Housing Poverty and Healthy Aging in China: Evidence from the China Health and Retirement Longitudinal Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data
2.2. Healthy Aging: CHAI Score
- Systolic blood pressure (SBP): the average value of SBP measured three times at 45 s intervals and then grouped into three categories: 0 = ≤120 mmHg, 1 = 120–140 mmHg, and 2 = >140 mmHg. We designated respondents diagnosed with hypertension or taking anti-hypertensive medications as the unhealthiest group (score = 2) [2,51];
- Pulmonary function: the average of expiratory peak flow (L/min) measured three times in a standing position, with gender-specific terciles grouped into three categories (for males: 0 = ≥320 L/min, 1 = 193–320 L/min, and 2 = ≤193 L/min; for females: 0 = ≥225 L/min, 1 = 153–225 L/min, and 2 = ≤153 L/min) [2,51]. We designated respondents diagnosed with pulmonary disease as the unhealthiest group (score = 2);
- Cognitive function: as evaluated by the Telephone Interview for Cognitive Status (TICS), whose validity has been confirmed in different populations, including Chinese [54,55]. CHARLS included two cognition measures: episodic memory and mental intactness. The former was based on respondent ability to immediately repeat back in any order 10 Chinese nouns directly read to them (immediate word recall) and then recall the same list 4 min later (delayed recall). By averaging the number of correct answers for both recall types, we generated a 0 to 10 score for aggregate word recall. The second measure, mental intactness, was based on respondent ability to name the date and day of the week, redraw a formerly shown photo, and perform up to five serial 7 subtractions from 100 [55,56]. First, following Lei and Liu [56], we counted each correct answer to generate a 1 to 11 mental intactness score that reflects fluid and crystallized cognition [57]. Then, similar to Luo et al. [55], we summed the mental intactness and episodic memory scores to generate a 0 to 21 total cognition score, which we then classified into the three categories proposed by Wu et al. [51]: for males: 0 = ≥19, 1 = 14–19, and 2 = ≤14; for females: 0 = ≥17, 1 = 10–17, and 2 = ≤10;
- Kidney function: after evaluating individual kidney function based on estimated glomerular filtration rate (eGFR) [58,59], we categorized the eGFR into three groups based on clinically relevant cutoffs taken [58]: 0 = ≥90 mL/min per 1.73 m2, 1 = 60–90 mL/min per 1.73 m2 and 2 = <60 mL/min per 1.73 m2;
2.3. Housing Poverty Variables
2.4. Control Variables
2.5. Methods
2.5.1. Psychometric Proprieties Analysis
2.5.2. Ordinary Least Squares (OLS) Estimation
2.5.3. UQR
2.5.4. BO Decomposition
2.5.5. Recentered Influence Function Regression (RIFR) Decomposition
3. Results
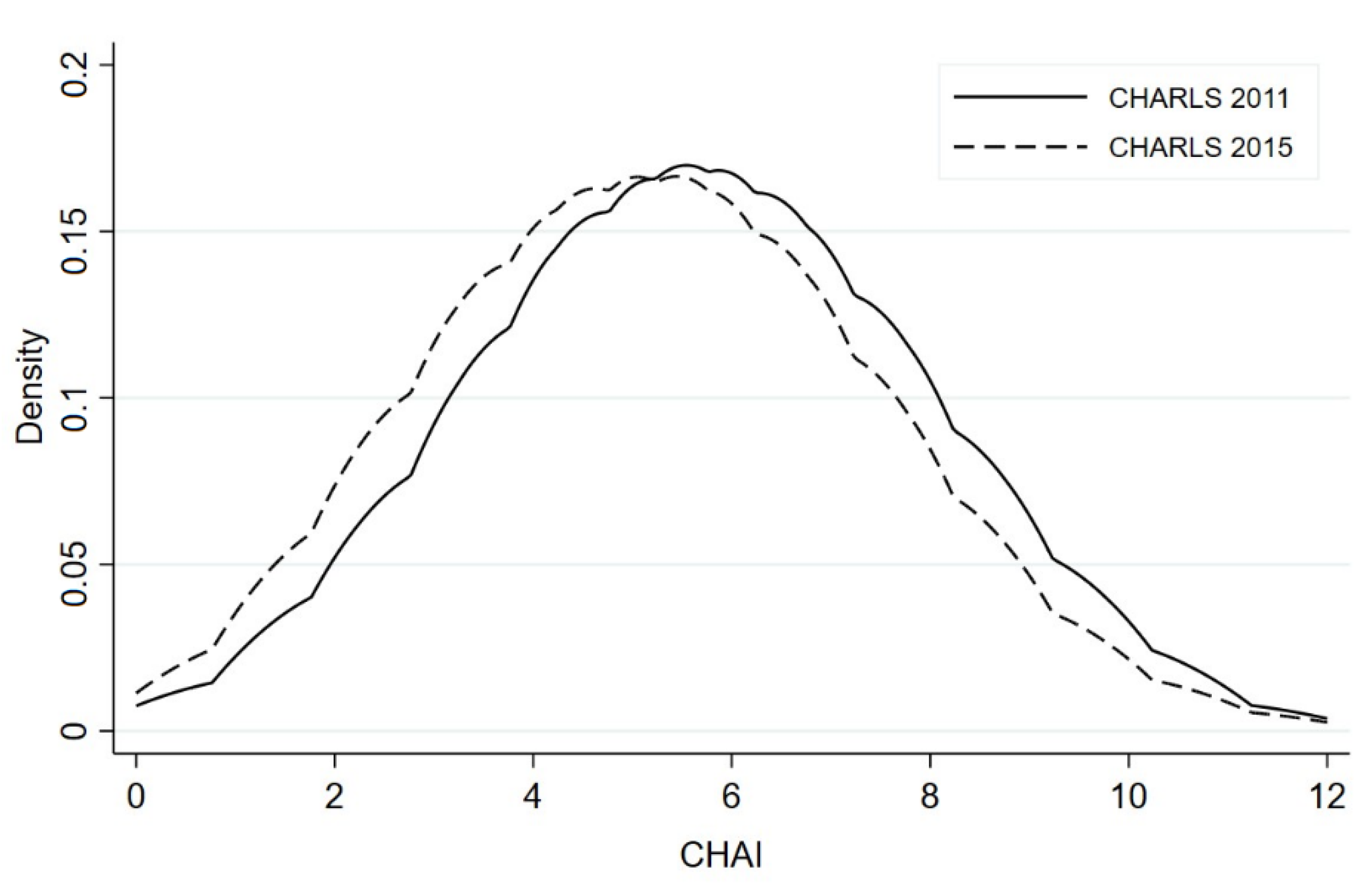
3.1. Descriptive Statistics
3.2. Analysis of Psychometric Properties
3.3. Impact of Housing Poverty on Healthy Aging
3.3.1. OLS Estimates
3.3.2. RIFR Estimates
3.4. CHAI Score Differences between the 2011 and 2015 CHARLS Waves
3.4.1. BO Decomposition Estimates
3.4.2. The RIFR Decomposition Estimates
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Acceptability and Internal Consistency | |||||||
|---|---|---|---|---|---|---|---|
| Fully Computable (%) | Mean | Median | SD | Skewness | Observed Min.–Max. | ITCC (Cronbach’s α) | |
| CHAI score | 100.0 | 5.41 | 5.00 | 2.06 | 0.11 | 0–12 | 0.71 |
| 1. Systolic blood pressure | 100.0 | 1.09 | 1.00 | 0.80 | −0.16 | 0–2 | 0.78 |
| 2. Pulmonary function | 100.0 | 0.85 | 1.00 | 0.80 | 0.28 | 0–2 | 0.78 |
| 3. Fasting glucose | 100.0 | 0.90 | 1.00 | 0.79 | 0.18 | 0–2 | 0.79 |
| 4. Cognitive function | 100.0 | 0.58 | 0.00 | 0.69 | 0.78 | 0–2 | 0.71 |
| 5. Kidney function | 100.0 | 0.93 | 1.00 | 0.45 | −0.30 | 0–2 | 0.71 |
| 6. High-sensitivity C-reactive protein | 100.0 | 1.07 | 1.00 | 0.81 | −0.12 | 0–2 | 0.70 |
| Convergent validity | |||||||
| Spearman’s rank correlation coefficient | |||||||
| CHAI score and Self-reported health (SRH) | 0.61 *** | ||||||
| Discriminative validity | |||||||
| Mean | SD | p-value | |||||
| Age | 0.0001 | ||||||
| 60–64 years | 4.71 | 1.93 | |||||
| 65–69 years | 5.24 | 1.85 | |||||
| 70–74 years | 5.96 | 2.00 | |||||
| 75–79 years | 6.55 | 1.90 | |||||
| 80 years and over | 7.34 | 1.83 | |||||
| Gender | 0.0001 | ||||||
| Women | 5.32 | 2.14 | |||||
| Men | 5.52 | 2.01 | |||||
| Marital status | 0.0001 | ||||||
| Others | 6.16 | 2.11 | |||||
| Married | 5.21 | 2.02 | |||||
| Education | 0.0001 | ||||||
| No education | 5.83 | 2.06 | |||||
| Primary school | 5.37 | 2.02 | |||||
| Middle school | 4.52 | 1.93 | |||||
| High school or higher | 4.73 | 1.95 | |||||
| Precision | |||||||
| Standard error of measurement (SEM) | 0.02 | ||||||
| Variable | OLS | ||
|---|---|---|---|
| Housing Poverty | (1) | (2) | (3) |
| Housing quality poverty | 0.099 ** | ||
| (0.044) | |||
| Housing quantity poverty | 0.043 | ||
| (0.041) | |||
| Housing quality–quantity poverty | 0.096 * | ||
| (0.053) | |||
| Age group | |||
| 65–69 | 0.487 *** | 0.492 *** | 0.490 *** |
| (0.049) | (0.049) | (0.049) | |
| 70–74 | 1.113 *** | 1.117 *** | 1.115 *** |
| (0.056) | (0.056) | (0.056) | |
| 75–79 | 1.806 *** | 1.808 *** | 1.806 *** |
| (0.066) | (0.066) | (0.066) | |
| ≥80 | 2.412 *** | 2.412 *** | 2.412 *** |
| (0.087) | (0.087) | (0.087) | |
| Male | 0.491 *** | 0.491 *** | 0.491 *** |
| (0.047) | (0.047) | (0.047) | |
| Married | −0.394 *** | −0.401 *** | −0.404 *** |
| (0.050) | (0.051) | (0.051) | |
| Rural resident | 0.032 | 0.006 | 0.015 |
| (0.047) | (0.046) | (0.046) | |
| Education: primary school | −0.388 *** | −0.392 *** | −0.389 *** |
| (0.050) | (0.050) | (0.050) | |
| Education: middle school | −0.917 *** | −0.926 *** | −0.921 *** |
| (0.063) | (0.063) | (0.063) | |
| Education: high school or higher | −0.876 *** | −0.888 *** | −0.882 *** |
| (0.081) | (0.081) | (0.081) | |
| Chronic disease | 0.362 *** | 0.364 *** | 0.363 *** |
| (0.054) | (0.054) | (0.054) | |
| Overweight (BMI ≥ 24 kg/m2) | 0.691 *** | 0.687 *** | 0.690 *** |
| (0.042) | (0.041) | (0.042) | |
| Smoking | 0.148 *** | 0.153 *** | 0.151 *** |
| (0.050) | (0.050) | (0.050) | |
| Social activity | −0.225 *** | −0.227 *** | −0.226 *** |
| (0.040) | (0.040) | (0.040) | |
| Pension | −0.195 *** | −0.195 *** | −0.194 *** |
| (0.043) | (0.043) | (0.043) | |
| Log (HH expenditure per capita) | −0.112 *** | −0.115 *** | −0.112 *** |
| (0.025) | (0.025) | (0.025) | |
| Year dummy | YES | YES | YES |
| Province dummy | YES | YES | YES |
| Observations | 8839 | 8839 | 8839 |
| Adj. R2 | 0.253 | 0.253 | 0.253 |
| Variable | 25th | 50th | 75th | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Housing Poverty | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) |
| Housing quality poverty | 0.124 ** | 0.033 ** | 0.141 ** | ||||||
| (0.052) | (0.048) | (0.060) | |||||||
| Housing quantity poverty | 0.131 *** | 0.005 | 0.060 | ||||||
| (0.049) | (0.046) | (0.057) | |||||||
| Housing quality–quantity poverty | 0.116 * | 0.037 * | 0.138 * | ||||||
| (0.063) | (0.059) | (0.073) | |||||||
| Age group | |||||||||
| 65–69 | 0.467 *** | 0.476 *** | 0.470 *** | 0.457 *** | 0.457 *** | 0.457 *** | 0.390 *** | 0.396 *** | 0.393 *** |
| (0.060) | (0.060) | (0.060) | (0.056) | (0.056) | (0.056) | (0.070) | (0.070) | (0.070) | |
| 70–74 | 0.907 *** | 0.920 *** | 0.910 *** | 1.002 *** | 1.002 *** | 1.003 *** | 1.077 *** | 1.083 *** | 1.080 *** |
| (0.067) | (0.068) | (0.067) | (0.063) | (0.063) | (0.063) | (0.078) | (0.079) | (0.078) | |
| 75–79 | 1.166 *** | 1.172 *** | 1.165 *** | 1.397 *** | 1.396 *** | 1.397 *** | 2.071 *** | 2.072 *** | 2.071 *** |
| (0.080) | (0.080) | (0.080) | (0.074) | (0.074) | (0.074) | (0.093) | (0.093) | (0.093) | |
| ≥80 | 1.353 *** | 1.356 *** | 1.353 *** | 1.718 *** | 1.717 *** | 1.718 *** | 2.689 *** | 2.687 *** | 2.688 *** |
| (0.105) | (0.106) | (0.106) | (0.098) | (0.098) | (0.098) | (0.122) | (0.123) | (0.123) | |
| Male | 0.543 *** | 0.540 *** | 0.542 *** | 0.494 *** | 0.494 *** | 0.494 *** | 0.396 *** | 0.395 *** | 0.396 *** |
| (0.057) | (0.057) | (0.057) | (0.053) | (0.053) | (0.053) | (0.066) | (0.066) | (0.066) | |
| Married | −0.293 *** | −0.310 *** | −0.305 *** | −0.372 *** | −0.372 *** | −0.376 *** | −0.403 *** | −0.413 *** | −0.418 *** |
| (0.061) | (0.061) | (0.061) | (0.056) | (0.057) | (0.057) | (0.071) | (0.071) | (0.071) | |
| Rural resident | 0.024 | 0.010 | 0.003 | 0.087 * | 0.080 | 0.082 * | 0.018 | 0.053 | 0.042 |
| (0.054) | (0.052) | (0.052) | (0.050) | (0.049) | (0.049) | (0.062) | (0.061) | (0.061) | |
| Education: primary school | −0.374 *** | −0.378 *** | −0.376 *** | −0.344 *** | −0.346 *** | −0.345 *** | −0.452 *** | −0.459 *** | −0.454 *** |
| (0.060) | (0.060) | (0.060) | (0.056) | (0.056) | (0.056) | (0.070) | (0.070) | (0.070) | |
| Education: middle school | −0.984 *** | −0.992 *** | −0.989 *** | −1.066 *** | −1.069 *** | −1.067 *** | −0.788 *** | −0.799 *** | −0.794 *** |
| (0.074) | (0.074) | (0.074) | (0.069) | (0.069) | (0.069) | (0.087) | (0.086) | (0.086) | |
| Education: high school or higher | −0.943 *** | −0.952 *** | −0.951 *** | −0.881 *** | −0.885 *** | −0.882 *** | −0.917 *** | −0.932 *** | −0.925 *** |
| (0.097) | (0.097) | (0.097) | (0.090) | (0.090) | (0.090) | (0.113) | (0.112) | (0.113) | |
| Chronic disease | 0.330 *** | 0.333 *** | 0.331 *** | 0.411 *** | 0.411 *** | 0.411 *** | 0.372 *** | 0.376 *** | 0.374 *** |
| (0.066) | (0.066) | (0.066) | (0.061) | (0.061) | (0.061) | (0.076) | (0.076) | (0.076) | |
| Overweight (BMI ≥ 24 kg/m2) | 0.598 *** | 0.593 *** | 0.597 *** | 0.581 *** | 0.580 *** | 0.581 *** | 0.581 *** | 0.576 *** | 0.580 *** |
| (0.050) | (0.050) | (0.050) | (0.046) | (0.046) | (0.046) | (0.058) | (0.058) | (0.058) | |
| Smoking | 0.092 | 0.099 * | 0.097 | 0.114 ** | 0.116 ** | 0.115 ** | 0.175 ** | 0.184 *** | 0.180 *** |
| (0.060) | (0.060) | (0.060) | (0.056) | (0.056) | (0.056) | (0.070) | (0.070) | (0.070) | |
| Social activity | −0.211 *** | −0.213 *** | −0.213 *** | −0.258 *** | −0.259 *** | −0.259 *** | −0.264 *** | −0.267 *** | −0.266 *** |
| (0.048) | (0.048) | (0.048) | (0.045) | (0.045) | (0.045) | (0.056) | (0.056) | (0.056) | |
| Pension | −0.155 *** | −0.156 *** | −0.155 *** | −0.081 * | −0.081 * | −0.081 * | −0.101 * | −0.102 * | −0.100 * |
| (0.051) | (0.051) | (0.051) | (0.047) | (0.047) | (0.047) | (0.059) | (0.059) | (0.059) | |
| Household expenditure per capita | −0.127 *** | −0.124 *** | −0.128 *** | −0.130 *** | −0.133 *** | −0.130 *** | −0.048 | −0.053 | −0.049 |
| (0.030) | (0.030) | (0.030) | (0.028) | (0.028) | (0.028) | (0.035) | (0.035) | (0.035) | |
| Year dummy | YES | YES | YES | YES | YES | YES | YES | YES | YES |
| Province dummy | YES | YES | YES | YES | YES | YES | YES | YES | YES |
| Observations | 8839 | 8839 | 8839 | 8839 | 8839 | 8839 | 8839 | 8839 | 8839 |
| Adj. R2 | 0.116 | 0.116 | 0.116 | 0.158 | 0.158 | 0.158 | 0.151 | 0.150 | 0.151 |
| Contribution (%) | Contribution (%) | Contribution (%) | ||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| CHAI: CHARLS 2011 | 5.685 *** | 5.685 *** | 5.685 *** | |||
| CHAI: CHARLS 2015 | 5.216 *** | 5.216 *** | 5.216 *** | |||
| Total difference | −0.469 *** | −0.469 *** | −0.469 *** | |||
| Explained part | −0.149 ** | 31.77 | −0.146 ** | 31.13 | −0.149 ** | 31.77 |
| Unexplained part | −0.321 *** | 68.44 | −0.324 *** | 69.08 | −0.321 *** | 68.44 |
| Explained part | ||||||
| Housing quality poverty | −0.012 *** | 8.05 | ||||
| (0.006) | ||||||
| Housing quantity poverty | −0.006 | 4.11 | ||||
| (0.007) | ||||||
| Housing quality–quantity poverty | −0.011 ** | 7.38 | ||||
| (0.007) | ||||||
| Age | −0.048 * | 32.21 | −0.048 * | 32.88 | −0.048 * | 32.21 |
| (0.026) | (0.026) | (0.026) | ||||
| Gender | 0.011 | −7.38 | 0.011 | −7.53 | 0.011 | −7.38 |
| (0.009) | (0.009) | (0.009) | ||||
| Married | −0.009 | 6.04 | −0.009 | 6.16 | −0.010 | 6.71 |
| (0.006) | (0.006) | (0.006) | ||||
| Rural resident | 0.001 | −0.67 | 0.000 | −0.01 | 0.000 | −0.01 |
| (0.002) | (0.002) | (0.002) | ||||
| Education | −0.042 ** | 28.19 | −0.043 ** | 29.45 | −0.042 ** | 28.19 |
| (0.015) | (0.015) | (0.015) | ||||
| Chronic disease | 0.031 *** | −20.81 | 0.031 *** | −21.23 | 0.031 *** | −20.81 |
| (0.007) | (0.007) | (0.007) | ||||
| Overweight (BMI ≥ 24 kg/m2) | 0.037 ** | −24.83 | 0.037 ** | −25.34 | 0.037 ** | −24.83 |
| (0.013) | (0.013) | (0.013) | ||||
| Smoking | 0.002 | −1.34 | 0.002 | −1.37 | 0.002 | −1.34 |
| (0.002) | (0.002) | (0.002) | ||||
| Social activity | −0.007 | 4.70 | −0.007 | 4.79 | −0.007 | 4.70 |
| (0.004) | (0.004) | (0.004) | ||||
| Pension | −0.047 *** | 31.54 | −0.047 *** | 32.19 | −0.047 *** | 31.54 |
| (0.014) | (0.014) | (0.014) | ||||
| Household expenditure per capita | −0.061 ** | 40.94 | −0.063 ** | 43.15 | −0.061 ** | 40.94 |
| (0.020) | (0.020) | (0.020) | ||||
| Province | −0.004 | 2.68 | −0.004 | 2.74 | −0.004 | 2.68 |
| (0.010) | (0.010) | (0.010) |
| 25th | 50th | 75th | |||||||
|---|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | |
| CHAI: CHARLS 2011 | 4.662 *** | 6.144 *** | 7.580 *** | ||||||
| (0.077) | (0.065) | (0.070) | |||||||
| CHAI: CHARLS 2015 | 4.176 *** | 5.627 *** | 7.146 *** | ||||||
| (0.055) | (0.051) | (0.062) | |||||||
| Total difference | −0.486 *** | −0.517 *** | −0.434 *** | ||||||
| (0.095) | (0.082) | (0.093) | |||||||
| Explained part | −0.181 * | −0.181 * | −0.181 * | −0.178 ** | −0.173 ** | −0.180 ** | −0.152 * | −0.142 * | −0.150 * |
| (0.072) | (0.074) | (0.072) | (0.065) | (0.065) | (0.064) | (0.066) | (0.067) | (0.066) | |
| Unexplained part | −0.305 * | −0.305 * | −0.305 * | −0.339 *** | −0.344 *** | −0.337 *** | −0.281 ** | −0.291 ** | −0.284 ** |
| (0.124) | (0.126) | (0.124) | (0.096) | (0.096) | (0.095) | (0.104) | (0.104) | (0.104) | |
| Explained part | |||||||||
| Housing quality poverty | −0.013 ** | −0.025 ** | −0.035 ** | ||||||
| (0.011) | (0.012) | (0.015) | |||||||
| Housing quantity poverty | −0.013 | −0.014 | −0.014 | ||||||
| (0.013) | (0.013) | (0.015) | |||||||
| Housing quality–quantity poverty | −0.013 ** | −0.029 ** | −0.030 ** | ||||||
| (0.011) | (0.012) | (0.014) | |||||||
| Age | −0.032 ** | −0.032 ** | −0.032 ** | −0.045 ** | −0.044 ** | −0.045 ** | −0.057 ** | −0.057 ** | −0.057 ** |
| (0.018) | (0.018) | (0.018) | (0.024) | (0.024) | (0.024) | (0.030) | (0.030) | (0.030) | |
| Gender | 0.011 | 0.011 | 0.011 | 0.002 | 0.003 | 0.002 | 0.008 | 0.008 | 0.008 |
| (0.009) | (0.010) | (0.009) | (0.003) | (0.004) | (0.004) | (0.007) | (0.007) | (0.007) | |
| Married | −0.011 | −0.011 | −0.011 | −0.009 | −0.009 | −0.010 | −0.008 | −0.008 | −0.008 |
| (0.007) | (0.007) | (0.007) | (0.006) | (0.006) | (0.006) | (0.006) | (0.006) | (0.006) | |
| Rural resident | 0.008 | 0.007 | 0.008 | 0.007 | 0.005 | 0.006 | 0.006 | 0.004 | 0.004 |
| (0.006) | (0.006) | (0.006) | (0.006) | (0.005) | (0.005) | (0.006) | (0.005) | (0.005) | |
| Education | −0.038 | −0.039 * | −0.039 | −0.037 * | −0.039 * | −0.037 * | −0.036 * | −0.038 * | −0.037 * |
| (0.020) | (0.020) | (0.020) | (0.018) | (0.018) | (0.018) | (0.017) | (0.017) | (0.017) | |
| Chronic disease | 0.037 ** | 0.037 ** | 0.037 ** | 0.038 *** | 0.038 *** | 0.038 *** | 0.025 * | 0.025 * | 0.025 * |
| (0.012) | (0.012) | (0.012) | (0.010) | (0.011) | (0.010) | (0.011) | (0.011) | (0.011) | |
| Overweight (BMI ≥ 24 kg/m2) | 0.026 * | 0.026 * | 0.026 * | 0.029 * | 0.029 * | 0.029 * | 0.035 * | 0.035 * | 0.035 * |
| (0.011) | (0.011) | (0.011) | (0.012) | (0.012) | (0.012) | (0.014) | (0.014) | (0.014) | |
| Smoking | 0.002 | 0.002 | 0.002 | 0.005 | 0.005 | 0.005 | 0.003 | 0.003 | 0.003 |
| (0.003) | (0.003) | (0.003) | (0.006) | (0.006) | (0.006) | (0.005) | (0.005) | (0.005) | |
| Social activity | −0.009 | −0.009 | −0.009 | −0.009 | −0.009 | −0.009 | −0.009 | −0.009 | −0.009 |
| (0.006) | (0.007) | (0.007) | (0.006) | (0.006) | (0.006) | (0.007) | (0.007) | (0.007) | |
| Pension | −0.061 * | −0.060 | −0.061 * | −0.018 | −0.017 | −0.018 | −0.025 | −0.025 | −0.026 |
| (0.031) | (0.031) | (0.031) | (0.030) | (0.030) | (0.030) | (0.033) | (0.033) | (0.033) | |
| Household expenditure per capita | −0.092 * | −0.092 * | −0.091 * | −0.112 ** | −0.116 *** | −0.109 ** | −0.056 | −0.063 | −0.055 |
| (0.038) | (0.036) | (0.038) | (0.035) | (0.035) | (0.035) | (0.039) | (0.038) | (0.039) | |
| Province | −0.010 | −0.010 | −0.010 | −0.004 | −0.005 | −0.004 | −0.003 | −0.004 | −0.003 |
| (0.026) | (0.026) | (0.026) | (0.022) | (0.023) | (0.023) | (0.019) | (0.019) | (0.019) |
References
- Department of Economic and Social Affairs; United Nations. The Sustainable Development Goals Report 2020; United Nations Statistics Division: New York, NY, USA, 2020. [Google Scholar]
- Nie, P.; Li, Y.; Zhang, N.; Sun, X.; Xin, B.; Wang, Y. The change and correlates of healthy ageing among Chinese older adults: Findings from the China health and retirement longitudinal study. BMC Geriatr. 2021, 21, 78. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Smith, J.P.; Strauss, J. Can China age healthily? Lancet 2014, 384, 723–724. [Google Scholar] [CrossRef] [Green Version]
- Smith, J.P.; Strauss, J.; Zhao, Y. Healthy aging in China. J. Econ. Ageing 2014, 4, 37–43. [Google Scholar] [CrossRef] [Green Version]
- National Bureau of Statistics of China: China Statistical Yearbook 2019; China Statistics Press: Beijing, China, 2020.
- Population Division, Department of Economic and Social Affairs; United Nations. World Population Ageing 2019 (ST/ESA/SER.A/444); United Nations: New York, NY, USA, 2020. [Google Scholar]
- WHO. World Report on Ageing and Health; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- WHO. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health. Final Report of the Commission on Social Determinants of Health; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- WHO. Housing and Health Guidelines; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Katz, L.F.; Kling, J.R.; Liebman, J.B. Moving to opportunity in Boston: Early results of a randomized mobility experiment. Q. J. Econ. 2001, 116, 607–654. [Google Scholar] [CrossRef]
- Kling, J.R.; Liebman, J.B.; Katz, L.F. Experimental analysis of neighborhood effects. Econometrica 2007, 75, 83–119. [Google Scholar] [CrossRef] [Green Version]
- Ludwig, J.; Duncan, G.J.; Gennetian, L.A.; Katz, L.F.; Kessler, R.C.; Kling, J.R.; Sanbonmatsu, L. Long-term neighborhood effects on low-income families: Evidence from Moving to Opportunity. Am. Econ. Rev. 2013, 103, 226–231. [Google Scholar] [CrossRef] [Green Version]
- Angel, S.; Bittschi, B. Housing and Health. Rev. Income Wealth 2019, 65, 495–513. [Google Scholar] [CrossRef]
- Clair, A.; Hughes, A. Housing and health: New evidence using biomarker data. J. Epidemiol. Community Health 2019, 73, 256. [Google Scholar] [CrossRef] [Green Version]
- Marsh, A.; Gordon, D.; Heslop, P.; Pantazis, C. Housing deprivation and health: A longitudinal analysis. Hous. Stud. 2000, 15, 411–428. [Google Scholar] [CrossRef]
- Navarro, C.; Ayala, L.; Labeaga, J.M. Housing deprivation and health status: Evidence from Spain. Empir. Econ. 2010, 38, 555–582. [Google Scholar] [CrossRef] [Green Version]
- Pevalin, D.J.; Taylor, M.P.; Todd, J. The dynamics of unhealthy housing in the UK: A panel data analysis. Hous. Stud. 2008, 23, 679–695. [Google Scholar] [CrossRef]
- Ellaway, A.; Macdonald, L.; Kearns, A. Are housing tenure and car access still associated with health? A repeat cross-sectional study of UK adults over a 13-year period. BMJ Open 2016, 6, e012268. [Google Scholar] [CrossRef] [Green Version]
- Pollack, C.E.; von dem Knesebeck, O.; Siegrist, J. Housing and health in Germany. J. Epidemiol. Community Health 2004, 58, 216. [Google Scholar] [CrossRef] [Green Version]
- Howden-Chapman, P.; Viggers, H.; Chapman, R.; O’Sullivan, K.; Telfar Barnard, L.; Lloyd, B. Tackling cold housing and fuel poverty in New Zealand: A review of policies, research, and health impacts. Energy Policy 2011, 49, 134–142. [Google Scholar] [CrossRef]
- Keall, M.; Baker, M.G.; Howden-Chapman, P.; Cunningham, M.; Ormandy, D. Assessing housing quality and its impact on health, safety and sustainability. J. Epidemiol. Community Health 2010, 64, 765–771. [Google Scholar] [CrossRef] [Green Version]
- Baker, E.; Pham, N.T.A.; Daniel, L.; Bentley, R.J. New evidence on mental health and housing affordability in cities: A quantile regression approach. Cities 2020, 96, 102455. [Google Scholar] [CrossRef]
- Mason, K.E.; Baker, E.; Blakely, T.; Bentley, R. Housing affordability and mental health: Does the relationship differ for renters and home purchasers? Soc. Sci. Med. 2013, 94, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Morris, A. Housing tenure and the health of older Australians dependent on the age pension for their income. Hous. Stud. 2018, 33, 77–95. [Google Scholar] [CrossRef]
- Li, B.; Chen, S. Aging, living arrangements, and housing in China. Ageing Int. 2010, 36, 463–474. [Google Scholar] [CrossRef]
- National Bureau of Statistics: China Statistical Yearbook 2020; China Statistics Press: Beijing, China, 2020.
- Baeten, S.; Van Ourti, T.; van Doorslaer, E. Rising inequalities in income and health in China: Who is left behind? J. Health Econ. 2013, 32, 1214–1229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- United Nations Population Division: World Population Prospects: 2019 Revision; United Nations: New York, NY, USA, 2019.
- Tang, S.; Meng, Q.; Chen, L.; Bekedam, H.; Evans, T.; Whitehead, M. Tackling the challenges to health equity in China. Lancet 2008, 372, 1493–1501. [Google Scholar] [CrossRef]
- WHO. China Country Assessment Report on Ageing and Health; Geneva Department of Ageing and Life Course: Geneva, Switzerland; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Zhao, R.; Zhao, Y. The gender pension gap in China. Fem. Econ. 2018, 24, 218–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Funke, M.; Leiva-Leon, D.; Tsang, A. Mapping China’s time-varying house price landscape. Reg. Sci. Urban Econ. 2019, 78, 103464. [Google Scholar] [CrossRef]
- Tsai, I.C.; Chiang, S.-H. Exuberance and spillovers in housing markets: Evidence from first- and second-tier cities in China. Reg. Sci. Urban Econ. 2019, 77, 75–86. [Google Scholar] [CrossRef]
- Cui, C.; Deng, W.; Lu, T. Pathways to homeownership in urban China: Transitions and generational fractures. J. Hous. Built Environ. 2019, 36, 1–19. [Google Scholar] [CrossRef]
- Gan, L.; Yin, Z.; Jia, N.; Xu, S.; Ma, S.; Zheng, L. Data You Need to Know about China: Research Report of China Household Finance Survey 2012; Springer: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Cheng, Y.; Rosenberg, M.W.; Wang, W.; Yang, L.; Li, H. Access to residential care in Beijing, China: Making the decision to relocate to a residential care facility. Ageing Soc. 2011, 32, 1277–1299. [Google Scholar] [CrossRef]
- Tan, S.; Wang, S.; Cheng, C. Change of Housing Inequality in Urban China and Its Decomposition: 1989–2011. Soc. Indic. Res. 2016, 22, 1–17. [Google Scholar] [CrossRef]
- Yu, J.; Rosenberg, M.W. “No place like home”: Aging in post-reform Beijing. Health Place 2017, 46, 192–200. [Google Scholar] [CrossRef]
- Huang, Y.; Yi, D.; Clark, W.A.V. Multiple home ownership in Chinese cities: An institutional and cultural perspective. Cities 2020, 97, 102518. [Google Scholar] [CrossRef]
- WHO. Global Age-Friendly Cities: A Guide; WHO: Geneva, Switzerland, 2007. [Google Scholar]
- Burgard, S.A.; Seefeldt, K.S.; Zelner, S. Housing instability and health: Findings from the Michigan recession and recovery study. Soc. Sci. Med. 2012, 75, 2215–2224. [Google Scholar] [CrossRef]
- Kavanagh, A.M.; Aitken, Z.; Baker, E.; LaMontagne, A.D.; Milner, A.; Bentley, R. Housing tenure and affordability and mental health following disability acquisition in adulthood. Soc. Sci. Med. 2016, 151, 225–232. [Google Scholar] [CrossRef]
- Pollack, C.E.; Griffin, B.A.; Lynch, J. Housing affordability and health among homeowners and renters. Am. J. Prev. Med. 2010, 39, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Munford, L.A.; Fichera, E.; Sutton, M. Is owning your home good for your health? Evidence from exogenous variations in subsidies in England. Econ. Hum. Biol. 2020, 39, 100903. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Liu, Z. Housing stress and mental health of migrant populations in urban China. Cities 2018, 81, 172–179. [Google Scholar] [CrossRef]
- Wang, S.; Cheng, C.; Tan, S. Housing determinants of health in urban China: A structural equation modeling analysis. Soc. Indic. Res. 2018, 143, 1245–1270. [Google Scholar] [CrossRef]
- Chung, R.Y.-N.; Chung, G.K.-K.; Gordon, D.; Mak, J.K.-L.; Zhang, L.-F.; Chan, D.; Lai, F.T.T.; Wong, H.; Wong, S.Y.-S. Housing affordability effects on physical and mental health: Household survey in a population with the world’s greatest housing affordability stress. J. Epidemiol. Community Health 2019, 74, 164. [Google Scholar] [CrossRef] [Green Version]
- Zhao, Y.; Hu, Y.; Smith, J.P.; Strauss, J.; Yang, G. Cohort profile: The China Health and Retirement Longitudinal Study (CHARLS). Int. J. Epidemiol. 2014, 43, 61–68. [Google Scholar] [CrossRef] [Green Version]
- Zhao, Y.; Strauss, J.; Chen, X.; Wang, Y.; Gong, J.; Meng, Q.; Wang, G.; Wang, H. China Health and Retirement Longitudinal Study Wave 4 User’s Guide; National School of Development, Peking University: Beijing, China, 2020. [Google Scholar]
- Chen, X.; Crimmins, E.; Hu, P.; Kim, J.K.; Meng, Q.; Strauss, J.; Wang, Y.; Zeng, J.; Zhang, Y.; Zhao, Y. Venous blood-based biomarkers in the China Health and Retirement Longitudinal Study: Rationale, design, and results from the 2015 wave. Am. J. Epidemiol. 2019, 188, 1871–1877. [Google Scholar] [CrossRef]
- Wu, C.; Newman, A.B.; Dong, B.-R.; Odden, M.C. Index of Healthy Aging in Chinese older adults: China Health and Retirement Longitudinal Study. J. Am. Geriatr. Soc. 2018, 66, 1303–1310. [Google Scholar] [CrossRef]
- Fried, L.P.; Borhani, N.O.; Enright, P.; Furberg, C.D.; Gardin, J.M.; Kronmal, R.A.; Kuller, L.H.; Manolio, T.A.; Mittelmark, M.B.; Newman, A.; et al. The cardiovascular health study: Design and rationale. Ann. Epidemiol. 1991, 1, 263–276. [Google Scholar] [CrossRef]
- Kuller, L.H.; Arnold, A.M.; Longstreth, W.; Manolio, T.A.; O’Leary, D.H.; Burke, G.L.; Fried, L.P.; Newman, A.B. White matter grade and ventricular volume on brain MRI as markers of longevity in the cardiovascular health study. Neurobiol. Aging 2007, 28, 1307–1315. [Google Scholar] [CrossRef] [PubMed]
- Fong, T.G.; Fearing, M.A.; Jones, R.N.; Shi, P.; Marcantonio, E.R.; Rudolph, J.L.; Yang, F.M.; Kiely, K.D.; Inouye, S.K. Telephone Interview for Cognitive Status: Creating a crosswalk with the Mini-Mental State Examination. Alzheimers Dement. 2009, 5, 492–497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luo, Y.; Zhang, L.; Pan, X. Neighborhood environments and cognitive decline among middle-aged and older people in China. J. Gerontol. Ser. B 2019, 74, e60–e71. [Google Scholar] [CrossRef] [PubMed]
- Lei, X.; Liu, H. Gender difference in the impact of retirement on cognitive abilities: Evidence from urban China. J. Comp. Econ. 2018, 46, 1425–1446. [Google Scholar] [CrossRef]
- Smith, J.P.; McArdle, J.J.; Willis, R. Financial decision making and cognition in a family context. Econ. J. 2010, 120, F363–F380. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Du, X.; Hu, B.; Jiang, L.; Wan, X.; Fan, L.; Wang, F.; Cao, C. Implication of CKD-EPI equation to estimate glomerular filtration rate in Chinese patients with chronic kidney disease. Ren. Fail. 2011, 33, 859–865. [Google Scholar] [CrossRef]
- Zuo, L.; Ma, Y.-C.; Zhou, Y.-H.; Wang, M.; Xu, G.-B.; Wang, H.-Y. Application of GFR-estimating equations in Chinese patients with chronic kidney disease. Am. J. Kidney Dis. 2005, 45, 463–472. [Google Scholar] [CrossRef]
- Brenner, D.R.; Scherer, D.; Muir, K.; Schildkraut, J.; Boffetta, P.; Spitz, M.R.; Le Marchand, L.; Chan, A.T.; Goode, E.L.; Ulrich, C.M.; et al. A review of the application of inflammatory biomarkers in epidemiologic cancer research. Cancer Epidemiol. Biomark. Prev. 2014, 23, 1729–1751. [Google Scholar] [CrossRef] [Green Version]
- Evandrou, M.; Falkingham, J.; Feng, Z.; Vlachantoni, A. Individual and province inequalities in health among older people in China: Evidence and policy implications. Health Place 2014, 30, 134–144. [Google Scholar] [CrossRef] [Green Version]
- Jackson, A.S.; Janssen, I.; Sui, X.; Church, T.S.; Blair, S.N. Longitudinal changes in body composition associated with healthy ageing: Men, aged 20–96 years. Br. J. Nutr. 2012, 107, 1085–1091. [Google Scholar] [CrossRef] [Green Version]
- Maresova, P.; Javanmardi, E.; Barakovic, S.; Barakovic Husic, J.; Tomsone, S.; Krejcar, O.; Kuca, K. Consequences of chronic diseases and other limitations associated with old age—A scoping review. BMC Public Health 2019, 19, 1431. [Google Scholar] [CrossRef]
- Sanders, J.L.; Boudreau, R.M.; Penninx, B.W.; Simonsick, E.M.; Kritchevsky, S.B.; Satterfield, S.; Harris, T.B.; Bauer, D.C.; Newman, A.B. For the Health ABCS: Association of a modified physiologic index with mortality and incident disability: The Health, Aging, and Body Composition Study. J. Gerontol. Ser. A 2012, 67, 1439–1446. [Google Scholar] [CrossRef] [Green Version]
- Sanders, J.L.; Minster, R.L.; Barmada, M.M.; Matteini, A.M.; Boudreau, R.; Christensen, K.; Mayeux, R.; Borecki, I.B.; Zhang, Q.; Perls, T.; et al. Heritability of and mortality prediction with a longevity phenotype: The Healthy Aging Index. J. Gerontol. Ser. A 2013, 69, 479–485. [Google Scholar] [CrossRef] [Green Version]
- Chen, X.; Wang, T.; Busch, S.H. Does money relieve depression? Evidence from social pension expansions in China. Soc. Sci. Med. 2019, 220, 411–420. [Google Scholar] [CrossRef]
- Hu, H.; Si, Y.; Chen, X. Social pension expansions and health-care utilisation in China: Cross-sectional evidence from the New Rural Pension Scheme. Lancet 2019, 394, S91. [Google Scholar] [CrossRef]
- Zhou, M.; Wang, H.; Zeng, X.; Yin, P.; Zhu, J.; Chen, W.; Li, X.; Wang, L.; Wang, L.; Liu, Y.; et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 394, 1145–1158. [Google Scholar] [CrossRef] [Green Version]
- Rodriguez-Blazquez, C.; Frades-Payo, B.; Forjaz, M.J.; Ayala, A.; Martinez-Martin, P.; Fernandez-Mayoralas, G.; Rojo-Perez, F. Spanish group on quality of life and ageing. Psychometric properties of the International Wellbeing Index in community-dwelling older adults. Int. Psychogeriatr. 2010, 23, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Martín, P.; Fernández-Mayoralas, G.; Frades-Payo, B.; Rojo-Pérez, F.; Petidier, R.; Rodríguez-Rodríguez, V.; Forjaz, M.J.; Prieto-Flores, M.E.; de Pedro Cuesta, J. Validación de la Escala de Independencia Funcional [Validation of the functional independence scale]. Gac. Sanit. 2009, 23, 49–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Daskalopoulou, C.; Chua, K.C.; Koukounari, A.; Caballero, F.F.; Prince, M.; Prina, A.M. Development of a healthy ageing index in Latin American countries—A 10/66 dementia research group population-based study. BMC Med. Res. Methodol. 2019, 19, 226. [Google Scholar] [CrossRef] [Green Version]
- Firpo, S.; Fortin, N.M.; Lemieux, T. Unconditional quantile regressions. Econometrica 2009, 77, 953–973. [Google Scholar]
- Jolliffe, D. Overweight and poor? On the relationship between income and the body mass index. Econ. Hum. Biol. 2011, 9, 342–355. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jann, B. The Blinder-Oaxaca decomposition for linear regression models. Stata J. 2008, 8, 453–479. [Google Scholar] [CrossRef] [Green Version]
- Fang, H.; Feng, J. The Chinese Pension System; National Bureau of Economic Research: Cambridge, MA, USA, 2018. [Google Scholar]
- Ning, M.; Gong, J.; Zheng, X.; Zhuang, J. Does New Rural Pension Scheme decrease elderly labor supply? Evidence from CHARLS. China Econ. Rev. 2016, 41, 315–330. [Google Scholar] [CrossRef]
- Wang, Y.; Yang, Q.; Xin, L.; Zhang, J. Does the New Rural Pension System promote farmland transfer in the context of aging in rural China: Evidence from the CHARLS. Int. J. Environ. Res. Public Health 2019, 16, 3592. [Google Scholar] [CrossRef] [Green Version]
- Cattaneo, M.D.; Galiani, S.; Gertler, P.J.; Martinez, S.; Titiunik, R. Housing, health, and happiness. Am. Econ. J. Econ. Policy 2009, 1, 75–105. [Google Scholar] [CrossRef] [Green Version]
- Krieger, J.; Higgins, D.L. Housing and health: Time again for public health action. Am. J. Public Health 2002, 92, 758–768. [Google Scholar] [CrossRef]
- Davies, J.-M.; Mazumder, A. Health and environmental policy issues in Canada: The role of watershed management in sustaining clean drinking water quality at surface sources. J. Environ. Manag. 2003, 68, 273–286. [Google Scholar] [CrossRef]
- Hunter, P.R.; Zmirou-Navier, D.; Hartemann, P. Estimating the impact on health of poor reliability of drinking water interventions in developing countries. Sci. Total Environ. 2009, 407, 2621–2624. [Google Scholar] [CrossRef]
- Tao, T.; Xin, K. Public health: A sustainable plan for China’s drinking water. Nat. News 2014, 511, 527. [Google Scholar] [CrossRef] [PubMed]
- Gilbertson, J.; Stevens, M.; Stiell, B.; Thorogood, N. Home is where the hearth is: Grant recipients’ views of England’s Home Energy Efficiency Scheme (Warm Front). Soc. Sci. Med. 2006, 63, 946–956. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomson, H.; Thomas, S. Developing empirically supported theories of change for housing investment and health. Soc. Sci. Med. 2015, 124, 205–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marmot, M. Social determinants of health inequalities. Lancet 2005, 365, 1099–1104. [Google Scholar] [CrossRef]
- Costa-Font, J.; Gil, J. What lies behind socio-economic inequalities in obesity in Spain? A decomposition approach. Food Policy 2008, 33, 61–73. [Google Scholar] [CrossRef] [Green Version]
- Martin, M.A.; Frisco, M.L.; Nau, C.; Burnett, K. Social stratification and adolescent overweight in the United States: How income and educational resources matter across families and schools. Soc. Sci. Med. 2012, 74, 597–606. [Google Scholar] [CrossRef] [Green Version]
- Wang, H.; Yu, Y. Increasing health inequality in China: An empirical study with ordinal data. J. Econ. Inequal. 2016, 14, 41–61. [Google Scholar] [CrossRef]
| Variable | Total | 2011 | 2015 | Mean Difference | |
|---|---|---|---|---|---|
| Mean | SD | Mean | Mean | ||
| Dependent variable | |||||
| CHAI (0–12) | 5.408 | 2.057 | 5.694 | 5.200 | −0.494 *** |
| Independent variable | |||||
| Housing poverty | |||||
| Housing quality poverty (1 = yes, 0 = no) | 0.488 | 0.500 | 0.554 | 0.440 | −0.114 *** |
| No potable water | 0.340 | 0.474 | 0.427 | 0.277 | −0.150 *** |
| No toilet for sole use | 0.247 | 0.431 | 0.281 | 0.222 | −0.059 *** |
| No kitchen | 0.086 | 0.280 | 0.090 | 0.083 | −0.007 ** |
| Housing quantity poverty (1 = yes, 0 = no) | |||||
| Rooms per household member <1 | 0.397 | 0.489 | 0.471 | 0.344 | −0.127 *** |
| Housing quality–quantity poverty (1 = yes, 0 = no) | 0.214 | 0.410 | 0.279 | 0.167 | −0.112 *** |
| Control variable | |||||
| Age group | 67.696 | 6.227 | 67.714 | 67.682 | −0.032 |
| 60–64 | 0.384 | 0.486 | 0.398 | 0.374 | −0.024 ** |
| 65–69 | 0.280 | 0.449 | 0.262 | 0.293 | 0.031 *** |
| 70–74 | 0.180 | 0.384 | 0.175 | 0.183 | 0.008 |
| 75–79 | 0.105 | 0.307 | 0.112 | 0.100 | −0.012 * |
| ≥80 | 0.051 | 0.221 | 0.053 | 0.050 | −0.003 |
| Gender (1 = male, 0 = female) | 0.498 | 0.500 | 0.501 | 0.497 | −0.004 |
| Marital status (1 = married, 0 = other) | 0.798 | 0.401 | 0.798 | 0.798 | 0.000 |
| Current residence (1 = rural, 0 = urban) | 0.648 | 0.478 | 0.656 | 0.642 | −0.014 |
| Educational level | 1.686 | 0.906 | 1.633 | 1.724 | 0.091 *** |
| Illiterate | 0.559 | 0.497 | 0.579 | 0.545 | −0.034 *** |
| Primary school | 0.253 | 0.435 | 0.258 | 0.250 | −0.008 |
| Middle school | 0.130 | 0.336 | 0.113 | 0.141 | 0.028 *** |
| High school or higher | 0.058 | 0.233 | 0.049 | 0.064 | 0.015 *** |
| Chronic disease (1 = yes, 0 = no) | 0.838 | 0.369 | 0.788 | 0.874 | 0.086 *** |
| Overweight (BMI ≥ 24 kg/m2) | 0.404 | 0.491 | 0.369 | 0.429 | 0.060 *** |
| Smoking (1 = yes, 0 = no) | 0.290 | 0.454 | 0.306 | 0.278 | −0.028 *** |
| Physical activity (1 = yes, 0 = no) | 0.140 | 0.347 | 0.122 | 0.152 | 0.030 *** |
| Social activity (1 = yes, 0 = no) | 0.458 | 0.498 | 0.443 | 0.468 | 0.025 ** |
| Pension (1 = yes, 0 = no) | 0.612 | 0.487 | 0.435 | 0.740 | 0.305 *** |
| Log (HH expenditure per capita) | 8.899 | 0.039 | 8.590 | 9.137 | 0.547 *** |
| Obs. | 8839 | 3732 | 5107 | ||
| Variable | OLS | ||
|---|---|---|---|
| Housing Poverty | (1) | (2) | (3) |
| Housing quality poverty | 0.099 ** | ||
| (0.044) | |||
| Housing quantity poverty | 0.043 | ||
| (0.041) | |||
| Housing quality–quantity poverty | 0.096 * | ||
| (0.053) | |||
| HH expenditure per capita | −0.112 *** | −0.115 *** | −0.112 *** |
| (0.025) | (0.025) | (0.025) | |
| Year dummy | YES | YES | YES |
| Province dummy | YES | YES | YES |
| Observations | 8839 | 8839 | 8839 |
| R2 | 0.253 | 0.253 | 0.253 |
| Variables | 25th | 50th | 75th | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Housing Poverty | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) |
| Housing quality poverty | 0.124 ** | 0.033 ** | 0.141 ** | ||||||
| (0.052) | (0.048) | (0.060) | |||||||
| Housing quantity poverty | 0.131 *** | 0.005 | 0.060 | ||||||
| (0.049) | (0.046) | (0.057) | |||||||
| Housing quality–quantity poverty | 0.116 * | 0.037 * | 0.138 * | ||||||
| (0.063) | (0.059) | (0.073) | |||||||
| HH expenditure per capita | −0.127 *** | −0.124 *** | −0.128 *** | −0.130 *** | −0.133 *** | −0.130 *** | −0.048 | −0.053 | −0.049 |
| (0.030) | (0.030) | (0.030) | (0.028) | (0.028) | (0.028) | (0.035) | (0.035) | (0.035) | |
| Year dummy | YES | YES | YES | YES | YES | YES | YES | YES | YES |
| Province dummy | YES | YES | YES | YES | YES | YES | YES | YES | YES |
| Observations | 8839 | 8839 | 8839 | 8839 | 8839 | 8839 | 8839 | 8839 | 8839 |
| R2 | 0.116 | 0.116 | 0.116 | 0.158 | 0.158 | 0.158 | 0.151 | 0.150 | 0.151 |
| Contribution (%) | Contribution (%) | Contribution (%) | ||||
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| CHAI: CHARLS 2011 | 5.685 *** | 5.685 *** | 5.685 *** | |||
| CHAI: CHARLS 2015 | 5.216 *** | 5.216 *** | 5.216 *** | |||
| Total difference | −0.469 *** | −0.469 *** | −0.469 *** | |||
| Explained part | −0.149 *** | 31.77 | −0.146 *** | 31.13 | −0.149 *** | 31.77 |
| Unexplained part | −0.321 *** | 68.44 | −0.324 *** | 69.08 | −0.321 *** | 68.44 |
| Explained part | ||||||
| Housing quality poverty | −0.012 *** | 8.05 | ||||
| (0.006) | ||||||
| Housing quantity poverty | −0.006 | 4.11 | ||||
| (0.007) | ||||||
| Housing quality–quantity poverty | −0.011 ** | 7.38 | ||||
| (0.007) | ||||||
| HH expenditure per capita | −0.061 ** | 40.94 | −0.063 ** | 43.15 | −0.061 ** | 40.94 |
| (0.020) | (0.020) | (0.020) |
| Quantiles | 25th | 50th | 75th | ||||||
|---|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | |
| CHAI: CHARLS 2011 | 4.662 | 6.145 | 7.580 | ||||||
| CHAI: CHARLS 2015 | 4.176 | 5.628 | 7.147 | ||||||
| Total difference | −0.486 *** | −0.517 *** | −0.434 *** | ||||||
| Explained part | 37.24 | 37.24 | 37.24 | 34.43 | 33.46 | 34.82 | 35.02 | 32.72 | 34.56 |
| Unexplained part | 62.76 | 62.76 | 62.76 | 65.57 | 66.54 | 65.18 | 64.75 | 67.05 | 65.44 |
| Explained part | |||||||||
| Housing quality poverty | 7.18 | 14.04 | 23.03 | ||||||
| Housing quantity poverty | 7.18 | 8.09 | 9.86 | ||||||
| Housing quality and quantity poverty | 7.18 | 16.11 | 20.00 | ||||||
| HH expenditure per capita | 50.83 | 50.28 | 50.28 | 62.91 | 67.05 | 60.56 | 36.84 | 44.37 | 36.67 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nie, P.; Li, Y.; Ding, L.; Sousa-Poza, A. Housing Poverty and Healthy Aging in China: Evidence from the China Health and Retirement Longitudinal Study. Int. J. Environ. Res. Public Health 2021, 18, 9911. https://doi.org/10.3390/ijerph18189911
Nie P, Li Y, Ding L, Sousa-Poza A. Housing Poverty and Healthy Aging in China: Evidence from the China Health and Retirement Longitudinal Study. International Journal of Environmental Research and Public Health. 2021; 18(18):9911. https://doi.org/10.3390/ijerph18189911
Chicago/Turabian StyleNie, Peng, Yan Li, Lanlin Ding, and Alfonso Sousa-Poza. 2021. "Housing Poverty and Healthy Aging in China: Evidence from the China Health and Retirement Longitudinal Study" International Journal of Environmental Research and Public Health 18, no. 18: 9911. https://doi.org/10.3390/ijerph18189911
APA StyleNie, P., Li, Y., Ding, L., & Sousa-Poza, A. (2021). Housing Poverty and Healthy Aging in China: Evidence from the China Health and Retirement Longitudinal Study. International Journal of Environmental Research and Public Health, 18(18), 9911. https://doi.org/10.3390/ijerph18189911







