Scholar] [CrossRef]
- Sivalingam, N.; Rajesvaran, D. Coital injury requiring internal iliac artery ligation. Singap. Med. J. 1996, 37, 547–548. [Google Scholar]
- Bhagat, M. Coital injury presenting in a 13 year old as abdominal pain and vaginal bleeding. Pediatric Emerg. Care 1996, 12, 354–355. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, B.E.; Murphy, W.M. The pains of love: Hemoperitoneum following sexual intercourse. JAMA 1986, 255, 1708–1709. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.W.; Buckley, C.J. Traumatic Pneumoperitoneum after Vaginal Intercourse. Pediatric Emerg. Care 2020, 36, e301–e303. [Google Scholar] [CrossRef] [PubMed]
- George, A.; Aziz, O.; Shah, A.; Baxter, S. Acute abdominal pain in a 16-year-old woman: The pitfalls of sexual history. Br. J. Hosp. Med. 2007, 68, 106–107. [Google Scholar] [CrossRef]
- Lask, S. Perforation of Posterior Fornix and Pouch of Douglas during Coitus. BMJ 1948, 1, 786. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cunningham, F.G. William’s Obstetrics, 22nd ed.; McGraw Hill Professional: New York, NY, USA, 2005; p. 122. [Google Scholar]
- Stabile, G.; Zinicola, G.; Romano, F.; Buonomo, F.; Mangino, F.P.; Ricci, G. Management of Non-Tubal Ectopic Pregnancies: A Single Center Experience. Diagnostics 2020, 10, 652. [Google Scholar] [CrossRef] [PubMed]
- Romano, F.; Sartore, A.; Mordeglia, D.; Di Lorenzo, G.; Stabile, G.; Ricci, G. Laparoscopic monolateral suspension for vaginal vault prolapse: A report of an exit surgical strategy during sacralcolpopexy. BMC Surg. 2020, 20, 1–5. [Google Scholar] [CrossRef] [PubMed]




| Author (Year) | Patient Age | Risk Factors | Coitus Position | Presentation | Side | Hemoperitoneum (mL) | Suture Type | Treatment | Surgeon |
|---|---|---|---|---|---|---|---|---|---|
| Hoffman R.J. et al. (2001) [7] | 14 | First coitus, Young Age | Dorsal Decubitus | Perforation | PF | Absent | NA | Laparoscopic | GS |
| Manchanda R. et al. (2005) [8] | 16 | Young age | NA | Perforation | PF | Absent | interrupted Vycril | Laparoscopic | Gyn |
| Ernest A. et al. (2014) [9] | 28 | NA | NA | Evisceration | PF | Absent | 2-0 chromic catgut | Laparotomic | GS |
| Jeng C. et al. (2007) [10] | 30 | First coitus, Genitalia Discrepancy | Dorsal Decubitus | Perforation | PF | Absent | 3-0 delayed absordable | Vaginal | Gyn |
| 20 | First coitus | Dorsal Decubitus | Perforation | PF | Absent | 3-0 delayed absordable | Vaginal | Gyn | |
| 24 | First coitus, Genitalia Discrepance, Retroversus uterus | Dorsal Decubitus | Perforation | PF | Absent | 3-0 delayed absordable | Vaginal | Gyn | |
| Lal P. et al. (2001) [11] | 45 | NA | NA | Perforation | PF | Absent | interrupted 3-0 Vycril | Laparotomic | Gyn |
| Austin J.M. et al. (2012) [12] | 23 | Genitalia Discrepancy, Extreme force, Abstinence (1 year) | Prone and supine | Perforation | PF | Absent | 0 Polysorb-Covidien (vag)+ 2-0 V-Loc (LPS) | Combined (laparoscopic+vaginal) | Gyn |
| Cohen A. et al. (2020) [13] | 18 | Young Age | Lateral Supine | Perforation | PF | Present (100) | 3-0 Vloc | Laparoscopic | Gyn |
| Fletcher H. et al. (2012) [14] | 15 | Young Age | Dorsal Decubitus | Perforation | PF | Present (100) | 0 polyglactin | Laparotomic | Gyn |
| 24 | Multiparity | Dorsal Decubitus | Perforation | PF | Present (900) | NA | Combined (laparotomic+vaginal) | Gyn | |
| Usifo F. et al. (2006) [15] | 13 | Young age | Prone | Perforation | PF | Present (1500) | interrupted polysorb | Laparotomic | GS |
| Khosla A.H. et al. (1997) [16] | 16 | First coitus, Young Age | NA | Perforation | PF | Present (150) | NA | Laparotomc | Gyn |
| Sivalingam N. et al. (1996) [17] | 21 | First coitus | Dorsal Decubitus | Perforation | PF | Absent | interrupted cutgut (vag)+Vicryl 0 per AII (LPT) | Combined (laparotomic + vaginal) | Gyn |
| Baghat M. (1996) [18] | 13 | First coitus, Young Age | NA | Perforation | PF | Present (600) | NA | Laparotomic | GS |
| Ferrara B.E. et al. (1986) [19] | 36 | TC Section | NA | Perforation | PF | Present (1200) | NA | Laparotomic | GS |
| Thomas J.W. et al. (2020) [20] | 16 | Young Age, “rough sex” | NA | Perforation | PF | Absent | NA | Laparoscopic | Gyn |
| George A. et al. (2007) [21] | 16 | Young age | NA | Perforation | PF | Absent | No suture | Laparotomic | GS |
| Results | |||
|---|---|---|---|
| N | % | ||
| AVERAGE AGE | 21.5 | ||
| <25 y | 14/18 | 77.7 | |
| >25 y | 4/18 | 22.2 | |
| VIRGINAL STATUS | 7/18 | 38.8 | |
| POSITION | Dorsal decubitus | 7/18 | 38.8 |
| VAGINAL PERFORATION | Without intestinal prolapse | 17/18 | 94.4 |
| Whit intesinal prolapse | 1/18 | 5.6 | |
| VAGINAL FORNIX | Posterior | 18/18 | 100 |
| SIDE OF PERFORATION | Right | 7/18 | 38.8 |
| Left | 0/10 | 0 | |
| NA | 11/18 | 61.2 | |
| HEMOPERITONEUM | Yes | 7/18 | 38.8 |
| No | 11/18 | 61.2 | |
| SUTURE | Natural | 2/18 | 11.1 |
| Synthetic | 9/18 | 50 | |
| NA | 6/18 | 33.3 | |
| SURGICAL APPROACH | Laparoscopy | 3/18 | 16.6 |
| Laparotomy | 8/18 | 44.4 | |
| Vaginal | 3/18 | 16.6 | |
| Laparotomy + vaginal | 2/18 | 11.1 | |
| Laparoscopy + vaginal | 1/18 | 5.5 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stabile, G.; Mordeglia, D.; Romano, F.; Carlucci, S.; Mangino, F.P.; Nappi, L.; Sorrentino, F.; De Manzini, N.; Ricci, G. Postcoital Vaginal Perforation and Evisceration in Women with No Prior Pelvic Surgery: Laparoscopic Management and Systematic Review of the Literature. Int. J. Environ. Res. Public Health 2021, 18, 9746. https://doi.org/10.3390/ijerph18189746
Stabile G, Mordeglia D, Romano F, Carlucci S, Mangino FP, Nappi L, Sorrentino F, De Manzini N, Ricci G. Postcoital Vaginal Perforation and Evisceration in Women with No Prior Pelvic Surgery: Laparoscopic Management and Systematic Review of the Literature. International Journal of Environmental Research and Public Health. 2021; 18(18):9746. https://doi.org/10.3390/ijerph18189746
Chicago/Turabian StyleStabile, Guglielmo, Denise Mordeglia, Federico Romano, Stefania Carlucci, Francesco Paolo Mangino, Luigi Nappi, Felice Sorrentino, Nicolò De Manzini, and Giuseppe Ricci. 2021. "Postcoital Vaginal Perforation and Evisceration in Women with No Prior Pelvic Surgery: Laparoscopic Management and Systematic Review of the Literature" International Journal of Environmental Research and Public Health 18, no. 18: 9746. https://doi.org/10.3390/ijerph18189746
APA StyleStabile, G., Mordeglia, D., Romano, F., Carlucci, S., Mangino, F. P., Nappi, L., Sorrentino, F., De Manzini, N., & Ricci, G. (2021). Postcoital Vaginal Perforation and Evisceration in Women with No Prior Pelvic Surgery: Laparoscopic Management and Systematic Review of the Literature. International Journal of Environmental Research and Public Health, 18(18), 9746. https://doi.org/10.3390/ijerph18189746









